Abstract
Oral submucous fibrosis is a chronic debilitating disease characterized by gradually increasing fibrosis of the oral cavity and pharynx, mainly the buccal mucosa, resulting in trismus. Prepotency of the disease is seen in the Indian subcontinent, with its highest incidence in South India due to various deleterious habits. In spite of the numerous medical modalities employed in the management of oral submucous fibrosis, occasionally surgical intervention becomes inevitable. Various flaps have been used to reconstruct the surgical defects following excision of fibrous bands. Undoubtedly; the buccal fat pad remains the most versatile because of its excellent blood supply and minimal donor site morbidity. Here we present a case of severe oral submucous fibrosis surgically treated and reconstructed using buccal fat pad.
Keywords: Buccal fat pad, oral submucous fibrosis, reconstruction
INTRODUCTION
The buccal fat pad is a supple and lobulated mass, easily accessible and mobilized. It was first described in 1977 by Egyedi for the closure of oroantral communications after oncological resections.[1] In 1983, Neder keyed out the use of buccal fat pad as a free graft for intraoral defects.[2] Tideman et al's discovery that the unlined pedicled fat pad graft could epithelize within 2 to 3 weeks surpassed the use of split thickness skin graft.[3] The accelerated wound healing property of the buccal fat pad can be attributed to its rich vascular supply through an abundant network of vascular anastomoses through the small branches of facial, internal maxillary and superficial temporal artery and veins.[4] Samman et al-, had shown histological evidence of wound healing in 2–3 weeks.[5] The fat cells are completely replaced with relatively acellular fibrous tissue and covered by stratified squamous epithelium. The clinical application of the buccal fat pad is strongly grounded on the results of studies on its anatomy and clinical significance by Tideman et al.[3] and Stuzin et al.[4]
Oral submucous fibrosis is a chronic progressive disease of the oral cavity, resulting in blanching, fibrosis and marble-like appearance of oral mucosa, which in later stages causes severe scarring, leading to limited mouth opening often referred to as trismus. This may be treated surgically or nonsurgically, with usually unpredictable results. Surgical treatment is warranted in patients with marked limitation of mouth opening, where fibrous bands are excised and the surgical defects reconstructed utilizing various grafts like split thickness skin graft, tongue flap, nasolabial flap and palatal island flap.
We employed the usage of buccal fat pad for intraoral reconstruction in the following case, which yielded excellent results.
CASE REPORT
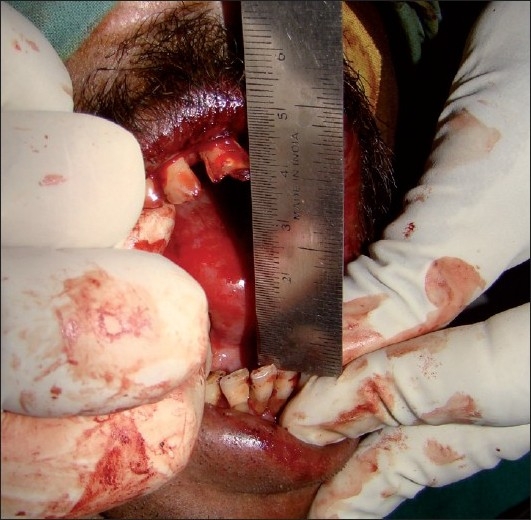
A 38 year-old male patient presented to the Department of Oral and Maxillofacial Surgery with a 10- year history of progressive inability to open the mouth. He had the habit of betel nut chewing for the past 20 years. Intraoral examination revealed blanching and the presence of dense fibrotic bands in the buccal, palatal and retromolar pad areas, extending upto anterior faucial regions of the oral mucosa. The interincisal distance at the time of presentation was 14 mm [Figure 1]. He was diagnosed as a case of severe oral submucosal fibrosis. After routine investigations, he was taken up for surgical excision of fibrous bands and reconstruction using buccal fat pad.
Figure 1.

Preoperative trismus
Under general anesthesia with nasal intubation, bilateral incisions were made in the buccal mucosa at the level of the occlusal plane away from Stensen's duct orifice. Anteriorly, a vertical releasing incision was made to prevent tearing of the commissure of lip [Figure 2]. The wounds created were further freed by digital manipulation and fibrous bands were sectioned. The mouth was then forced open with a mouth gag and an interincisal opening of 23 mm was recorded [Figure 3]. The anterior border of the ramus upto the coronoid process was then exposed through the same wound. Bilateral coronoidectomies were done, which further improved the mouth opening to 40 mm [Figure 4].
Figure 2.

Standard incision for releasing fibrous bands in oral submucous fibrosis
Figure 3.

Mouth opening achieved after bilateral release of fibrous bands
Figure 4.
Mouth opening achieved after bilateral coronoidectomies
The buccal fat pad was approached through the postero-superior margin of the surgical wound [Figure 5]. The fat was gently teased out, interposed in the raw area and was secured to the margins of the wound using 3-0 vicryl sutures. The same procedure was carried out on the contralateral side.
Figure 5.
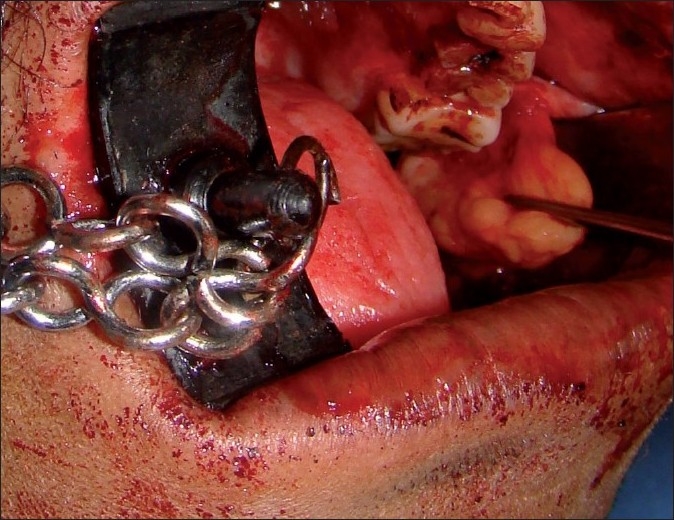
Buccal fat pad being teased out to cover the surgical defect
Postoperative period was uneventful. Mouth opening exercises were started on the third day. The patient was discharged on the fourth day with instructions to maintain proper oral hygiene and to continue active oral dilatation exercises. At 2 weeks follow-up, the oral wounds had healed well [Figure 6]. The patient reported no pain or intolerance to spicy foods. A passive mouth opening of 35 mm and a forceful mouth opening of 40 mm has been maintained [Figure 7]. The patient is currently under regular follow-up.
Figure 6.

Postoperative healing after 2 weeks
Figure 7.

Postoperative relief of trismus
DISCUSSION
Oral submucous fibrosis is a chronic inflammatory disease affecting the oral mucosa and has a high risk of malignant transformation. This disease is predominantly found in the Indian subcontinent. The highest incidence is found in South India, with an overall prevalence rate of 2.5% in various states of the country.[6] Though the exact etiology is not known, chronic irritation due to habit of chewing betel nut in various forms is considered as a major contributory factor. Experimentally, alkaloid component of the arecanut, Arecoline and Capsaicin, the active irritant in chillies have been implicated. Numerous medical and surgical modalities have been proposed to alleviate the signs and symptoms of the disorder. Conservative measures include topical application of vitamin A, steroids and oral iron applications in milder cases[7] to local submucosal injection of placental extract, steroids and hyaluronidase for moderate cases.[8] But in severe cases, surgical excision of the fibrotic bands and reconstruction with a graft is the popular and accepted treatment of choice.
Traditionally, the buccal fat pad has been considered as a nuisance when it accidentally herniates into mouth during intraoral surgery,[9] where it is treated by excision or reduction and mucosal suturing. Yen, who first described the application of buccal fat pad for oral submucosal fibrosis,[10] found that a pedicled graft of buccal fat enables closure of oral defects up to 3 × 5 cm and 6 mm in thickness with no obliteration of the oral vestibule and very little morbidity at the donor site as compared to other local flaps. Mehrotra et al. also used buccal fat pad in various maxillofacial surgeries like submucosal fibrosis, oroantral fistulae and scar tissue adhesions in the cheek with good results.[11]
The buccal fat pad is a mass of specialized fatty tissue which is distinct from subcutaneous fat. It is termed syssarcosis-; it enhances intermuscular motion. It consists of a main body and five extensions: buccal, pterygopalatine, pterygomandibular, superficial and deep temporal. The body is centrally positioned and is located above the parotid duct and extends along the anterior border of masseter muscle. It courses medially to rest on the periosteum of the posterior maxilla and overlies the uppermost fibres of buccinator muscle. The buccal extension lies superficially within the cheek. The superficial and deep temporal extensions reside in the temporal region.
The numerous advantages of employing buccal fat pad include ease of accessibility through the very incision used for creating surgical defect, thereby obviating the necessity of an alternative donor site and its ensuing morbidity. In addition, the buccal fat pad can be teased out and spread to cover the depth and width of the surgical defect, unlike just the superficial thin layer as seen in a split thickness skin graft. The buccal fat pad as a donor tissue is not involved in the pathological process unlike other donor tissues such as the tongue or palate. It also improves the physiological functions of cheek by regaining its suppleness and elasticity post surgically.[12] The rich vascularity of the pedicled graft ensures its vitality and resistance to infections compared to a free graft.[4] Early return to function with normal eating can be commenced within 5 to 7 days with rapid and predictable wound healing expected confidently. Yeh reported elimination of symptoms such as painful ulceration, burning sensation and intolerance to spicy foods.[12] The buccal fat pad is of course no substitute for early, vigorous and sustained physiotherapy, which continues to be an important perquisite for success. However, the resilience of the graft encourages immediate commencement of mouth opening exercises. These factors make the buccal fat pad a logical, reliable and convenient technique for the treatment of oral submucous fibrosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Egyedi P. Utilization of buccal fat pad for closure of oroantral communication. J Maxillofac Surg. 1977;5:241–3. doi: 10.1016/s0301-0503(77)80117-3. [DOI] [PubMed] [Google Scholar]
- 2.Neder A. Use of buccal fat pad for grafts. Oral Surg Oral Med Oral Pathol. 1983;55:349–51. doi: 10.1016/0030-4220(83)90187-1. [DOI] [PubMed] [Google Scholar]
- 3.Tideman H. Buccal fat pad as a pedicled graft. J Oral Maxillofac Surg. 1986;44:435–8. doi: 10.1016/s0278-2391(86)80007-6. [DOI] [PubMed] [Google Scholar]
- 4.Stuzin JM, Wagstrom L, Kawamto HK, Baker TJ, Wolfe SA. The anatomy and clinical applications of buccal fat pad. Plast Reconstr Surg. 1990;85:29–37. doi: 10.1097/00006534-199001000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Samman N, Cheung LK, Tideman H. The buccal fat pad in oral reconstruction. Int J Oral Maxillofac Surg. 1993;22:2–6. doi: 10.1016/s0901-5027(05)80346-7. [DOI] [PubMed] [Google Scholar]
- 6.Gupta SC. “Mist” an aetiological factor in oral submucosal fibrosis. Indian J Otolaryngol. 1978;30(1):5–6. [Google Scholar]
- 7.Borle RM, Borle SR. Management of oral submucous fibrosis: a conservative approach. J Oral Maxillofac Surg. 1991;49:788–91. doi: 10.1016/0278-2391(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 8.Gupta D, Sharma SC. Oral submucous fibrosis: A new treatment regimen. J Oral Maxillofac Surg. 1988;46:830–3. doi: 10.1016/0278-2391(88)90043-2. [DOI] [PubMed] [Google Scholar]
- 9.Messenger KL, Cloyd W. Traumatic herniation of the buccal fat pad: Report of a case. Oral Surg Oral Med Oral Pathol. 1977;43:41–3. doi: 10.1016/0030-4220(77)90348-6. [DOI] [PubMed] [Google Scholar]
- 10.Yen DJ. Surgical treatment of submucous fibrosis. J Oral Surg. 1986;54:230–69. doi: 10.1016/0030-4220(82)90094-9. [DOI] [PubMed] [Google Scholar]
- 11.Mehrotra D, Bhargav A, Pradhan R, Mohammad S, Singh RK. Buccal fat pad for reconstruction in maxillofacial surgery. Indian J Maxillofac Surg- 2001;16:7–11. [Google Scholar]
- 12.Yeh CJ. Application of the buccal fat pad to the surgical treatment of Oral Submucous Fibrosis. Int J Oral Maxillofac Surg. 1996;25:130–3. doi: 10.1016/s0901-5027(96)80058-0. [DOI] [PubMed] [Google Scholar]


