Abstract
To review the complications associated with laparoscopic surgery and provide clinical direction regarding the best practice based on the best available evidence. The laparoscopic entry techniques and technologies reviewed include the classic pneumoperitoneum (Veress/trocar), the open (Hasson), the direct trocar insertion, the use of disposable shielded trocars, radially expanding trocars and visual entry systems. Medline, Pubmed and Cochrane Databases were searched for English language articles published before December 2008. It is an evidence based fact that minimal access surgery is superior to conventional open surgery since this is beneficial to the women, community and the healthcare system.Over the past 50 years, many techniques, technologies and guidelines have been introduced to eliminate the risks associated with laparoscopic entry. No single technique or instrument has been proved to eliminate laparoscopic entry associated injury. Proper evaluation of the women, supported by surgical skills and good knowledge of the technology and instrumentation is the keystone to safe access and prevention of complications during laparoscopic surgery.
Keywords: Direct trocar, entry, laparoscopy complications, laparoscopy, open access (Hasson) technique, pneumoperitoneum, shielded trocar, veress needle, visual entry system
INTRODUCTION
Laparoscopic surgery has evolved over the past two decades to now be accepted as the method of first choice for tackling most gynaecological problems.
A meta-analysis of 27 randomised controlled trials comparing laparoscopy and laparotomy for benign gynaecological procedures concluded that the risk of minor complications after gynaecological surgery is 40% lower with laparoscopy than with laparotomy, although the risk of major complications is similar.[1]
Access into the abdomen is the one challenge of laparoscopy that is particular to the insertion of surgical instruments through small incisions. Access is associated with injuries to the gastrointestinal tract and major blood vessels and at least 50% of these major complications occur prior to commencement of the intended surgery.[2–3] This complication rate has remained the same during the past 25 years.
Abdominal access and the creation of a pneumoperitoneum in the initial stage of any laparoscopic surgery carry a significant risk of bowel and vascular injuries. These are unique to laparoscopic surgery and are rarely seen in an open surgery.
Increased morbidity and mortality result when surgeons or patients do not recognise injuries early or do not address them quickly.[4] The postoperative rather than intraoperative recognition of these injuries increases the severity of the sequelae as well as the medicolegal liability.
INCIDENCE OF LAPAROSCOPIC ENTRY COMPLICATIONS
In Finland after 70,607 laparoscopic procedures, 256 complications were reported to the national patient insurance association. The overall rate of major complications was 1.4 per 1,000 procedures. This included 0.6 per 1,000 intestinal injuries, 0.3 per 1,000 urological injuries and 0.1 per 1,000 vascular injuries.
In the Netherlands, a multicentric prospective study from 72 hospitals revealed the overall incidence of intestinal injuries and major complications was 5.7 per 1,000 procedures. 70% of these were related to the primary port entry. The overall incidence of laparoscopic entry injuries was 3.3 per 1,000. There were 29 cases of gastrointestinal damage (1.3 per 1,000) and 27 cases of abdominal vessel injuries (1.05 per 1,000).
To minimise entry-related injuries, several techniques, instruments and approaches have been introduced during the last century. These include the Veress-pneumoperitoneum trocar; classic or closed entry,[5] the open (Hasson) technique,[6] direct trocar insertion without prior pneumoperitoneum,[7] use of shielded disposable trocars,[8–9] optical Veress needle,[10,11] optical trocars,[12,13] radially expanding trocars[14,15] and a trocarless reusable, visual access cannula.[16,17] Each of these methods of entry enjoys a certain degree of popularity according to the surgeon's training, experience and bias according to regional and interdisciplinary variability.
COMMON ENTRY COMPLICATIONS DURING LAPAROSCOPIC SURGERY
Studies have suggested that 30-50% of bowel injuries and 13-50% of vascular injuries are undiagnosed at the time of surgery. Since bowel injury is more common than vascular injury, it is more likely to produce serious sequelae because of the delay in diagnosis. The mortality rate from bowel injury is 2.5-5%.[18]
Vascular injuries
Major vascular injury during the initiation of a pneumoperitoneum is a much feared complication of laparoscopic procedures. Vascular injury is a major cause of death from laparoscopy, with a reported mortality rate of 15%. Major vascular injury can occur when the Veress needle is inserted prior to insufflation or when a trocar is inserted after insufflation.
The reason for these injuries is the close proximity of the anterior abdominal wall to the retroperitoneal vascular structures. In thin patients, this distance may be as little as two centimeters. The distal aorta and right common iliac artery are particularly prone to injury. This is not surprising given the fact that the take off of the right common iliac artery lies directly below the umbilicus [Figure 1].
Figure 1.
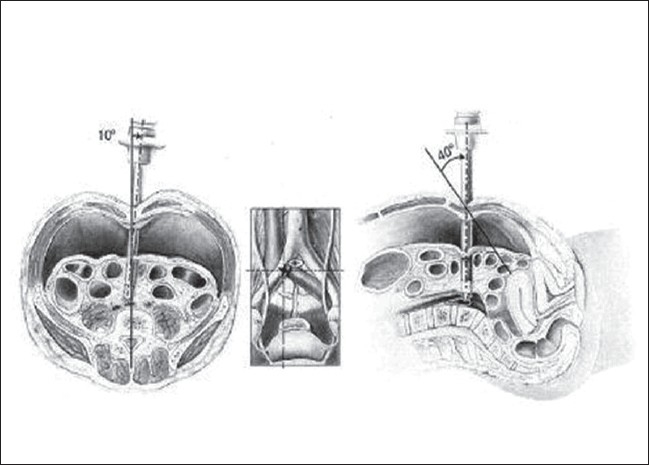
Structures encountered during entry through the umbilicus
Minor vascular injuries are so named since these are injuries to vessels of lesser importance than the aorta, inferior vena cava and iliac vessels. However, these are by no means minor in nature.
The most common minor vascular injury is to the inferior epigastric vessels, occurring in up to 2.5% of laparoscopic hernia repairs. There were 76 cases of minor vascular injuries involving principally the epigastric vessels in a review of 10,837 patients undergoing a hernia repair. These injuries invariably occur during the placement of the secondary cannulas which should be placed under direct vision and with prior transillumination of the abdominal wall. Although injury to the epigastric vessels is still possible if these measures are taken, the incidence should be dramatically reduced [Table 1].
Table 1.
Factors responsible for large vessel injury
Bowel injuries
Bowel injury is the third cause of death from a laparoscopic procedure after major vascular injury and anaesthesia. Unlike major vascular injuries where the risk and presentation are immediate, many bowel injuries go unrecognised at the time of the procedure. Consequently, patients present postoperatively, often after discharge with peritonitis. This delay makes it a significant cause of morbidity and mortality.
A large survey of nearly 37,000 gynaecologic laparoscopies in the US revealed a 0.16% incidence of bowel injury. 39.8% of vascular and intestinal injuries were caused by the Veress needle, 37.9% by insertion of the primary trocar and 22% by the insertion of the secondary trocar.
Urological injuries
Unlike vascular or bowel injuries, urological injuries are mostly related to the gynaecological procedure being performed and not to entry alone. The incidence of bladder injury during laparoscopic hysterectomy ranges from 0.02-8.3%.[19] Harkki-Siren noted urinary tract injuries in 2.5 per 1,000 laparoscopies, the majority occurring during laparoscopic hysterectomies.[20]
Ureteric injuries occur in approximately 1% of cases. These are more common in complex surgical procedures such as hysterectomy, urinary stress incontinence and/or genital prolapse procedures and severe endometriosis resection.
CARBON DIOXIDE GAS EMBOLISM
The incidence of carbon dioxide embolism was 0.001% in a review of 489,335 closed laparoscopies. Several case reports have detailed fatal or near-fatal coronary, cerebral or other gas embolism.[21] Such a complication has not been reported at open laparoscopy.
SUGGESTED STEPS FOR SAFE ENTRY
Classic entry technique and Veress needle safety tests
Blind Veress needle insertion and insufflation followed by blind trocar insertion is the technique most widely used. One third to one half of major intra-abdominal vascular and intestinal injuries occurs from the Veress needle itself.
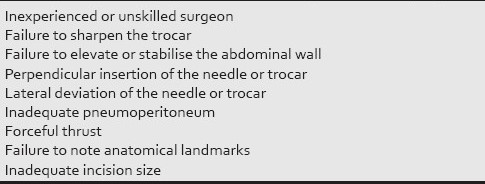
Important procedural steps during insertion of the Veress needle are [Figure 2]:
Figure 2.
Veress entry technique and intra-abdominal pressure
The following tests should be done to confirm the presence of the needle in the peritoneum and not in a visceral organ.
Manometer test – involves connecting the gas tubing to the Veress needle and raising the abdominal wall to create negative pressure.
Hissing sound test – involves turning the valve to the off position after it has been properly positioned. The abdomen is elevated and the valve opened, creating a hissing sound.
Aspiration test – involves attaching a syringe filled with saline to the Veress needle and attempting to aspirate any material. If material is aspirated such as bowel contents or urine, the Veress needle should be removed. If blood is aspirated, the needle is left in place and preparation for exploratory laparotomy is made for a presumed vascular injury.
If no material is aspirated, 5 mL of saline is inserted and a reattempt to aspirate is made. If no fluid can be aspirated, entry into the peritoneal cavity is confirmed. If the saline is aspirated, an enclosed space was probably entered such as the preperitoneal space and the needle should be repositioned.
Hanging drop test – involves placing a drop of water on the open end of the Veress needle and the abdominal wall is elevated. If the needle is correctly positioned, the water should disappear down the shaft. Until confirmation of proper position of the needle, insufflation should be low at a rate of 1 L/min.
Finally, the needle is attached to an insufflator that measures the pressure at the tip. The pressure will be low (5 mm Hg) if it is appropriately placed. Insufflation to 12-15 mm Hg with carbon dioxide gas follows.
Once this pressure is achieved, a 10 mm trocar with or without a safety shield is placed blindly into the abdomen. It must be emphasized that a full pneumoperitoneum should be established prior to insertion of the blind umbilical trocar. Once again, care must be taken to elevate and stabilise the abdominal wall and to ensure that the trocar is inserted in the midline safely.
Value of safety tests
Although these tests and techniques may be helpful in accessing the peritoneal cavity, the fact that visceral and vascular injuries occur shows that they are not foolproof. A recent retrospective study evaluating the double click sound test, aspiration test, hanging drop of saline test and the syringe test concluded that none of these tests is confirmatory for the intraperitoneal placement of the Veress needle and concluded that the most valuable test is to observe the actual insufflation pressure to be 8 mm or less and that the gas is flowing freely.[22]
Some surgeons waggle the needle from side to side, believing that this shakes an attached organ from the tip of the needle and confirms correct intra-abdominal placement. However, this manoeuvre can enlarge a 1.6 mm puncture injury to an injury of up to 1 cm in viscera or blood vessels.[23]
Veress intraperitoneal pressure
Prospective studies have concluded that initial intra-abdominal pressures of 10 mm Hg or below indicate correct placement of the Veress needle, regardless of the woman's body habitus, parity or age.[24] A recent study has confirmed that the initial intraperitoneal insufflation pressure (less than and equal to 10 mm Hg) correlates positively with the patient's weight and BMI and negatively with parity.[25]
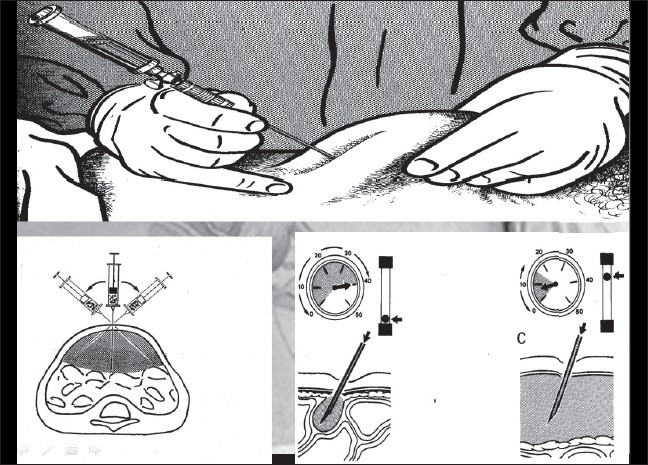
Angle of Veress needle insertion
Hurd et al. reported on CT scans of 38 unanaesthetised women of reproductive age that the position of the umbilicus was found, on average, 0.4 cm, 2.4 cm and 2.9 cm caudal to the aortic bifurcation in normal weight (BMI < 25 kg/m2), overweight (BMI 25-30 kg/m2) and obese (BMI >30 kg/m2) women respectively. In all cases, the umbilicus was cephalad to where the left common iliac vein crossed the midline at the sacral promontory. Therefore, the angle of Veress needle insertion should vary accordingly from 45 degrees in non-obese women to 90 degrees in very obese women [Figure 3].[26]
Figure 3.

Angulation of Veress’ needle in obese patients
Number of insertion attempts
Studies have reported placing the Veress needle into the peritoneal cavity on the first attempt at frequencies of 85.5-86.9%; two attempts required in 8.5-11.6%, three attempts in 2.6-3.0% and more than three attempts in 0.3-1.6%.
Complication rates associated are: one attempt 0.8-16.3%, two attempts 16.31-37.5%, three attempts 44.4-64% and more than three attempts 84.6-100%. The complications associated were extraperitoneal insufflation, omental and bowel injuries and failed laparoscopy.[27]
Adequate pneumoperitoneum
Controversy exists regarding what constitutes an “adequate” pneumoperitoneum prior to insertion of the primary trocar. Traditionally it has been defined as achieving a volume of 1-4 litres depending on the BMI and parity of the patient. This is usually achieved by an intra-peritoneal pressure of 10-15 mm Hg.
It has been shown that achieving a high intraperitoneal pressure (HIP) entry ranging from 20-25 mm Hg increases the gas bubble and produces greater splinting of the anterior abdominal wall and maintains a distance of at least four centimeters from the abdominal contents. It also increases the distance between the umbilicus and bifurcation of the aorta from 0.6 cm (at pressure of 12 mm Hg) to 5.9 cm.[28]
HIP entry thus allows easy entry of the primary trocar and minimises the risk of vascular injury. It does not adversely affect cardiopulmonary function in healthy women.
ALTERNATIVE VERESS NEEDLE INSERTION SITES
Left upper quadrant (LUQ, palmer's point)
In patients with a previous laparotomy, Palmer advocated insertion of the Veress needle three centimeters below the left subcostal border in the midclavicular line.[29] This may be considered in the obese as well as in the very thin patient. The stomach should be emptied by nasogastric suction and the needle should be introduced perpendicular to the skin. Patients with previous splenic or gastric surgery, portal hypertension or significant gastropancreatic masses should be excluded.
Transuterine and trans cul-de-sac
Using a long Veress needle, pneumoperitoneum has been established through the fundus of the uterus transvaginally.[30] This has especially been helpful in obese women.[31] The posterior vaginal fornix has been reported as another site through which to establish pneumoperitoneum, especially in obese women.[32]
However, these two sites are not routinely recommended as they carry the risk of sepsis and the risk of perforation of the rectum in the presence of pelvic inflammatory disease or severe endometriosis.
9th or 10th intercostal space
The Veress needle is inserted directly through the intercostals space at the anterior axillary line along the superior surface of the lower rib to avoid injury to the underlying neurovascular bundle.[33]
ALTERNATIVE MEANS OF ENTRY
Open laparoscopy
In general, trocar injuries to abdominal viscera occur a) when the viscera are unusually close to the point of trocar insertion or b) where the trocar penetrates too far into the abdominal cavity as it is inserted. The former can be anticipated when the patient has undergone a surgery previously. The best method of avoiding visceral injury in this case is to use the open Hasson technique or if the closed technique is used to place the first trocar at a site remote from the previous incision.
The concept in the open technique [Figure 4] is to create a tiny incision, directly incise the layers of the abdominal wall, directly cut the peritoneum and enter the abdomen. Since gas can escape around the incision, an olive is placed over the end of the trocar to occlude the incision and sutures are placed on the abdominal fascia and attached to the cannula.
Figure 4.
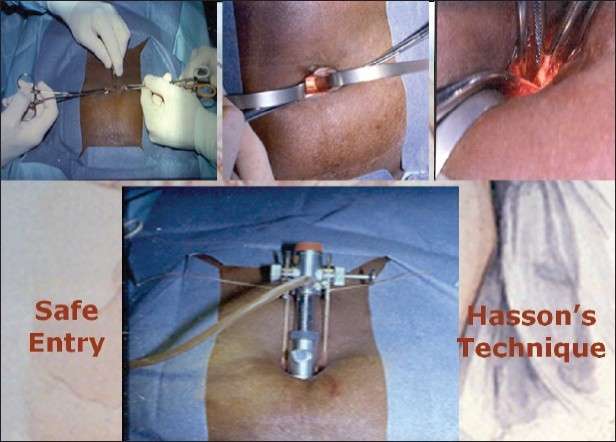
Hasson's technique
The proposed advantages for the open technique are avoidance of blind puncture with a needle and subsequent trocar, certainty of establishing a pneumoperitoneum and correct anatomical repair of the abdominal wall incision.
Widespread use of this technique has been limited to women with previous lower abdominal surgery, pregnant women, children and very thin women where little space exists between the abdominal wall and the spine. Reasons for limiting the use of the open technique include greater time needed for performance, difficulty with the technique, obese patients and difficulty in maintenance of the pneumoperitoneum.
There are considerably fewer reports of bowel and major vascular injury in the literature using this technique than the Veress needle technique. Penfield noted a 0.06% incidence of bowel injury but the injuries were mostly partial and were recognised immediately because of the proximity of the bowel to the wound.
Hasson presented his review of 5,284 women who had open laparoscopies and developed complications related to primary access. 21 had minor wound infections, four had minor haematomas, one developed an umbilical hernia that required surgery and one had an inadvertent injury to the small bowel that was repaired intraoperatively without adverse outcome. Access to the abdominal cavity was generally secured within three to ten minutes.[34]
A meta-analysis of 760,890 closed laparoscopy and 22,465 open laparoscopy cases reported the incidence of vascular injury rate in closed laparoscopy was 0.44% compared with 0% in open laparoscopy. The incidence of bowel injury was 0.7% compared with 0.5% respectively. The authors concluded that the open (Hasson) technique eliminates the risk of vascular injury and gas embolism and reduces the risk of bowel injury and recommend the open technique to be adopted for primary laparoscopic entry.
Direct trocar entry
Dingfelder in 1978 was the first to advocate this technique in which where the abdomen is entered with a trocar without prior Veress needle entry and pneumoinsufflation. The advantages of this method are the avoidance of complications related to the use of the Veress needle: failed pneumoperitoneum, preperitoneal insufflation, intestinal insufflation and CO2 embolism.
The direct entry method is faster than any other method of entry but is the least performed laparoscopic technique in clinical practice.
In the United States, a review of 51 publications including 21,547 open technique, 16,739 direct entry technique and 134,917 Veress/trocar reported entry related bowel injuries: 0.11% (open), 0.05% (direct entry) and 0.04% (Veress/trocar). Vascular injury rates were 0.01%, 0% and 0.04% respectively.[35]
Disposable shielded trocars
These are designed with a shield that partially retracts and exposes a sharp tip as it encounters resistance through the abdominal wall. As the shield enters the abdominal cavity, it springs forward and covers the sharp tip of the trocar.
However, there is a brief moment when the sharp trocar tip is exposed and unprotected as it enters the abdominal cavity.[36]
RADIALLY EXPANDING ACCESS SYSTEM
These are not recommended as being superior to traditional trocars. They have blunt tips that may provide some protection from injuries by the force required for entry is significantly greater than with disposable trocars.
Optical trocar/Visual entry systems
The optical trocar allows visualisation of the layers of the abdominal wall on the monitor and these are cut under vision by advancement of the edge of the cannula which is surgically sharp or conical. This allows the surgeon to advance through the layers to the peritoneum in a clear area where there is no bowel. Jirecek et al. reviewed 1500 patients in whom no major complications were observed in the Optiview insertion group as compared to the group undergoing blind insertion.
Challenging situations
Previous abdominal surgery
This group of patients clearly represents a risk factor for adhesion formation. Brill et al. studied 360 women undergoing operative laparoscopy after a previous laparotomy. Patients with prior midline incisions had significantly more adhesions (58 of 102) than those with Pfannenstiel incisions (70 of 258). 28% (21 patients) suffered direct injury to the adherent omentum and bowel during the laparoscopic procedure.
Adhesions may be right under a scar or may be further away. Some investigators have recommended a preoperative sonographic mapping of adhesions to help determine a safe site for trocar insertion. A midline incision clearly presents a high risk for bowel adhesions under a planned umbilical trocar site; however, even scars away from the umbilicus can lead to adhesions at the umbilical site.
Alternative sites may be used for access with open or blind access techniques. One advantage of placing the first port in a site away from previous scars is the improved ability to see the abdominal cavity because vision is not obscured by adhesions. This allows for better assessment of location of remaining ports. Also, there is appropriate working distance necessary for manipulating the instruments.
Obesity
The most major technical problem in this group of patients is access to the abdominal cavity, which is especially difficult with the needle insertion technique. Owing to the thickness of the abdominal wall and the preperitoneal fat, accurate assessment of the location of the needle tip is difficult, making preperitoneal insufflation common.
The umbilicus is the thinnest area of the abdominal wall and needle insertion at this point is the easiest. The saline drop test and confirmation of an initial low intra-abdominal pressure are crucial in confirming proper intra-abdominal placement.
Another alternative is the use of the open insertion technique with a Hasson trocar. Controversy exists over the advantages and disadvantages of this access technique compared with a closed technique in obese patients. Some investigators believe that a large skin incision is necessary for Hasson trocar insertion in obese patients, leading to preoperative leakage of gas and to increased rates of wound infection postoperatively.
Studies suggest that the use of optical trocars may be beneficial and may reduce the unacceptable risk of vascular and bowel injury in this group of women.
Large pelvic mass
In this group of women, selecting an alternative supraumbilical site for primary entry will allow the greatest freedom of movement for manipulation of instruments as well as offer greater safety vis-à-vis damage to the pelvic mass e.g. fibroid, ovarian tumour or pregnancy.
RECOMMENDATIONS
The patient must be properly evaluated, including a full clinical history and thorough clinical examination and relevant investigations.
Clear explanations must be offered and information given regarding the associated risks and potential complications associated with laparoscopic surgery and the possibility of conversion to laparotomy if the clinical circumstances so dictate.
The surgeon must have adequate training and experience in laparoscopic surgery before intending to perform any procedure independently. He should be familiar with the equipment and instruments he intends to use.
There is no single safe technique that reduces laparoscopic surgery entry complications in low risk patients. The surgeon should select the technique which he feels most comfortable with. It is recommended that the HIP entry be used to optimise the insertion of the primary trocar and cannula.
The open (Hasson) technique and Palmer's point pneumoperitoneum should be considered in the obese patient and those with suspected peri-umbilical adhesions.
The different Veress needle safety tests are not sensitive indicators for the correct placement of the Veress needle. The most confirmatory test is to observe that the actual intra-peritoneal pressure is below 8 mm Hg and gas is flowing freely. Excessive movement of the needle should be avoided as this will convert a tiny puncture to vessel or bowel from 1.6 mm to 1 cm diameter.
The distension pressure should be reduced to 12-14 mm Hg once the insertion of the trocar is complete to avoid cardiopulmonary complications and gas embolism.
After introduction of the telescope, the bowel should be inspected for obvious injury and abdomen visualised for presence of adherent bowel around the umbilicus.
CONCLUSIONS
The only surgeon who does not encounter complications is one who is not operating. All procedures have their risks. Complications can occur even in the best of hands and it is vital that these are recognised promptly and immediately addressed.
The importance of proper training and the value of experience is clear. It must be our goal to train our future laparoscopic surgeons in the necessary skills and encourage the development of specially designed fellowships for those performing the most advanced procedures.
When complications do occur, excellent training and experience will allow these to be managed by laparoscopy.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Chapron C, Fauconnier A, Goffinet F, Bréart G, Dubuisson JB. Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynecologic pathology: results of a meta-analysis. Hum Reprod. 2002;17:1334–42. doi: 10.1093/humrep/17.5.1334. [DOI] [PubMed] [Google Scholar]
- 2.Jansen FW, Kapiteyn K, Trimbos-Kemper T, Hermans J, Trimbos JB. Complications of laparoscopy: a prospective multicentre observational study. Br J Obstet Gynaecol. 1997;104:595–600. doi: 10.1111/j.1471-0528.1997.tb11539.x. [DOI] [PubMed] [Google Scholar]
- 3.Jansen FW, Kolkman W, Bakkum EA, de Kroon CD, Trimbos-Kemper TC, Trimbos JB. Complications of laparoscopy:an inquiry about closed versus open-entry technique. Am J Obstet Gynecol. 2004;190:634–8. doi: 10.1016/j.ajog.2003.09.035. [DOI] [PubMed] [Google Scholar]
- 4.Fuller J, Scott W, Ashar B, Corrado J. Laparoscopic trocar injuries: a report from a US FDA Center for Devices and Radiological Health (CDRH) Systematic Technology Assessment of Medical Products (STAMP) Committee. 2005 Aug 25;:1–14. [Google Scholar]
- 5.Palmer R. Safety in laparoscopy. J Reprod Med. 1974;13:1–5. [PubMed] [Google Scholar]
- 6.Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971;110:886–7. doi: 10.1016/0002-9378(71)90593-x. [DOI] [PubMed] [Google Scholar]
- 7.Dingfelder JR. Direct laparoscope trocar insertion without prior pneumoperitoneum. J Reprod Med. 1978;21:45–7. [PubMed] [Google Scholar]
- 8.Byron JW, Fujiyoshi CA, Miyazawa K. Evaluation of the direct trocar insertion technique at laparoscopy. Obstet Gynecol. 1989;74:423–5. [PubMed] [Google Scholar]
- 9.Lanvin D, Elhage A, Querleu D. Does the use of pneumoperitoneum and disposable trocars prevent bowel injury at laparoscopy.A randomised experimental study in the rabbit? Gynaecol Endosc. 1996;5:343–8. [Google Scholar]
- 10.Riek S, Bachmann KH, Gaiselmann T, Hoernstein F, Marzusch K. A new insufflation needle with a special optical system for use in laparoscopic procedures. Obstet Gynecol. 1994;84:476–8. [PubMed] [Google Scholar]
- 11.McGurgan P, O’Donovan P. Optical Veress as an entry technique. Gynaecol Endosc. 1999;8:379–92. [Google Scholar]
- 12.Kaali SG. Introduction of the Opti-Trocar. J Am Assoc Gynecol Laparosc. 1993;1:50–3. doi: 10.1016/s1074-3804(05)80758-3. [DOI] [PubMed] [Google Scholar]
- 13.Mettler I, Schmidt EH, Frank V, Semm K. Optical trocar systems: laparoscopic entry and its complications ( a study of case in Germany) Gynaecol Endosc. 1999;8:383–9. [Google Scholar]
- 14.Turner DJ. A new radially expanding access system for laparoscopic procedures versus conventional cannulas. J Am Assoc Gynecol Laparosc. 1996;34:609–15. doi: 10.1016/s1074-3804(05)80175-6. [DOI] [PubMed] [Google Scholar]
- 15.Turner DJ. Making the case for the radially expanding access system. Gynaecol Endosc. 1999:8391–5. [Google Scholar]
- 16.Ternamian AM. Laparoscopy without trocars. Surg Endosc. 1997;11:8159–68. doi: 10.1007/s004649900461. [DOI] [PubMed] [Google Scholar]
- 17.Ternamian AM. A second generation laparoscopic port system: EndoTIP. Gynaecol Endosc. 1999;8:397–401. [Google Scholar]
- 18.Chandler JG, Corson SL, Way LW. Three spectra of laparoscopic entry access injuries. J Am Coll Surg. 2001;192:478–91. doi: 10.1016/s1072-7515(01)00820-1. [DOI] [PubMed] [Google Scholar]
- 19.Ostrzenski A, Ostrzenska KM. Bladder injury during laparoscopic surgery. Obstet Gynecol. 1986;53:175–80. doi: 10.1097/00006254-199803000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Härkki-Siren P, Sjöberg J, Kurki T. Major complications of laparoscopy: A follow-up Finnish study. Obstet Gynecol. 1999;94:94–8. [PubMed] [Google Scholar]
- 21.Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, et al. The European Association for Surgery Clinical Practice Guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16:1121–43. doi: 10.1007/s00464-001-9166-7. [DOI] [PubMed] [Google Scholar]
- 22.Teoh B, Sen R, Abbott J. An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. J Minim Invasive Gynecol. 2005;12:153–8. doi: 10.1016/j.jmig.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Brosens I, Gordon A. Bowel injuries during gynaecological laparoscopy: a multinational survey. Gynaecol Endosc. 2001;10:141–5. [Google Scholar]
- 24.Vilos GA, Vilos AG. Safe laparoscopic entry guided by Veress needle CO2 insufflation pressure. J Am Assoc Gynecol Laparosc. 2003;10:415–20. [PubMed] [Google Scholar]
- 25.Vilos AG, Vilos GA, Abu-Rafea B, Hollett-Caines J, Al-Omran M. Effect of body habitus and parity on the initial Veress intraperitoneal (VIP) CO2 insufflation pressure during laparoscopic access in women. J Minim Invasive Gynecol. 2006;13:108–13. doi: 10.1016/j.jmig.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Hurd WW, Bude RO, DeLancey JO, Pearl ML. The relationship of the umbilicus to the aortic bifurcation: complications for laparoscopic technique. Obstet Gynecol. 1992;80:48–51. [PubMed] [Google Scholar]
- 27.Richardson RF, Sutton CJG. Complications of first entry: a prospective laparoscopic audit. Gynaecol Endosc. 1999;8:327–34. [Google Scholar]
- 28.Phillips G, Garry R, Kumar C, Reich H. How much gas is required for initial insufflation at laparoscopy? Gynaecol Endosc. 1999;8:369–74. [Google Scholar]
- 29.Palmer R. Safety in laparoscopy. J Reprod Med. 1974;13:1–5. [PubMed] [Google Scholar]
- 30.Sanders RR, Filshie GM. Transfundal induction of pneumoperitoneum prior to laparoscopy. J Obstet Gynaecol Br Commonw. 1994;107:316–7. doi: 10.1111/j.1471-0528.1974.tb00390.x. [DOI] [PubMed] [Google Scholar]
- 31.Wolfe WM, Pasic R. Transuterine insertion of Veress needle in laparoscopy. Obstet Gynecol. 1990;75:456–7. [PubMed] [Google Scholar]
- 32.van Lith DA, van Schie KJ, Beekhuizen W, du Plessis M. Cul-de-sac insufflation:an easy alternative route for safely inducing pneumoperitoneum. Int J Gynaecol Obstet. 1980;17:357–8. doi: 10.1002/j.1879-3479.1980.tb00304.x. [DOI] [PubMed] [Google Scholar]
- 33.Lam KW, Pun TC. Left upper quadrant approach in gynecologic laparoscopic surgery with reusable instruments. J Am Assoc Gynecol Laparosc. 2002;9:199–203. doi: 10.1016/s1074-3804(05)60132-6. [DOI] [PubMed] [Google Scholar]
- 34.Hasson HM. Open laparoscopy as a method of access in laparoscopic surgery. Gynaecol Endosc. 1999;8:353–62. [Google Scholar]
- 35.Molloy D, Kaloo PD, Cooper M, Nguyen TV. Laparoscopic entry: A literature review and analysis of techniques and complications of primary port entry. Aust N Z J Obstet Gynaecol. 2002;42:246–54. doi: 10.1111/j.0004-8666.2002.00246.x. [DOI] [PubMed] [Google Scholar]
- 36.Trocars: safety and selection. Emergency Care Research Institute. Health Devices. 1998;27:376–98. [PubMed] [Google Scholar]


