Abstract
Odontogenic tumors represents a broad spectrum of lesions ranging from benign to malignant to dental hamartomas all arising from odontogenic residues, that is, the odontogenic epithelium, ectomesenchyme with variable amounts of dental hard tissues formed in the same sequence as in normal tooth development. We report two cases of myxoma, which were misdiagnosed initially and latter, reported as odontogenic myxoma; and were treated by conservative surgical excision in one case and radical resection with hemimandibulectomy in the other case.
Keywords: Ectomesenchyme, epithelium, hamartoma, myxoma, odontogenic
INTRODUCTION
The German pathologist Rudolph Virchow was probably the first to describe the histologic features of myxofibroma in 1863, although the lesions of jaws were not particularly mentioned. In 1947, Thoma and Goldman first described myxomas of the jaws. Since then odontogenic myxoma has been a subject of continuous scientific debate.[1]
Odontogenic myxoma is an uncommon benign mesenchymal odontogenic tumor arising from the dental papilla, follicle, or the periodontal ligament. The evidence for its odontogenic origin arises from its almost exclusive location in the tooth—bearing areas of the jaws, its occasional association with missing or unerupted teeth and the presence of odontogenic epithelium. Clinically, odontogenic myxoma is a benign painless, invasive, slowly enlarging mass causing marked asymmetry of the face. It commonly involves the mandibular premolar and molar regions. Females have higher predilection than males. It usually occurs in second and third decades of life and causes expansion of bony cortices, displacement and loosening of teeth.[2] Radiographically, its appearance ranges from unilocular pericoronal radiolucency with variable trabecular pattern giving rise to soap bubble, tennis racquet, or honey comb appearance. The “sunray” or “sunburst” appearance has also been reported in the literature.
Histopathologically, the odontogenic myxoma is characterized by loose, abundant mucoid stroma that contains rounded, spindle shaped or angular cells. Cellular and nuclear pleomorphism is rare, as is mitotic activity. The stroma may be relatively avascular or may exhibit delicate capillaries. Various surgical procedures were mentioned which includes curettage, excision (0.5 mm from apparent normal bony margin), resection (1 cm from apparent bony margin), resection with disarticulation, excision of tumor with dento-alveolarsegment and preservation of the mandibular lower boarder and maxillectomy.[1]
While generally considered a slow-growing neoplasm, odontogenic myxomas may be infiltrative and aggressive with high recurrence rates. Due to poor follow-up and lack of reports, a precise analysis of recurrence rates is still missing. In view of its rarity, diagnostic and operative dilemmas encountered while managing, the present case is herewith reported.
CASE REPORTS
Case 1
A 25-year-old male patient presented at St Joseph Dental College, Eluru with painless gradually progressive swelling in the left side of the jaw for 2 years. The intraoral examination of the maxillary and mandibular arch revealed permanent dentition except for the absence of three-dimensional (3D) molars in the maxillary jaw and amalgam filling of tooth 15, 16, 26 and 46. There was no history of trauma present. The extra oral and general examinations revealed no other abnormalities. On palpation, there was diffuse, non tender swelling of 2 × 2 cm involving tooth 36 with the expansion of cortical plates. Radiographic examination revealed periapical radiolucency involving tooth 36, which extends posteriorly. Based on the clinical and radiographic finding, a provisional diagnosis of odontogenic cyst was made.
Fine needle aspiration was attempted to confirm the provisional diagnosis, but it was inconspicuous and this attempted aspiration precipitated pain and inflammation to the subject. No incisional biopsy was done due to non cooperation of the patient. Keeping the view of provisional diagnosis and small size of the lesion, surgical excision with curettage was done under local anesthesia and the excised tissue was sent for the histopathological examination.
Grossly, the excised mass was brownish-white in color, without encapsulation and soft in consistency [Figure 1]. Cut surface was slimy and gelatinous. Microscopic examination revealed haphazardly arranged stellate, spindle-shaped cells in an abundant, loose myxoid stroma that contains only few collagen fibrils, thus confirming it to be odontogenic myxoma.
Figure 1.
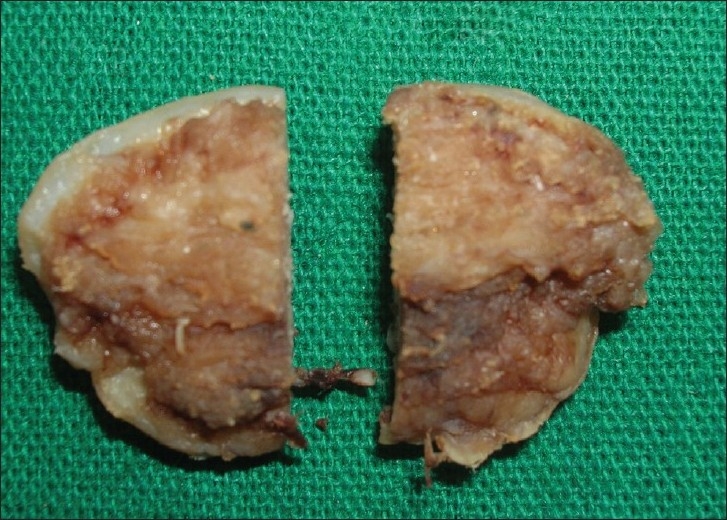
Photograph showing the biopsy specimen of case 1
Case 2
A 26-year female reported to the Department of Oral and Maxillofacial surgery with a chief complaint of swelling on the left side of the face since 1 month. On intraoral examination, the swelling presented as an exophytic growth, soft to firm in consistency and tender. The mucosa overlying the swelling was pale pink in color [Figure 2]. On palpation, the swelling was diffuse, firm, non-fluctuant, hard and tender. Displacement of the teeth along with expansion of buccal and lingual cortical plates was evident. There was no history of trauma present. General examinations revealed no abnormalities. There were no similar findings in any of the family members.
Figure 2.

Preoperative intraoral photograph case 2
The panoramic tomogram was taken which showed well-demarcated multilocular radiolucent lesion with honey comb or tennis racquet appearance [Figure 3]. Hence, the provisional diagnosis of odontogenic keratocyst, ameloblastoma, central giant cell granuloma and odontogenic myxoma was made. Incisional biopsy was performed under local anesthesia and the specimen was sent for the histopathological examination. On examination, the specimen showed a dense and diffuse collection of the fibers and fibroblasts and small inconspicuous strands of odontogenic epithelium. These features confirmed it to be odontogenic fibroma.
Figure 3.

Radiograph showing honeycomb or tennis racquet appearance
Based on the incisional biopsy report, progressive nature of the lesion and cortical expansion, radical resection with hemimandibulectomy was advised. A submandibular approach was followed under general anesthesia to expose this ill-defined mandibular mass [Figure 4]. After the incision through skin, dissection was carried out through subcutaneous tissues, platysma, deep fascia and finally, the pterygomassetric sling with periosteum is divided to approach the inferior border of the mandible. Subperiosteal reflection of the masseter muscle is done along the lateral surface of the mandible to expose the coronoid process, sigmoid notch and condylar neck. The anterior portion of the resection is determined and dissected using the saw blade for complete osteotomy. The temporalis muscle is detached from the coronoid process. The condylar head is separated from lateral pterygoid muscle attachment. The specimen is completely removed and the surgical area is irrigated [Figure 5]. Reconstruction is done by placing the iliac graft, which can be appreciated in the postoperative radiograph [Figure 6]. The resected specimen is sent for the histopathological examination, which discovered it to be odontogenic myxoma [Figure 7].
Figure 4.
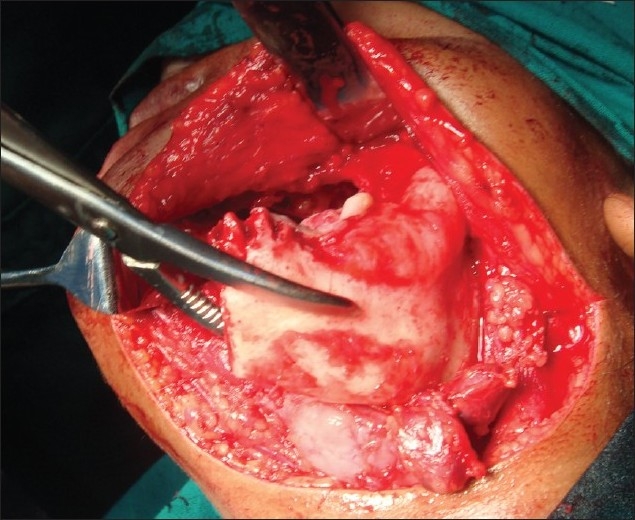
Intraoperative procedure
Figure 5.
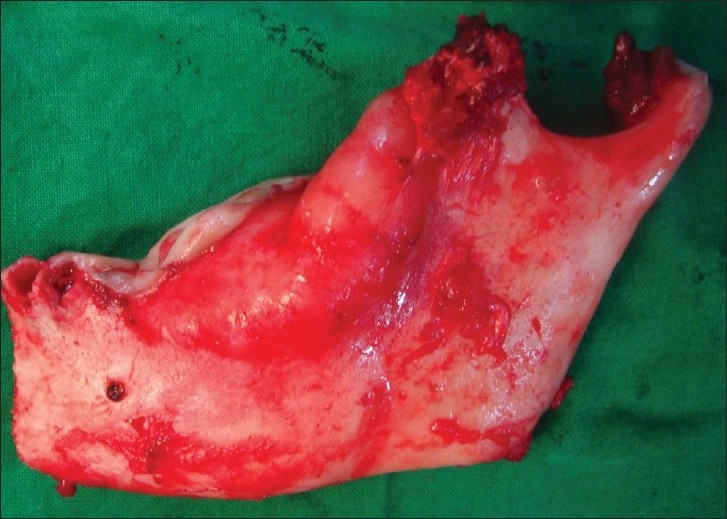
Excised specimen
Figure 6.

OPG showing reconstruction with iliac graft
Figure 7.
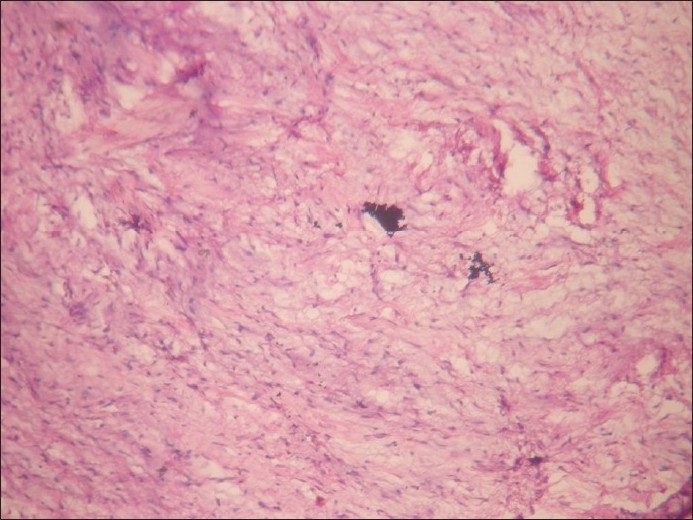
H and E stained section showing stellate, spindle-shaped cells in an abundant, loose myxoid stroma
DISCUSSION
Odonogenic myxoma is a nonencapsulated benign tumor of the jaw bones, comprising around 3–6% of all odontogenic tumors. Previous studies by white et al., refer the tip of the incidence with an age range of 11–70 years, but the majority of the cases are between 10 and 40 years of age.[3,4] Our two cases surpass the second decade of life, but can be addressed within the range referred in the literature. Although its most frequent location is the posterior mandible, other locations such as the incisive sector, upper maxilla and mandibular condyle must be considered.[4] Present cases showed lesion in the mandible with extension in the posterior region of the mandible.
Odontogenic myxoma often grows without symptoms, most commonly presenting as a painless swelling. Pain, displacement of teeth and parasthesia are uncommon, thus the lesion can reach considerable size before the patients becomes aware of its presence and seeks treatment.[5,6] Our cases showed a large mass as the main aspect in physical examination, but in case one patient developed pain after aspiration. Radiologically, the appearance may vary from a unilocular radiolucency to a multicystic lesion with a well defined or diffused margin.[7] A unilocular appearance may be seen more commonly in children and in the anterior parts of the jaws. In tooth-bearing areas, the tumor is often scalloped between the roots; root resorption can occur but is rare. Differential diagnosis must be established with other clinically similar entities, such as simple cyst, ameloblastoma, intraosseous hemangioma, giant cell granuloma, osseous aneurismatic cyst and metastasis.[8,9]
Histologically, odontogenic myxoma shows a spectrum of fibrous connective tissue stroma is present, from myxoid to dense hyalinized and from relatively acellular to cellular. Calcification may or may not be present.[10–14] The variation in the histopathological diagnosis between the initial biopsy as odontogenic fibroma and the final diagnosis as odontogenic myxoma in our case 2 could be attributed either to the biological spectrum of this lesion or non–inclusion of myxomatous areas in the incisional biopsy.[15]
The aggressive nature of odontognic myxoma is well documented in the literature. The tumor is not radiosensitive and treatment is by surgery. Despite surgery it has been established as the treatment of choice of these tumors, no unanimous consensus exists concerning the extension of surgery. Although it is our opinion that enucleation should be avoided, curettage with scarification of the cavity with acrylic bur may be used for small mandibular lesions particularly in the anterior region and especially where the patient is educated and available for periodic reviews. It would appear that for extensive lesions a more radical approach is more appropriate.[10,11] In the present cases, the surgical management involved an intra and extra oral approaches. Prognosis after excision is excellent in this 2-year follow up period in both the cases.
CONCLUSION
Odontogenic myxoma is a slow growing benign, locally malignant tumor, notorious for recurrence. Due to the unspecific nature of these lesions along with diagnostic and operative dilemmas related to myxomatous tumors, a sound knowledge with proper histopathological diagnosis is required for maxillofacial surgeons to improve skills in their management.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Reichart PA, Philipsen HP. Odontogenic tumors and Allied lesions. London: Quintessence publishing Co Ltd; 2004. pp. 189–99. [Google Scholar]
- 2.Shafer WG, Hine MK, Levy BM. A textbook of oral pathology. Philadelphia. P.A: Saunders; 1983. pp. 160–1. (295-7). [Google Scholar]
- 3.Gnepp DR. Diagnostic surgical pathology of head and neck. London: WB Saunders Company Ltd; 2001. p. 643. [Google Scholar]
- 4.Simon EN, Merkx MA, Vuhahula E, Ngassapa D, Stoelinga PJ. Odontogenic myxoma: A clinicopathological study of 33 cases. Int J Oral Maxillofac Surg. 2004;33:333–7. doi: 10.1016/j.ijom.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Spencer KR, Smith A. Odontogenic myxoma: Case report with reconstructive considerations. Aust Dent J. 1998;43:290–12. doi: 10.1111/j.1834-7819.1998.tb00166.x. [DOI] [PubMed] [Google Scholar]
- 6.Slootweg PJ, Wittkamp Myxomas of the jaws.An analysis of 15 cases. J Maxillofac Surg. 1986;14:46–52. doi: 10.1016/s0301-0503(86)80258-2. [DOI] [PubMed] [Google Scholar]
- 7.Wood NK, Goaz PW. Differential diagnosis of oral lesions. St Louis: Mosby; 1987. pp. 543–5. [Google Scholar]
- 8.Peltola J, Magnusson B, Happoren Rp, Bomen H. Odontogenic myxoma - A radiological study of 21 tumors. Br J Oral Maxillofac surg. 1994;32:298–302. doi: 10.1016/0266-4356(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 9.Hernández Vallejo G, Cohn C, García Peñín A, Martínez Lara S, Llanes Menéndez F, Montalvo Moreno JJ. Myxomas of the jaws: Report of three cases. Med Oral. 2001;6:106–13. [PubMed] [Google Scholar]
- 10.Bucci E, Lo Muzio L, Mignogna MD, De Rosa G. Odontogenic myxoma: Report of a case with peculiar features. J Oral Maxillofac surg. 1991;49:91–4. doi: 10.1016/0278-2391(91)90276-r. [DOI] [PubMed] [Google Scholar]
- 11.Adamo AK, Locricchio RC, Freedman P. Myxoma of the mandible treated by peripheral ostectomy and immediate reconstruction. J Oral Surg. 1980;38:530–3. [PubMed] [Google Scholar]
- 12.Halfpenny W, Verey A, Bradsley V. Myxoma of the mandibular condyle.A case report and review of the literature. Oral Surg Oral Med Oral Pathol Endod. 2000;90:348–53. doi: 10.1067/moe.2000.107364. [DOI] [PubMed] [Google Scholar]
- 13.Kangur TT, Dahlin DC, Turlington EG. Myxomatous tumors of the jaws. J Oral Surg. 1975;33:523–8. [PubMed] [Google Scholar]
- 14.Sivakumar G, Kavitha B, Saraswathi TR, Sivapathasundharam B. Odontogenic myxoma of the maxilla. Indian J Dent Res. 2008;19:62–5. doi: 10.4103/0970-9290.38934. [DOI] [PubMed] [Google Scholar]
- 15.Sarode TP, Malik NA. Odontogenic myxoma in a child: Diagnostic and treatment dilemmas. J Indian Soc Pedod Prev Dent. 2002;20:68–72. [PubMed] [Google Scholar]


