Abstract
Introduction:
Fibroids are very common tumors affecting women for centuries, however surprising that no significant data is still available as to what could be the cause of fibroid? What could be the predisposing or risk factors? Does it has any impact on fertility? Outcomes of Laparoscopic myomectomy in infertility?
Setting:
Advanced Tertiary Gynecologic endoscopic unit.
Aims and Objectives:
1) What are the predisposing factors to develop fibroids? 2) Do fibroids lead to infertility? 3) What are the indications for removal of fibroids in infertility? 4) Is laparoscopic surgery better than open surgery? 5) Is the risk of rupture uterus more after laparoscopic myomectomy? 6) What is the success in terms of pregnancy rate after myomectomy? 7) What are the chances of abortions with or without myomectomy?
Materials and Methods:
A retrospective research study was carried out on 2540 women at the National Institute of Laser and Endoscopic Surgery and Aakar IVF Centre, Mumbai, a referral centre in India. This study was done over a period of 14 years. Women varied in age from 23 to 51 years and infertility of at least more than three years. The woman had fibroids from one to seventeen in number and two centimeters to eighteen centimeters in size which were either submucous, intramural, serosal, cervical or broad ligament. The women requiring hysteroscopic myoma resection were excluded in this study and Laparoscopic myomectomy done in woman other than infertility are also excluded from the study.
Results:
During the course of our study we found that the diet, weight, hypertension, habits had a bearing on incidence of fibroid. In one of the most promising research fact we found that fibroids itself produce prolactin and due to three times high level of aromatase had higher level of estradiol locally compared to normal myometrium. This was detrimental to fertility. A mild elevation of blood levels of prolactin usually in the range of 40 – 60 ng/ml was noticed in nearly 42% of the cases. Fibroids with infertility as a major complaint along with excessive vaginal bleeding in 33%, pain abdomen and dysmenorhea 10%, pressure symptoms in 3%, accidental finding of a large mass in 5% were the major indications for laparoscopic myomectomy. The pregnancy rate after removal of fibroids with active fertility treatment was 42 % and in donor oocyte IVF was 50%, abortion rate was 5%, 64% LSCS, 31% vaginal deliveries. There was no scar rupture in all pregnancies post laparoscopic myomectomy.
Conclusion:
Presence of fibroids in first degree female relative, predominantly red meat eating women, excess weight and high Blood pressure increased incidence of fibroids. Pregnancies & oral contraceptives decreased chances of fibroids. In infertile patient fibroids of significant size, multiple, had high local prolactin & aromatase level affecting fertility. Laparoscopic removal of fibroids increased pregnancy rate to 37.2% & 50% in donor oocyte IVF.
Keywords: Fibroids, infertility, predisposing factors, laparoscopic myomectomy
INTRODUCTION
Treatment innovations have been slow, perhaps because many women have an asymptomatic fibroids, myomas are benign and mortality is very low.[1] If hysterectomy was the treatment options given; some women choose to bear with the symptoms and stop seeking treatment.
It is surprising that for more than a century there is no major research on causes of Fibroids, actual impact on fertility and outcome of newer minimally invasive surgical techniques.
MATERIALS AND METHODS
In our retrospective research study over 14 years on 2540 patients of fibroids managed at our Endoscopic Surgery and IVF Centre, a tertiary specialized centre, we analyzed factors contributing to the incidence of fibroids. The impact of fibroids on fertility and outcome of Laparoscopic myomectomy in 1788 indicated cases was studied. Those women who required hysteroscopic resection of myoma and Laparoscopic myomectomy for women with no fertility problems also were not included in this study.
Inclusion criteria
Indications of laparoscopic myomectomy for fertility enhancement
Our criteria for removal of fibroid in an infertile woman was
-
(a)
Multiple more than four fibroids of more than four centimeters in size.
-
(b)
Large fibroids more than five centimeters upto 18 cms in size with more than three years of infertility
-
(c)
Fibroid indenting the endometrial cavity.
-
(d)
Fibroid compressing the tubal ostia or distorting tubo ovarian anatomy.
-
(e)
Fibroids associated with raised prolactin levels.
-
(f)
Fibroids associated with increased vascularity and excessive bleeding.
-
(g)
Any non pedunculated fibroids of more than five cm in size in a patient to be taken up for IVF or ICSI [Figures 1 and 2].
-
(h)
Women with fibroids of more than five centimeters with history of more than one spontaneous abortion.
-
(i)
Fibroid affecting tubo-ovarian anatomy/multiple fibroids [Figures 3–5 and Table 1].
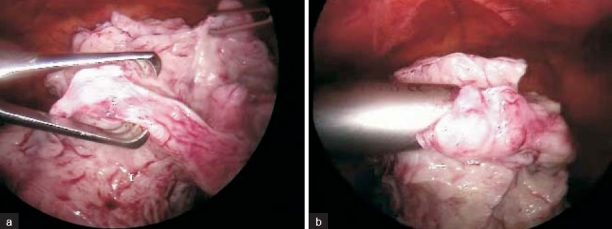
Figure 1.
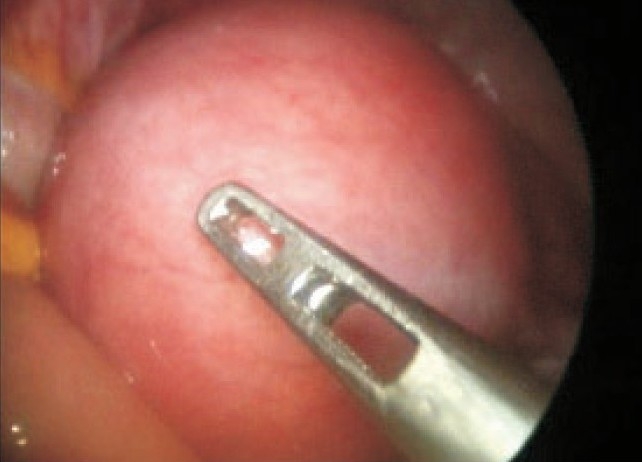
Large intramural fibroid
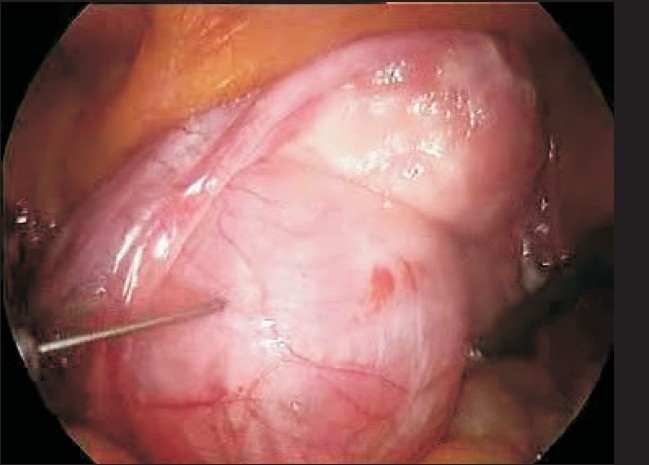
Figure 2.

Multiple and large intramural fibroids
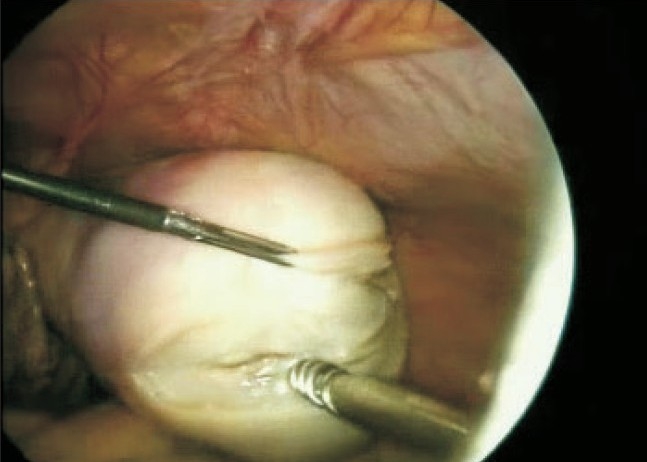
Figure 3.
Left broad ligament fibroid
Figure 5.
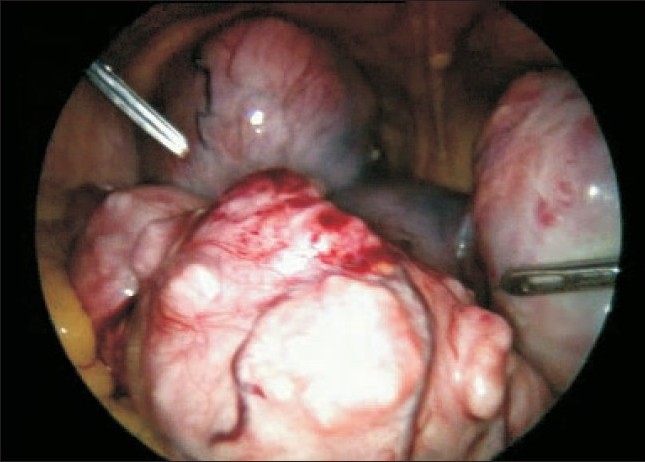
Multiple large fibroids
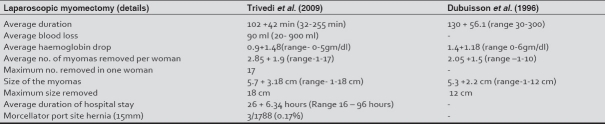
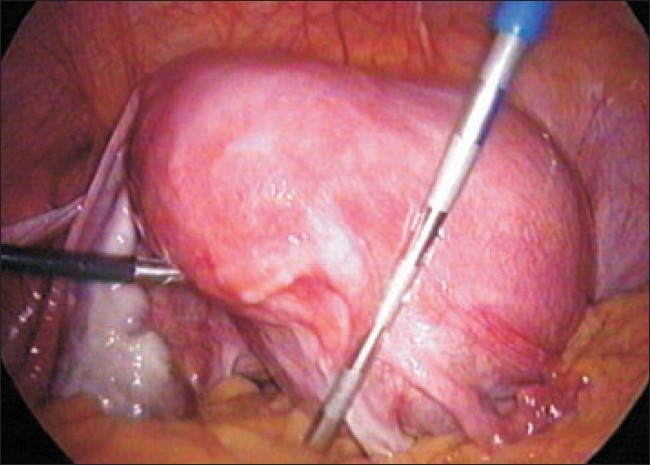
Table 1.
Details of women of laparoscopic myomectomy (788 cases)
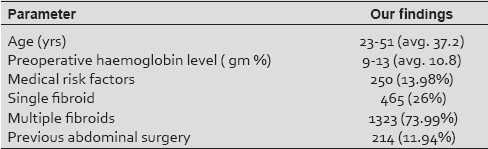
Figure 4.
Fibroid distorting tuboovarian anatomy
Surgical procedure
Patient's position
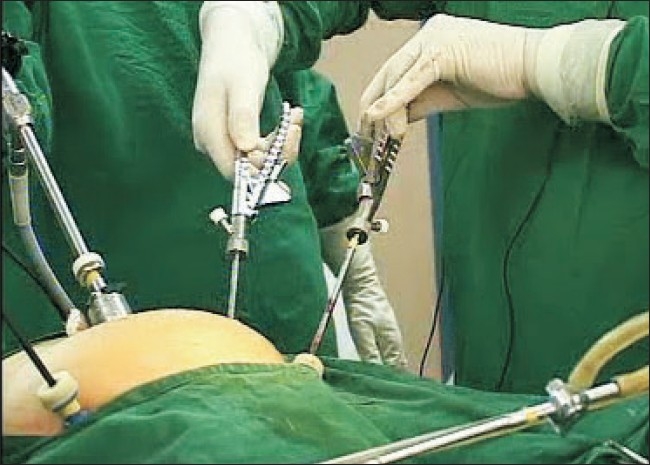
Woman is placed in modified lithotomy position as shown in Figure 6. Allen's stirrups are the ideal leg rests to have but in absence, 45 degree angle in padded leg holders was the option.
Figure 6.

Patient's position – Modified lithotomy position with Allen's stirrups
Unlike the popular belief, fibroids of any size do not have stalk blood supply. They have a “parasitic” blood supply, Myoma is completely surrounded by vascular layer that supplies the myoma and there is no so-called vascular pedicles existing at the base of myoma.[2]
After pneumoperitoneum is created 10mm trocar is inserted through umbilical incision (or two inches above umbilicus in uterus of more than 18-20 wks). We prefer five mm, short flower valve trocars at the three ancillary ports (two Ipsilateral port placement [Figure 11).
Figure 11.
Ipsilateral port placement
A dilute vasopressin one ampoule (20 units) in 100ml. of normal saline is injected in the cleavage between fibroid capsule and uterine muscle Nezhatet al.[3] [Figure 7]. Pitressin, is synthetic vasopressin decreases blood loss during myomectomy and in a prospective, randomized study, was as effective as mechanical closure of uterine and ovarian vessels.[4,5]
Figure 7(a-d).
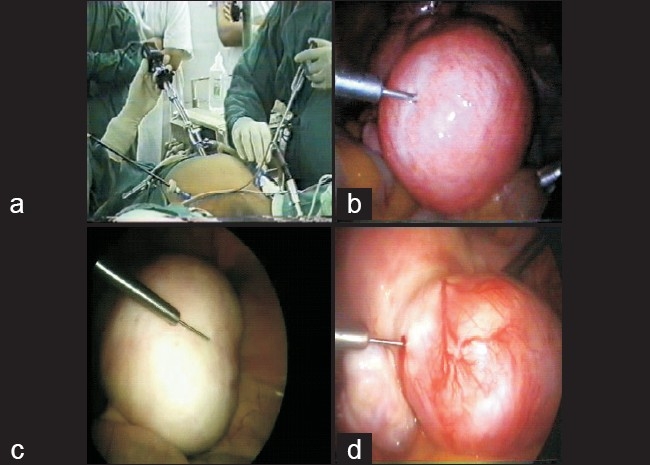
Injecting vasopressin in the proper plane
We prefer a horizontal incision made with a monopolar or plasma kinetic spatula or hook of harmonic scalpel, adequate to remove the fibroid Figure 8. The midline vertical incision cuts multiple arcuate vessels and may be associated with greater blood loss.[6] Transverse incisions parallel to the arcuate vessels may reduce bleeding by avoiding many of these vessels[7] [Figure 8].
Figure 8.

Horizontal incision with spatula
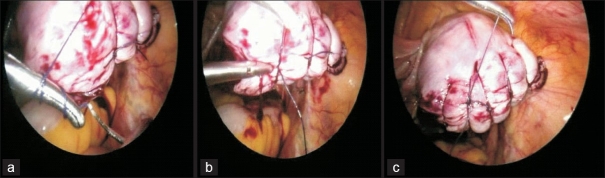
A myoma screw is put in left upper port to fix the fibroid and gently pull it as spatula dissects the surrounding tissue of the fibroid [Figure 9a,b].
Figure 9 (a-b).
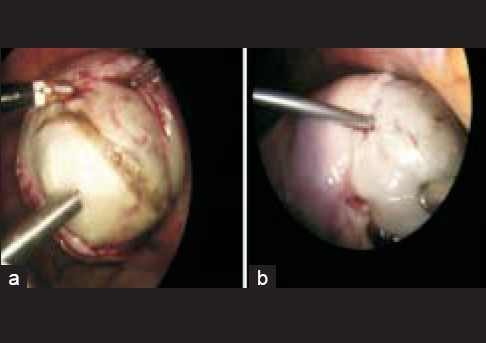
Enucleation of fibroid from uterus
After removal fibroids are parked in appendicular area [Figure 10].
Figure 10.
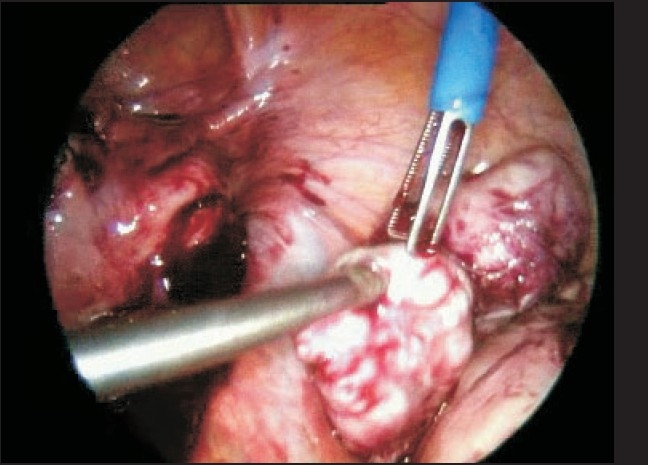
Parking separated fibroids near appendix
Some surgeons use scissors to cut the myometrium over the fibroids due to a belief that electrocautery may affect tissue healing. We don’t agree with this and use pure cutting current or plasma kinetic spatula or harmonic hook set at a proper level, for last 15 years this has not increased any rupture uterus.
We have designed the “Ipsilateral technique of laparoscopic suturing”, standing on the same left side of the patient Figure 11 which is comfortable. This method simulates the physiological movements while operating prevents fatigue and 6-7 sutures can be taken with a 100 cm suture length on curved needle.
The suture with curved on-needle is introduced through the left lower port by H. Reich and Clarke method. We commonly use polygalactin 910 no.1-0 for suturing the myometrium. Deep interrupted sutures in single layer are taken with distance of one centimeter in between to obliterate the myometrial bed completely [Figures 12 and 13]. This ensures proper haemostasis and also approximates the myometrial flaps.
Figure 12.
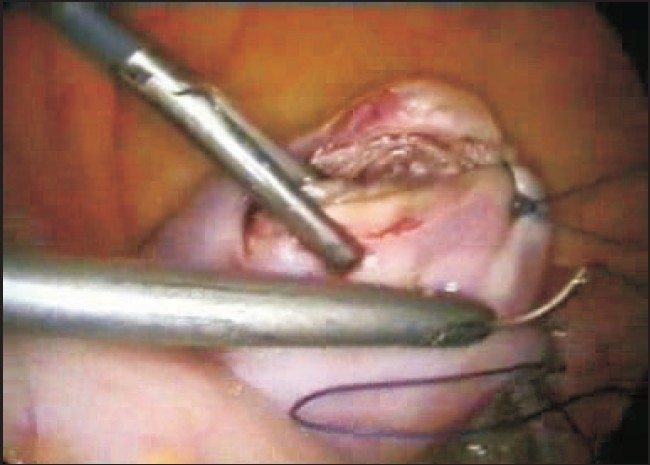
Grasping and driving the needle through posterior wall
Figure 13.
Intracorporeal ipsilateral suturing of incision on uterus
Intracorporeal suturing
After proper suturing a meticulous lavage is given and fibroids are removed by morcellation. We have found that in majority of cases suturing in single layer had no disadvantages over multiple layer suturing. In our experience, multiple layer suturing rather has associated risk of eversion of layers while suturing, which makes suturing difficult and adds to the risk of rupture due to improper approximation.
Paul et al. [8] have also reported that single layer suturing, if done by a skilled laparoscopic surgeon, does not compromise the integrity of the subsequent scar. In cases of broad ligament fibroid, we prefer a posterior incision [Figure 14].
Figure 14.

Broad ligament fibroid
The ureters are always lateral and their course is altered. Most of the broad ligament fibroids might not require the suturing of the bed or dead space, as they do not involve a bulk of the myometrial tissue. Drainage in such cases is always posterior. We would emphasize here that if an anterior incision is made, then the exudates or blood may get collected in the leaves of the broad ligament. In cases of multiple fibroids it is always prudent to remove the fibroids from the most prominent area. Limiting the number of uterine incisions can reduce adhesions on the uterine serosa.[9] However distant myomas extracted through the tunnel created within the myometrium make haemostatic defects and difficulty to control bleeding.[10]
Morcellation is done with a 10 mm or 15 mm morcellator. We normally prefer a reusable morcellator–Rotocut's morcellator, [Figure 15a,b] (Karl Storz, Gmbh Germany).
Figure 15 (a-b).
Morcellation of fibroid with rotocut morcellator
The left lower port is the preferred port wherein the five mm incision is widened to 10-15 mm, morcellation is always under vision. Long pieces of fibroids morcellated are seen in the tray [Figure 16].
Figure 16.

Tray full of morcellated pieces of fibroid
In cases of very large fibroid the author prefers to use a 10 mm myoma screw from the right sided port introduced higher than normal. Figure 17 In the absence or malfunction of morcellator, if the woman is sexually active, colpotomy is a “poor man's morcellator”. Colpotomy is performed by a spatula or hook incising over the protruding CCL Colpo Chirurgie Lausane trocar in the posterior fornix. Fibroids are fed from above to the claw forceps in the vagina. The stretchability of the vagina is remarkable and hence even the large fibroid can be removed. The wound is closed from below using polyglactin No. 1 or 1-0. An intraperitoneal drain, usually 16 G Ryle's tube is placed through the right port, reduces postoperative pyrexia and adhesion formation.
Figure 17.
10 mm Myoma screw for very large fibroid enucleation
Out of 2540 women with fibroid, only 1788 needed myomectomy which we essentially did laparoscopically excluding hysteroscopic myoma resection. In nearly 28.3% surgery was not needed, since the fibroid was not contributing to infertility.
Women were advised to plan conception two months after surgery. The average operating time of laparoscopic myomectomy varied from 32 minutes to 255 minutes depending on the number and size of the fibroids [Table 2].
Table 2.
Comparison of different parameters of laparoscopic myomectomy between Trivedi et al. and Dubuisson et al.
In our study we had a pregnancy rate after laparoscopic myomectomy of 42% with active fertility management including IUI, IVF – ICSI. Surprisingly the highest pregnancy rate was 50% in the group of donor oocyte IVF or ICSI. Out of the total number of pregnancies we had 64% caesarian section, 31% vaginal delivery and 5% abortions. There was no uterine scar rupture noticed or reported so far in our study. We had to convert less than 1% of our cases to laparotomy mainly because of poor case selection or history of previous open surgery coexisting with extensive endometriosis. In 22 cases of laparoscopic myomectomy, women needed blood transfusion because of either primarily border line low hemoglobin or in few cases due to excess blood loss.
DISCUSSION
Predisposing factors of fibroid obtained in our study were
If a first-degree female relative had the fibroid detected before the age of 45 then she carries six times higher chances of having fibroids than the control group i.e. 30% vs 5% in controls.[11]
Age at 45 to 50 years of age, fibroids was 20 times more than women between 25 to 30 years of age (6.2 per thousand vs 0.3 per thousand).[12]
A red meat eating women has three times higher chances of having fibroids compared to women having a vegetarian diet or mainly fish eating women.[13]
For every 10 kg rise in weight of patient there is 18% increase in incidence of fibroids.[14]
For every 10 mm rise in diastolic blood pressure there is 10% increase in incidence of fibroids. Hypertensive women in later years had 24 % chances to be having fibroids and the degree of fibroids were proportionate to the severity of the hypertension.[15]
A women who had a habit of smoking cigarettes, beedi's etc they had less incidence of fibroids this was probably due to associated lower levels of estrogen.[16,17]
The use of oral contraceptive and parity also reduced the incidence of fibroids. In the group with the longest use more than 145 months, the risk of fibroids was half that of control. However, if the oral contraceptive was used for the first time between 13 to 16 years of age than this increase the risk of fibroid.[18]
The growth rate of fibroids we noticed was average 1.25 cm in 2.5 years.[19] Even sometimes a fast-growing fibroid didn’t mean that it was sarcomatous.
Parity reduced the risk of fibroids three to five fold, showed more specifically in the later age as the incidence of fibroids are higher in later age.[20]
The recurrence rate of fibroids after removal is from 25 to 62% by the end of 5 years follow-up, in nearly 10 to 20% needed a second surgery within one to ten years.[21]
The tissue prolactin level was high in the fibroid tissue acts as a stimulator of the proliferation of Leiomyoma cells by the mitogen activated protein kinase cascade.[22] This was suppressed by anti-prolactin antibodies and also progestrone showed suppressive effect.[23–26]
Fibroids express three times high aromatase levels than surrounding myometrium, increases active estradiol promoting growth of fibroids. Aromatase mRNA was detectable in 91% of myomas 75% at two cm from the myoma and not detectable in disease-free myometrium of the uterus. [27–32] A situation of local hyperprolactineamia and local hyperestrogenimea leading to infertility and abortions. Uterine Leiomyoma is even reported in 27% of infertile women[33] and 50% of women with unexplained infertility became pregnant after myomectomy.
Myomas of less than five centimeters increases in size in the first trimester however myomas which were larger they reduce in the second trimester and all myomas reduced in the third trimester of pregnancy.[34,35] The spontaneous abortion rate was 41% in cases of myomas of significant size, this reduced to 19% after myomectomy.[36–38] Patients of fibroids with pregnancy had increased incidence of bleeding in the first trimester premature rupture of membranes, breech presentation placental abruption prolonged labor higher caesarean section rate. The estimation of premature labor was 15 to 20%, intrauterine growth restrictions in 10% and malpresentations in 20%.[39–41]
The risk of malignant transformation in myomas: Literature suggests Leiomyosarcoma incidence from 0.23% in premenopausal women to 2% in postmenopausal women .[42] The incidence of Leiomyosarcoma is 0.67 per 1,00,000 women per year.[43]
Specific risks of laparoscopic myomectomy
Surgery and anesthesia is longer judicious monitoring and good anesthesia avoids morbidity.
Major risk imagined is the future rupture of the uterus in pregnancy in antenatal period or during labor. [44–49] This is due to the popular belief, rather misconception, that laparoscopic suturing is inferior to an open surgery.
Excessive bleeding, but use of dilute vasopressin and right plane of dissection, decreases the blood loss. GnRh analogues offer significant benefit, only in severely anaemic patients, in whom immediate surgery is avoided. We do not advocate prophylactic suturing of both uterine vessels to reduce bleeding in a patient keen for conception. This increases risk of ureteric injury and bleeding can occur due to collateral blood supply.
Conversion to laparotomy: In our study we had 0.75% (14 cases) of conversion to a Laparotomy, mainly due to inappropriate patient selection. The risk of conversion is nearly three times more, when the sizes of the fibroid are more than eleven centimeters, or are anterior in location. Dubuissonet al .[44] reported a three times higher conversion rate when fibroids measured more than eight centimeters or located anteriorly. Conversion to a Laparotomy is actually a prudent judgment on the part of the surgeon.
Post operative adhesions: after laparoscopic myomectomy, chances of adhesions are much lesser than that of an open surgery .Adhesion barriers are thought to prevent or significantly reduce the incidence of formation of postoperative adhesions[50] their actual benefit is still a matter of debate.
Technical complications of laparoscopic myomectomy and prevention
Breakage of myoma screw (nine cases) happened while pulling the myoma with the screw out of the uterus. One should ensure that removal of the broken piece is always done before the conclusion of the procedure, taking care of not slipping suddenly when it can get lost in the peritoneal cavity
Laparoscopic myomectomy if judiciously employed in properly selected cases definitely offers significant advantages over an abdominal myomectomy, but the surgeon should be well trained and skilled in the procedure. The advantages: short hospital stay, faster recovery, less post operative pain, decreased thrombo-embolic phenomenon.[51]. The maximum number and size of fibroids removed laparoscopically can not be generalized as it is dependent on surgeon's skill, skill of endosuturing, operation theatre setup and assisting team.
The true contraindication of laparoscopic myomectomy is any medical condition which can worsen with abdominal distention and trendelenburg position for prolonged period. The relative contraindication may be diffuse leiomyomata.
In a series reported by Seinera et al.,[52] 65 pregnancies were achieved in 54 women with no case of uterine rupture. In another study by Dubuisson et al.,[53] The estimated risk of uterine rupture has been reported to be 1.0 % (95% CI 0.0-5.5).
Dubuisson et al. [4] reported a scar rupture from a three cm posterior wall fibroid removed and sutured properly by him. The author has observed an interesting fact relevant to uterine scar rupture post myomectomy namely when a lower segment caesarean section is done the round ligaments are very close to the lower segment incision even at full term suggesting that the stretchable part of the uterus is usually above the round ligament and posterior wall, hence whenever there is a large or multiple fibroids removed from this area an elective caesarean section is strongly recommended at 36–37 weeks or unexplained pain in abdomen with tachycardia suggesting an impending rupture.
An interesting detail from the world fibroid registry has clearly pointed out that the uterine scar rupture after open myomectomy is grossly under reported or missed.[54,55] Further the International registry of fibroid also firmly quotes that chances of laparoscopic myomectomy scar to rupture in the hands of expert is less than a lower segment caesarean section scar rupture and far less than a classical caesarean section scar rupture1.[56]
Breakthrough in histopathology of fibroids
In histopathology we had one Endometrial stromal tumor, one Desmoid, one Primary uterine malignancy thought to be Fibroid. Kempson and co-workers[57–61] for four decades[62,63] evaluated whether the cells show smooth muscle or endometrial stromal differentiation. Architectural features, such as fascicular alignment of the tumor cells and the presence of thick walled vascularity, favor with a smooth muscle tumor. The vessels in endometrial stromal tumor are mainly thin-walled capillaries in arching pattern. In difficult cases, immunohistochemical staining with this Desmin, CD-10, and caldesmon may aid in determining whether the cells are of smooth muscles or endometrial stromal origin[64]. In endometrial stromal tumors infiltration of myometrium or vessels indicates malignant behavior[65]. In smooth muscle tumors, despite of infiltrating pattern the clinical course may be benign. Fibroids without any features of malignancy, such as coagulative necrosis, significant atypia or increased mitotic index (MI), yet they do metastasize. There can be nodes in lung, lymph nodes yet relatively non aggressive.[66–69]
Unusual differentiation of so called fibroids
Epitheloid (clear cell)/ Myxoid differentiation with M.I. equal or more than 5mf / 10 HPF prognosis is poor irrespective of absent tumor necrosis or cytological atypia.[70,71]
Molecular markers of prognosis immunostaining for Ki-- 67 can be useful for differentiation of Leomyosarcoma (50%) from Leiomyoma (8%).[72–75]
Leiomyosarcoma are isolated lesions and not originating from fibroids, an Austrian multi-institutional study of 71 cases of Leiomyosarcoma accumulated over ten years revealed that none arise from any myoma, which may mean that Leiomyosarcoma is primarily a tumor on its own thought to be myoma at some stage which may be myth than reality.[76]
CONCLUSIONS
In a retrospective study of 2540 cases fibroids over 14 years we could find certain factors predisposing occurrence of fibroids: first degree female relative having fibroid, diet, weight, age, hypertension increases but oral contraceptives, parity reduces chances.
A major breakthrough revealed fibroids having higher levels of aromatase converting estrogens to estradiol and high prolactin were detrimental to pregnancy. Laparoscopic removal of significant size fibroids increased pregnancy rate both spontaneous, or on infertility ~ ART treatment specially even in donor oocyte program.
Laparoscopic myomectomy in properly selected cases has significant advantages in the hands of well trained and skilled surgeon. The pregnancy rates after removal of fibroids laparoscopically in infertility and ART was higher with less abortion rate. Also the unnecessary feared uterine scar rupture after the laparoscopic myomectomy is disproved in the hands of expert.
In our study we had a pregnancy rate after laparoscopic myomectomy of 42% with active fertility management including IUI, IVF – ICSI. Surprisingly the highest pregnancy rate was 50% in the group of donor oocyte IVF or ICSI. There was no uterine scar rupture noticed or reported so far in our study. We had to convert more than 1% of our cases to laparotomy.
Finally what looks like Fibroids can be Leiomyoma, Endometrial stromal tumor, Epitheloid, Myxoid, Leiomyosarcoma or rarely desmoid tumor.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Walker CL, Stewart EA. Uterine fibroids: the elephant in the room. Science. 2005;308:1589–92. doi: 10.1126/science.1112063. [DOI] [PubMed] [Google Scholar]
- 2.Walocha JA, Litwin JA, Miodoński AJ. Vascular system of intramural leiomyomata revealed by corrosion casting and scanning electron microscopy. Hum Reprod. 2003;18:1088–93. doi: 10.1093/humrep/deg213. [DOI] [PubMed] [Google Scholar]
- 3.Nezhat C, Siegler A, Nezhat F. 2nd ed. Vol. 18. McGraw-Hill; 2000. Laparoscopic operations on the uterus. In operative Gynaecologic Laparoscopy principles and techniques; pp. 1088–93. 2000: 261-99d. [Google Scholar]
- 4.Frederick J, Fletcher H, Simeon D, Mullings A, Hardie M. Intramyometrial vasopressin as a haemostatic agent during myomectomy. Br J Obstet Gynaecol. 1994;101:435–7. doi: 10.1111/j.1471-0528.1994.tb11918.x. [DOI] [PubMed] [Google Scholar]
- 5.Ginsburg ES, Benson CB, Garfield JM, Gleason RE, Friedman AJ. The effect of operative technique and uterine size on blood loss during myomectomy: a prospective randomized study. Fertil Steril. 1993;60:956–62. [PubMed] [Google Scholar]
- 6.Guarnaccia MM, Rein MS. Traditional surgical approaches to uterine fibroids: abdominal myomectomy and hysterectomy. Clin Obstet Gynecol. 2001;44:385–400. doi: 10.1097/00003081-200106000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Igarashi M. Value of myomectomy in the treatment of infertility 1993;59:1331-2. Fertil Steril. 1993;59:1331–2. doi: 10.1016/s0015-0282(16)56003-8. [author reply 1332-3] [DOI] [PubMed] [Google Scholar]
- 8.Paul PG, Koshy AK, Thomas T. Pregnancy outcomes following myomectomy and single layer myometrial closure. Hum Reprod. 2006;21:3278–81. doi: 10.1093/humrep/del296. [DOI] [PubMed] [Google Scholar]
- 9.Guarnaccia MM, Rein MS. Traditional surgical approaches to uterine fibroids: abdominal myomectomy and hysterectomy. Clin Obstet Gynecol. 2001;44:385–400. doi: 10.1097/00003081-200106000-00024. [DOI] [PubMed] [Google Scholar]
- 10.West S, Ruiz R, Parker WH. Abdominal myomectomy in women with very large uterine size. Fertil Steril. 2006;85:36–9. doi: 10.1016/j.fertnstert.2005.05.073. [DOI] [PubMed] [Google Scholar]
- 11.Sato F, Mori M, Nishi M, Kudo R, Miyake H. Familial aggregation of uterine myomas in Japanese women. J Epidemiol. 2002;12:249–53. doi: 10.2188/jea.12.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faerstein E, Szklo M, Rosenshein N. Risk factors for uterine leiomyoma: a practice based case-control study. 1. African-American heritage, reproductive history, body size, and smoking. Am J Epidemiol. 2001;153:1–10. doi: 10.1093/aje/153.1.1. [DOI] [PubMed] [Google Scholar]
- 13.Chiaffarino F, Parazzini F, La Vecchia C, Chatenoud L, Di Cintio E, Marsico S. Diet and uterine myomas. Obstet Gynecol. 1999;94:395–8. doi: 10.1016/s0029-7844(99)00305-1. [DOI] [PubMed] [Google Scholar]
- 14.Faerstein E, Szklo M, Rosenshein N. Risk factors for uterine leiomyoma: a practice based case-control study. 1. African-American heritage, reproductive history, body size, and smoking. Am J Epidemiol. 2001;153:1–10. doi: 10.1093/aje/153.1.1. [DOI] [PubMed] [Google Scholar]
- 15.Boynton-Jarrett R, Rich-Edwards J, Malspeis S, Missmer SA, Wright R. A prospective study of hypertension and risk of uterine leiomyomata. Am J Epidemiol. 2005;161:628–38. doi: 10.1093/aje/kwi072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross RK, Pike MC, Vessey MP, Bull D, Yeates D, Casagrande JT. Risk factors for uterine fibroids: reduced risk associated with oral contraceptives. Br Med J. 1986;293:359–61. doi: 10.1136/bmj.293.6543.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parazzini F, Chiaffarino F, Polverino G, Chiantera V, Surace M, La Vecchia C. Uterine fibroids risk and history of selected medical conditions linked with female hormones. Eur J Epidemiol. 2004;19:249–53. doi: 10.1023/b:ejep.0000020448.43323.2a. [DOI] [PubMed] [Google Scholar]
- 18.Ross RK, Pike MC, Vessey MP, Bull D, Yeates D, Casagrande JT. Risk factors for uterine fibroids: reduced risk associated with oral contraceptives. Br Med J. 1986;293:359–61. doi: 10.1136/bmj.293.6543.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeWaay DJ, Syrop CH, Nygaard IE, Davis WA, Van Voorhis BJ. Natural history of uterine polyps and leiomyomata. Obstet Gynecol. 2002;100:3–7. doi: 10.1016/s0029-7844(02)02007-0. [DOI] [PubMed] [Google Scholar]
- 20.Chen CR, Buck GM, Courey NG, Perez KM, Wactawski-Wende J. Risk factors for uterine fibroids among women undergoing tubal sterilization. Am J Epidemiol. 2001;153:20–6. doi: 10.1093/aje/153.1.20. [DOI] [PubMed] [Google Scholar]
- 21.Hanafi M. Predictors of leiomyoma recurrence after myomectomy. Obstet Gynecol. 2005;105:877–81. doi: 10.1097/01.AOG.0000156298.74317.62. [DOI] [PubMed] [Google Scholar]
- 22.Daly DC, Walters CA, Prior JC, Kuslis ST, Chapitis J, Andreoli J, et al. Prolactin production from proliferative phase leiomyoma. Am J Obstet Gynecol. 1984;148:1059–63. doi: 10.1016/s0002-9378(84)90445-9. [DOI] [PubMed] [Google Scholar]
- 23.Austin DJ, Nowak RA, Stewart EA. Onapristone suppresses prolactin production in explant cultures of leiomyoma. Gynecol Obstet Invest. 1999;47:268–71. doi: 10.1159/000010120. [DOI] [PubMed] [Google Scholar]
- 24.Wolf JP, Hsiu JG, Anderson TL, Ulmann A, Baulieu EE, Hodgen GD. Noncompetitive antiestrogenic effect of RU 486 in blocking the estrogen-stimulated luteinizing hormone surge and the proliferative action of estradiol on endometrium in castrate monkeys. Fertil Steril. 1989;52:1055–60. doi: 10.1016/s0015-0282(16)53174-4. [DOI] [PubMed] [Google Scholar]
- 25.Horwitz KB. The molecular biology of RU486.Is there a role for antiprogestins in the treatment of breast cancer? Endocr Rev. 1992;13:146–63. doi: 10.1210/edrv-13-2-146. [DOI] [PubMed] [Google Scholar]
- 26.Nowak RA, Mora S, Diehl T, Rhoades AR, Stewart EA. Prolactin is an autocrine or paracrine growth factor for human myometrial and leiomyoma cells. Gynecol Obstet Invest. 1999;48:127–32. doi: 10.1159/000010154. [DOI] [PubMed] [Google Scholar]
- 27.Folkerd EJ, Newton CJ, Davidson K, Anderson MC, James VH. Aromatase activity in uterine leiomyomata. J Steroid Biochem. 1984;20:1195–200. doi: 10.1016/0022-4731(84)90366-2. [DOI] [PubMed] [Google Scholar]
- 28.Yamamoto T, Takamori K, Okada H. Effect of aminoglutethimide on androstenedione aromatase activity in human uterine leiomyoma. Horm Metab Res. 1985;17:548–9. doi: 10.1055/s-2007-1013603. [DOI] [PubMed] [Google Scholar]
- 29.Bulun SE, Simpson ER, Word RA. Expression of the CYP19 gene and its product aromatase cytochrome P450 in human leiomyoma tissues and cells in culture. J Clin Endocrinol Metab. 1994;78:736–48. doi: 10.1210/jcem.78.3.8126151. [DOI] [PubMed] [Google Scholar]
- 30.Sumitani H, Shozu M, Segawa T, Murakami K, Yang HJ, Shimada K, et al. In situ estrogen synthesized by aromatase P450 in uterine leiomyoma cells promotes cell growth probably via and autocrine/intracrine mechanism. Endocrinology. 2000;141:3852–61. doi: 10.1210/endo.141.10.7719. [DOI] [PubMed] [Google Scholar]
- 31.Otubu JA, Buttram VC, Besch NF, Besch PK. Unconjugated steroids in leiomyomas and tumor bearing myometrium. Am J Obstet Gynecol. 1982;143:130–3. doi: 10.1016/0002-9378(82)90640-8. [DOI] [PubMed] [Google Scholar]
- 32.Pasqualini JR, Cornier E, Grenier J, Vella C, Schatz B, Netter A. Effect of decapeptyl, an agonistic analog of gonadotropin-releasing hormone on estrogens, estrogen sulfates, and progesterone receptors in leiomyoma and myometrium. Fertil Steril. 1990;53:1012–7. [PubMed] [Google Scholar]
- 33.Bulletti C, De Ziegler D, Polli V, Flamigni C. The role of leiomyomas in infertility. J Am Assoc Gynecol Laparosc. 1999;6:441–5. doi: 10.1016/s1074-3804(99)80008-5. [DOI] [PubMed] [Google Scholar]
- 34.Lev-Toaff AS, Coleman BG, Arger PH, Mintz MC, Arenson RL, Toaff ME. Leiomyomas in pregnancy: sonographic study. Radiology. 1987;164:375–80. doi: 10.1148/radiology.164.2.3299488. [DOI] [PubMed] [Google Scholar]
- 35.Strobelt N, Ghidini A, Cavallone M, Pensabene I, Ceruti P, Vergani P. Natural history of uterine leiomyomas in pregnancy. J Ultrasound Med. 1994;13:399–401. doi: 10.7863/jum.1994.13.5.399. [DOI] [PubMed] [Google Scholar]
- 36.Buttram VC, Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981;36:433–45. doi: 10.1016/s0015-0282(16)45789-4. [DOI] [PubMed] [Google Scholar]
- 37.Propst AM, Hill JA., 3rd Anatomic factors associated with recurrent pregnancy loss. Semin Reprod Med. 2000;18:341–50. doi: 10.1055/s-2000-13723. [DOI] [PubMed] [Google Scholar]
- 38.Benson CB, Chow JS, Chang-Lee W, Hill JA, 3rd, Doubilet PM. Outcome of pregnancies in women with uterine leiomyomas identified by sonography in the first trimester. J Clin Ultrasound. 2001;29:261–4. doi: 10.1002/jcu.1031. [DOI] [PubMed] [Google Scholar]
- 39.Rice JP, Kay HH, Mahony BS. The clinical significance of uterine leiomyomas in pregnancy. Am J Obstet Gynecol. 1989;160:1212–6. doi: 10.1016/0002-9378(89)90194-4. [DOI] [PubMed] [Google Scholar]
- 40.Muram D, Gillieson M, Walters JH. Myomas of the uterus in pregnancy: ultrasonographic follow-up. Am J Obstet Gynecol. 1980;138:16–9. doi: 10.1016/0002-9378(80)90005-8. [DOI] [PubMed] [Google Scholar]
- 41.Phelan JP. Myomas and pregnancy. Obstet Gynecol Clin North Am. 1995;22:801–5. [PubMed] [Google Scholar]
- 42.Parker WH, Fu YS, Berek JS. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet Gynecol. 1994;83:414–8. [PubMed] [Google Scholar]
- 43.Harlow BL, Weiss NS, Lofton S. The epidemiology of sarcomas of the uterus. J Natl Cancer Inst. 1986;76:399–402. [PubMed] [Google Scholar]
- 44.Dubuisson JB, Chapron C, Levy L. Difficulties and complications of laparoscopic myomectomy. J Gynecol Surg. 1996;12:159–65. [Google Scholar]
- 45.DAVIDS AM. Myomectomy: Surgical technique and results in a series of 1150 cases. Am J Obstet Gynecol. 1952;63:592–604. doi: 10.1016/0002-9378(52)90074-4. [DOI] [PubMed] [Google Scholar]
- 46.Brown AB, Chamberline R, TE Linde RW. Myomectomy. Am J Obstet Gynecol. 1956;71:759–63. doi: 10.1016/0002-9378(56)90570-1. [DOI] [PubMed] [Google Scholar]
- 47.Golan D, Aharoni A, Gonen R, Boss Y, Sharf M. Early spontaneous rupture of the post myomectomy gravid uterus. Int J Gynaecol Obstet. 1990;31:167–70. doi: 10.1016/0020-7292(90)90716-x. [DOI] [PubMed] [Google Scholar]
- 48.Dubuisson JB, Chavet X, Chapron C, Gregorakis SS, Morice P. Uterine rupture during pregnancy after laparoscopic myomectomy. Hum Reprod. 1995;10:1475–77. [PubMed] [Google Scholar]
- 49.Harris WJ. Uterine dehiscence following laparoscopic myomectomy. Obstet Gynecol. 1992;80:545–6. [PubMed] [Google Scholar]
- 50.Nezhat Laparoscopically assisted Myomectomy: a comparison of a new technique to myomectomy by laparotomy and laparoscopy. Int J Fertil. 1994;39:39. [PubMed] [Google Scholar]
- 51.Hasson HM, Rotman C, Rana N, Sistos F, Dmowski WP. Laparoscopic myomectomy. Obstet Gynecol. 1992;80:884–8. [PubMed] [Google Scholar]
- 52.Seinera P, Farina C, Todros T. Laparoscopic myomectomy and subsequent pregnancy: results in 54 patients. Hum Reprod. 2000;15:993. doi: 10.1093/humrep/15.9.1993. [DOI] [PubMed] [Google Scholar]
- 53.Dubuisson JB, Chapron C, Chavet X, Gregorakis SS. Fertility after laparoscopic myomectomy of large intramural myomas: preliminary results. Hum Reprod. 1996;11:518–22. doi: 10.1093/humrep/11.3.518. [DOI] [PubMed] [Google Scholar]
- 54.Dubuisson JB, Fauconnier A, Deffarges JV, Norgaard C, Kreiker G, Chapron C. Pregnancy outcome and deliveries following Laparoscopic myomectomy. Hum Reprod. 2000;15:869–73. doi: 10.1093/humrep/15.4.869. [DOI] [PubMed] [Google Scholar]
- 55.Garnet JD. Uterine rupture during pregnancy.An analysis of 133 patients. Obstet Gynecol. 1964;23:898. [PubMed] [Google Scholar]
- 56.Stotland NE, Lipschitz LS, Caughey AB. Delivery strategies for women with a previous classic cesarean delivery: a decision analysis. Am J Obstet Gynecol. 2002;187:1203. doi: 10.1067/mob.2002.127123. [DOI] [PubMed] [Google Scholar]
- 57.Bell SW, Kempson RL, Hendrickson MR. Problematic uterine smooth muscle neoplasms: a clinicopathologic study of 213 cases. Am J Surg Pathol. 1994;18:535–58. [PubMed] [Google Scholar]
- 58.Hart WR. Problematic uterine smooth muscle neoplasms. Am J Surg Pathol. 1997;21:252–5. doi: 10.1097/00000478-199702000-00019. [DOI] [PubMed] [Google Scholar]
- 59.Kempson RL, Bari W. Uterine sarcomas: classification, diagnosis, and prognosis. Hum Pathol. 1970;1:331–49. [PubMed] [Google Scholar]
- 60.Kempson RL, Hendrickson MR. Smooth muscle, endometrial stromal, and mixed mullerian tumors of the uterus. Mod Pathol. 2000;13:328–42. doi: 10.1038/modpathol.3880055. [DOI] [PubMed] [Google Scholar]
- 61.Longacre TA, Hendrickson MR, Kempson RL. Predicting clinical outcome for uterine smooth muscle neoplasms with a reasonable degree of certainty. Adv Anat Pathol. 1997;4:95–104. [Google Scholar]
- 62.Bell SW, Kempson RL, Hendrickson MR. Problematic uterine smooth muscle neoplasms: a clinicopathologic study of 213 cases. Am J Surg Pathol. 1994;18:535–58. [PubMed] [Google Scholar]
- 63.Hendrickson MR, Longarc TA, Kempson RL. The uterine corpus. In: Mills SE, Carter D, Greenson JK, editors. Sternberg's diagnostic surgical pathology. 4th ed. Vol. 2. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 2435–42. [Google Scholar]
- 64.Franquemont DW, Frierson HF, Jr, Mills SE. An immunohistochemical study of normal endometrial stroma and endometrial stromal neoplasms: evidence for smooth muscle differentiation. Am J Surg Pathol. 1991;15:861–70. doi: 10.1097/00000478-199109000-00006. [DOI] [PubMed] [Google Scholar]
- 65.Abell MR, Littler ER. Benign metastasizing uterine leiomyoma: multiple lymph nodal metastases. Cancer. 1975;36:2206–13. doi: 10.1002/cncr.2820360938. [DOI] [PubMed] [Google Scholar]
- 66.Tench WD, Dail D, Gmelich JT. Benign metastasizing leiomyomas: a review of 21 cases. Lab Invest. 1978;38:367. [Google Scholar]
- 67.Esteban JM, Allen WM, Schaerf RH. Benign metastasizing leiomyoma of the uterus: histologic and immunohistochemical characterization of primary and metastatic lesions. Arch Pathol Lab Med. 1999;123:960–2. doi: 10.5858/1999-123-0960-BMLOTU. [DOI] [PubMed] [Google Scholar]
- 68.Tietze L, Günther K, Hörbe A, Pawlik C, Klosterhalfen B, Handt S, et al. Benign metastasizing leiomyoma: a cytogenetically balanced but clonal disease. Hum Pathol. 2000;31:126–8. doi: 10.1016/s0046-8177(00)80210-5. [DOI] [PubMed] [Google Scholar]
- 69.Hilsenbeck SG, Allred DC. Improved methods of estimating mitotic activity in solid tumors. Hum Pathol. 1992;23:601–2. doi: 10.1016/0046-8177(92)90312-q. [DOI] [PubMed] [Google Scholar]
- 70.Kunzel KE, Mills NZ, Muderspach LI, d’Ablaing G., 3rd Myxoid leiomyosarcoma of the uterus. Gynecol Oncol. 1993;48:277–80. doi: 10.1006/gyno.1993.1048. [DOI] [PubMed] [Google Scholar]
- 71.Atkins K, Bell S, Kempson RL. Myxoid smooth muscle neoplasms of the uterus. Mod Pathol. 2001;14:132A. [Google Scholar]
- 72.Mittal K, Demopoulos RI. MIB-1 (Ki-67), p53, estrogen receptor, and progesterone receptor expression in uterine smooth muscle tumors. Hum Pathol. 2001;32:984–7. doi: 10.1053/hupa.2001.27113. [DOI] [PubMed] [Google Scholar]
- 73.Zhai YL, Kobayashi Y, Mori A, Orii A, Nikaido T, Konishi I, et al. Expression of steroid receptors, Ki-67, and p53 in uterine leiomyosarcomas. Int J Gynecol Pathol. 1999;18:20–8. doi: 10.1097/00004347-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 74.Jeffers MD, Oakes SJ, Richmond JA, Macaulay EM. Proliferation, ploidy and prognosis in uterine smooth muscle tumours. Histopathology. 1996;29:217–23. doi: 10.1111/j.1365-2559.1996.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 75.Mayerhofer K, Lozanov P, Bodner K, Bodner-Adler B, Kimberger O, Czerwenka K. Ki-67 expression in patients with uterine leiomyomas, uterine smooth muscle tumors of uncertain malignant potential (STUMP) and uterine leiomyosarcomas (LMS) Acta Obstet Gynecol Scand. 2004;83:1085–8. doi: 10.1111/j.0001-6349.2004.00502.x. [DOI] [PubMed] [Google Scholar]
- 76.Mayerhofer K, Obermair A, Windbichler G, Petru E, Kaider A, Hefler L, et al. Leiomyosarcoma of the uterus: a clinicopathologic multicenter study of 71 cases. Gynecol Oncol. 1999;74:196–201. doi: 10.1006/gyno.1999.5436. [DOI] [PubMed] [Google Scholar]