Abstract
Ameloblastoma is a slow-growing, persistent and locally aggressive neoplasm of epithelial origin accounting for 10% out of 30% of all odontogenic tumors. According to the World Health Organization, ameloblastomas are classified into the following types: conventional, unicystic, and peripheral. Unicystic ameloblastoma (UA) refers to those cystic lesions that show clinical, radiographic, or gross features of a mandibular cyst, but on histologic examination show a typical ameloblastomatous epithelium lining part of the cyst cavity, with or without luminal and/or mural tumor growth. We report a case of young female with a radiolucent lesion in the right posterior mandible. Surgical removal of the lesion was performed, with differential diagnosis of a radicular cyst. However, histopathologic examination revealed UA. The patient was kept under observation and showed signs of local bone regeneration. The purpose of presenting this report of a clinical case of UA previously misdiagnosed as radicular cyst is to emphasize the significance of histopathologic examination of all tissue specimens recovered in surgery even when clinical and radiological finding are innocuous.
Keywords: Conservative treatment, radicular cyst, unicystic ameloblastoma
INTRODUCTION
Mandibular swellings can be caused by many benign lesions of odontogenic or non-odontogenic origin. The most common tumor of odontogenic origin is ameloblastoma which develops from epithelial cellular elements and dental tissues in various phases of development. It is a slow-growing, persistent and locally aggressive neoplasm of epithelial origin, affecting the posterior area of lower jaw in 80% of cases.[1] There are three forms of ameloblastomas, namely, multicystic, peripheral and unicystic tumors.[2]
The unicystic ameloblastoma (UA) is a less encountered variant of the ameloblastoma. It appears more frequently in the second or third decade with no sexual or racial predilection. It is almost exclusively encountered asymptomatically in the posterior mandible.[3] The clinical and radiological simulation of an UA with mandibular cyst often leads to simple enucleation of lesion.
This report highlights the importance of histopathologic analysis of any pathology in jaws even if it seems innocuous in clinical as well as radiological examination.
CASE REPORT
A 23-year-old female reported in the outpatient department with the chief complaint of an asymptomatic bony hard swelling in respect to the right posterior mandible, which gradually increased in size in the past 3 years to attain the present size of concern. Dental and medical history was insignificant. On clinical examination, there was evidence of a large non-tender, non-compressible, hard swelling measuring 2 × 2 cm on the right body of mandible, about 1 cm anterior to the posterior border of ramus, but no lymphadenopathy was noted. Overlying skin was normal in color, texture and consistency and was not adherent to the underlying swelling.
Intraoral examination revealed a painless swelling in the right posterior mandibular vestibule from right mandibular second premolar to the distal aspect of second molar on the same side. The swelling was firm and covered by normal mucous membrane [Figure 1]. In place of the right mandibular first molar, only root stumps were present, but molar and premolar adjacent to it tested vital.
Figure 1.

Intraoral view
Radiographically, it presented as a unilocular, radiolucent lesion, well circumscribed by a radiopaque border, about 3 × 2 cm, extending from the root of second molar posteriorly to the root of the first premolar anteriorly [Figure 2]. The lesion also caused a displacement of the right inferior alveolar canal toward the cortical inferior border of the mandible.
Figure 2.

Panoramic radiograph demonstrating well defined unilocular radiolucent lesion in the right mandible
The lesion was perforated with a wide bore needle to rule out vascular lesion and aspirate the content. The aspirate was sent for pathological evaluation and the report stated it to be a cystic fluid with inflammatory exudates, confirming the clinical and radiographic diagnosis of radicular cyst in association with root stumps of 46.
So, enucleation of cyst with extraction of root stumps of first molar was planned. Under local anesthesia, an incision was made from distal of third molar to the medial of canine. Mucoperiosteal flap was raised and it was possible to see a thin expanded cortical plate which was removed with a scalpel. The cavity contained fibrous tissue wall full of liquid.
The lesion with all its fibrous tissue lining was enucleated carefully to ensure complete removal. The remaining bone tissue showed normal contour and consistency without any clinical signs of lesion. Root stump of first molar was extracted and mucoperiosteal flap sutured back after thorough curettage and lavage of bony cavity.
The histopathologic examination of the removed lining revealed UA contrary to the provisional diagnosis of radicular cyst [Figure 3]. Hence, root canal of 47 and 45 was done and radiologic observation of patient to monitor the relapse of lesion was chosen as the well-defined cystic envelope ensured the complete removal.
Figure 3.
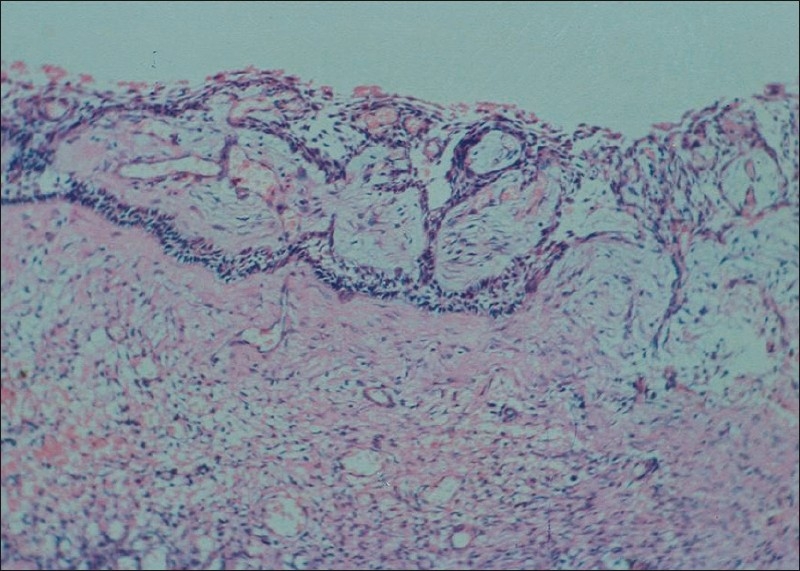
Photomicrograph showing cyst lined by ameloblastic epithelium with hyperchromatic polarized basal layer
Presently, the patient is under follow-up since 1 year without any signs of relapse and with bony restoration in the affected area [Figure 4].
Figure 4.

Panoramic radiograph showing bone regeneration in the affected area during 12-month follow-up
DISCUSSION
UA, first described by Robinson and Martinez in 1977, refers to those cystic lesions that show clinical, radiologic or gross features of a mandibular cyst, but on histologic examination show a typical ameloblastomatous epithelium lining part of the cyst cavity, with/without luminal and/or mural tumor growth. It accounts for 5–10% of all intraosseous ameloblastomas.[3–5] UA is believed to be less aggressive and responds more favourably to conservative surgery than the solid or multicystic ameloblastomas.[6]
Histologically, the minimum criteria for diagnosing a lesion as UA is the demonstration of a single cystic sac lined by odontogenic (ameloblastomatous) epithelium often seen only in focal areas.
In a clinicopathologic study of 57 cases of UA , Ackermann[7] classified this entity into three histologic groups:
-
I.
luminal UA (tumor confined to the luminal surface of the cyst);
-
II.
intraluminal/plexiform UA (nodular proliferation into lumen without infiltration of tumor cells into connective tissue wall); and
-
III.
mural UA (invasive islands of ameloblastomatous epithelium in the connective tissue wall not involving the entire epithelium).
Another subgrouping by Philipsen and Reichart[8] has also been described as follows:
Subgroup 1: luminal UA;
1.2: luminal and intraluminal;
1.2.3: luminal, intraluminal and intramural; and
1.3: luminal and intramural.
The UA diagnosed as subgroups 1 and 1.2 can be treated conservatively (careful evaluation), whereas subgroups 1.2.3 and 1.3 showing intramural growths require radical resection.[3]
In the present case, radiologic presentation suggested a radicular cyst with decayed first molar and vital second molar and first and second premolars, although they were included in the cyst. Moreover, the cytological examination of aspirate taken during initial clinical examination showed normal cystic fluid with few inflammatory cells. Thirdly, there was no root resorption of any tooth which may indicate the aggressive nature of the lesion.
Hence, finally taking into account the age of the patient, clinical and radiologic features, the simple enucleation procedure was chosen as the treatment of choice, for it involves least patient morbidity and effect on the quality of life is minimal. It has also been advocated that vigorous curettage of the bone should be avoided as it may implant foci of ameloblastoma more deeply in bone.[9]
In the present case, histopathologic examination of the enucleated sample showed ameloblastic changes confined to luminal surface of the cyst, i.e. as in group I and subgroup I.
The patient is being followed up at regular intervals to check for any recurrences. Recurrence is also related to the histologic subtypes, among which those invading the fibrous wall have a rate of 35.7%, but others have a rate of only 6.7%.[10] UAs are considered to be less aggressive form of ameloblastomas and can be successfully removed by simple enucleation or less aggressive surgery.
In the present case, the diagnosis was possible only because histopathologic examination was performed in the enucleated material. Hence, we conclude that the surgical protocol must include the postoperative histopathologic examination for all lesions to rule out any ameloblastomatous changes, so that the patient can be followed up properly to take care of any recurrences happening.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Gerzenshtein J, Zhang F, Caplan J, Anand V, Lineaweaver W. Immediate mandibular reconstruction with microsurgical fibula flap transfer following wide resection for ameloblastoma. J Craniofac Surg. 2006;17:178–82. doi: 10.1097/01.scs.0000190350.37978.2c. [DOI] [PubMed] [Google Scholar]
- 2.Philipsen HP, Reichart PA. London: Quintessence Pub Co Ltd; 2004. Classification of odontogenic tumors and allied lesions. Odontogenic tumors and allied lesions; pp. 21–3. [Google Scholar]
- 3.Philipsen HP, Reichart PA. London: Quintessence Pub; 2004. Unicystic ameloblastoma. Odontogenic tumors and allied lesions; pp. 77–86. [Google Scholar]
- 4.Leider AS, Eversole LR, Barkin ME. Cystic ameloblastoma: A clinicopathological analysis. Oral Surg Oral Med Oral Pathol. 1985;60:624–30. doi: 10.1016/0030-4220(85)90366-4. [DOI] [PubMed] [Google Scholar]
- 5.Gardner DG, Corio RL. Plexiform unicystic ameloblastoma: Variant of ameloblastoma with a low recurrence rate after enucleation. Cancer. 1984;53:1730–5. doi: 10.1002/1097-0142(19840415)53:8<1730::aid-cncr2820530819>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 6.Robinson L, Martinez MG. Unicystic ameloblastoma: A prognostically distinct entity. Cancer. 1977;40:2278–85. doi: 10.1002/1097-0142(197711)40:5<2278::aid-cncr2820400539>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 7.Ackermann GL, Altini M, Shear M. The unicystic ameloblastoma: A clinicopathological study of 57 cases. J Oral Pathol. 1988;17:541–6. doi: 10.1111/j.1600-0714.1988.tb01331.x. [DOI] [PubMed] [Google Scholar]
- 8.Chana JS, Chang YM, Wei FC, Shen YF, Chan CP, Lin HN, et al. Segmental mandibulectomy and immediate free fibula osteoseptocutaneous flap reconstruction with endosteal implants: An ideal treatment method for mandibular ameloblastoma. Plast Reconstr Surg. 2004;113:80–7. doi: 10.1097/01.PRS.0000097719.69616.29. [DOI] [PubMed] [Google Scholar]
- 9.Li TJ, Kitano M, Arimura K, Sugihara K. Recurrence of unicystic ameloblastoma: A case report and review of the literature. Arch Pathol Lab Med. 1998;122:371–4. [PubMed] [Google Scholar]
- 10.Li T, Wu Y, Yu S, Yu G. Clinicopathological features of unicystic ameloblastoma with special reference to its recurrence. Zhonghua Kou Qiang Yi Xue Za Zhi. 2002;37:210–2. [PubMed] [Google Scholar]


