Abstract
Human growth and development is a meticulously planned and precisely executed process. Even a mild disturbance can have clinically significant manifestations later on. Even today, ancient beliefs and practices override/delay patient's aspiration for seeking treatment as seen in the case report presented here. Congenital bifid tongue in association with various other orofacial abnormalities has been reported, many of which have been linked to various syndromes. But congenital bifid tongue occurring in the absence of other orofacial abnormalities is very rare. Here, we discuss a case of bifid tongue involving the anterior one-third of tongue, reported in a 45-year-old male patient unusually with no other intraoral abnormalities.
Keywords: Bifid tongue, congenital, syndromes
INTRODUCTION
The tongue develops during the fourth week of intrauterine life, originating from a median swelling, the tuberculum impar on the floor of the pharynx and two lateral lingual swellings joining this central structure. These lateral lingual structures grow rapidly to cover the tuberculum impar to form the anterior two-thirds of the tongue.[1] When this process is disturbed, tip of the tongue is divided longitudinally for a certain distance giving rise to cleft tongue/bifid tongue. The occurrence of bifid tongue in the absence of other orofacial abnormalities is a rare entity by itself and usually receives attention much later compared to those seen in association with certain syndromes.[1]
CASE REPORT
A 45-year-old male patient reported to our department with complaints of difficulty in speech and unusual appearance of tongue. Being a lecturer by profession, the above-mentioned complaint was affecting his professional career as well, which probably prompted to seek consultation at this rather advanced age. Further enquiry revealed that since he was from a conservative Hindu family, his parents considered this bifid tongue as a sign of “good fortune” because it had resemblance to those found in snakes. Snakes are worshipped and considered as holy creatures in Hindu mythology and hence, the patient's parents were against changing something that is “God given”. All this led to delay in seeking treatment earlier. It took a lot of convincing from the patient's part and our part to convince them to allow for surgical correction of the defect.
The patient was healthy, vitals were well within normal limits and he had no contributing family/medical history. Extraoral and intraoral examination negated any other associated congenital orofacial defects [Figure 1].
Figure 1.

Preoperative photograph
Surgical correction of the defect was undertaken under local anesthesia [Figure 2]. The median parts of the defect were freshened and the tongue was reconstructed by suturing the muscles in layers. Post surgical healing was uneventful and no speech therapy sessions were required [Figure 3].
Figure 2.
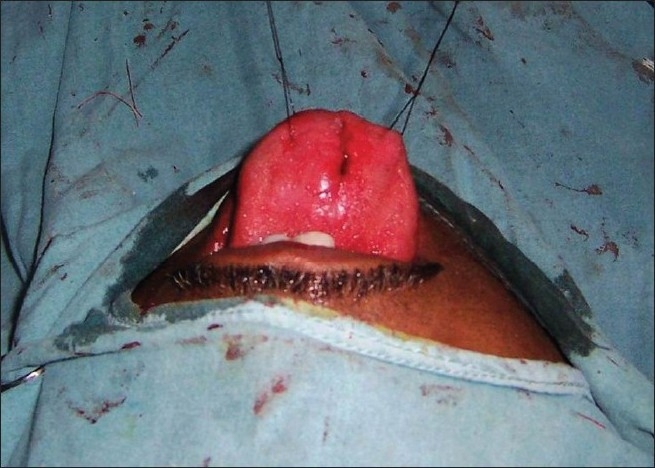
Intraoperative photograph
Figure 3.

Postoperative photograph
DISCUSSION
The literature reports median tongue clefts only to be associated with orofacial digital syndromes type I, II, IV and VI.[2–4] These syndromes are all associated with median lip and/or mandibular clefts and digital variations. Case reports of median tongue clefts in the literature show mostly a combination with a cleft of the median lower lip.[5–7] Bartholdson et al. described a baby boy with a bifid tongue combined with a cleft palate.[8]
The development of the tongue starts at the fourth week of intrauterine life in the floor of the primitive cavity from the first three or four brachial arches.[1] Abnormal/partial/non-fusion of these arches may lead to congenital anomalies of tongue, including bifid tongue. In fact, any process affecting mesenchymal fusion and acting toward the end of fourth week of gestation has been suggested to account for this malformation. They may occur as an isolated entity or a part of clinical syndromes.[9] Aglossia, syndromicmicroglossia, macroglossia, accessory tongue, long tongue and cleft or bifid tongue are the commonest occurrences listed in the order of frequency. The syndromic cases associated with other anomalies receive the early attention of parents and physicians, but non-syndromic cases are neglected and usually present late.
Bifid tongue has been reported in syndromic cases like Opitz G BBB syndrome, oral–facial–digital syndrome type I, Klippel–Feil anomaly and Larsen syndrome.[10–13] Bifid tongue has also been reported as a rare feature associated with infants of diabetic mother syndrome.[14] Literature also gives a reference of bifid tongue as a complication of tongue piercing.[15] Associations have also been postulated with cleft palate, mandibular cleft, midline palatomandibular bony fusion and cervical vertebrae.[16]
Our case cannot be put in any well-defined syndrome. We were unable to identify any associated orofacial abnormalities, genetic predisposition, tongue piercing or history of postnatal trauma.
If the clinical appearance is described without any association to an orofacial syndrome, the Tessier 30 cleft definition could be used as the best description of the symptoms. The Tessier cleft is described as a median cleft from the lower lip to the manubrium sterni, a fissured tongue, an absence of the hyoid bone and a cleft of the manubrium sterni.[17]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Emmanouil-Nikoloussi EN, Kerameos-Foroglou C. Developmental malformations of human tongue and associated syndromes (review) Bull Group Int Rech Sci Stomatol Odontol. 1992;35:5–12. [PubMed] [Google Scholar]
- 2.Martinot VL, Manouvrier S, Anastassov Y, Ribiere J, Pellerin PN. Orodigitofacial syndromes type I and III: Clinical and surgical studies. Cleft Palate Craniofac J. 1994;31:401–8. doi: 10.1597/1545-1569_1994_031_0401_ostiai_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Mattei JF, Ayme S. Syndrome of polydactyly, cleft lip, lingual hamartomas, renal hypoplasia, hearing loss and psychomotor retardation: Variant of the Mohr syndrome or a new syndrome.? J Med Genet. 1983;20:433–5. doi: 10.1136/jmg.20.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wey PD, Neidich JA, Hoffmann LA, LaTrenta GS. Midline defects of the orofaciodigital syndrome type VI (Varandi syndrome) Cleft Palate Craniofac J. 1994;31:397–400. doi: 10.1597/1545-1569_1994_031_0397_mdotos_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 5.Chidzonga MM, Shija JK. Congenital cleft of the lower lip, bifid tongue with ankyloglossia, cleft palate and submental epidermoid cyst: report of a case. J Oral Maxillofac Surg. 1998;46:809–12. doi: 10.1016/0278-2391(88)90196-6. [DOI] [PubMed] [Google Scholar]
- 6.Ishii M, Moriyama T, Enomoto S, Ono T, Ohyama K, Kuroda T. Seventeenyear follow-up of a patient with median cleft of the lower lip, mandible and tongue with flexion contracture: A case report. Cleft Palate Craniofac J. 2002;39:359–65. doi: 10.1597/1545-1569_2002_039_0555_syfuoa_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 7.Martinot-Duquennoy V, Bardot J, Magalon G. Median cleft of the lower lip. Apropos of a case. Ann Chir Plast Esthet. 1991;36:480–5. [PubMed] [Google Scholar]
- 8.Bartholdson L, Hellstrom SO, Sonderberg O. A case of double tongue.Case report. Scand Plast Reconstr Surg Hand Surg. 1991;25:93–5.2. doi: 10.3109/02844319109034931. [DOI] [PubMed] [Google Scholar]
- 9.Mattei JF, Ayme S. Syndrome of polydactyly, cleft lip, lingual hamartomas, renal hypoplasia, hearing loss and psychomotor retardation: variant of the Mohr syndrome or a new syndrome? J Med Genet. 1983;20:433–5. doi: 10.1136/jmg.20.6.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mihci E, Tacoy S, Ozbilim G, Franco B. Oral-Facial- Digital Syndrome Type 1. Indian Pediatrics. 2007;44:854–6. [PubMed] [Google Scholar]
- 11.Orhan D, Balci S, Deren O, Utine EG, Basaran A, Kale G. Prenatally diagnosed lethal type Larsen-like syndrome associated with bifid tongue. Turk J Pediatr. 2008;50:395–9. [PubMed] [Google Scholar]
- 12.Parashar SY, Anderson PJ, Cox TC, McLean N, David DJ. Management of Opitz G BBB Syndrome. Ann Plast Surg. 2005;55:402–7. doi: 10.1097/01.sap.0000174355.56130.0a. [DOI] [PubMed] [Google Scholar]
- 13.Widgerow AD. Klippel-Feil anomaly, cleft palate and bifid tongue. Ann Plast Surg. 1990;25:216–22. doi: 10.1097/00000637-199009000-00014. [DOI] [PubMed] [Google Scholar]
- 14.James AW, Culver K, Hall B, Golabi M. Bifid tongue: A rare feature associated with infants of diabetic mother syndrome. Am J Med Genet. 2007;143A:2035–9. doi: 10.1002/ajmg.a.31877. [DOI] [PubMed] [Google Scholar]
- 15.Fleming PS, Flood TR. Bifid tongue - a complication of tongue piercing. Br Dent J. 2005;198:265–6. doi: 10.1038/sj.bdj.4812117. [DOI] [PubMed] [Google Scholar]
- 16.Rao S, Oak S, Wagh M, Kulkarni B. Congenital midline palatomandibular bony fusion with a mandibular cleft and a bifid tongue. Br J Plast Surg. 1997;50:139–41. doi: 10.1016/s0007-1226(97)91328-x. [DOI] [PubMed] [Google Scholar]
- 17.Verma A, Jain N. Tessie cleft no 30 (median cleft from lower lip to manubrium) Indian J Pediatr. 2001;68:1163–4. doi: 10.1007/BF02722937. [DOI] [PubMed] [Google Scholar]


