Abstract
Background
Tobacco smoking remains the leading preventable cause of death among American women. Aerobic exercise has shown promise as an aid to smoking cessation because it improves affect and reduces nicotine withdrawal symptoms. Studies outside the realm of smoking cessation have shown that yoga practice also reduces perceived stress and negative affect.
Methods
This pilot study examines the feasibility and initial efficacy of yoga as a complementary therapy for smoking cessation. Fifty-five women were given 8-week group-based cognitive behavioral therapy for smoking cessation and were randomized to a twice-weekly program of Vinyasa yoga or a general health and wellness program (contact control). The primary outcome measure was 7-day point prevalence abstinence at the end of treatment validated by saliva cotinine testing. Longitudinal analyses were also conducted to examine the effect of intervention on smoking cessation at 3- and 6-month follow-up. We examined the effects of the intervention on potential mediating variables (e.g., confidence in quitting smoking, self-efficacy), as well as measures of depressive symptoms, anxiety, and perceived health (SF-36).
Results
At end of treatment, women in the yoga group had a greater 7-day point-prevalence abstinence rate than controls (odds ratio [OR], 4.56; 95% CI, 1.1–18.6). Abstinence remained higher among yoga participants through the six month assessment (OR, 1.54; 95% CI, 0.34–6.92), although differences were no longer statistically significant. Women participating in the yoga program also showed reduced anxiety and improvements in perceived health and well-being when compared with controls.
Conclusions
Yoga may be an efficacious complementary therapy for smoking cessation among women.
Introduction
The health risks of tobacco smoking are well established. Heart disease, the number one killer among women in the United States, and lung cancer, the leading cause of cancer death among women, are both linked to smoking.1 Approximately 21% of U.S. adults are current smokers,2 nearly the same as in 2004.3 This suggests that previously observed declines in smoking may have stalled. While approximately 70% of smokers report wanting to quit, only about 40% attempt to quit each year,3 and overall success rates remain low.4 Although smoking prevalence is somewhat higher among men (22.3%) than women (17.4%),3 it has been suggested that quitting smoking may be more difficult for women because women show lower cessation rates and higher relapse rates compared with men.5–8
Several efficacious medications are available to assist smokers in their efforts to quit.9 Using these medications approximately doubles the likelihood of successful quitting.10 However, 50%–80% of smokers who attempt to quit will elect not to use medications,11–14 and efforts to encourage medication use during quit attempts have met with mixed success.15–18 Smokers may avoid medication use because of legitimate concerns about adverse side effects, contraindications based on their personal health history, costs of pharmacotherapy, and the perceived desirability of a chemical-free quit experience.19–23 Thus, alternative smoking cessation programs are needed to assist women who cannot quit with self-help or with pharmacologic approaches.24
Exercise was initially proposed as a therapy for smoking cessation among women because it may help offset weight gain and concerns regarding weight gain, both of which are important barriers to cessation among women.25–30
Previous studies by our research group and others have not consistently shown an exercise-mediated effect on weight gain or weight concerns but have instead more generally demonstrated that traditional aerobic exercise programs (i.e., brisk walking, bicycling) incorporated into smoking cessation treatment result in higher quit rates compared with smoking treatments without exercise.29,31–35 The lack of consistent evidence that exercise ameliorates increases in weight in women who quit smoking suggests that other important mechanisms by which exercise may increase rates of smoking cessation. Indeed, exercise has been shown to improve affect among nonsmoking adults and women who are attempting to quit smoking.36–43 Exercise may enhance cessation efforts by alleviating the rise in negative affect that often accompanies quit attempts44–47 and increases the risk of relapse.46,48–49
Yoga is an alternative to traditional (Western) aerobic exercise that may have promise as a complementary treatment for smoking cessation. Yoga contains a number of components that contribute to stress reduction including asanas, yoga postures that have been shown to improve mood and well-being similar to the effects of traditional Western exercise,37,39,41,42 and pranayama, breathing exercises that involve regulation of breath and conscious deep breathing that stimulates pulmonary stretch receptors similar to the deep inhalations associated with smoking.50 Together, these components of yoga work to still the mind and focus the attention of the practitioner, regulating the agitated onrush of thoughts and anxieties and producing physiological and cognitive relaxation. While yoga is associated with health benefits similar to exercise, the goal of yoga practice is also to create a calm state of mind through the combination of physical postures, breathing techniques, and directed meditative focus.51,52 Several studies have shown that the practice of yoga reduces perceived stress and negative affect.53–56 Thus, the practice of yoga may also improve the chances of successful smoking cessation.
The present study investigates the feasibility and preliminary efficacy of an 8-week yoga program on perceived stress, affect, transtheoretical constructs, and smoking cessation among healthy, adult women smokers.
Methods
Design
We conducted a randomized, controlled pilot study comparing two conditions: (1) group-based cognitive–behavioral therapy (CBT) for smoking cessation plus a twice-weekly group-based yoga program (yoga); and (2) CBT for smoking cessation plus a group-based wellness program that served as a contact-control (wellness). Groups of 8–10 individuals were enrolled and randomized into either the yoga or wellness conditions in the 8-week treatment program in parallel sequential cohorts. Study measures were administered at study enrollment (baseline), posttreatment (week 8), and 3- and 6-month follow-up.
Participant recruitment
Women were recruited through advertisements in local newspapers and websites and on television and through flyers posted at physician's offices and commercial locations (e.g., convenience stores, grocery stores). The study research assistant was trained to provide information about the program to individuals who called the program in response to the advertisements and to screen interested persons for eligibility. Callers were excluded if they smoked fewer than five cigarettes per day; were already physically active (>3 days of moderate-intensity physical activity or >2 days of vigorous intensity physical activity per week); were currently practicing yoga; had a current diagnosis of heart disease, lung disease, or orthopedic conditions that could make participation in yoga difficult or dangerous; or were currently in treatment for psychiatric illness or were using illegal substances. Individuals were also screened to ensure safe participation in physical activity using the PAR-Q.57 A letter was also mailed to them requesting they obtain physician consent to participate in the program. Eligible individuals also attended an orientation session at which the research assistant explained the study, reviewed participation requirements, and administered informed consent. All recruitment procedures and materials including advertisements, consent forms, and procedures were approved by the institutional human subjects review board.
Procedures
Participants were individually randomized to either yoga or wellness conditions within parallel sequential cohorts. The differential numbers between the two conditions reflect the replacement of yoga and wellness participants who dropped at different stages of the study after informed consent was obtained. All participants were given a weekly 1-hour group-based CBT for smoking cessation session; separate groups were held in different locations for yoga and wellness participants to control for cross-treatment contamination. One yoga and one wellness session was scheduled each week on the same night as the respective CBT smoking treatment group to minimize participant travel to the program to only two evenings a week.
Yoga classes were conducted twice weekly for 8 weeks by certified yoga instructors with over 15 years experience and who were trained in the Vinyasa style. Vinyasa is a form of Hatha yoga that emphasizes the continuous flow of movement between postures (asanas) and links breath with the movements. In collaboration with the researchers, yoga instructors selected a pattern of asanas that was appropriate for beginners and taught them consistently during each class. Each class consisted of 5 minutes of breathing exercises (pranayamas) and seated meditation, followed by 45 minutes of dynamically linked asanas. Classes concluded with 10 minutes of closing postures (similar to the “cooling down” period following aerobic exercise) and a final seated meditation.
Participants attending the wellness sessions were shown videos on a variety of health topics (e.g., low fat diets, breast cancer screenings, and back health). A discussion guided by a Ph.D. psychologist and distribution of written materials relevant to the video topic followed the video segment of each wellness session.
The CBT smoking cessation program was lead by a psychologist with over 10 years experience in conducting smoking cessation groups. A program manual developed from our previous studies using CBT for smoking cessation58,59 was used to administer treatment to ensure consistent delivery of program content. Topics included self-monitoring, stimulus control, coping with high-risk situations, and stress management for smoking cessation. The program also focused on topics of concern to women when quitting, including healthy eating, weight management, and balancing multiple roles and multiple demands. This program had been used successfully in our previous studies.29,31,58,59 Participants were also encouraged to select healthy, low-calorie snacks throughout the program and were provided with examples of these snacks to sample. Participants were not provided with nicotine replacement therapy or other smoking cessation medications but were allowed to use them in conjunction with the program if advised to do so by primary care physician. The second week of the program was targeted as quit day.
Measures
Assessments included surveys of demographic variables, smoking history and nicotine dependence (FTND).60,61 We also administered measures of anxiety (STAIT),62 depressive symptoms (CESD-10),63 and overall well being (Short-form Health Survey: SF-36).64 We assessed cognitive variables found to predict smoking abstinence in previous research, including temptations to smoke (smoking situations temptations scale,65 stage of change for smoking cessation,66 severity of nicotine withdrawal symptoms during previous quit attempts67). Confidence in achieving abstinence was assessed using a single item answered on a 7-point Likert scale. Finally, participants also answered questions about the degree to which they were concerned about post-cessation weight gain (smoking and weight control),68 including one item that asked whether they intentionally smoked to control their weight (yes/no).
Weekly, throughout the 8-week program, self-report of >24-hour abstinence was confirmed by breath carbon monoxide. The primary smoking outcome variable was 7-day point prevalence abstinence (7PPA), verified by saliva cotinine level less than 57 nmol/L (15 ng/mL) at the end of treatment (week 8) and all follow-up assessments.
Participants completed the full assessment packet at program entry (baseline), end of treatment (week 8), and at 3- and 6-month follow-ups. Participants also completed weekly assessments of affect (PANAS)69 immediately before and again after one yoga or wellness session weekly. Assessments of current nicotine withdrawal symptoms67 were also completed weekly.
Analyses
Baseline demographic, smoking and other measured variables were examined for group differences using chi-square tests or analysis of variance (ANOVA) depending on the variable characteristics. Descriptive, correlational, logistic regression and analysis of covariance (ANCOVA) analyses were conducted using PASW Statistics 18, Release 18.0.0 (SPSS, Inc.).
Primary analyses
We conducted intention-to-treat analyses (in which all those missing at follow-up are assumed to be smoking) using logistic regression and longitudinal generalized estimating equations (GEE) analysis to examine abstinence outcomes. Pearson r correlations were conducted to analyze the association between baseline smoking characteristics (nicotine dependence, smoking rate, and severity of withdrawal symptoms during previous quit attempts) and anxiety (STAIT), depression (CESD), and self-perception (PSPP) at baseline. We examined short-term abstinence (>24 hour) and 7-day abstinence during active treatment (weeks 1–8). Cotinine-validated 7PPA70 was examined across treatment group and time (week 8, 3- and 6-month follow-ups) using the ITT principle within GEE approach of Zeger and Liang71 as implemented in SAS 9.1.3 (SAS Institute). The model was fit with an autoregressive working correlation structure.
Secondary analyses
ANCOVAs were used to examine the effects of treatment on the change score from baseline to end of treatment (week 8) using baseline values of each variable as covariates. ANCOVAs were also conducted by using baseline values of each variable as covariates to examine differences based on 7-day smoking cessation status on the change score from baseline to end of treatment on the same set of variables.
Results
Baseline demographic characteristics
One hundred eighty-four individuals called in response to our advertisements and were screened for eligibility by the study research assistant. The most common reasons for study ineligibility were medical conditions limiting exercise participation (58%), current major depression (47%), scheduling conflicts (18%), and smoking fewer than five cigarettes per day (15%). Fifty-five women were randomized to treatment conditions (n=32 yoga; n=23 wellness). Descriptive characteristics overall and by treatment condition are listed in Table 1. In brief, participants' average age was 45.6 years (±8.3), 35% had completed college, median household income was $30,000–$45,000/year, and 18% of participants were ethnic or racial minorities. No significant cohort effects were found with respect to smoking outcome and all further analyses were performed with participants pooled into their respective treatment groups. There were also no significant baseline differences between participants randomized to the yoga versus wellness treatments in terms of demographic, smoking history, or other study measures (presented in Table 1).
Table 1.
Participant Characteristics Overall and by Condition at Baseline Assessment
| Yoga (n=32) | Wellness (n=23) | All (N=55) | Statistic | p value | |
|---|---|---|---|---|---|
| Age, mean (SD) | 43.8 (9.4) | 48.1 (5.9) | 45.6 (8.3) | F1,53=3.83 | 0.06 |
| Education, % | χ2(4)=4.66 | 0.32 | |||
| Less than high school | 13 | 13 | 13 | ||
| High school | 25 | 17 | 22 | ||
| Some college | 31 | 30 | 31 | ||
| College grad | 31 | 39 | 35 | ||
| White, % | 88 | 74 | 82 | χ2(1)=1.66 | 0.20 |
| Married or live with significant other, % | 50 | 39 | 45 | χ2(1)=0.64 | 0.43 |
| Employed, % | 59 | 48 | 55 | χ2(1)=0.72 | 0.40 |
| Cigarettes per day, mean (SD) | 16.5 (8.1) | 15.3 (6.1) | 16 (7.3) | F1,53=0.40 | 0.53 |
| Fagerstrom tolerance questionnaire (nicotine dependence), mean (SD) | 5.1 (1.4) | 4.9 (1.5) | 5.0 (1.4) | F1,53=0.33 | 0.57 |
| Stage of change for smoking cessation, % | χ2(1)=0.02 | 0.90 | |||
| Contemplation | 62.5 | 60.9 | 61.8 | ||
| Preparation | 37.5 | 39.1 | 38.2 | ||
| Confidence in quitting, mean (SD) | 4.9 | 4.7 | 4.9 | F1,52=0.32 | 0.58 |
| Withdrawal symptoms, mean (SD) | 41.0 | 44.6 | 42.5 | F1,53=1.17 | 0.28 |
| Smoking weight control, mean (SD) | 2.2 (1.1) | 2.4 (1.2) | 2.2 (1.1) | F1,53=0.40 | 0.53 |
| I smoke to control my weight (yes) | 6 | 2 | 8 | χ2=1.08 | 0.26 |
| Smoking situations temptation scale, mean (SD) | |||||
| Habit | 9.2 (2.7) | 10.5 (3.3) | 9.7 (3.0) | F1,53=2.81 | 0.10 |
| Social | 10.4 (3.2) | 11.2 (2.0) | 10.7 (2.7) | F1,53=1.05 | 0.31 |
| Mood | 11.4 | 12.0 | 11.7 | F1,53=0.60 | 0.44 |
| Total | 31.0 | 33.7 | 32.1 | F1,53=2.42 | 0.13 |
| Smoking self-efficacy | 2.6 | 2.4 | 2.5 | F1,53=0.53 | 0.47 |
| Anxiety (STAIT) | 43.3 | 43.0 | 43.2 | F1,53=0.01 | 0.91 |
| CESD-10 (depression symptoms) | 10.6 | 8.9 | 9.9 | F1,53=1.33 | 0.25 |
| Overall wellbeing (SF-36) | 48.3 | 48.7 | 48.5 | F1,53=0.03 | 0.87 |
Program adherence
Individuals randomized to the yoga intervention attended an average of 76.2% of the yoga classes and 82.6% of the smoking cessation group sessions. Women in the wellness group attended 67.1% of the wellness sessions and 78.2% of the smoking cessation group sessions.
Smoking behaviors and readiness to quit
Baseline smoking patterns and history information are listed in Table 1. In brief, participants smoked an average of 16.0 (±7.3) cigarettes per day (range: 3–40) and reported an average of 4.5 (±10.3) previous quit attempts. Nearly half (41.8%) had quit for at least 24 hours in the past year. The average nicotine dependence score was 5.0 (±1.4). On the stage of change measure of readiness to quit smoking, 38% of participants were in the preparation stage (planning to quit in the next 30 days and had made at least one quit attempt in the past year) at study enrollment, and 62% were in the contemplation stage. Confidence in quitting smoking averaged 4.9 (±0.9) on a 7-point scale. During previous quit attempts, many participants reported experiencing moderate-to-severe withdrawal symptoms (mean=42.5, range 20–70). Fourteen percent of participants endorsed smoking for weight control.
During the program five participants used quit smoking medications (two yoga and two wellness participants used varenicline; one wellness participant used nicotine patch).
Smoking outcomes
At the end of treatment (week 8), participants in the yoga condition demonstrated increased odds of 24-hour smoking cessation compared with those in the wellness condition (46.9% vs. 17.4%; odds ratio [OR], 4.19; 95% confidence interval [CI], 1.2–15.1; p=0.029). Yoga participants were also more likely to have attained 7PPA at end of treatment compared with those in the wellness condition (40.6% vs. 13.0%; OR, 4.56; 95% CI, 1.1–18.6; p=0.034) as verified by saliva cotinine. Across the 3- and 6-month follow-up assessments, participants who had been randomized to the yoga condition continued to show greater rates of abstinence compared with those randomized to wellness, although these differences did not achieve statistical significance (Table 2). At 3 months, the odds ratio for abstinence between yoga and wellness arms was 2.94 (95% CI, 0.55–15.70). At 6 months, the odds ratio was reduced to 1.54 (95% CI, 0.34–6.92). There was no overall significant effect for treatment group (p=0.11), time (p=0.17), or the treatment group by time interaction (p=0.20) across the follow-up period (Table 2).
Table 2.
Smoking Outcomes by Treatment Group
| Yoga | Wellness | Odds ratio | Confidence interval | p value | |
|---|---|---|---|---|---|
| Summary 7-day quit using intention to treat (ITT) outcomes | |||||
| 8 weeks (N=55) | 40.6% (13/32) | 13.0% (3/23) | 4.56 | 1.12–18.57 | 0.03 |
| 3 months (N=55) | 21.9% (7/32) | 8.7% (2/23) | 2.94 | 0.55–15.70 | 0.21 |
| 6 months (N=55) | 18.8% (6/32) | 13.0% (3/23) | 1.54 | 0.34–6.92 | 0.57 |
| Summary 24-hour quit using intention to treat (ITT) outcomes | |||||
| 8 weeks (N=55) | 46.9% (15/32) | 17.4% (4/23) | 4.19 | 1.16–15.11 | 0.03 |
| 3 months (N=55) | 21.9% (7/32) | 8.7% (2/23) | 2.94 | 0.55–15.70 | 0.21 |
| 6 months (N=55) | 21.9% (7/32) | 13.0% (3/23) | 1.87 | 0.43–8.16 | 0.41 |
Outcomes: secondary analyses
Pairwise comparisons examining within-group changes between baseline and posttreatment in anxiety (STAIT), depression symptoms (CESD), overall wellbeing (SF-36), and temptations to smoke (SST) showed that yoga participants had significant reductions in anxiety (STAIT) and temptations to smoke (SST) and increases in overall well-being (SF-36), while wellness participants had improvements in temptations to smoke only (Table 3). We then conducted a series of ANCOVAs to examine changes in these variables using the baseline value of each dependent measure as a covariate. Yoga participants showed greater reductions in anxiety (STAIT; −9.6% vs. −0.7%), and greater increases in general health (SF-36; 8.1% vs. 1.7%) than wellness participants, although differences between groups were not statistically significant (Table 4).
Table 3.
Pairwise Comparisons to Examine for Change From Baseline to 8-Weeks Within the Yoga and Wellness Groups
| Variable | Group | Baseline (SD) | Posttreatment (SD) | p value |
|---|---|---|---|---|
| CESD-10 (Depression symptoms) | Yoga | 10.4 (5.9) | 9.3 (5.6) | 0.35 |
| Wellness | 8.8 (6.7) | 8.8 (7.7) | 0.99 | |
| STAIT (Anxiety) | Yoga | 43.6 (11.4) | 39.4 (10.4) | 0.00 |
| Wellness | 41.6 (12.0) | 41.3 (11.3) | 0.83 | |
| Well being (SF-36) | Yoga | 48.8 (6.0) | 52.8 (4.4) | 0.00 |
| Wellness | 52.1 (4.5) | 53.0 (5.2) | 0.66 | |
| SST (overall) | Yoga | 31.1 (6.6) | 27.4 (7.7) | 0.04 |
| Wellness | 32.5 (6.5) | 25.8 (9.2) | 0.01 | |
| SST_Habit subscale | Yoga | 9.2 (2.7) | 7.7 (2.9) | 0.05 |
| Wellness | 9.6 (3.4) | 7.4 (3.3) | 0.02 | |
| SST_Social subscale | Yoga | 10.5 (3.3) | 8.9 (3.0) | 0.05 |
| Wellness | 10.7 (2.0) | 8.4 (3.7) | 0.03 | |
| SST_Mood subscale | Yoga | 12.1 (2.4) | 10.0 (3.9) | 0.01 |
| Wellness | 11.5 (2.9) | 10.7 (3.4) | 0.22 |
Table 4.
Group Comparisons to Examine for Posttreatment Change Using Baseline Values as Covariates in Analysis of Covariance
| Variable | Group | Baseline (SD) | Posttreatment (SD) | % change | p value |
|---|---|---|---|---|---|
| CESD | Yoga | 10.4 (5.4) | 9.3 (5.6) | −10.5 | 0.86 |
| Wellness | 8.8 (6.7) | 8.8 (7.7) | 0 | ||
| STAIT | Yoga | 43.6 (11.4) | 39.4 (10.4) | −9.6 | 0.09 |
| Wellness | 41.6 (12.0) | 41.3 (11.3) | −0.07 | ||
| Wellbeing (SF-36) | Yoga | 48.8 (6.0) | 52.8 (4.4) | 8.1 | 0.60 |
| Wellness | 52.1 (4.5) | 53.0 (5.2) | 1.7 | ||
| SST | Yoga | 31.1 (6.6) | 27.4 (7.7) | −11.9 | 0.50 |
| Wellness | 32.5 (6.5) | 25.8 (9.2) | −20.6 | ||
| SST_Habit | Yoga | 9.2 (2.7) | 7.7 (2.9) | −16.3 | 0.63 |
| Wellness | 9.6 (3.4) | 7.4 (3.3) | −22.9 | ||
| SST_Social | Yoga | 10.5 (3.3) | 8.9 (3.0) | −15.9 | 0.63 |
| Wellness | 10.7 (2.0) | 8.4 (3.7) | −21.5 | ||
| SST_Mood | Yoga | 12.1 (2.4) | 10.0 (3.9) | −17.4 | 0.28 |
| Wellness | 11.5 (2.9) | 10.7 (3.4) | −7.0 |
Predictors of cessation
To examine changes in variables between baseline and end of treatment that predicted smoking abstinence at week 8, we conducted a second series of ANCOVAs, using the baseline value of each dependent measure as a covariate, examining for differences based on posttreatment smoking status (quit vs. smoking). These analyses revealed significant differences for temptations to smoke (SST; p<0.001) and depression symptoms (CESD; p=0.04). Anxiety and weight concerns at baseline were not predictive of smoking status at week 8 (Table 5).
Table 5.
Comparisons by End of Treatment (Week 8) 7-Day Point Prevalence Abstinence Status (Quit n=16; Smoking n=39) Using Baseline Values as Covariates
| Variable | Group | Baseline (SD) | Posttreatment (SD) | % change | Group difference (%) | p value |
|---|---|---|---|---|---|---|
| CESD-10 (depression symptoms) | Quit | 8.9 (7.3) | 6.2 (5.2) | −30 | −40.9 | 0.04 |
| Smoking | 10.3 (5.1) | 10.5 (6.5) | 1 | |||
| STAIT (anxiety) | Quit | 36.1 (9.9) | 32.9 (9.5) | 8.8 | −20.7 | 0.08 |
| Smoking | 46.1 (11.0) | 41.5 (9.5) | 9.9 | |||
| Well-being (SF-36) | Quit | 50.2 (6.1) | 54.0 (5.4) | 7.5 | 3.5 | 0.32 |
| Smoking | 49.4 (5.7) | 52.1 (3.9) | 5.4 | |||
| SST (overall) | Quit | 31.2 (7.8) | 20.5 (6.8) | −34.3 | −31.2 | 0.00 |
| Smoking | 31.8 (6.0) | 29.8 (7.2) | −6.2 | |||
| SST_Habit subscale | Quit | 9.4 (2.8) | 5.3 (2.6) | −43.6 | −39.1 | 0.00 |
| Smoking | 9.3 (3.1) | 8.7 (2.6) | −6.5 | |||
| SST_Social subscale | Quit | 11.0 (3.3) | 6.9 (2.2) | −37.3 | −28.1 | 0.01 |
| Smoking | 10.3 (2.7) | 9.6 (3.3) | −6.8 | |||
| SST_Mood subscale | Quit | 10.8 (3.7) | 8.3 (3.7) | −23.1 | −27.2 | 0.01 |
| Smoking | 12.1 (2.1) | 11.4 (3.1) | −5.8 |
Acute effects of yoga on affect
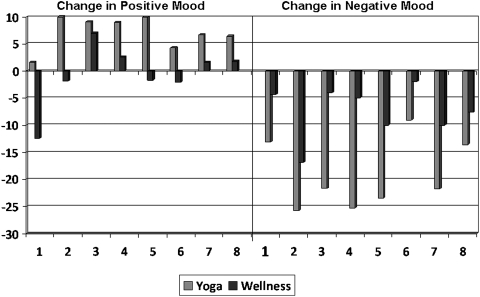
Analyses of acute changes in positive and negative affect (PANAS) following yoga or wellness sessions showed that across the 8 weeks of the program, yoga participants reported a three times greater reduction in negative affect compared with wellness participants (−19.1±7.6 vs. −7.4±3.7). Yoga participants also reported a larger increase in positive affect after yoga (+6.1±1.0) than wellness participants did following their wellness session (−0.8.1±9.5). Week-by-week changes in affect pre- to postsession are presented in Fig. 1.
FIG. 1.
Percent change in positive and negative moods across 8 weeks: yoga vs. wellness.
Discussion
This is the first study to examine the effect of yoga on smoking cessation. Our results provide preliminary evidence that yoga may be an effective adjunctive treatment for smoking cessation in women. Specifically, yoga appears to enhance the effects of CBT on short-term smoking cessation outcomes. While the sample size precluded formal mediation analysis, results of secondary analyses suggest that the positive effects of yoga on smoking outcomes may occur via reduction of negative symptoms associated with quitting smoking, decreasing stress and cigarette cravings, and improving mood and perception of quality of life.
Numerous studies have shown that stress is a strong predictor of both inability to quit smoking and smoking relapse.72–74 Other research has shown significant reduction in stress and negative mood following even a few weeks of yoga practice.75–77
In addition to making quitting smoking uncomfortable and difficult, perceived stress, negative affect, and withdrawal symptoms themselves have all been shown to increase an individual's risk for relapse to smoking. Relapse within the first week of quitting is preceded by a marked increase in withdrawal symptoms, including craving for cigarettes, distress, and reductions in positive affect.49 Perceived stress and negative activated affect have also been shown to predict time to relapse among recent exsmokers.46,48,78 Thus, providing smokers with methods of coping with stress, such as a yoga program, may improve their ability to quit and remain exsmokers.
These findings are important because they suggest that yoga is a viable treatment adjunct for women who would like to quit smoking without the use of medications. Since this study did not include the use of medications, the relative effect of yoga versus medications on nicotine withdrawal and cigarette craving is not established. Additional work would be needed not only to compare those effects but also to determine whether the effect of yoga and medications might be redundant or have an additive or synergistic effect when used together.
Vinyasa yoga, which incorporates features of breathing exercises (pranayama) and meditative components in addition to moderate-to-vigorous intensity exercise, may be especially appealing relative to traditional aerobic exercise. For example, in addition to producing improvements in cardiopulmonary functioning, the practice of yoga has been linked to improvements in affect, reductions in stress and anxiety, increases in self-efficacy, and improvements in overall well-being.53–56 These benefits may result from the unique aspects of yoga, including meditative approaches to focus attention and deliberate regulation of breathing during pranayama exercises. Finally, yoga is intended to be a lifelong practice often sustained for years once begun by practitioners thereby having the potential to continue to reinforce quitting smoking once formal smoking treatment ends.
This pilot study had a number of strengths. First, in terms of study design, we used random assignment to study conditions, a contact control comparison condition, objective indicators of smoking cessation, and an ITT approach to analysis. Second, participants demonstrated good treatment adherence and retention rates, with no differential adherence to treatment or withdrawal from the study. Third, abstinence rates at follow-up were strong compared with previous smoking cessation studies of this kind, although these outcomes must be considered preliminary given the small sample size used in this pilot. Fourth, the observed differences between yoga and control conditions on variables hypothesized as mechanisms of action suggest that the treatment operated through the intended mechanisms and was not due to nonspecific effects. Fifth, our sample was representative for our recruitment area and was similar in age, demographic characteristics, and smoking behaviors to samples of women in our previous studies,58,59 suggesting good generalizability.
The study also had a number of limitations, many of which might be addressed in future research. First, because it is not possible to blind participants to study condition, expectancy effects cannot be completely ruled out. Second, the intervention period was only 8 weeks in duration. This allowed us to demonstrate proof of concept; however, a longer treatment period may be needed to demonstrate sustained efficacy. The superior results obtained in the yoga intervention appear to weaken over time during follow-up. An intervention protocol that encouraged more home-practice of yoga or eased the transition from active treatment/studio practice to practice on one's own may have reduced this attrition in efficacy. Third, the sample size was small, thus limiting power to detect significant differences between conditions during the follow-up period. A slow recruitment process necessitated randomization by cohort, which produced unequal groups. Finally, our intervention targeted generally healthy adult women smokers. It is unclear what the ultimate reach of the yoga intervention might be for less healthy populations or whether it would offer additional benefits to smokers who are not sedentary.
Summary and Future Directions
Finally, in addition to a longer treatment period, a longer follow-up period may be needed, perhaps with a yoga maintenance period to see if sustained yoga leads to sustained smoking cessation. These limitations would be easily addressed in a larger trial, which appears warranted given the preliminary findings from this study. Future work should also examine whether yoga is more appropriate, acceptable, and/or more effective for certain types of smokers (e.g., younger vs. older, light vs. heavy smokers, men vs. women, those who prefer or cannot use medications).
Acknowledgments
This study was funded by a grant from the National Center for Complementary and Alternative Medicine (NCCAM) to Dr. Bock (AT003669).
Disclosure Statement
No competing financial interests exist for any of the authors.
References
- 1.Centers for Disease Control Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2009;57:1226–1228. [PubMed] [Google Scholar]
- 2.Centers for Disease Control Prevention. State-specific prevalence and trends in adult cigarette smoking—United States, 1998–2007. MMWR Morb Mortal Wkly Rep. 2009;58:221–226. [PubMed] [Google Scholar]
- 3.Centers for Disease Control Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 4.Hughes JR. Peters EN. Naud S. Relapse to smoking after 1 year of abstinence: a meta-analysis. Addict Behav. 2008;33:1516–1520. doi: 10.1016/j.addbeh.2008.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynoso J. Susabda A. Cepeda-Benito A. Gender differences in smoking cessation. J Psychopathol Behav Assess. 2005;27:227–234. [Google Scholar]
- 6.Royce JM. Corbett K. Sorenson G. Ockene J. Gender, social pressure, and smoking cessations: the Community Intervention Trial for Smoking Cessation (COMMIT) at baseline. Soc Sci Med. 1997;44:359–370. doi: 10.1016/s0277-9536(96)00149-9. [DOI] [PubMed] [Google Scholar]
- 7.Wetter DW. Kenford SL. Smith SS. Fiore MC. Jorenby DE. Baker TB. Gender differences in smoking cessation. J Consult Clin Psychol. 1999;67:555–562. doi: 10.1037//0022-006x.67.4.555. [DOI] [PubMed] [Google Scholar]
- 8.Piper ME. Cook JW. Schlam TR. Jorenby DE. Smith SS. Bolt DM. Loh WY. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine Tob Res. 2010;12:647–657. doi: 10.1093/ntr/ntq067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hudmon KS. Corelli RL. Prokhorov AV. Current approaches to pharmacotherapy for smoking cessation. Ther Adv Respir Dis. 2010;4:35–47. doi: 10.1177/1753465809353768. [DOI] [PubMed] [Google Scholar]
- 10.Fiore MC. Jaén CR. Baker TB, et al. Clinical Practice Guideline. Rockville MD: U.S. Department of Health and Human Services, Public Health Service; 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- 11.Cokkinides VE. Ward E. Jemal A. Thun MJ. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prevent Med. 2005;28:119–122. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Lader D. Goddard E. Smoking related behaviour and attitudes. London: Office for National Statistics; 2003. [Google Scholar]
- 13.Amodei N. Lamb RJ. Over-the-counter nicotine replacement therapy: can its impact on smoking cessation be enhanced? Psychol Addict Behav. 2008;22:472–485. doi: 10.1037/0893-164X.22.4.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu S. Melcer T. Sun J. Rosbrook B. Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prevent Med. 2000;18:305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 15.Bush TM. McAfee T. Deprey M. Mahoney L. Fellows JL. McClure J. Cushing C. The impact of a free nicotine patch starter kit on quit rates in a state quit line. Nicotine Tob Res. 2008;10:1511–1516. doi: 10.1080/14622200802323167. [DOI] [PubMed] [Google Scholar]
- 16.Murphy JM. Mahoney MC. Cummings KM. Hyland AJ. Lawvere S. A randomized trial to promote pharmacotherapy use and smoking cessation in a Medicaid population (United States) Cancer Causes Control. 2005;16:373–382. doi: 10.1007/s10552-004-6573-9. [DOI] [PubMed] [Google Scholar]
- 17.Raupach T. Shahab L. Eimer S. Puls M. Hasenfuss G. Andreas S. Increasing the use of nicotine replacement therapy by a simple intervention: an exploratory trial. Subst Use Misuse. 2010;45:403–413. doi: 10.3109/10826080903452496. [DOI] [PubMed] [Google Scholar]
- 18.Solomon LJ. Marcy TW. Howe KD. Skelly JM. Reinier K. Flynn BS. Does extended proactive telephone support increase smoking cessation among low-income women using nicotine patches? Prevent Med. 2005;40:306–313. doi: 10.1016/j.ypmed.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 19.Cummings KM. Hyland A. Giovino GA. Hastrup B. Bauer JE. Bansal MA. Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine Tob Res. 2004;6(Suppl. 3):S333–S340. doi: 10.1080/14622200412331320734. [DOI] [PubMed] [Google Scholar]
- 20.Hammond D. McDonald PW. Fong GT. Borland R. Do smokers know how to quit? Knowledge and perceived effectiveness of cessation assistance as predictors of cessation behavior. Addiction. 2004;99:1042–1048. doi: 10.1111/j.1360-0443.2004.00754.x. [DOI] [PubMed] [Google Scholar]
- 21.Juliano L. Brandon T. Smokers' expectancies for nicotine replacement therapy vs. cigarettes. Nicotine Tob Res. 2004;6:569–574. doi: 10.1080/14622200410001696574. [DOI] [PubMed] [Google Scholar]
- 22.Mooney ME. Leventhal AM. Hatsukami DK. Attitudes and knowledge about nicotine and nicotine replacement therapy. Nicotine Tob Res. 2006;8:435–446. doi: 10.1080/14622200600670397. [DOI] [PubMed] [Google Scholar]
- 23.Vogt F. Hall S. Marteau TM. Understanding why smokers do not want to use nicotine dependence medications to stop smoking: qualitative and quantitative studies. Nicotine Tob Res. 2008;10:1405–1413. doi: 10.1080/14622200802239280. [DOI] [PubMed] [Google Scholar]
- 24.Bock BC. Lewis BM. Jennings E. Marcus-Blank J. Marcus BH. Women and smoking cessation: challenges and opportunities. Curr Cardiovasc Risk Rep. 2009;3:205–210. [Google Scholar]
- 25.Clark MM. Hurt RD. Croghan IT. Patten CA. Novotny P. Sloan JA. Dakhil SR. Croghan GA. Wos EJ. Rowland KM. Bernath A. Morton RF. Thomas SP. Tschetter LK. Garneau S. Stella PJ. Ebbert LP. Wender DB. Loprinzi CL. The prevalence of weight concerns in a smoking abstinence clinical trial. Addict Behav. 2006;31:1144–1152. doi: 10.1016/j.addbeh.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 26.Galanti MR. Ivarsson BH. Helgason AR. Gilljam H. Smoking cessation: gender on the agenda. Drugs. 2002;9:71–84. [Google Scholar]
- 27.Perkins KA. Smoking cessation in women. Special considerations. CNS Drugs. 2001;15:391–411. doi: 10.2165/00023210-200115050-00005. [DOI] [PubMed] [Google Scholar]
- 28.Pomerleau CS. Zucker AN. Stewart AJ. Characterizing concerns about post-cessation weight gain: results from a national survey of women smokers. Nicotine Tob Res. 2001;3:51–60. doi: 10.1080/14622200020032105. [DOI] [PubMed] [Google Scholar]
- 29.Marcus BH. Albrecht AE. King TK. Parisi AF. Pinto BM. Roberts M. Niaura RS. Abrams DB. The efficacy of exercise as an aid for smoking cessation in women. Arch Intern Med. 1999;159:1229–1234. doi: 10.1001/archinte.159.11.1229. [DOI] [PubMed] [Google Scholar]
- 30.Pinto BM. Borrelli B. King TK. Bock BC. Clark MM. Roberts M. Marcus BH. Weight control smoking among sedentary women. Addict Behav. 1999;24:75–86. doi: 10.1016/s0306-4603(98)00034-3. [DOI] [PubMed] [Google Scholar]
- 31.Marcus BH. Lewis BA. Hogan J. King TK. Albrecht AE. Bock BC. Parisi AF. Niaura RS. Abrams DB. The efficacy of moderate-intensity exercise as an aid for smoking cessation in women: a randomized controlled trial. Nicotine Tob Res. 2005;7:871–880. doi: 10.1080/14622200500266056. [DOI] [PubMed] [Google Scholar]
- 32.Ussher M. Exercise interventions for smoking cessation. Cochrane Database of Systematic Rev. 2005;(1):CD002295. doi: 10.1002/14651858.CD002295.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Ussher M. West R. Doshi R. Sampuran AK. Acute effect of isometric exercise on desire to smoke and tobacco withdrawal symptoms. Hum Psychopharmacol. 2006;21:39–46. doi: 10.1002/hup.744. [DOI] [PubMed] [Google Scholar]
- 34.Ussher M. Taylor AH. West R. McEwen A. Does exercise aid smoking cessation? A systematic review. Addiction. 2000;95:199–208. doi: 10.1046/j.1360-0443.2000.9521996.x. [DOI] [PubMed] [Google Scholar]
- 35.Ussher M. West R. McEwen A. Taylor AH. Steptoe A. Efficacy of exercise counseling as an aid for smoking cessation: a randomised controlled trial. Addiction. 2003;98:523–532. doi: 10.1046/j.1360-0443.2003.00346.x. [DOI] [PubMed] [Google Scholar]
- 36.Annesi JJ. Relations of self-motivation, perceived physical condition, and exercise-induced changes in revitalization and exhaustion with attendance in women initiating a moderate cardiovascular exercise regimen. Womens Health. 2005;42:77–93. doi: 10.1300/j013v42n03_05. [DOI] [PubMed] [Google Scholar]
- 37.Annesi JJ. Changes in depressed mood associated with 10 weeks of moderate cardiovascular exercise in formerly sedentary adults. Psychol Rep. 2005;96(3 Pt 1):855–862. doi: 10.2466/pr0.96.3.855-862. [DOI] [PubMed] [Google Scholar]
- 38.Dunn AL. Trivedi MH. Kampert JB. Clark CG. Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prevent Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 39.Dunn AL. Trivedi MH. O'Neal HA. Physical activity dose-response effects on outcomes of depression and anxiety. Med Sci Sports Exerc. 2001;33(6 Suppl):S587–597. doi: 10.1097/00005768-200106001-00027. [DOI] [PubMed] [Google Scholar]
- 40.Knubben K. Reischies FM. Adli M. Schlattmann P. Bauer M. Dimeo F. A randomised, controlled study on the effects of a short-term endurance training programme in patients with major depression. Brit J Sports Med. 2007;41:29–33. doi: 10.1136/bjsm.2006.030130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsouka O. Kabitsis C. Harahousou Y. Trigonis I. Mood alterations following an indoor and outdoor exercise program in healthy elderly women. Percept Mot Skills. 2005;100:707–715. doi: 10.2466/pms.100.3.707-715. [DOI] [PubMed] [Google Scholar]
- 42.Scully D. Kremer J. Meade MM. Graham R. Dudgeon K. Physical exercise and psychological well being: a critical review. Brit J Sports Med. 1998;32:111–120. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bock BC. Marcus BH. King T. Borrelli B. Exercise effects on withdrawal symptoms and mood among women attempting smoking cessation. Addict Behav. 1999;24:399–410. doi: 10.1016/s0306-4603(98)00088-4. [DOI] [PubMed] [Google Scholar]
- 44.Gilbert DG. McClernon FJ. Rabinovich NE. Plath LC. Masson CL. Anderson AE. Sly KF. Mood disturbance fails to resolve across 31 days of cigarette abstinence in women. J Consult Clin Psychol. 2002;70:142–152. doi: 10.1037//0022-006x.70.1.142. [DOI] [PubMed] [Google Scholar]
- 45.Kassel JD. Stroud LR. Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 46.Shiffman S. Waters AJ. Negative affect and smoking lapses: a prospective analysis. J Consult Clin Psychol. 2004;72:192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- 47.Williams DM. Lewis BA. Dunsiger S. Whiteley JA. Papandonatos GD. Napolitano MA. Bock BC. Ciccolo JT. Marcus BH. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36:186–194. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kenford SL. Smith SS. Wetter DW. Jorenby DE. Fiore MC. Baker TB. Predicting relapse back to smoking: contrasting affective and physical models of dependence. J Consult Clin Psychol. 2002;70:216–227. [PubMed] [Google Scholar]
- 49.al'Absi M. Amunrud T. Wittmers LE. Psychophysiological effects of nicotine abstinence and behavioral challenges in habitual smokers. Pharmacol Biochem Behav. 2004;72:707–716. doi: 10.1016/s0091-3057(02)00739-6. [DOI] [PubMed] [Google Scholar]
- 50.Mishra RS. Fundamentals of Yoga: A Handbook of Theory, Practice and Applications. New York: Harmony Books; 1987. [Google Scholar]
- 51.Daubenmier JJ. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychol Women Q. 2005;29:207–219. [Google Scholar]
- 52.Janakiramaiah N. Gagadhar BN. NagaVenkatesha-Murthy PJ. Harish MG. Subbakrishna DK. Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–259. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]
- 53.Carlson LE. Culos-Reed N. Daroux LM. The effects of therapeutic yoga on salivary cortisol, stress symptoms, quality of life and mood states in cancer outpatients: a randomized controlled study. Presented at the Annual Meeting of the American Psychosomatic Society; Vancouver, BC. Mar;2005 . [Google Scholar]
- 54.Khumar SS. Kaur P. Kaur S. Effectiveness of shavasana on depression among university students. Indian J Clin Psychol. 1993;20:82–87. [Google Scholar]
- 55.Malathi A. Damodaran A. Shah N. Patil N. Maratha S. Effect of yoga practices on subjective well being. Indian J Physiol Pharmacol. 2000;44:202–206. [PubMed] [Google Scholar]
- 56.Woolery A. Myers H. Sternlieb B. Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60–63. [PubMed] [Google Scholar]
- 57.Thomas S. Reading J. Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can J Sport Sci. 1992;17:338–345. [PubMed] [Google Scholar]
- 58.Marcus BH. King TK. Albrecht AE. Parisi AF. Abrams DB. Rationale, design, and baseline data for commit to quit: an exercise efficacy trial for smoking cessation among women. Prevent Med. 1997;26:586–597. doi: 10.1006/pmed.1997.0180. [DOI] [PubMed] [Google Scholar]
- 59.Marcus BH. Lewis BA. King TK. Albrecht AE. Hogan J. Bock BC. Parisi AF. Abrams DB. Rationale, design, and baseline data for Commit to Quit II: an evaluation of the efficacy of moderate-intensity physical activity as an aid to smoking cessation in women. Prevent Med. 2003;36:479–492. doi: 10.1016/s0091-7435(02)00051-8. [DOI] [PubMed] [Google Scholar]
- 60.Bieling PJ. Antony MM. Swinson RP. The State-Trait Anxiety Inventory, Trait version: structure and content re-examined. Behav Res Ther. 1998;36:777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- 61.Heatherton TF. Kozlowski LT. Frecker RC. Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Brit J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 62.Spielberger CD. Gorsuch RL. Lushene R. Vagg PR. Jacobs GA. Manual for the State-trait Anxiety Inventory (Form Y Self-evaluation Questionnaire) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 63.Andresen EM. Malmgren JA. Carter WB. Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prevent Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 64.Ware JJ. Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 65.Velicer WF. DiClemente CC. Rossi JS. Prochaska JO. Relapse situations and self-efficacy: an integrative model. Addict Behav. 1990;15:271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- 66.Prochaska JO. DiClemente CC. Norcross JC. In search of how people change. Am Psychologist. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 67.Hughes JR. Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289–294. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 68.Weekley CK., 3rd Klesges RC. Reylea G. Smoking as a weight-control strategy and its relationship to smoking status. Addict Behav. 1992;17:259–271. doi: 10.1016/0306-4603(92)90031-p. [DOI] [PubMed] [Google Scholar]
- 69.Watson D. Clark LA. Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 70.Society for Research on Nicotine Tobacco. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 71.Zeger SL. Liang KY. Feedback models for discrete and continuous time series. Statistica Sinica. 1991;1:51–64. [Google Scholar]
- 72.Kassel JD. Stroud LR. Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 73.Kenford SL. Smith SS. Wetter DW. Jorenby DE. Fiore MC. Baker TB. Predicting relapse back to smoking: contrasting affective and physical models of dependence. J Consult Clin Psychol. 2002;70:216–227. [PubMed] [Google Scholar]
- 74.Shiffman S. Waters AJ. Negative affect and smoking lapses: a prospective analysis. J Consult Clin Psychol. 2004;72:192–201. doi: 10.1037/0022-006X.72.2.192. [DOI] [PubMed] [Google Scholar]
- 75.Bower JE. Woolery A. Sternlieb B. Garet D. Yoga for cancer patients and survivors. Cancer Control. 2005;12:165–171. doi: 10.1177/107327480501200304. [DOI] [PubMed] [Google Scholar]
- 76.Culos-Reed N. Carlson LE. Daroux LM, et al. Discovering the physical and psychological benefits of yoga for cancer survivors. Int J Yoga Ther. 2004;14:45–52. [Google Scholar]
- 77.Woolery A. Myers H. Sternlieb B, et al. A yoga intervention for young adults with elevated symptoms of depression. Alt Ther Health Med. 2004;10:60–63. [PubMed] [Google Scholar]
- 78.Manning BK. Catley D. Haris KJ. Mayo MS. Ahluwalia JS. Stress and quitting among African American smokers. J Behav Med. 2005;28:1–9. doi: 10.1007/s10865-005-9004-9. [DOI] [PubMed] [Google Scholar]