Abstract
Background.
Resistance training programs have been found to improve muscle strength, physical function, and depressive symptoms in middle-aged and older adults. These programs have typically been provided in clinical facilities, health clubs, and senior centers, which may be inconvenient and/or cost prohibitive for some older adults. The purpose of this study was to investigate the effectiveness of an automated telemedicine intervention that provides real-time guidance and monitoring of resistance training in the home.
Methods.
A randomized clinical trial in 103 middle-aged or older participants. Participants were assigned to use of a theory-driven interactive voice response system designed to promote resistance training (Telephone-Linked Computer-based Long-term Interactive Fitness Trainer; n = 52) or to an attention control (n = 51) for a period of 12 months. Measurements of muscle strength, balance, walk distance, and mood were obtained at baseline, 3, 6, and 12 months.
Results.
We observed increased strength, improved balance, and fewer depressive symptoms in the intervention group than in the control group. Using generalized estimating equations modeling, group differences were statistically significant for knee flexion strength (p = .035), single-leg stance time (p = .029), and Beck Depression Inventory (p = .030).
Conclusions.
This computer-based telecommunications exercise intervention led to improvements in participants’ strength, balance, and depressive symptoms. Because of their low cost and easy accessibility, computer-based interventions may be a cost-effective way of promoting exercise in the home.
Keywords: Muscle strength, Balance, Resistance training
SEDENTARY behavior is highly prevalent among middle-aged and older U.S. adults and is associated with a loss of muscle strength (1). Reduced muscle strength is linked to falls, functional disability, and impaired mobility (2–5). Resistance exercise training has been shown to improve balance performance, muscle strength, functional status, and depression symptoms even in the elderly adults (6–11). These studies have typically employed supervised exercise programs, which are not only costly but also often inconvenient to attend. Moreover, most of these trials have been performed over a relatively short duration, although exercise must be continued indefinitely to maintain muscle strength.
We have previously used interactive voice recognition and response systems to monitor health behavior and adherence to treatment and to provide feedback to patients with chronic disease (12,13). For the present study, we have developed a fully home-based resistance exercise training program that makes novel use of this interactive voice response technology. This Telephone-Linked Computer-based Long-term Interactive Fitness Trainer (TLC-LIFT) system provides real-time guidance, meaning that the system provides instructions on what exercises to do and how to do them, guiding the participants through the exercises as they perform them in their homes. Because it is fully automated and administered by telephone in the participant’s own home, it offers great flexibility and sufficiently low cost to continue indefinitely. The TLC-LIFT includes counseling modules designed to improve adherence to exercise training, which are delivered at the conclusion of each exercise session. These modules target specific constructs from Social Cognitive Theory that have been shown to mediate adherence and promote participation in physical activity programs (14–19). The purpose of this study was to assess the effect of the TLC-LIFT system on muscle strength, balance, walk distance, and mood over a period of 12 months in a group of community-dwelling older men and women.
METHODS
Study Sample
Participants were drawn from the Normative Aging Study, a longitudinal cohort study of aging that was established by the Veterans Administration in 1963 (20). The original cohort consisted of community-dwelling men in the Boston area. Beginning in 1991, women who were wives of Normative Aging Study participants were recruited into the cohort. At the time of study, the cohort consisted of 500 men and 159 women with a mean age of 74 years (range 50–94). Normative Aging Study participants undergo regular medical examinations, detailed clinical evaluations including electrocardiograms, at 3-year intervals. A research assistant identified participants who passed exclusion criteria from a daily list of Normative Aging Study participants who had scheduled on-site visits for their periodic examination, described the study protocol, and invited participants to participate. The exclusion criteria were (a) angina pectoris (unless symptomatically resolved postrevascularization), (b) history of myocardial infarction within 6 months or remote (>6 months) myocardial infarction with current myocardial ischemia on exercise stress test, (c) history of ventricular dysrhythmia requiring therapy, (d) baseline systolic blood pressure greater than or equal to 165 mm Hg and/or diastolic blood pressure greater than or equal to 100 mm Hg, and (e) currently participating in a regular exercise program less than one time per week for 20 minutes per session. The medical records and electrocardiograms of interested participants were reviewed by a physician investigator for final clearance. Because the TLC-LIFT system is quite simple to use, there were no specific educational or intellectual criteria for participation. After eligible participants gave written informed consent, we collected baseline study data and then randomized them to one of two groups using a computer-based algorithm (randomize function in Visual Basic) to perform random assignment without blocking or stratification. One group was assigned to use an educational control TLC system (“attention control group”) and the other group to use the TLC-LIFT system. The study protocol was approved by the Institutional Review Board at the VA Boston Healthcare System and registered at ClinicalTrials.gov (NCT 00248781).
TLC-LIFT Intervention
Hands-on instructions.—
Initially, a trained staff member provided hands-on instruction on each of eight resistance exercises and the warm-up and cooldown. The participants were asked to perform a couple of repetitions of each exercise with light weights under supervision. After the exercise instruction, participants were instructed on the use of the TLC-LIFT system, including the use of a cordless phone with attached headset and proper responses to the system prompts. Participants then underwent an abbreviated TLC-LIFT session consisting of actual use of the cordless phone and headset with four repetitions of each exercise using 2-pound weights. Over the first 3 months of the intensive 6-month use of TLC-LIFT, we conducted periodic home visits (at 2, 4, and 8 weeks) and contacted participants by phone (at 1, 6, and 10 weeks) to check on their exercise technique and use of the TLC-LIFT system.
Resistance exercise training with TLC-LIFT.—
We used a home-based resistance exercise training program adapted from Ettinger and colleagues (21). The program comprised three 1-hour sessions per week consisting of a warm-up phase (10 minutes), a stimulus phase (40 minutes), and a cooldown phase (10 minutes). The stimulus phase was made up of eight exercises: knee extension, knee curl, step-up, heel raise, chest fly, upright row, front shoulder raise, and biceps curl. Upper body exercises were performed with dumbbells and lower body exercises with cuff weights. All equipment was provided by the study staff.
During each session, participants were asked to perform two sets of 12 repetitions of the eight exercises. Each participant started the program using the lowest available resistance (2 lbs for both upper and lower body). Weight was increased by 2 lbs each succeeding session for a given exercise as long as the participant was able to complete two sets of 10 or more repetitions. Because the weight used and the number of repetitions performed in previous sessions were stored in TLC-LIFT’s database, the system was able to review and guide the participant on the weight and repetition goals for each exercise in the current session. Once the participant reached a weight at which he or she was unable to complete two sets of 10 or more repetitions, the resistance was held at this weight for at least three succeeding sessions. When the participant was able to complete two sets of 12 repetitions for three consecutive sessions at that weight, the weight again increased by 2 lbs for the next session. A rating of perceived exertion (RPE) was obtained weekly following an exercise session using the Borg scale (22). A rating of 15–16 was targeted. If the RPE was less than or equal to 14, the participant was encouraged to increase the number of repetitions performed in the subsequent sessions. If the RPE was greater than or equal to 17, the participant was encouraged to decrease the number of repetitions in subsequent sessions.
The exercise program lasted 12 months, but after 6 months, participants were switched into a maintenance phase by the system during which they were prompted to perform their exercises with the system at least once a week. TLC-LIFT was programmed to contact the participant at least every 7 days. With each call, TLC-LIFT motivated and encouraged the participant to continue exercising three times per week, even without using the system. However, during the maintenance phase, the participants had the option of exercising with TLC-LIFT for all their exercise sessions if they chose to exercise more than once per week.
Scheduled calls.—
The TLC-LIFT called participants, with a target exercise schedule of 3 days per week. At the initiation visit, users indicated what their preferred time to exercise was, and this was the time that TLC-LIFT was scheduled to call. The TLC-LIFT system is security enabled, so at the beginning of a call, each participant was asked to enter a personal password (PIN) to ensure security and confidentiality. Following the identification confirmation, TLC-LIFT asked the participant if he/she was ready to perform his/her exercises. If the participant was not ready, he/she was asked to call a toll-free number when ready, which informed TLC-LIFT to call the person shortly thereafter to begin the exercise session. If the person failed to call back within 4 hours of TLC’s call, calls were repeated periodically during a time period previously set by the user. After a 24-hour period had elapsed without the user completing a scheduled exercise session, the TLC system administrator was notified automatically and informed a staff member so that he or she could contact the user.
During the first week, before each exercise, the TLC-LIFT system provided the user with detailed instructions on the proper technique for that exercise. Thereafter, the user was asked before each exercise if he or she would like to hear this description. “Yes” triggered the TLC-LIFT system to play a recorded message describing the proper technique of the exercise; “No” bypassed the instruction, and TLC-LIFT gave a short tip on the proper technique: for example, before beginning knee extensions, “Remember to extend your legs without locking your knees.” During all exercise sessions, the TLC-LIFT system instructed the user to begin and to count each repetition out loud. Between sets of repetitions, the TLC-LIFT system prompted the participant to take a timed 30-second break and continue with the session when the 30 seconds were up. Voice recognition of each counted repetition allows the system to monitor the number of repetitions for each exercise and store this information to determine whether the resistance can be raised for the succeeding exercise sessions, and by monitoring the amount of time the participant takes to perform the repetitions, it allows the system to remind the participant to slow down or speed up the exercise. To reduce the risk of any injury from exercising, participants were instructed in every call to stop exercising if they experienced symptoms suggestive of a musculoskeletal injury or cardiac or neurological problems. Participants all had a phone number that could be called 24 hours a day to page a study physician to report any problems or concerns.
Attention Control
Participants randomized to the attention control group received general health education via a TLC system at weekly intervals. This system provides general information about a variety of health topics via telephone calls. At each call, participants selected a topic from a list of content areas that included common symptoms, medical conditions, and preventive medicine topics. The health information dialogs were adapted from Harvard Health Letter articles (http://www.health.harvard.edu). The dialogs were developed to allow users to identify subtopics about which they wanted more information, and to skip others, and avoided long stretches of uninterrupted talking by the system (23).
Data Collection
Data for analyses were collected during four clinic-based examinations (baseline, 3, 6, and 12 months), conducted by research assistants blind to group assignment. At the baseline examination, height and weight were measured, and assessments of strength, balance, walking, and depressive symptoms were recorded. These assessments were repeated at 3, 6, and 12 months. Six primary outcomes were measured, covering four domains of interest: strength, balance, functional status, and mood, as described later.
Maximal voluntary strength was measured during dynamic contractions against a hydraulic resistance system (HF STAR, Hydrafitness Total Power; Henley Health Care, Belton, TX) previously used in participants with cardiopulmonary disorders (24). With the participant seated, the peak force (measured in kilograms) at each of six levels of hydraulic resistance was recorded during bilateral knee extensions and bilateral knee flexions. Using this apparatus, during contraction, the positively accelerating nature of the pressure/flow relationship is such that flow reaches an approximately constant value as pressure increases. Therefore, the force generated by the participant increases with increasing voluntary effort, while the velocity of contraction remains relatively constant (24,25). The peak force at the highest resistance level for knee extension and knee flexion was used in the analysis.
Balance was assessed using two tests: single-leg stance with the eyes open and tandem stance, both measured in seconds up to a maximum of 60 seconds (26). The single-leg stance time was how long the participant maintained the posture without moving the support foot, touching the floor or support leg with the suspended foot, or requiring assistance. The tandem stance was how long the participant stood with the heel of one foot touching the toe of the other and the feet kept in a straight line. Testing consisted of one practice and three recorded trials for each test. The mean of the three recorded trials was used for analysis.
Functional status was assessed by a 6-minute walk, which was performed according to a standardized protocol (27). Participants were instructed to walk up and down a 100-foot level hallway as far as they could in 6 minutes under observation by research staff who provided standardized encouragement.
Depressive symptoms were assessed with the Beck Depression Inventory-revised (BDI-II), a 21-item (each item scored 0–3) self-report rating scale (28). This revised version of the original BDI was updated to correspond to Diagnostic and Statistical Manual of Mental Disorders-IV criteria.
Data Analysis
Analyses were performed by intention to treat, using all outcome data collected regardless of adherence to assigned treatment. The analysis took the form,
where INT is a dummy variable indicating that the participant is (INT = 1) or is not (INT = 0) receiving the TLC-LIFT intervention, TIME6 and TIME12 are dummy variables indicating whether the outcome is recorded at 3 (TIME6 = 0 and TIME12 = 0) or 6 (TIME6 = 1 and TIME12 = 0) or 12 (TIME6 = 0 and TIME12 = 1) months postbaseline, and age, body mass index, and baseline level of the outcome variable (BASE) are the baseline covariates. Because each individual contributes three values at 3, 6, and 12 months, generalized estimating equations (29) were used to estimate effects properly adjusted for nonindependent contributions. The exchangeable working covariance model was used as there is only one intrasubject correlation parameter for the three-period study. Because there were three participants with no outcome data, the above analysis was repeated with the use of the last-observation-carried-forward approach in which baseline values were carried forward for individuals with no outcome measures.
Analyses of all six primary outcomes were preplanned, with a p value less than .05 (two tailed) considered significant for each analysis. Power estimates for this study are based on a prior study in middle-aged and older adults of supervised progressive resistance training, which utilized the same device that we have used to measure lower extremity strength (30). In that study, the addition of resistance training to a pulmonary rehabilitation program resulted in increases in knee flexion and extension strength of 1.63 and 1.2 SD, respectively. Our study sample of 100 evaluable participants, approximately equally divided between intervention and control groups, provided 99.9% power to detect the smaller of these effects at α (2) = .05, and 80% power to detect a more conservative effect of 0.57 SD. A smaller effect size was anticipated due to the unsupervised nature of the resistance training in the current study.
RESULTS
A total of 103 participants were randomized to the TLC-LIFT intervention (n = 52) or attention control (n = 51) groups. The mean age of the participants was 71.0 (SD 7.4) years, the mean body mass index was 28.8 (SD 4.5), and 69% were men. The intervention and control groups were similar on baseline characteristics except for 6-minute walk (p = .02; Table 1). Follow-up outcome data were available from either the 3-, 6-, or 12-month examinations in 97% of participants (Figure 1), who were therefore included in the primary analysis. For the first 3 months, 66% of scheduled intervention sessions were completed and 42% of scheduled control sessions were completed. For Months 4–6, the percentage of scheduled sessions completed was 43 in the intervention group and 24 in the control group. Adverse events were not different between TLC-LIFT and attention control. Serious adverse events (all hospitalizations) were reported in six TLC-LIFT and seven attention control participants and were not related to the intervention. Nonserious adverse events (all musculoskeletal injury and discomfort) were reported in eight TLC-LIFT and seven control participants.
Table 1.
Baseline Characteristics of Study Participants (N = 103)*
| Intervention (TLC-LIFT) | Control | |
| Age (years) | 70.3 ± 7.5 | 71.7 ± 7.2 |
| Male (%) | 67.3 | 70.6 |
| Body mass index (kg/m2) | 29.3 ± 4.1 | 28.2 ± 4.9 |
| Knee extension strength (kg) | 20.3 ± 9.9 | 19.6 ± 8.7 |
| Knee flexion strength (kg) | 35.7 ± 13.5 | 33.8 ± 12.1 |
| Single-leg stance with eyes open (s) | 18.5 ± 16.9 | 21.6 ± 21.0 |
| Tandem stance (s) | 14.7 ± 29.7 | 11.0 ± 3.5 |
| 6-min walk (m) | 459 ± 77.3 | 422.9 ± 78.3 |
| BDI | 3.8 ± 4.3 | 5.0 ± 6.3 |
Notes: Telephone-based resistance training. BDI = Beck Depression Inventory; TLC-LIFT = Telephone-Linked Computer-based Long-term Interactive Fitness Trainer.
Results are mean ± standard deviation.
Figure 1.
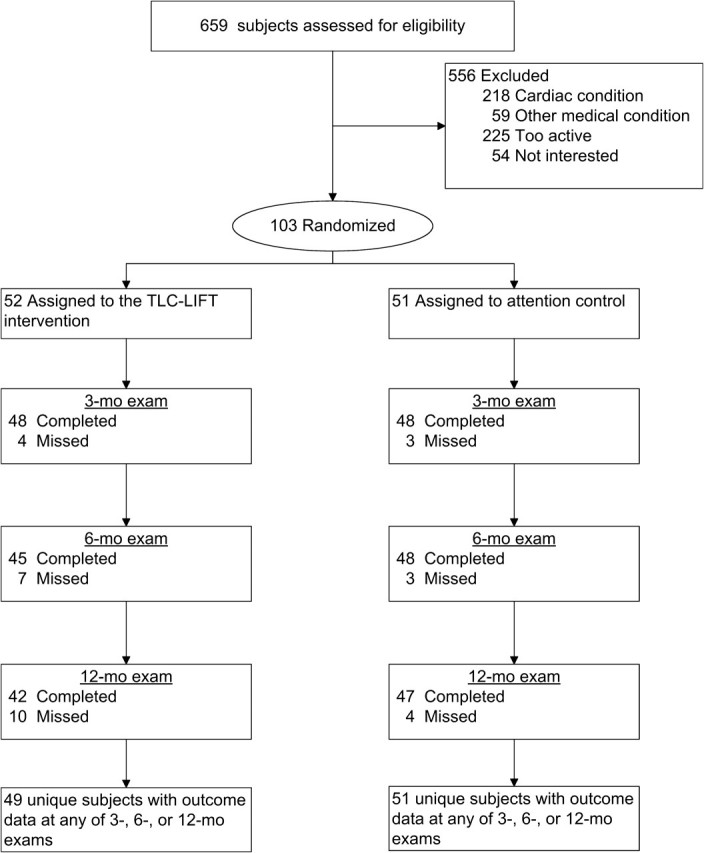
Participant flow.
In the TLC-LIFT participants, the exercise training intensity increased progressively. Single-leg knee extension intensity was as follows: 1 month = 4.4 ± 2.6 kg (mean ± standard deviation), 3 months = 6.6 ± 2.1, 6 months = 7.5 ± 2.0, and 12 months = 8.1 ± 1.6. RPE ratings were 11.6 ± 3.4 after 1 month but then were stable subsequently (Month 3 = 12.5 ± 3.4, Month 6 = 12.8 ± 3.3, and Month 12 = 12.2 ± 3.0). The number of repetitions also varied little as participants moved up in weight (Month 1 = 10.4 ± 2.4, Month 3 = 10.7 ± 2.4, Month 6 = 10.7 ± 2.6, and Month 12 = 11.8 ± 0.6).
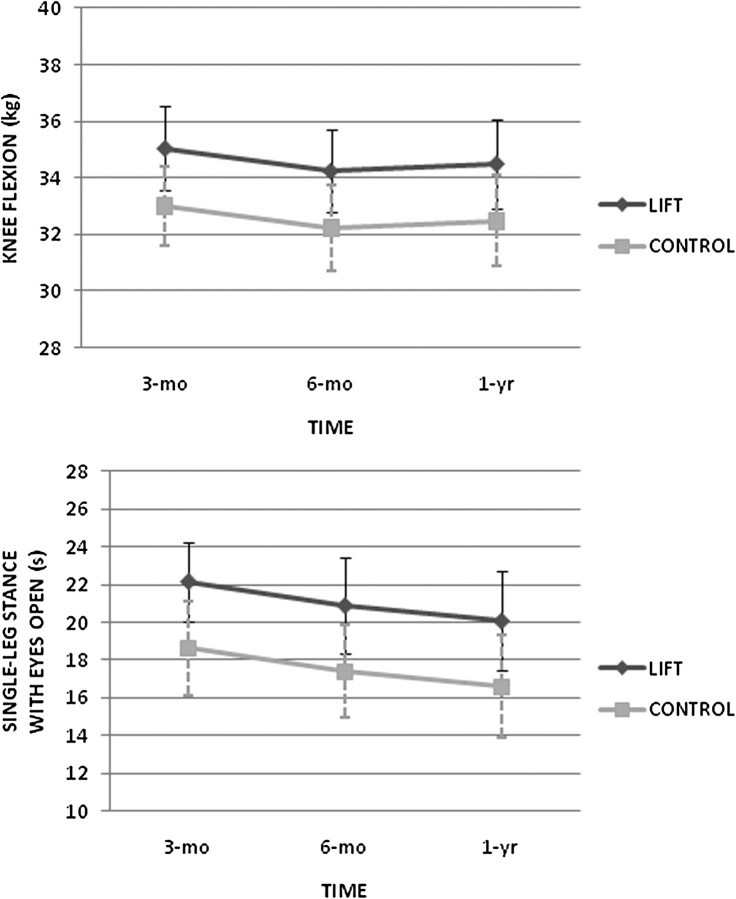
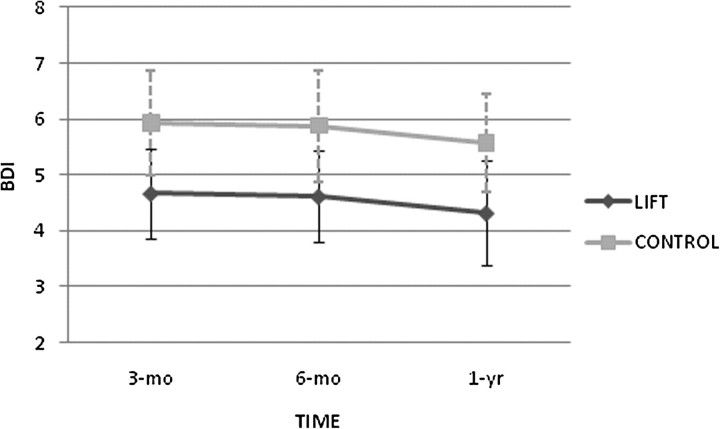
We found that exercise training using TLC-LIFT was associated with greater knee flexion strength in the generalized estimating equations analysis (b = 2.04 and p = .035; Figure 2). Exercise training was not significantly associated with knee extension strength (b = 1.13 and p = .17). Balance was significantly improved with resistance training when assessed with the single-leg stance (b = 3.51 and p = .029; Figure 2) but not with the tandem stance (b = 4.57 and p = .10). There was no association between exercise training and 6-minute walk distance (b = 0.78 and p = .91). Lower levels of depressive symptoms, as assessed with the BDI, were observed in TLC-LIFT participants than in controls (b = −1.26 and p = .030; Figure 3). Results of the last-observation-carried-forward analyses yielded the same statistical conclusions for these six outcomes.
Figure 2.
Knee flexion strength and single-leg stance measurements by group over time.
Figure 3.
Beck Depression Inventory measurements by group over time.
We administered a questionnaire to TLC-LIFT participants to assess their impressions of the system. Participants were asked to respond to a number of statements using 5-point Likert scales varying from “strongly agree” to “strongly disagree.” Seventy-six percent of participants “strongly agreed” (“5”) or “agreed” (“4”) that “I find the computer system easy to use.” Fifty-nine percent of participants “strongly agreed” or “agreed” that “The telephone system’s advice is right on target for me.” Seventy-six percent of participants “strongly agreed” or “agreed” that “The computer system motivates me to exercise.”
DISCUSSION
In this study, we administered a minimally supervised resistance training program via a novel interactive voice recognition and response system. This permitted an inexpensive and fully home-based training program that could be maintained over a long period of time. A novel feature of this intervention is that this progressive relatively high intensity resistance training program was administered with very little staff contact and almost entirely via telephone. Notwithstanding the unsupervised nature of the intervention, this study did find increased strength, improved balance, and fewer depressive symptoms in the intervention than in the control group. These differences were statistically significant for knee flexion strength, single-leg standing time, and BDI, with nonsignificant trends favoring the intervention for knee extension strength, tandem stance time, and 6-minute walk distance. Notwithstanding the performance of six separate tests of association, the consistent direction of effect across all six study outcomes makes it unlikely that the observed differences were due to chance.
Several prior studies have evaluated the effect of fully home-based or hybrid supervised and home-based progressive resistance training programs on isokinetic lower extremity strength. In the only other fully home-based program, Jette and colleagues (31) used a videotaped program of exercise with elastic bands of varying thickness to allow progressive resistance. In this study of 215 adults older than 60 years and reporting at least some functional limitations, the intervention group increased strength by 6%–12% in various muscle groups at 6 months including a 1.6 kg greater increase in peak knee extension force; knee flexion strength was not measured. This result is similar to the effect of our intervention, which resulted in a 1.1 kg greater increase in peak knee extension force and a 2.0 kg greater increase in knee flexion force. In a study of 3 months of supervised exercise followed by 15 months of unsupervised home-based exercise in 439 patients with knee osteoarthritis, Ettinger and colleagues found that isokinetic knee extension and flexion strength were 3.2 and 3.7 Nm higher, respectively, in the resistance training group than in a health education control group. As in the present study, this difference was statistically significant only for knee flexion (21). Another study in 221 patients with osteoarthritis compared 12 months of mixed supervised and home-based resistance training, followed by home exercise for an additional 18 months, with a range of motion control condition. That study found a nonsignificant decrease in the rate of loss of isokinetic knee flexion and extension strength in the resistance training group (32).
In the present study, we found that exercise training was associated with a significant improvement in static balance using the single-leg stance, the most commonly employed measure of balance. We also found a trend toward improvement in balance using the tandem stance. The one prior home-based study to assess effects of resistance training on balance found a significant improvement in tandem gait, a measure of dynamic balance, although no significant difference in single-leg stance time (31). Neither that study nor a study using a 12-week hybrid supervised and home training program (33) found significant changes in functional reach, another measure of dynamic balance. However, Nelson and colleagues (34) reported an increase in dynamic balance in mobility-limited older adults following 6 months of a home-based multimodal exercise intervention. Overall, the improvements in balance with home-based resistance training are less consistent than those in strength.
Prior studies in community-dwelling adults with depression or dysthymia demonstrated a reduction in depressive symptoms with supervised resistance training using the BDI or Hamilton Rating Scale for depression (10,11). However, two previous home-based or hybrid resistance training programs found no significant effect of training on depressive symptoms (31,35). This may reflect the low number of depressive symptoms reported in those studies, which utilized the Profile of Mood States and Center for Epidemiological Studies-Depression scale, respectively, as a trend toward greater reduction in depressive symptoms was noted in one of these studies when participants with higher baseline depressive symptoms were analyzed separately (35). In contrast, despite the mild severity of depressive symptoms in our sample, which was selected independent of depressive symptoms, we found a significant reduction in depressive symptoms in the intervention group using the BDI-II.
In summary, we report on a novel telephone-based interactive system that can successfully and safely administer a progressive resistance training program to older adults. This system resulted in significant improvements in muscle strength and balance. Future studies should be designed to evaluate the effectiveness of this type of intervention delivery on more distal health and disability-related outcomes in older adults.
FUNDING
This work was supported by the Rehabilitation Research and Development Service of the Department of Veterans Affairs, the Boston Claude D. Pepper Older Americans Independence Center (1P30AG031679), and the U.S. Department of Agriculture under agreement No. 58-1950-7-707. The VA Normative Aging Study, a component of the Massachusetts Veterans Epidemiology Research and Information Center, Boston, Massachusetts, is supported by the Cooperative Studies Program/Epidemiology Research and Information Center of the U.S. Department of Veterans Affairs.
Acknowledgments
We would like to thank Vincent Carey for his assistance in many aspects of the study design and data analysis.
References
- 1.Kruger J, Carlson SA, Buchner D. How active are older Americans? Prev Chronic Dis. 2007;4:A53. [PMC free article] [PubMed] [Google Scholar]
- 2.Schwendner KI, Mikesky A, Holt WS, Peacock M, Burr DB. Differences in muscle endurance and recovery between fallers and nonfallers, and between young and older women. J Gerontol A Med Sci. 1997;52:M155–M160. doi: 10.1093/gerona/52a.3.m155. [DOI] [PubMed] [Google Scholar]
- 3.Janssen I. Influence of sarcopenia on the development of physical disability: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:56–62. doi: 10.1111/j.1532-5415.2005.00540.x. [DOI] [PubMed] [Google Scholar]
- 4.Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60:324–333. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 5.Latham NK, Bennett DA, Stretton CM, Anderson CS. Systematic review of progressive resistance strength training in older adults. J Gerontol A Biol Sci Med Sci. 2004;59A:48–61. doi: 10.1093/gerona/59.1.m48. [DOI] [PubMed] [Google Scholar]
- 6.Rooks DS, Kiel DP, Parsons C, et al. Self-paced resistance training and walking exercise in community-dwelling older adults: effects on neuromotor performance. J Gerontol A Med Sci. 1997;52A(3):M161–M168. doi: 10.1093/gerona/52a.3.m161. [DOI] [PubMed] [Google Scholar]
- 7.Liu-Ambrose T, Khan KM, Eng JJ, et al. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vincent KR, Braith RW, Feldman RA, et al. Resistance exercise and physical performance in adults aged 60 to 83. J Am Geriatr Soc. 2002;50(6):1100–1107. doi: 10.1046/j.1532-5415.2002.50267.x. [DOI] [PubMed] [Google Scholar]
- 9.Whiteford J, Ackland TR, Dhaliwal SS, et al. Effects of a 1-year randomized controlled trial of resistance training on lower limb bone and muscle structure and function in older men. Osteoporos Int. 2010;21:1529–1536. doi: 10.1007/s00198-009-1132-6. [DOI] [PubMed] [Google Scholar]
- 10.Singh NA, Clements KM, Fiatarone Maria A. A randomized controlled trial of progressive resistance training in depressed elders. J Gerontol A Med Sci. 1997;52:M27–M35. doi: 10.1093/gerona/52a.1.m27. [DOI] [PubMed] [Google Scholar]
- 11.Singh NA, Stavrinos TM, Scarbek Y, Galambos G, Liber C, Fiatarone Singh MA. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol A Biol Sci Med Sci. 2005;60:768–776. doi: 10.1093/gerona/60.6.768. [DOI] [PubMed] [Google Scholar]
- 12.Sparrow D, Aloia M, DeMolles DA, Gottlieb DJ. A telemedicine intervention to improve CPAP adherence: a RCT. Thorax. 2010;65:1061–1066. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- 13.Young M, Sparrow D, Gottlieb D, Selim A, Friedman R. A telephone-linked computer system for COPD care. Chest. 2001;19:1565–1575. doi: 10.1378/chest.119.5.1565. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Exercise of personal agency through the self-efficacy mechanism. In: Schwarzer R, editor. Self-efficacy: Thought Control of Action. Washington, DC: Hemisphere; 1992. pp. 3–38. [Google Scholar]
- 15.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 16.Sallis JF, Hovell MF, Hofstetter CR, et al. A multivariate study of determinants of vigorous exercise in a community sample. Prev Med. 1989;18:20–34. doi: 10.1016/0091-7435(89)90051-0. [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Self-efficacy: The Exercise of Control. New York: WH Freeman and Company; 1997. [Google Scholar]
- 18.O’Leary KD, Wilson GT. Behavior Therapy: Application and Outcome. 2nd ed. Englewood Cliffs, NJ: Prentice Hall; 1987. [Google Scholar]
- 19.Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in Addictive Behavior Change. New York: Guilford Press; 1985. [Google Scholar]
- 20.Bell B, Rose CL, Damon A. The Normative Aging Study: an interdisciplinary and longitudinal study of health and aging. Aging Hum Dev. 1972;3:4–17. [Google Scholar]
- 21.Ettinger WH, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. JAMA. 1997;277:25–31. [PubMed] [Google Scholar]
- 22.Borg G. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- 23.Ramelson HZ, Bassey B, Friedman RH. The use of computer telephony to provide interactive health information. AMIA Annu Symp Proc. 2003:539–543. [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton AL, Killian KJ, Summers E, Jones NL. Muscle strength, symptom intensity, and exercise capacity in patients with cardiorespiratory disorders. Am J Respir Crit Care Med. 1995;152:2021–2031. doi: 10.1164/ajrccm.152.6.8520771. [DOI] [PubMed] [Google Scholar]
- 25.Sale DG. Testing strength and power. In: MacDougall JD, Wonge HA, Green HJ, editors. Physiologic Testing of the High-Performance Athlete. Champaign, IL: Human Kinetics Publishers; 1991. pp. 21–106. [Google Scholar]
- 26.Rossiter-Fornoff JE, Wolf SL, Wolfson LI, Buchner DM. A cross-sectional validation study of the FICSIT common data base static balance measures—frailty and injuries: cooperative studies of intervention techniques. J Gerontol A Med Sci. 1995;50A(6):M291–M297. doi: 10.1093/gerona/50a.6.m291. [DOI] [PubMed] [Google Scholar]
- 27.Guyatt G, Sullivan M, Thompson P, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio TX: Psychological Corporation; 1996. [Google Scholar]
- 29.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 30.Mador MJ, Bozkanat E, Aggarwal A, Shaffer M, Kufel TJ. Endurance and strength training in patients with COPD. Chest. 2004;125:2036–2045. doi: 10.1378/chest.125.6.2036. [DOI] [PubMed] [Google Scholar]
- 31.Jette AM, Lachman M, Giorgetti MM, et al. Exercise—it’s never too late: the strong-for-life program. Am J Public Health. 1999;89(1):66–72. doi: 10.2105/ajph.89.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55(5):690–699. doi: 10.1002/art.22245. [DOI] [PubMed] [Google Scholar]
- 33.Skelton DA, Young A, Greig CA, Malbut KE. Effects of resistance training on strength, power, and selected functional abilities of women aged 75 and older. J Am Geriatr Soc. 1995;43:1081–1087. doi: 10.1111/j.1532-5415.1995.tb07004.x. [DOI] [PubMed] [Google Scholar]
- 34.Nelson ME, Layne JE, Bernstein MJ, et al. The effects of multidimensional home-based exercise on functional performance in elderly people. J Gerontol A Biol Sci Med Sci. 2004;59A(2):154–160. doi: 10.1093/gerona/59.2.m154. [DOI] [PubMed] [Google Scholar]
- 35.Penninx BWJH, Rejeski WJ, Pandya J, et al. Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J Gerontol B Psychol Sci. 2002;57(2):P124–P132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]