Abstract
Although there are many studies the ongoing debate on the management of posthysterectomy vault prolapse whether it should be abdominal, vaginal, or laparoscopic still continues. However there is no clear consensus. Though the incidence of vaginal vault prolapse is said to range from 0.2 to 45%, the choice of the optimal treatment depends on the surgeon's experience, suitability for surgery, age, symptoms, quality of life impairment, and prolapse grade. Abdominal sacrocopopexy (ASCP) with mesh interposition is the traditional surgical procedure for treating pelvic organ prolapse and has been shown to have one of the highest long-term success rates for vaginal vault prolapse. The laparoscopic approach offers reduced morbidity, shorter hospitalization, and decreased post operative pain. The disadvantages of the laparoscopic approach include longer operating time and need for advanced laparoscopic surgical skills including suturing. Robot-assisted laparoscopic procedure allows the performance of complex laparoscopic maneuvers with less difficulty, and thereby simplifies the complex procedure. The aim is to describe and demonstrate the use and benefit of robot-assisted laparoscopic sacrocolpopexy in the treatment of posthysterectomy vaginal vault prolapse in obese patients along with mid-urethral sling application.
Keywords: Mid-urethral sling, obese women, robotic sacrocolpopexy
INTRODUCTION
Although there are many studies the ongoing debate on the management of posthysterectomy vault prolapse whether it should be abdominal, vaginal, or laparoscopic still continues. However there is no clear consensus. Though the incidence of vaginal vault prolapse is said to range from 0.2 to 45%, the choice of the optimal treatment depends on the surgeon's experience, suitability for surgery, age, symptoms, quality of life impairment, and prolapse grade.
As a visiting clinician in Mayo Clinic, Scottsdale, Arizona, watching those fabulous gynecological surgeries with robotic technology, I wondered when would India be ready for a robot. As I googled to write this article, I was surprised to know that India already has 6 robots in different centers used by different specialties. Urologists are the front runners in using robotics but gynecologists are taking the cue.
Robotic technology has given the US gynecological surgeons a definite advantage over the surgeons of other countries.
Being first trained in open gynecological surgeries at Andhra Medical College and King George Hospital - a premier Medical Institute in India - and then in Laparoscopic procedures in University of Schelswitz, Kiel, Germany, and now being here for learning robotic technology, this experience has given me a unique insight into the technology. The rapid dissemination of the emerging new concepts, and technology with evidence-based medicine have positively altered the fundamental foundations of gynecological surgeries be it be in Oncology or Urogynecology with superior outcomes to Laparoscopy and Open methods. One such surgery with a new technique is Robotic sacrocolpopexy with mid-urethral sling application.
Abdominal sacrocopopexy (ASCP) with mesh interposition is the traditional surgical procedure for treating pelvic organ prolapsed and has been shown to have very high long-term success rates for vaginal vault prolapse.[1] The laparoscopic approach offers reduced morbidity, shorter hospitalization, and decreased postoperative pain. The disadvantages of the laparoscopic approach include longer operating time and need for advanced laparoscopic surgical skills including suturing. The new robot-assisted laparoscopic procedure allows the performance of complex laparoscopic maneuvers with less difficulty, and thereby simplifies the complex procedure.[2]
The aim of presenting this paper as a case report is to introduce the new technology to the readers as an important promising tool in the surgical armamentarium. The new robotic procedure tends to minimize blood loss, cuts hospital stay, and also offers advantages of faster post-op recovery, decreased pain, and improved quality of life
The case report describes and demonstrates the use and benefit of robot-assisted laparoscopic sacrocolpopexy in the treatment of posthysterectomy vaginal vault prolapse in obese patients along with mid-urethral sling application.
The department of Urogynecology, Mayo clinic, AZ, has come across a morbidly obese patient with vault prolapse and SUI. We managed this patient with transabdominal robot-assisted sacrocolpopexy and mid-urethral (Align Mesh) slings with the robotic technique which combines the advantages of open sacrocolpopexy with the decreased morbidity and improved cosmesis of laparoscopic surgery.
The objective of this case report is to present the feasibility of robot-assisted sacrocolpopexy in morbidly obese patients, and to describe the minimally invasive surgical technique of vault prolapse, sacrocolpopexy through the Da Vinci robotic surgical system, and the application of mid-urethral sling.
CASE
A 50-year-old morbidly obese, para 2 with BMI 39 kg/m2 made a self-referral to us, when she noticed a vaginal bulge in the last two months, primarily with wiping. The patient had hysterectomy in 1998, and also had her bladder “lifted” at that time. She did not recall any meshes used at that time. She had admitted to stress incontinence and also leakage with urgency. She uses a pad on a daily basis and also complained of nocturia. She denied any frequent urinary tract infections, vaginal bleeding. She also stated that her intercourse is uncomfortable because of the bulge and she also noticed a more loss of urine during intercourse as well.
Her past medical history revealed morbid obesity, hyperlipidemia, and asthma. Her past surgical history included tonsillectomy (1966), anterior cruciate ligament at right knee replaced (1998), a bladder lift, and hysterectomy (1998) as described.
Her social history states that she was married and had two vaginal deliveries. She was not a smoker or an alcoholic.
Her vitals were stable and physical examination showed a morbidly large abdomen and no palpable organomegaly. The bladder neck appeared to be well supported, and no actual leakage was noted with Valsalva. She had grade 2-3 cystocele, grade 2 apical descensus, grade 3-4 rectocele. Bimanual examination was negative. Pelvic side walls were smooth.
This patient was advised about pelvic floor strengthening exercises and weight loss. The options of a pessary versus surgical intervention with sacrocolpopexy approached robotically was also discussed. A lengthy discussion regarding the risks and benefits of all of the above was done with her and she was sent back home.
The patient returned to us after 5 months, with significant weight loss up to 35 pounds. She decided to go ahead with the surgery as she has been feeling her bulge more with her increased activity and also difficulty has pronounced with intercourse. Her pelvic examination is unchanged from the last visit. She had also been advised of urodynamics. Because of her obesity we decided to go ahead with robotic sacrocolpopexy and possible sling procedure. She was advised to start with an estrogen cream.
Procedure
The procedure included the following processes: robotic sacrocolpopexy, adhesiolysis, retropubic mid-urethral sling using the align retropubic urethral sling.
Description of the procedure
Under general anesthesia the patient was placed in the dorsal lithotomy position using the Welch-Allyn stirrups. Abdomen, perineum, and vagina were then prepped and draped. Using the open Hasson technique the abdomen was entered.
Some adhesions were noted from the bowel to the pelvic sidewall. These were lysed. The presacral dissection was initiated identifying the pertinent anatomy and sacral promontery, opening the peritoneum overlying the promontory. The peritoneum was then incised down to the vaginal apex. The peritoneum was taken off the bladder and dissected at least 4 cm inferior to the urethral meatus. The rectovaginal septum was developed all the way down to the perineal body. The graft is robotically attached to the anterior and posterior vaginal wall with 5-6 sutures. The 30° lens and vaginal retractor maximize exposure for precise placement of the sutures in the vaginal muscularis. The posterior sutures should be placed first, because they are more difficult, followed by suturing the anterior portion of the Y-graft. Standard full-thickness bites through the vagina are usually used to allow for maximal strength of the repair. The full-thickness bites used are identical to those placed during traditional transabdominal sacrocolpopexy. The anterior and the posterior aspects of the mesh were attached in at least 5-6 points. The tail of the Y segment was attached to the sacrum at two points using 2-0 Gore-Tex. Reperitonealization was then performed using 2-0 Monocryl. Intraoperative cystoscopy confirmed no inadvertent bladder injuries, ureteral efflux bilaterally, and no stitches within the bladder.
The mid-urethral sling was then placed under no tension and without any difficulties. We used The Align R (Retropubic) Urethral support system which is a mesh-like tape that is surgically inserted through the vagina to support the bladder neck and urethra. For obese women with SUI, a weakened pelvic muscle floor or a defect in the urethral fascia cannot support the urethra in its correct position and this system is very helpful. A small 1 cm vaginal incision was made at mid-urethra. Dissection is carried laterally at 45° toward the contralateral shoulder with long curved scissors. An introducer needle was guided into the space of Retzius and rectus sheath and muscle were perforated. The introducer needle was grasped through the abdominal incision until the green guide tube is visualized through the abdominal incision. The same procedure was repeated on the other side with second introducer. At this point a cystoscopy was performed to confirm bladder integrity. A blunt instrument like an artery forceps was placed between the urethra and mesh while positioning the sling. When appropriate tension is attained the mesh was exposed by removing the sheath. The mid-urethral sling is then placed under no tension and without any difficulties. The exposed mesh strips are cut at the level of subcutaneous tissue and skin incision is closed. Intraoperative cystoscopy confirmed no inadvertent bladder injuries. The patient tolerated the entire procedure well [Figures 1–2]. The total console time was 1 hour, 18 minutes, and blood loss was minimal.
Figure 1.
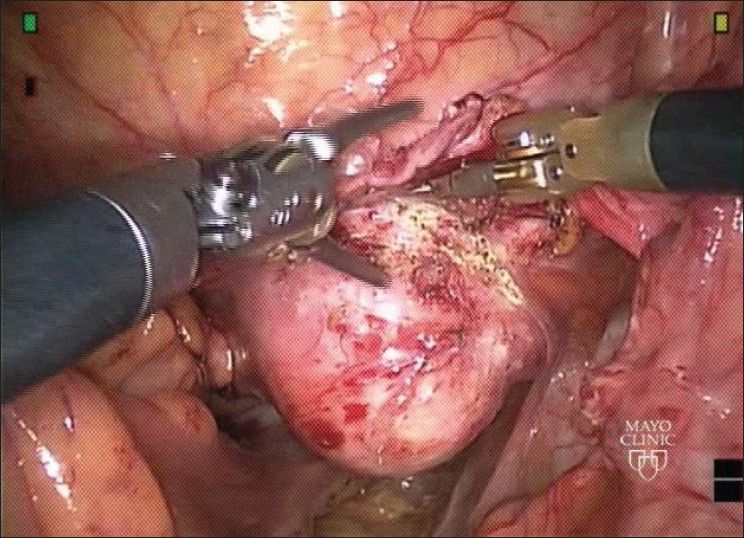
Anterior dissection
Figure 2.
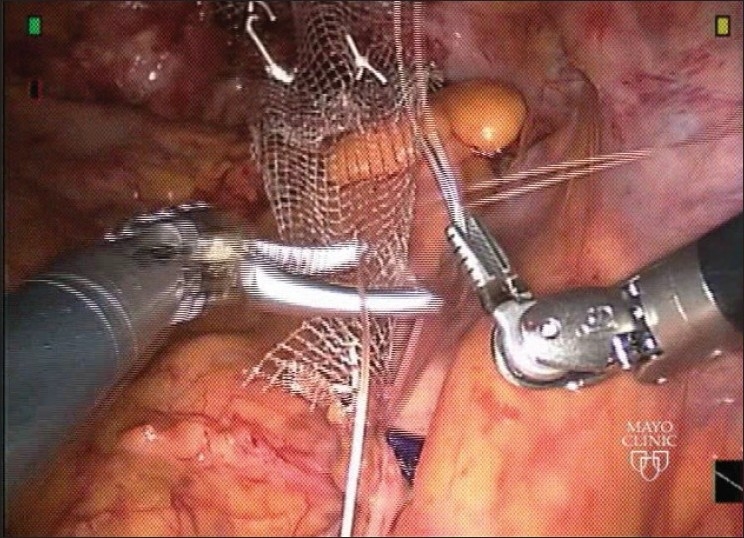
Mesh attachment
The patient was kept for 4 hours in the hospital and sent home. The next morning we scheduled a telephone call with her and found out her to be doing very well.
DISCUSSION
The lifetime chance of developing a vault prolapse after hysterectomy done due to other conditions is 1-8%, whereas that of developing a vault prolapse after hysterectomy due to uterine prolapse is reported to be 11.6%.[3] The highest risk for undergoing surgical treatment for pelvic organ disorders is 50-79 years of age. In a developing country like India morbid obesity has reached epidemic proportions in the 21st century. India is following a trend of other developing countries whose people are steadily becoming more obese. Unhealthy, processed food, genetical susceptibility to weight accumulation especially around the waist, urbanization, and modernization have all been associated with obesity.[4]
Obese women are more likely to have both SUI and pelvic organ prolapse (POP). Studies suggest that surgery holds more risks for obese people, and may influence surgical effectiveness because of the longer operating times and difficult maneuvers. But they also state with mixed results that in obese women undergoing pelvic floor disorder surgeries, through robot-assisted technology, though operative times are longer, complications are not uncommon.
In the past 10 years there has been significant evolution in the treatment of SUI and POP. The laparoscopic retropubic urethropexy was first introduced in 1991[5] but was abandoned because of several small studies reporting lower cure rates. The next major stride in minimally invasive treatment of SUI occurred in 1996 with the introduction of the tension-free vaginal tape (TVT).[6] This sling has been a significant impetus for the development of the vaginal mesh “kits” that are now available for treatment of SUI and POP. Attributable in great part to the simplicity of these techniques, the number of pelvic reconstructive cases performed per annum has increased significantly over the past decade.
In an effort to incorporate minimally invasive techniques in POP treatment, laparoscopic and robotic approaches have been applied to several transabdominal surgical techniques. The often-cited advantages of laparoscopic and robotic surgery include improved visualization because of magnification and insufflation, better cosmesis and hemostasis, shorter hospital stay, and less postoperative pain with an overall more rapid recovery relative to corresponding open approaches. The disadvantages of minimally invasive techniques are the long “learning curve,” the potentially increased difficulty of the retroperitoneal dissection, and the potential increase in hospital costs. It is likely that with the increased application of robotics and laparoscopy, the learning curve is eventually likely to become a less significant barrier [Figure 3].[7]
Figure 3.
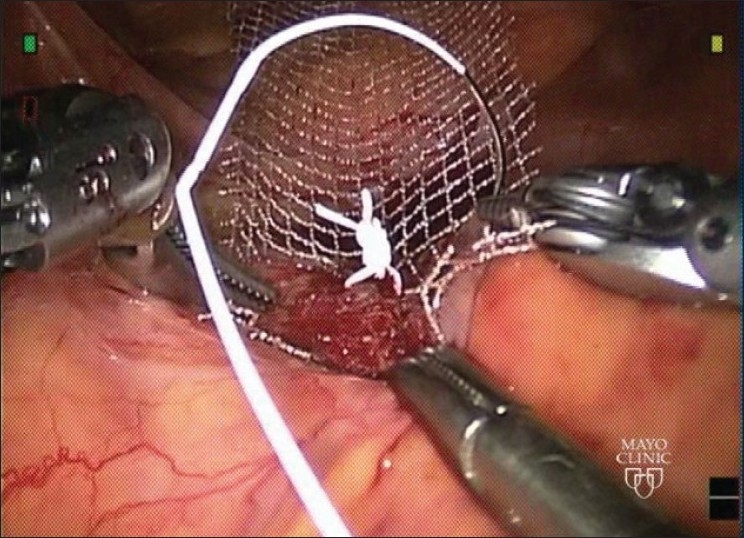
Retroperitonealization
Robotic sacrocolpopexy
We describe a robotic technique of sacrocolpopexy and presented our experience with a morbidly obese patient. This technique combines the advantages of open sacrocolpopexy with the decreased morbidity and improved cosmesis of laparoscopic surgery.[2] It is associated with decreased hospital stay, low complication and conversion rates, and high patient satisfaction. The goal of using a robot-assisted approach is to simplify the execution of laparoscopic maneuvers and shorten the learning curve of laparoscopy.[8]
The Da Vinci robotic surgical system (Intutive surgicals, Sunnyvale, CA, USA) was approved by FDA for performing gynecological procedures in 2005. It was designed to overcome the current limitations of conventional laparoscopy by providing the surgeon with adequate 3D vision, improved dexterity, and precision.
The current body of literature on this approach is primarily limited to short case series and short-term studies. Elliott and colleagues followed 21 patients up until a year after surgery and reported a 95% apical cure rate. This case reported a subjective outcome with a surgical satisfaction rate of 100%.[9]
A recent study by Kramer and colleagues[1] followed 12 patients for an average of 25.2 months after robot-assisted laparoscopic sacral colpopexy without any other concomitant procedure. The largest series by Akl and colleagues[2] followed 80 patients and showed a recurrence rate of 3.7%. Although postoperative bladder function following robot-assisted laparoscopic sacral colpopexy was not investigated well, a small study described resolution of preoperative urge urinary incontinence in 5 out of 6 patients (83%).[10] To date, there are no studies that describe bowel or sexual function relative to preoperative status following robot-assisted laparoscopic sacrocolpopexy. Intra- and postoperative complications associated with robot-assisted laparoscopic sacrocolpopexy have been reported at very low rates.[11]
The results of this surgery on this obese patient should be followed up and effects on bladder, bowel, and sexual function are to be evaluated. The case represents the surgeons challenge to accomplish a large feat to provide an improved and better outcome in obese patient. The Da Vinci surgical system utilizes robotic technology and three-dimensional viewing aids depth perception and optic magnification improves precision deep within the pelvis. Instrument articulation allows for seven degrees of freedom for difficult dissection and eliminates tremor interference (Narula). Appropriate port placement allows for access in multiple abdominal quadrants without collision or restriction. Robotic surgery overcomes the limitations of conventional laparoscopy and facilitates a minimally invasive approach in the setting of complex pathology and advanced dissection (Advincula, Rawlings). Such a minimally invasive surgical technique provides decreased blood loss, improved convalescence, and favorable aesthetics while ensuring comparable outcomes, morbidity, and complication rates.
After viewing the most modern way of robotic surgery for pelvic floor disorder, I googled again to find out whether such surgeries are being done in India. To my surprise I found few articles but definitely found out that India is moving ahead with robotic revolution – leaving behind the days of low technology methods; doctors are ushering in the new era of modern surgical techniques successfully. Robotic surgery in India's premier hospital AIIMS is one of the success stories And now with Robotic centers at Delhi and Chennai, surgeons will find robotic technology to be the solution. Many gynecological surgeons would prefer working as a real team, quickly and efficiently where difficult steps of suturing are made easy. For gynecological patients, in India, it would be a “quantum leap” - patients who are typically going home 4-5 days after the procedure can now go home in 4-6 hours and can sleep in their own bed at home.
ACKNOWLEGMENT
My sincere thanks to Dr. Rosanne Kho, MD. FACOG, Dept. of Urogynecology, Mayoclinic, Scottsdale, Arizona, USA for being my guide and mentor and helping me to complete this article.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.McDermott CD, Hale DS. Abdominal, laparoscopic, and robotic surgery for pelvic organ prolapse. Obstet Gynecol Clin North Am. 2009;36:585–614. doi: 10.1016/j.ogc.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Akl MN, Long JB, Giles DL, Cornella JL, Pettit PD, Chen AH, et al. Robotic-assisted sacrocolpopexy: technique and learning curve. Surg Endosc. 2009;23:2390–4. doi: 10.1007/s00464-008-0311-4. [DOI] [PubMed] [Google Scholar]
- 3.Rosenblatt PL, Chelmow D, Ferzandi TR. Laparoscopic sacrocervicopexy for the treatment of uterine prolapse: a retrospective case series report. J Minim Invasive Gynecol. 2008;15:268–72. doi: 10.1016/j.jmig.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Garg C, Khan SA, Ansari SH, Garg M. Prevalence of obesity in Indian women. Obes Rev. 2010;11:105–8. doi: 10.1111/j.1467-789X.2009.00666.x. [DOI] [PubMed] [Google Scholar]
- 5.Vancaillie TG, Schuessler W. Laparoscopic bladderneck suspension. J Laparoendosc Surg. 1991;1:169–73. doi: 10.1089/lps.1991.1.169. [DOI] [PubMed] [Google Scholar]
- 6.Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81–5. doi: 10.1007/BF01902378. [DOI] [PubMed] [Google Scholar]
- 7.Takacs EB, Kobashi KC. Minimally invasive treatment of stress urinary incontinence and vaginal prolapse. (ix).Urol Clin North Am. 2008;35:467–76. doi: 10.1016/j.ucl.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Novara G, Artibani W. Surgery for pelvic organ prolapse: current status and future perspectives. Curr Opin Urol. 2005;15:256–62. doi: 10.1097/01.mou.0000172399.47019.e9. [DOI] [PubMed] [Google Scholar]
- 9.Elliott DS, Krambeck AE, Chow GK. Long-term results of robotic assisted laparoscopic sacrocolpopexy for the treatment of high grade vaginal vault prolapse. J Urol. 2006;176:655–9. doi: 10.1016/j.juro.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 10.Akladios CY, Dautun D, Saussine C, Baldauf JJ, Mathelin C, Wattiez A. Laparoscopic sacrocolpopexy for female genital organ prolapse: establishment of a learning curve. Eur J Obstet Gynecol Reprod Biol. 2010;149:218–21. doi: 10.1016/j.ejogrb.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Patel V. Robotic surgery: India is not ready yet. Indian J Urol. 2007;23:244–5. doi: 10.4103/0970-1591.33717. [DOI] [PMC free article] [PubMed] [Google Scholar]


