Abstract
Aims and objectives:
To compare the success rate of implant placed immediately in extraction socket vs implant placed delayed in extraction socket.
Materials and Methods:
The study comprised of 8 patients (6 male and 2 female, aged from 14 to 58 year) for evaluation of implant placement immediately (i.e. Group – A) or delayed (i.e. Group – B) into extraction site, in which at 12 sites implants were placed.
Results:
The inclusion criteria for implantation was tooth/teeth with one or two degree mobility, root stumps, tooth with failure root canal treatment and extraction sockets. HI-TEC TRX-OP (Life Care) with abutment, non-submerged, tapered at apical 5 mm, sand-blasted & acid etched surfaced implants were used. These are one stage single implants made of commercially pure titanium. The length of implants used was 10 mm and 13 mm and diameter was 3.70 mm and 4.50 mm. The vertical bone dimension was determined by palpation and radiograph (intra-oral periapical, orthopantomograph and dentascan in some patients). Gingival condition, bone condition was examined clinically and radiographically.
Discussion:
Post-operative evaluation was done under clinical parameters (i.e. Pain (VAS), Swelling, Stability (By Glickman method), Gingival status, Probing depth (By Williams Periodontal probe), Patient's compliance / satisfaction, Complications (If any) and Radiological parameters was (Intra-oral periapical radiograph, orthopantomograph, Dentascan).
Conclusion:
Overall conclusion drawn from this study was that both the groups are showing similar results but Group-A is slightly better than Group-B
Keywords: Bone resorption, dental implant, osteosynthesis
INTRODUCTION
Conventional rehabilitation of partial or complete teeth loss has limitations for many people, and such devices can cause eating difficulties, psychological problems and problems related to esthetics, retention and stability of prosthesis. Because of these problems, patients often suffer decreased self-confidence and develop psychological problems. The prosthetic treatments that have been used are removable partial dentures, fixed partial dentures, or composite retained onlay partial dentures. In addition to the risk of complications, most of these treatments include the sacrifice of healthy tooth substance of the adjacent teeth. In order to overcome the problems associated with conventional prosthesis, implants came into existence. Furthermore, the patients wish that their lost teeth should be replaced as earlier as possible in order to continue their normal life without any psychological trauma of being edentulous and to reduce the appointments. The present study was therefore undertaken to evaluate the implant placement immediately and delayed into the extraction site.
Review of literature
Classification of implants according to timing of placement
In the classification of Wilson and Weber,[1] the terms immediate, recent, delayed, and mature are used to describe the timing of implant placement in relation to soft tissue healing and predictability of guided bone regeneration procedures. Gomez-Roman and coworkers[2] defined immediate implants as occurring between 0 and 7 days after tooth extraction. Zitmann et al.[3] considered implant placement as delayed when it occurred between 6 weeks and 6 months after extraction. Mayfield,[4] in his recent classification, used the terms immediate, delayed, and late to describe time intervals of 0 week, 6–10 weeks, and 6 months or more after extraction, respectively. The interval between 10 weeks and 6 months was not addressed. Hammerle and Lang[5] in a report stated placement of delayed implant between 8 and 14 weeks. Schropp and associates[6] defined immediate implantation as implants placed between 3 and 15 days (mean 10 days) following tooth extraction.
Immediate dental implant
Yukna[7] suggested from his study that hydroxyapatite (HA)-coated dental implants can be successfully placed in fresh extraction sockets utilizing otherwise standard implant placement techniques and that they appear to clinically perform equally well in fresh extraction sockets and healed sites. Devorah Schwartz-Arad[8] drew some conclusions after reviewing the relevant literature on immediate dental implants, which are:
-
i)
Implants placed into fresh extraction sockets have a high rate of survival ranging between 93.9 and 100%.
-
ii)
Implants must be placed 3–5 mm beyond the apex in order to gain a maximal degree of stability.
-
iii)
Implants should be placed as close as possible to alveolar crest level (0–3 mm).
-
iv)
There is no consensus regarding the need for gap filling and the best grafting material.
-
v)
The use of membrane does not imply better results; on the contrary, membrane exposure may carry complications in its wake.
-
vi)
The absolute need for primary closure remains to be established.
Parel and Schow[9] concluded from their study that within limited parameters, the one-piece implant design can be used effectively as a basis for restoring single tooth defects. Schwartz-Arard et al.[10] evaluated the survival rates of implants placed immediately after extraction of molar teeth to support a fixed ceramometal prosthesis, and concluded that immediate implantation in the molar region is an alternative, predictable surgical treatment. Immediate implantation in the posterior mandible has a better prognosis than in the posterior maxilla.
Procedure
Kees Heydenrijk et al.[11] concluded that both the crestal incision and the labial flap approach are reliable procedures for insertion of IMZ implants in a single-stage procedure. However, because of the smaller risk of soft tissue overgrowth, there is a preference for the labial flap approach. Vergara and Caffesse reported a protocol in which single molar tooth is replaced immediately with implant, minimizing the need for other surgical procedures.[12] Ugo Covani et al. concluded from their study that successful osseointegration and complete bone healing were observed for all the patients in whom implants were placed immediately after tooth extraction without incision. The soft tissue healing and morphology were satisfactory, and additional mucogingival surgery was not required before definitive prosthetic rehabilitation.[13]
Comparison
Buser et al., in their review article, described the scientific documentation of one-stage, non-submerged dental implants. They demonstrated that non-submerged titanium implants achieve osseointegration as predictable as that of submerged titanium implants. All studies showed success rates well above 90%. The non-submerged approach is a true alternative to the original healing modality with submerged titanium implants. The non-submerged approach offers several clinical advantages:[14]
-
i)
The avoidance of second surgical procedure and less chair time per patient, resulting in less overall treatment cost.
-
ii)
The lack of microgap at the bone crest level, leading to less crestal bone during healing and resulting in a more favorable crown-to-implant length ratio.
-
iii)
A simplified prosthetic procedure, presenting an ideal basis for cemented implant restoration.
Chen concluded from his study that short-term survival rates of immediate and delayed implants appear to be similar. Furthermore, survival rates for immediate and delayed implants appear comparable to those of implants placed conventionally in healed alveolar ridges.[15]
As an alternative to immediate implant placement, delayed placement has several advantages. These include restoration of infection at the site and an increase in the area and volume of soft tissue for flap adaptation. However, these advantages are diminished by concomitant ridge resorption in the buccolingual direction. Thus, 4–8 weeks appears to be the optimal period to defer implant placement to allow adequate soft tissue healing to take place without under loss of bone volume.
Peri-implant defects associated with immediate and delayed implants have a high potential for bone regeneration. At sites with horizontal defects of 2 mm or less, spontaneous bone regeneration and osseointegration may be expected when implants with a rough surface are used. At sites with horizontal defects greater than 2 mm, or when one or more walls of the socket are missing, concomitant augmentation procedures with combination of barrier membranes and bone grafts are required.
Implants placed immediately after tooth extraction offer several advantages, but many authors have reported problems in filling the residual gap between the implant and the socket walls. Barrier and grafting techniques have been tested and found to yield varying results, so it has been suggested that the timing of implant placement may be important for success. Covani et al. analyzed bone healing and coronal bone remodeling around 35 implants, 20 placed immediately after tooth removal and 15 placed 6–8 weeks after extraction. All the implants were submerged and placed within the alveoli confines, leaving circumferential defects because the implants did not contact the bone at their coronal aspects; stabilization was achieved in the bone apically.[16]
Clinical and radiographic evaluation
Lindebroom et al. concluded from their study that immediate implant placement in chronic periapical lesions may be indicated.[17]
Cecchinato et al. concluded from their study that peri-implant bone-level change during function seemed to be unrelated to whether initial soft and hard tissue healing following implant installation had occurred under submerged or non-submerged conditions.[18]
Management of peri-implantitis
Schous et al. suggest numerous implant surface decontamination methods as part of the surgical treatment of peri-implantitis. Decontamination of affected implants with titanium plasma-sprayed or sandblasted, acid-etched surfaces may most easily and effectively be achieved by applying gauze soaked alternately in chlorhexidine and saline.[19]
MATERIALS AND METHODS
The present study was conducted in the Department of Oral and Maxillofacial Surgery, U. P. King George's University of Dental Sciences, Lucknow. The study comprised eight patients (six males and two females), in whom at 12 sites the implants were placed and the age of the patients ranged from 14 to 58 years. The inclusion criteria for implantation were tooth/teeth with one or two degree mobility, root stumps, tooth with failure root canal treatment and extraction sockets.
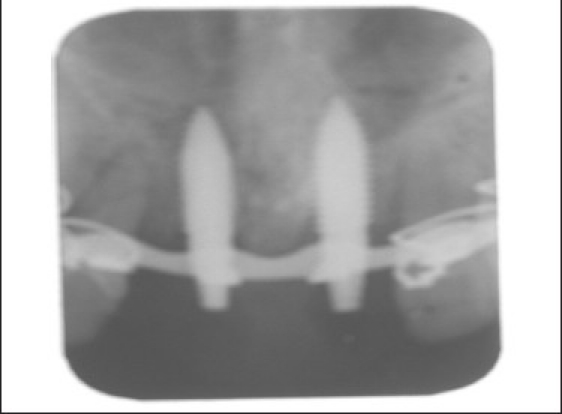
The vertical bone dimension was determined by palpation and radiograph (intraoral periapical, orthopantomograph and dentascan in some patients) [Figures 1 and 2]. Gingival condition and bone condition were examined clinically and radiographically. Exclusion criteria were patients with uncontrolled diabetes, radiation therapy in orofacial region, smoking, alcohol abuse, acute illness, pregnancy, and sockets after traumatic extraction, old patients, patients having unrealistic expectations and psychological problems.
Figure 1.

Preoperative IOPA radiograph
Figure 2.

Preoperative orthopantomograph
HI-TEC TRX-OP
(Life Care Company, Mumbai, India) with abutment, non-submerged, tapered at apical 5 mm, sandblasted and acid etched surfaced implants were used. These are one-stage single implants made of commercially pure titanium. The length of implant was 10 and 13 mm and diameter was 3.70 and 4.50 mm.
Surgical procedure
The surgical procedure was performed under local anesthesia and under premedication. The patients were divided into two groups:
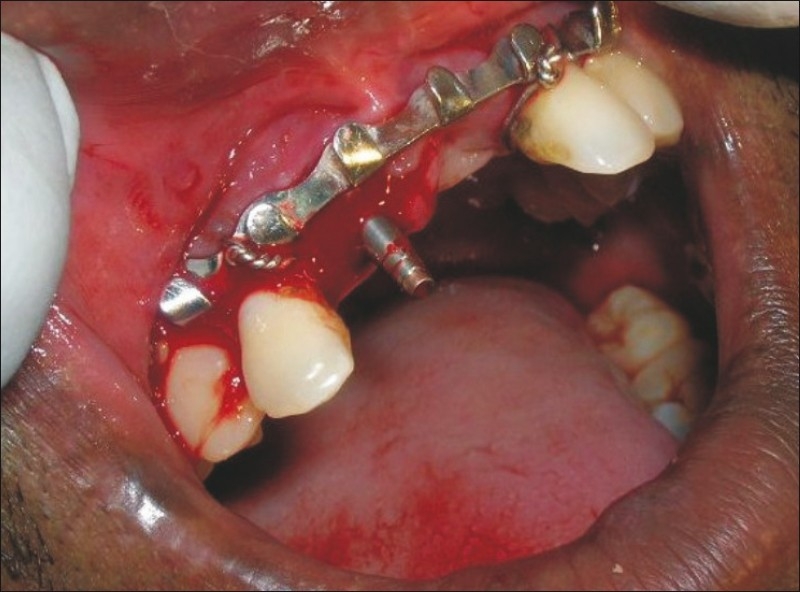
In Group A (five samples), the implant was placed immediately after non-traumatic extraction of tooth/root [Figures 3–10].
Figure 3.

Preoperative intraoral view
Figure 10.
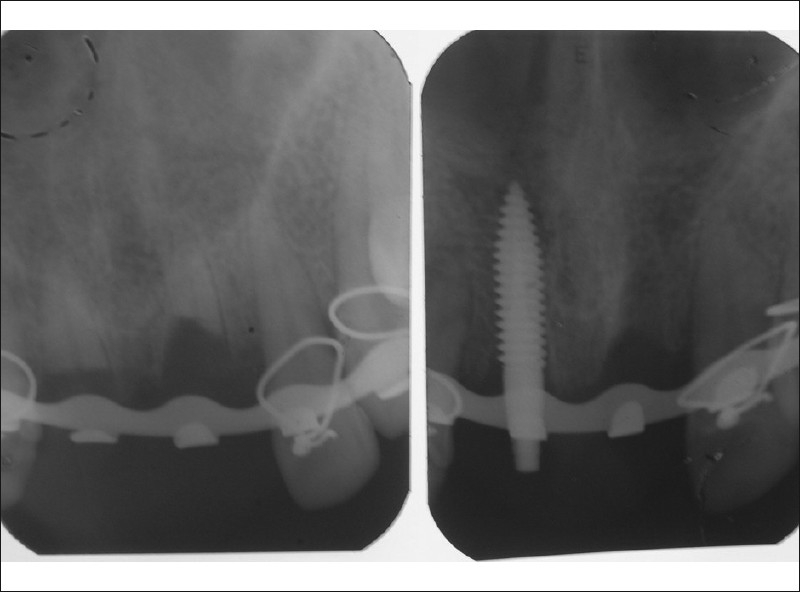
Postoperative radiograph after 4 weeks
Figure 4.
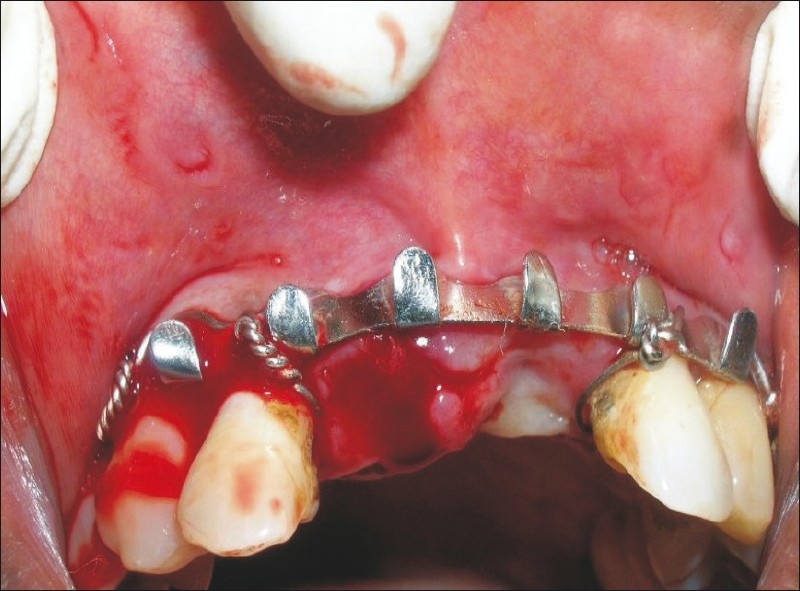
Intraoral view after extraction of root
Figure 5.
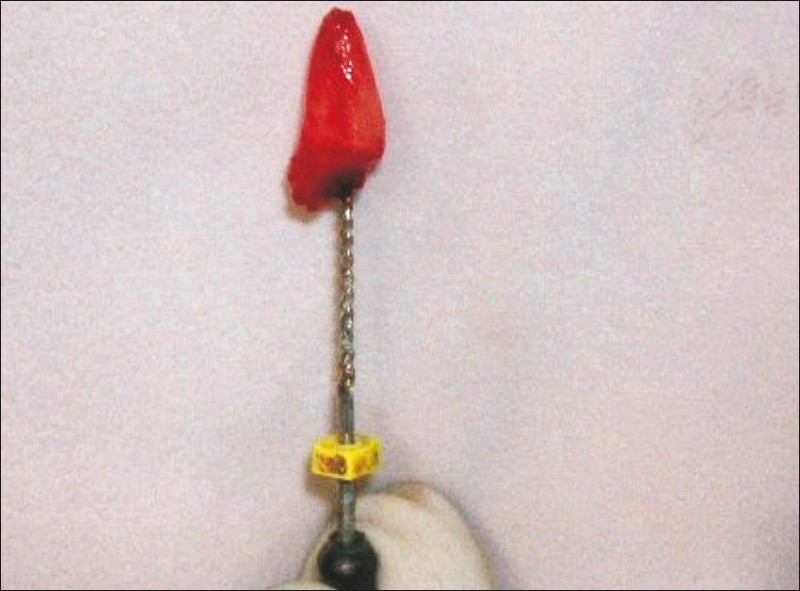
Root after extraction
Figure 6.

Implant with carrier
Figure 7.

Implant within the extraction socket
Figure 8.
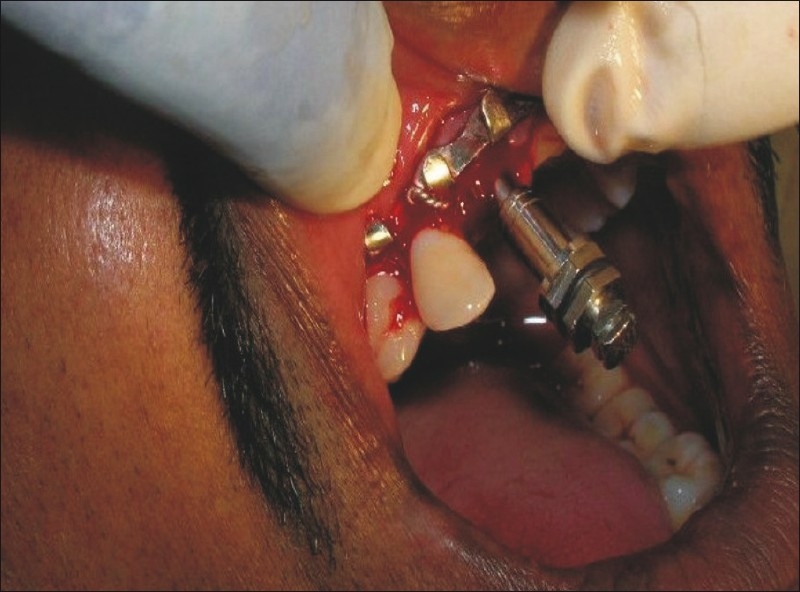
Implant with fixture insertion tool
Figure 9.
Immediate implant in its final position
In Group B (seven samples) the implants were placed 2-4 weeks after the extraction of tooth/root [Figures 11–16].
Figure 11.

Intraoral view of the implant
Figure 16.
Dentascan of delayed implant
Figure 12a.
Delayed implant in socket
Figure 12b.

Delayed implant in socket
Figure 13.

Postoperative radiograph after 12 weeks
Figure 14.

Implant with prosthesis
Figure 15.
Dentascan of immediate implant
In Group A, access was gained through extraction socket, and in Group B, access was gained by crestal incision followed by flap elevation. After implant placement, the mucosa was adapted to the abutment and sutured with 3-0 black silk suture.
Patients were then advised to follow standard postoperative instructions and asked to do thorough rinsing with antiseptic mouth washes, i.e. chlorhexidine gluconate (0.12%). They was called for the postoperative checkup after 24 h. The sutures were removed 7 days after the surgery. The patients were then followed up postoperatively at 1st day, 1st week, 4th week and up to 12th week, and from thereon any other required investigation was done whenever needed.
Postoperative assessment of the patients was done for the following parameters:
Postoperative clinical evaluation
Pain [visual analogue scale (VAS)], swelling, stability (by Glickman method), gingival status, probing depth (by William's periodontal probe), patient's compliance/satisfaction, complications (if any).
Radiological assessment
Intraoral periapical radiograph (IOPA) at regular intervals to assess bone implant relation; dentascan preoperatively and at the completion of the study to assess the availability and status of bone; assessment of alveolar bone (in mm).
RESULTS
The present study was done to evaluate the placement of implant into freshly extracted tooth socket (Group A) and in the post-extraction tooth socket after 2–4 weeks (Group B). Twelve implants were placed, five in Group A and seven in Group B. In Group A, the five implants were placed in maxilla; in Group B, six implants were placed in maxilla and one implant was placed in mandible. Observations were made postoperatively on 1st day, 1st week, 4th week, and 12th week for pain, swelling, stability, gingival status, mean probing depth, peri-implant radiolucency and marginal bone loss.
Pain
Statistically, pain reduction was significantly higher in Group B than in Group A at 1st week and there was no significant difference in pain at 4th week and 12th week.
Swelling
Swelling was absent in 100% of Group A patients, while in Group B, there was presence of swelling in 2 (28.6%) patients on 1st day. Statistically, the incidence of swelling was higher in Group B.
Implant stability
There was no difference in implant stability in both the groups at 1st day and 1st week. But there was less stability in Group B patients (71% at 4th week and 71% at 12th week) than the patients in Group A at the same time period.
Gingival status
Statistically, there was no significant difference in gingival status in Groups A and B at 1st week, 4th week and 12th week.
Mean probing depth
Statistically, there was no significant difference in mean probing depth of Group A and Group B patients.
Peri-implant radiolucency in groups
There was higher incidence of peri-implant radiolucency in Group B than in Group-A at different time intervals.
Marginal bone loss
Statistically, bone loss was higher in Group B patients than in Group A patients at 4th week and 12th week, which was not significant.
DISCUSSION
Pain
The mean pain scores in Group A at 1st day, 1st week, 4th week and 12th week were 6.40, 3.20, 0.8 and 0, respectively, showing significant reduction with time. The mean pain scores in Group B at 1st day, 1st week, 4th week and 12th week were 6.142, 1.4289, 0 and 0, respectively, also showing significant reduction with time. Pain on the 1st day was higher than during any other time period because of drilling of bone and the pressure effect of implant insertion. On comparing these two groups, the mean pain was significantly higher in Group B than in Group A at 1st week. At 4th week and 12th week, there was no significant difference in pain reduction. Various studies have shown that pain after implantation subsides as the healing occurs with the passage of time; similar results were also found in this study and the pain completely subsided with time.
Swelling
In the present study, there was no swelling in Group A at different time intervals. In Group B, there was swelling in 2 (28.6%) patients on the 1st day and later on there was no swelling at any time interval. On comparing Group A and Group B patients, swelling was slightly higher in Group B patients. The results of this study corroborated with the results reported by Babbush et al.
Implant stability
This study shows no mobility occurred in Group A patients at any time interval, and in Group B, mobility was present in 29% patients at 4th week and 12th week. According to the findings of Becker et al., implants placed at the time of extraction and inserted into native bone and not directly into the extraction socket have a higher degree of initial stability as evidenced by resonance frequency analysis (RFA).[20] While as found by Smith, that individual unattached implant should be immobile when tested clinically.[21]
Gingival status
In the present study there, was mild inflammation in both the groups on the 1st day because of surgical trauma. Later on, there was no swelling at any time interval. The gingival status remained normal at 1st week, 4th week and 12th week. Same observation was also reported by Covani that the soft tissue healing and morphology were satisfactory.[13]
Mean probing depth
The mean probing depth was evaluated using Williams's periodontal probe at 4th week and 12th week. In Group A, the mean probing depth at 4th week was 2.88 mm, and at 12th week, it was 2.54 mm, which shows reduction in mean probing depth with time. In Group B, the mean probing depth at 4th week was 2.5571 mm, and at 12th week, it was 2.4429 mm, which also shows reduction in mean probing depth with time. On comparing both the groups, there was no significant difference in mean probing depth. According to the findings of Ricci, the mean probing depth was >5 mm in 4.5% of cases and the survival rate of implants was 100%.[22]
Peri-implant radiolucency
In the present study, there was no evidence of peri-implant radiolucency in Group A patients at any time interval, while in Group B patients, there was evidence of peri-implant radiolucency in 29% of patients at 1st week and in 57% of patients at 4th and 12th weeks, which is contradicted by the findings of Smith who proposed that there should be no peri-implant radiolucency on undistorted radiograph for the success of an implant.[21]
Marginal bone loss
The present study shows no bone loss in Group A patients at any time interval, while the mean bone loss in group B patients at 4th week was 0.50 mm, and at 12th week, it was 1.2857 mm, while as reported by Smith, Albrektsson the vertical bone loss less than 0.2 mm annually after 1 year of service.[21]
In the present study, bone loss was higher in Group B than in Group A at 4th and 12th weeks.
According to Ogiso et al., the delay method of implantation shows earlier and wide bone formation and less surrounding fibrous encapsulation. Their results indicate that the delay technique can be an efficient method for establishing good bone binding,[23] while Schropp reported that new bone formation occurs in infrabony defects associated with immediately placed implants in extraction sockets.[6] Chen observed that comparison between immediate and delayed implantation sites showed a trend toward higher percentage of defect height and defect area at delayed sites (ranges between studies for defect height, 86% and 97%; for defect area, 86% and 97%) compared with immediate sites (defect height 77–95%; defect area 77–95%).[15] Weber estimated bone loss of about 0.6 mm around mandibular implants and 1.1 mm around maxillary implants in the 1st year after implant placement.
Dentascan was also done in few cases for preoperative planning and postoperative assessment. It has been observed that dentascan provides an outstanding view of jaws with or without implant but due to cost factor it was not carried out in all patients. However, it has a better edge enhancement for the assessment of marginal bone loss and peri-implant radiolucency.
Implant loading was done after 3 months in all the cases except two cases in the delayed group and it was observed that there was no change in stability, peri-implant radiolucency and marginal bone loss of the implant. On the day of loading, there was slight discomfort in the gingival tissue which subsided after 3 days.
CONCLUSION
Based on the observations made, statistically analyzed and duly discussed, the following conclusions were drawn from the present study.
Stability
In Group A (immediate implantation) patients, the stability was present in 100% cases, while it was present in 71% cases of Group B (delayed implantation).
Gingival status
Both the groups were having mild inflammation on the 1st day; later on, there was no inflammation at any time interval in both the groups.
Mean probing depth
On comparing both the groups, there was no significant difference in mean probing depth.
Peri-implant radiolucency
In Group B patients, there was evidence of peri-implant radiolucency, while Group A patients did not shows any peri-implant radiolucency.
Marginal bone loss
There was no bone loss in Group A patients at any time interval, while it was present in Group B patients.
Overall conclusion that can be drawn from this study is that both the groups showed more or less similar results, but Group A was slightly better than Group B. Due to small sample size and short duration of the study, long-term survival rate cannot be determined, for which a long-term study and bigger sample size are warranted.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wilson TG, Weber HP. Classification of and therapy for areas of deficient bony housing prior to dental implant placement. Int J Periodontics Restorative Dent. 1993;13:451–9. [Google Scholar]
- 2.Gomez-Roman G, Schulte W, d’Hoedt B, Axman-Krcmar D. The Frialit-2 implant system: Five-year clinical experience in single-tooth and immediately post extraction applications. Int J Oral Maxillofacial Implants. 1997;123:299–309. [PubMed] [Google Scholar]
- 3.Zitzmann NU, Naef R, Scharer P. Resorbable versus nonresorbable membranes in combination with Bio-oss for guided bone regeneration. Int J Oral Maxillofacial Implants. 1997;12:844–52. [PubMed] [Google Scholar]
- 4.Mayfield LJ. Immediate, delayed and late submerged and transmucosal implants. In: Lindhe J, editor. Proceedings of the 3rd European Workshop on Periodontology: Implant Dentistry. Berlin: Quintessenz; 1999. pp. 520–34. [Google Scholar]
- 5.Hammerle CH, Lang NP. Single-stage surgery combining transmucosal implant placement with guided bone regeneration and bioresorbable materials. Clin Oral Implants Res. 2001;12:9–18. doi: 10.1034/j.1600-0501.2001.012001009.x. [DOI] [PubMed] [Google Scholar]
- 6.Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: A prospective clinical study. Int J Oral Maxillofacial Implants. 2003;182:189–99. [PubMed] [Google Scholar]
- 7.Yukna RA. Clinical comparison of hydroxyapatite-coated titanium dental implants placed in fresh extraction sockets and healed sites. J Periodontal. 1991;62:468–72. doi: 10.1902/jop.1991.62.7.468. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz-Arad D, Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: A literature review. J Periodontol. 1997;68:915–23. doi: 10.1902/jop.1997.68.10.915. [DOI] [PubMed] [Google Scholar]
- 9.Parel SM, Schow SR. Early clinical experience with a new one-piece implant system in single tooth sites. J Oral Maxillofacial Surg. 2005;63(9 Suppl 2):2–10. doi: 10.1016/j.joms.2005.05.150. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz-Arad D, Chaushu G, Grossman Y. The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J Periodontol. 2000;71:839–44. doi: 10.1902/jop.2000.71.5.839. [DOI] [PubMed] [Google Scholar]
- 11.Heydenrijk K, Raghoebar GM, Batenburg RH, Stegenga B. A comparison of labial and crestal incisions for the 1-stage placement of IMZ implants: A pilot study. J Oral Maxillofacial surg. 2000;58:1119–23. doi: 10.1053/joms.2000.9570. [DOI] [PubMed] [Google Scholar]
- 12.Vergara JA, Caffesse RG. Immediate replacement of single upper posterior teeth: A report of cases. Clin Implant Dent Relat Res. 2003;5:130–6. doi: 10.1111/j.1708-8208.2003.tb00194.x. [DOI] [PubMed] [Google Scholar]
- 13.Covani U. Soft tissue healing around implants placed immediately after tooth extraction without incision: A clinical report. Int J Oral Maxillofacial Implants. 2004;19:549–53. [PubMed] [Google Scholar]
- 14.Buser D, Mericske-Stern R, Dula K, Lang NP. Clinical experience with one-stage, non-submerged dental implants. Adv Dent Res. 1999;13:153–61. doi: 10.1177/08959374990130010501. [DOI] [PubMed] [Google Scholar]
- 15.Chen ST, Wilson TG, Jr, Hämmerle CH. Immediate or early placement of implants following tooth extraction: Review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofacial Implants. 2004;19(Suppl):12–25. [PubMed] [Google Scholar]
- 16.Covani U, Bortolaia C, Barone A, Sbordone L. Bucco-lingual crestal bone changes after immediate and delayed placement. J Periodontol. 2004;75:1605–12. doi: 10.1902/jop.2004.75.12.1605. [DOI] [PubMed] [Google Scholar]
- 17.Lindeboom JA, Tjiook Y, Kroon FH. Immediate placement of implants in periapical infected sites: A prospective randomized study in 50 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:705–10. doi: 10.1016/j.tripleo.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 18.Cecchinato D, Olsson C, Lindhe J. Submerged or non-submerged healing of endosseous implants to be used in the rehabilitation of partially dentate patients. J Clin Periodontol. 2004;31:299–308. doi: 10.1111/j.1600-051X.2004.00527.x. [DOI] [PubMed] [Google Scholar]
- 19.Schou S, Berglundh T, Lang NP. Surgical treatment of peri-implantitis. Int J Oral Maxillofacial Surg. 2004;19:140–9. [PubMed] [Google Scholar]
- 20.Becker W, Sennerby L, Bedrossian E, Becker BE, Lucchini JP. Implant stability measurements for implants placed at the time of extraction: A cohort, prospective clinical trial. J Periodontol. 2005;76:391–7. doi: 10.1902/jop.2005.76.3.391. [DOI] [PubMed] [Google Scholar]
- 21.Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567–72. doi: 10.1016/0022-3913(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 22.Ricci G, Aimetti M, Stablum W, Guasti A. Crestal bone resorption 5 year after loading: Clinical and radiologic results with a 2-stage implant system. Int J Oral Maxillofacial Implants. 2004;19:597–602. [PubMed] [Google Scholar]
- 23.Ogismo M, Tabata T, Lee RR, Borgese D. Delay method of implantation enhances implant-bone binding: A comparison with the conventional method. Int J Oral Maxillofacial Implants. 1995;10:415–20. [PubMed] [Google Scholar]


