Abstract
Anxiety disorders are the most common mental health problems experienced by young people, and even mild anxiety can significantly limit social, emotional, and cognitive development into adulthood. It is, therefore, essential that anxiety is treated as early and effectively as possible. Young people are unlikely, however, to seek professional treatment for their problems, increasing their chance of serious long-term problems such as impaired peer relations and low self-esteem. The barriers young people face to accessing services are well documented, and self-help resources may provide an alternative option to respond to early manifestations of anxiety disorders. This article reviews the potential benefits of self-help treatments for anxiety and the evidence for their effectiveness. Despite using inclusive review criteria, only six relevant studies were found. The results of these studies show that there is some evidence for the use of self-help interventions for anxiety in young people, but like the research with adult populations, the overall quality of the studies is poor and there is need for further and more rigorous research.
Keywords: adolescent, young adult, children, mental disorder, self-administered, bibliotherapy, therapist-guided
Introduction
Young people have high rates of mental disorder, with the National Comorbidity Survey-Adolescent Supplement (NCS-A) finding that 22.2% of young people aged 13–18 years in the United States suffer from a mental health problem that causes them severe distress.1 The most common mental health problems are anxiety disorders, and the median age of onset is prior to adolescence. Consequently, the preadolescent and adolescent years are critical for implementing preventive and early interventions, yet young people are reluctant to seek professional mental health care. Self-help therapies may, therefore, be critical to effectively intervening to address young people’s anxiety without the need for professional service use. This paper reviews the development and current evidence base for such self-help therapies for use by young people with mild anxiety disorders.
Mild anxiety disorder
Anxiety disorders comprise a number of specific mental disorders including: generalized anxiety disorder, social anxiety disorder (SAD), panic disorder without agoraphobia, panic disorder with agoraphobia, specific/isolated phobia, separation anxiety disorder, obsessive compulsive disorder, post-traumatic stress disorder, anxiety disorder due to a medical condition, and anxiety disorder not specified.2 Anxiety disorders have been identified as being the most common mental health problem, with 18.1% of the adult population in the United States meeting the criteria as described in the DSM-IV.3 The most common of the anxiety disorders are generalized anxiety disorder and SAD. Anxiety disorders are of particular concern for young people with the median age of onset for all anxiety disorders being 11 years of age. Estimates for the median age of onset for specific anxiety disorders, such as separation anxiety disorder, are as low as 7 years.4
Each of the anxiety disorders can be classified as being severe, moderate, or mild and such classifications depend upon the criteria of the particular measure used. However, the main distinctions between mild disorders and those that are moderate or severe tend to be suicide risk and role impairment, which are used to distinguish clinically significant from clinically non-significant (mild) disorder.5 For example, Kessler et al3 describe the components for severe anxiety disorders as including: a 12-month suicide attempt with serious lethality intent; work disability or substantial limitation due to the anxiety disorder; or 30 or more days out of a role in a year due to the anxiety disorder. Anxiety disorders were “moderate” if they did not fit into the “severe” category and had: suicide gesture, plan or ideation; concurrent substance dependence without serious role impairment; moderate work limitation; or moderate role impairment.6 Anxiety disorders which did not fit into either the “severe” or “moderate” category were described as mild.
Anxiety disorders are highly debilitating in childhood and adolescence and if left untreated can lead to other mental health problems, suicidal behavior, teenage parenthood, early marriage, and unemployment.7–11 Anxious children are less likely to complete schooling, with their teachers stating that they have problems with attention, deficits in academic performance, and are significantly more immature than their non-anxious peers.12 Anxious children face social disadvantages as they are often less liked by their peers who find them socially withdrawn and shy.12 The social pressure faced by young people with anxiety disorders can result in many turning to inefficient and harmful coping strategies such as overeating or harmful alcohol use.13 Serious longterm effects that impact throughout adulthood can occur even for young people with relatively mild problems,14 and it is imperative that effective preventive and early interventions are developed for young people with anxiety.
Treating anxiety
The accepted evidence-based approach in the treatment of anxiety disorders is cognitive-behavioral therapy (CBT), which challenges and tries to change negative or irrational thinking and behavior patterns.15,16 CBT involves identifying components of the disorder and applying specific treatments to those components. For anxiety disorders, these components may include physiological arousal, muscle tension, cognitive worries, and avoidance behaviors.17 Specific treatments include relaxation techniques, cognitive restructuring, targeting irrational fears through education, and graded exposure therapy.17
Anxiety treatments for children generally comprise five components: psychoeducation, somatic management skills training, cognitive restructuring, exposure, and relapse prevention.18 Psychoeducation involves teaching information about anxiety and feared stimuli. Somatic management skills training involves targeting automatic arousal responses. Cognitive restructuring focuses on changing maladaptive thoughts. Exposure comprises graduated, systematic, and controlled exposure to feared stimuli and situations. Relapse prevention consolidates learning and supports generalization of treatment to other situations.18 Even relatively brief CBT, based on these components, effectively reduces anxiety symptoms and distress and improves psychosocial functioning in children and adolescents, and can be delivered in individual therapy or group sessions.19,20
Barriers to young people accessing service-based treatment
Despite high rates of mental disorder and the availability of effective treatments, most young people do not access mental health treatment services. Studies from many countries show that only 10%–30% of young people will seek professional help for their mental health problems.21–27 For example, a study conducted in Germany of young people aged 12–17 years who had anxiety, found that only 18.2% had sought help for their problem.28 Within this study, young people with post-traumatic stress disorder were most likely to seek help (47.1%), and young people with a non-specific phobia were least likely to seek treatment (0.22%).
Several barriers have been consistently identified as reasons why young people fail to seek professional help.29 One of these reasons is the strong belief held by young people that they should cope alone.30 This is reflected in their high admiration of peers who do not require help from others for their personal problems.31 Other factors include negative beliefs or attitudes about mental illnesses or the available treatments,32,33 being male,34–37 low mental health literacy,38–40 and inadequate social or interpersonal skills.14,41 Young people who have had negative past experiences with mental health professionals have also been shown to be less likely to seek treatment in the future.42
The pathways to care for younger children are also complex. Children need to rely on their parents or caregivers to first identify that a problem exists and then seek out appropriate support.43 Commonly reported reasons why parents do not seek help for their children are because of cost, not knowing where to seek help, and long waiting lists.44 Other identified reasons include a lack of knowledge about the consequences of untreated child mental disorders, lack of knowledge of effective treatments, and difficulty in getting their child to regular appointments.45
Self-help interventions
Self-help approaches avoid many of the barriers that affect access to traditional face-to-face treatment services, and provide an important alternative that can increase access to effective interventions. Self-help is likely to be particularly attractive for adolescents as it allows young people to seek help independently from their parents, supporting their natural developmental trend towards independence.30,46 The anonymity of self-help interventions is likely to be valued by young people who fear the stigma associated with service use and negative attitudes towards mental health care. Self-help approaches also allow for flexibility in time and place of delivery, and can be especially beneficial for those who cannot easily access face-to-face services.47–49
There are many variations of self-help, which means that as a category of interventions they are not easy to define. Self-help ranges from non-interactive information and psychoeducation to interactive intervention programs based on empirically supported treatments with individualized feedback.50,51 A comprehensive definition is provided by Bower, Richards, and Lovell who state that self-help is:
a therapeutic intervention administered through text, audio, video, or computer text, or through group meetings or individualized exercises such as “therapeutic writing,” and
designed to be conducted predominantly independently of professional contact.52
Self-help interventions can be classified into one of three categories: general self-help; problem-focused self-help; and technique-focused self-help.53 General self-help approaches are those that address broad-spectrum emotional and relational problems, and provide guidelines for general well-being.53 These may also involve various social support interventions. 54 Problem-focused approaches are those that target a specific disorder, such as anxiety.53 Technique-focused approaches teach users how to use a specific technique that may be useful in multiple situations, such as CBT or relaxation.53 Problem and technique-focused approaches are generally informed by theory and have been empirically tested and specifically designed to create positive cognitive, behavioral, and emotional changes.17,50 Interventions that use problem-focused or technique-focused methods are usually delivered through modules with moderate to high interactivity, automated or human-generated feedback, and automated tailoring.50
Self-help books for anxiety have been widely available for many years and are frequently amongst the top 100 best sellers.55 These are available for both adults and children and some well-known titles include: Calming Your Anxious Mind: How Mindfulness and Compassion Can Free You From Anxiety, Fear and Panic;56 Helping Your Anxious Child: A Step-by-step Guide for Parents;57,58 Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child’s Fears, Worries, and Phobias;59 and Anxiety in Childhood and Adolescence.60 Although such books are popular, and they are often developed by experienced clinicians and based on strong conceptual frameworks, they are rarely supported by direct evidence of their effectiveness.61
Over the past decade or so, self-help treatments have moved from being based mostly on self-help books and bibliotherapy to use of new technologies.62 Self-help approaches have been quick to adopt new technologies, and recent interventions have been developed to use on internet sites, through email or chatrooms, on palmtops, with virtual reality technology, and on CD-ROM programs.45 Some of these interventions are highly advanced and offer multiple sessions using specific therapeutic techniques, as well as containing non-specific features that affect important therapeutic processes, such as the therapeutic alliance, engagement, motivation, and trust.63 Online self-help approaches have grown rapidly in recent years, responding to the increase in house-holds that have access to the internet and, in particular, the high level of uptake of new technologies by young people. 64 The majority of these interventions have undergone only initial trials to aid their development, however, and quality evidence of effectiveness is lagging.
Although self-help interventions are by definition devised to be undertaken without the support of a professional, in practice they are often implemented with varying degrees of professional support. They span the entire spectrum – from being entirely self-administered without even professional recommendation to being integrated within traditional face-to-face therapy as homework, a component of therapy or recommended self-management resources.16,55,65 Self-help options are also often used to treat important comorbidities that are not the main focus of therapy, freeing valuable therapy session time to focus on the primary issue.
Current evidence
To date, the majority of research on self-help treatments for anxiety disorders has been undertaken with adult samples, and the results are mixed. A recent systematic review identified 13 studies meeting the inclusion criteria for a review of the clinical effectiveness of CBT-based guided self-help for anxiety and depressive disorders.66 A subsequent meta-analysis indicated moderate effectiveness at post-treatment for anxiety, although limited effectiveness at follow-up was found among more clinically representative samples. Studies that reported greater effectiveness tended to be of lower methodological quality and generally involved participants who were self-selected rather than recruited through clinical referrals.
Other meta-analytic reviews also show that self-help interventions in the treatment of anxiety disorders for adults produce improvements with a medium effect size, but with poor-to-moderate quality evidence.17,47,48,52,61,65,67–73 Some trials have failed to show significant improvements in symptoms when compared to control groups,74,75 while others indicate significant improvements, comparable to that of traditional face-to-face therapy interventions.76–81 Most studies, however, have significant methodological limitations, such as small sample sizes, high attrition rates, no control group, and limited control over whether participants were also seeking additional psychological treatments or were taking medications.52,65 The best outcomes have been demonstrated in the treatment of panic disorder and specific phobias.61,70 Overall, as stated by Bower et al,52 based on the Cochrane collaboration classification, self-help strategies for anxiety “appear promising but require further investigation.”
A review of self-help interventions for anxiety specifically for young people has not been undertaken. The current study aimed to redress this gap by conducting a systematic review of the literature on self-help interventions for anxiety disorders in young people to determine the state and nature of the current evidence base.
Methodology
A systematic review of the literature was undertaken by reviewing all studies that met the selection criteria for self- help interventions for anxiety for young people. Self- help interventions were defined as those that claimed to be self- help or self-administered, and did not involve a service or therapist-based therapy component or be based primarily on a parent-focused intervention. All anxiety disorders referred to as anxiety were included. Young people were defined as those aged 6–25 years. While the term “young people” usually denotes those aged 12–25 years,82 interventions aimed at those in the preadolescent years were also included because anxiety disorders are highly likely to first emerge in young people aged 6–11 years.4
Initially, a broad search strategy was implemented covering all studies published in English between January 1, 1970 and October 20, 2011 from the following EBSCO databases: Academic Search Complete, CINAHL Plus, Computers and Applied Sciences Complete, Education Research Complete, Health Source – Consumer Edition, Health Source – Nursing/Academic Edition, Humanities International Complete, MasterFILE Premier, MEDLINE, PsychArticles, Psychology and Behavioral Sciences Collection, Psych INFO, and Teacher Reference Center. The search terms used were: “anxiety” AND “self-help” OR “self help” OR “bibliotherapy” OR “self-administered” OR “therapist guided” OR “young people”; “anxiety” AND “children” AND “self-help”; “mental disorder” AND “self-help”; “self-help” AND “young people” OR “adolesc*”; “anxiety” AND “prevention” OR “early intervention.” Further studies were identified through hand searching the references of relevant studies and reviews.
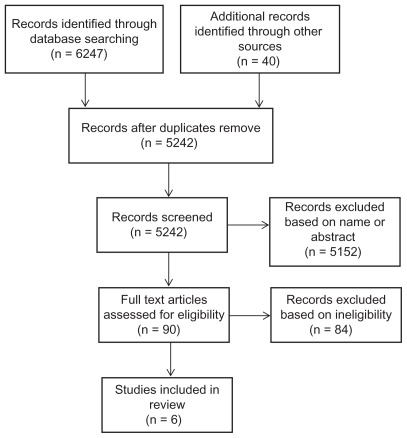
Following the database search, abstracts and titles were scanned independently by both authors and irrelevant studies were removed; the remaining full text articles were assessed for eligibility. The final eligibility criteria were that the study: examined a type of self-help intervention for an anxiety disorder; was published after 1995; involved participants aged between 6–25 years; had little or no parental involvement; was published in English; had more than one participant (ie, not single case studies); and comprised an outcome study with a focus on change in a measure of anxiety. Acceptable designs included randomized controlled trials (RCT), quasi-experimental trials, pre-post test case series, and longitudinal designs all able to be included. Figure 1 shows the Prisma flow diagram for study inclusion.
Figure 1.
Prisma flow diagram.
Results
A total of six studies met the inclusion criteria and a summary of each is provided in Table 1. These studies involved three interventions that are available to the general public – MoodGym,83 CoolTeens CD-ROM,15 the Online Anxiety Prevention Program,84,85 and three interventions that are not publicly available – an internet-based CBT program,86 a computer-based Cognitive-Behavioral Analysis System of Psychotherapy (CBASP),87 and a series of self-administered interventions for worry.88 Four of the studies were RCTs,83–86,88 comparing the intervention group(s) with a wait-list control (WLC) group and one was a small sample case series design.15
Table 1.
Study characteristics
| Study | Sample | Intervention | Design | Attrition | Main findings |
|---|---|---|---|---|---|
| Cukrowicz and Joiner87 | Undergraduate psychology students Age 95% between 18–21 years (M = 19.2, SD = 1.9) Beck anxiety inventory scores ≤18; and Beck depression inventory scores ≤19 n = 231 (169 female, 69 male) |
CBASP 6 × 20 minutes sessions completed in one 2-hour time frame (with a 10-minute break half way through) Weekly emails for 8 weeks following intervention reminding participants to practice learned skills Note. Although intervention was completed individually, all participants were in the same lab when completing the program |
RCT CBASP intervention Educational program as control |
90% return rate | Significantly lower scores on measures of depression and anxiety for intervention group when compared to control group at follow-up. Cohen’s d effect sizes ranged from small to medium for outcome measures. |
| Cunningham et al15 | Age 14–16 years Primary diagnosis of anxiety disorder n = 5 (4 female, 1 male) |
“Cool Teens” CD-ROM 8 sessions over 12-week period 15–30 minutes per session Fortnightly phone contact with psychologist questioned progress and understanding of material, provided motivation and clarified issues |
Case series | 4/5 completed at least 6 of the 8 modules | After completion, 40% (n = 2) were at subclinical levels for anxiety, 2 showed some improvement, and 1 showed no change. At 3 months, 40% (n = 2) did not meet anxiety diagnosis criteria. All participants were generally satisfied with program. Participants identified “finding time” as a completion barrier. |
| Kenardy et al84 | First year psychology students (M = 19.92 years) Diagnosis of anxiety (scored >24 on Anxiety Sensitivity Index) n = 83 (43 intervention, 40 control) |
“Online Anxiety Prevention Program” Based on SERENA software for palmtop computers 6 sessions over 6 weeks |
RCT Wait-list control Intervention group |
Significant improvements on the Agoraphobic Cognitions Questionnaire, Catastrophic Cognitions Questionnaire-Modified, and the Centre for Epidemiologic Studies Depression Scale when compared to control group. No significant differences on the Anxiety Sensitivity Index or the Body Sensations Questionnaire. Improvements on Agoraphobic Cognitions Questionnaire, Catastrophic Cognitions Questionnaire-Modified, and Centre for Epidemiologic Studies Depression Scale remained at 6-month follow-up (53% retained in intervention group and 61% in control group at follow-up). |
|
| Sethi et al83 | First year undergraduate students Age 18–23 years (M = 19.47, SD = 1.57) Diagnosis of low to moderate depression or anxiety n = 38 (25 female, 13 male) |
“MoodGYM” 5 sessions over 3 weeks 30–45 minutes per session |
RCT Face-to-face CBT MoodGYM in conjunction with face-to-face CBT MoodGYM alone Wait-list control |
Significant reductions in anxiety as rated by the Depression Anxiety Stress Scale (DASS-21) in the combined MoodGYM and face-to-face CBT group when compared to all other groups. Significant improvements in DASS-21 scores for both face-to-face CBT and MoodGYM alone when compared to control group. Differences between groups non-significant No improvements pre- to post-on the DASS-21 for the control group. |
|
| Tillfors et al86 | High school students Age 15–21 years (M = 16.5, SD = 1.6) n = 19 (17 female, 2 male) |
Internet delivered CBT program 9 modules over 9 weeks Weekly email feedback from therapist If no contact from participant in 2-week time frame the therapist phoned the participant to assess reasons why |
RCT Treatment group Wait-list control |
Follow-up measures obtained from 15 participants Only 4 participants completed 3 or more modules 1 participant completed 5–6 modules No participant completed 7 or more modules |
Significant improvements on measures of social anxiety when compared to control group. Non-significant findings for measures of social avoidance and quality of life. |
| Wolitzky-Taylor and Telch88 | College students moderate levels of academic worry n = 113 |
Expressive writing, worry exposure or audio-photic stimulation 12 sessions of 20 minutes Participants instructed to self-administer treatment |
RCT Guided worry exposure Expressive writing Audio-photic stimulation Wait-list control |
84 participants completed at least 1/3 of the recommended home sessions On average only half of participants completed all home expressive writing sessions |
All three treatment conditions reduced academic worry and general anxiety Slightly better outcomes for worry exposure. Delayed outcome for expressive writing Outcomes maintained at 3-month follow-up. |
Abbreviations: CBASP, cognitive-behavioral analysis system of psychotherapy; RCT, randomized controlled trials; CBT, cognitive-behavioral therapy.
Cognitive-behavioral analysis system of psychotherapy
Cukrowicz and Joiner87 adapted CBASP into a computer-based program to determine whether it could be used as a self-help approach to reducing mild symptoms of anxiety and depression. CBASP asks participants to analyze specific incidents to determine and change patterns of maladaptive thinking and behaving. It involves five steps: description of the situation; interpretation of the situation; behaviors during the situation; actual outcome of the situation; and desired outcome of the situation. In the study, 231 young adults were randomly assigned to CBASP or an education program control group. The intervention comprised six, 20 minute sessions which were all completed in one 2-hour time frame undertaken in a computer laboratory at the university. Following the intervention, participants were sent weekly emails for 8 weeks reminding them to practice the skills they had learnt. The control group completed a program of similar length that focused on educational material around anxiety disorders. At the 8-week follow-up, participants in the intervention group had significantly lower scores on the measures of anxiety when compared to the control group. The effect size for the reduction in anxiety was moderate; on average, anxiety levels of participants in the intervention group reduced by half a standard deviation point following the intervention.
Although the sample size was large in this study, and there was a low attrition rate of 10%, it is difficult to generalize these completion rates to the wider population. The sample was predominately female, and obtained from an introductory psychology course where participants received course credit for completion. In addition, although the program was conducted independently, it was completed at a specified time with researchers and other participants present. This is likely to have greatly increased the completion rates and does not indicate how many young people are likely to independently complete this program at home.
Online anxiety prevention program
Studies by Kenardy et al84,85 investigated the Online Anxiety Prevention Program, which is a computer assisted CBT-based intervention comprising six sessions that incorporate psychoeducation about anxiety, relaxation training, interoceptive exposure, cognitive restructuring, and relapse prevention. Each session required participants to cover the program material, practice a set of skills, and record their progress daily. The study used 83 first year university students high on a measure of anxiety sensitivity who were randomly assigned to an intervention or WLC group. At 6-week follow-up, those in the intervention group showed improvements in some outcome measures, but not the Anxiety Sensitivity Index measure.84 At 6 months, 53% of the intervention group and 61% of the control group were followed up.85 Significant decreases in anxiety sensitivity were evident for both the control and intervention group participants. The study was significantly limited by its mostly adult and university population sample group, small sample size, and lack of significant findings.
MoodGYM
MoodGYM is a free internet-based CBT intervention developed by researchers at the Australian National University and designed to treat anxiety and depression.89 The program was originally developed for adults, is accessible 24 hours a day and is self-paced. It consists of five CBT modules that take approximately 30–45 minutes each to complete, a personal workbook that records and updates user’s responses, an interactive game, and a feedback evaluation form.
The study by Sethi et al83 was an RCT using 38 first year undergraduate psychology students (aged 18–23 years) randomized into four conditions: MoodGYM as a pure self-help intervention; MoodGYM in conjunction with face-to-face therapy; a traditional face-to-face therapy group; and a control group. At 5-week post-test, there was no change in anxiety for participants in the control group, and those in the MoodGYM only condition had significantly decreased anxiety scores with a medium effect size compared with the control group. A similar decrease was evident for those in the traditional face-to-face therapy group. However, the greatest reduction in anxiety was achieved in the combined condition where MoodGYM was provided in conjunction with face-to-face therapy. The study authors suggest that meeting with a therapist first and then using MoodGYM motivates the user to do well on the self-help program and allows for skills to be practiced, leading to superior outcomes.
There were considerable limitations to this study, however. Foremost, the sample was made up of university students undertaking the study for credit points. Participants undertook the self-help component in group sessions at the university. Furthermore, no follow-up data were obtained to determine whether treatment gains were maintained.
Internet CBT
Tillfors et al86 examined the effectiveness of an internet-based CBT program for social anxiety that was developed for use with adult university students and adapted for use with high school students. There were nine weekly modules that each consisted of information, exercises, and essay questions. Each week, participants were also asked to summarize in their own words a section of the module, describe the outcome of the exercises, and answer an interactive multiple-choice quiz. In the study, 19 speech-anxious high school students with SAD were randomly assigned to the intervention or a WLC group. Participants received a weekly email with therapist feedback. Significant improvements were found on measures of social anxiety, general anxiety, and depression, with a large effect size, and these were maintained at 1-year follow-up. No improvements were evident for social avoidance or quality of life measures.
Although large effects were evident in this study, it comprised a small sample of highly selected high school students, who were mostly females. Furthermore, only four participants completed more than two modules and none completed all nine modules during the study period. The authors argue that components central to obtaining therapeutic effects, such as cognitive restructuring, behavior experiments, exposure, modifying safety behaviors, and shifting of focus are provided early in the treatment, and that working on these components could lead to improvements despite limited exposure to the program.
Self-administered approaches for worry
Three self-administered approaches to treating pathological worry among college students were investigated in the study by Wolitzky-Taylor and Telch.88 The study evaluated the efficacy of worry exposure, expressive writing, and relaxation consisting of pulsed audio-photic stimulation. There were 113 college students randomly assigned to one of the three interventions, which were practiced three times per week for 1 month, compared with a WLC. Academic worry and general anxiety were assessed at baseline, post-test, and at a 3-month follow-up. The pre- to post-treatment effect sizes for the primary outcome measure of academic worry were large for each of the three interventions and significantly larger than that observed for the WLC group. Each intervention led to significant reductions in general worry, with a large effect size for worry exposure and moderate effects for expressive writing group and audio-photic stimulation. Improvements in all three treatments continued at 3-month follow-up, with greater improvement from post-test to follow-up for the expressive writing group.
Treatment compliance was a concern in this study, with those in the audio-photic stimulation condition completing about two-thirds of the twelve assigned home practice sessions, whereas those assigned to worry exposure or expressive writing completed on average only about half of the sessions. The sample was primarily female and all college students.
CoolTeens
Only one trial was not an RCT, and this was a case series study investigating the CoolTeens CD-ROM,15 which is a computerized self-help program adapted from previously validated bibliotherapy and group therapy programs.15,90 It has eight modules which each take 30–60 minutes to complete. Modules are designed to be completed on a weekly or fortnightly basis over an 8- to 12-week period. The trial was a very small sample study of only five participants diagnosed with anxiety, using a pre-post design. Significant positive outcomes were found for two of the participants, who were identified as having anxiety levels that had dropped to sub-clinical level at post-treatment. Two other participants showed positive gains in some areas, and one showed no change. Two participants no longer met the criteria for an anxiety disorder at the 3-month follow-up.
Excluded interventions
Some interventions that were excluded by the selection criteria are worth mention. The BRAVE interventions were excluded because of the high level of parental and trainer involvement. BRAVE for Children-ONLINE (8–12 year olds) and BRAVE for Teenagers-ONLINE (13–17 year olds), are anxiety treatment programs designed to treat SAD, generalized anxiety disorder, separation anxiety disorder, and specific anxiety disorders using CBT.91 BRAVE for Children-ONLINE consists of 10 weekly sessions in the initial treatment schedule, backed up by a booster session at 1 and 3 months post intervention. There are also six sessions to be completed by parents. BRAVE for Teenagers-ONLINE consists of 13 weekly sessions, two booster sessions and seven parent sessions. In both interventions users are supported by a BRAVE trainer who helps guide and motivate users through the intervention by providing weekly contact via email and/or over the phone.92 Specific techniques used within the program include relaxation training, identification of emotions and thoughts, positive self-talk, coping skills, problem solving, and approaching feared situations. A randomized-control study of BRAVE for Children-ONLINE found that the treatment had moderate levels of consumer satisfaction and high levels of credibility.93 At post-treatment 30% of children in the trial group no longer met the criteria for an anxiety disorder, compared to 10% of children in the control group. At a 6-month follow-up, the number of children in the treatment group no longer meeting the diagnostic criteria for an anxiety disorder had risen to 75%, however the control group was not tested at this time so it is unclear exactly how much of this improvement can be attributed to the treatment program. Notably, at post-treatment only 60% of parents and one-third of children had completed the entire intervention. Initial studies of the teen program using case samples indicate that it can successfully be used to treat young people with anxiety.92
The “Camp Cope-a-lot: The Coping Cat” CD-ROM is designed for children aged 7–12 years, and was excluded because it is designed to be used in conjunction with a mental health professional. It uses “Flash” animation and interactive activities with an inbuilt reward system to deliver CBT.94 The guide character, “Charlie,” teaches users about anxiety, physiological symptoms, relaxation techniques, coping, and problem solving strategies, as well as walking users through step-by-step exposure tasks. The professional does not need to be trained or experienced in CBT, however. Initial case studies of the program have had positive outcomes.95
Discussion
Surprisingly, the literature search revealed very little research evidence currently available regarding the effectiveness of self-help interventions to treat mild anxiety in young people. Although initially a large number of published papers were extracted from the database search, most of these did not meet the search criteria. In particular, very few studies were undertaken with young people specifically, and those that did focus on children or youth generally included considerable therapist involvement and could not be considered self-help. The six studies that remained showed mixed results, although most reported medium sized effects. These studies comprise a very poor evidence base for self-help for young people with anxiety; the outcomes were based mostly on findings with young adult female university students and had low treatment compliance and high attrition rates.
Similar methodological issues have been identified in reviews of self-help for anxiety with adults.52,55,65,74 Sample sizes were small, attrition rates were high, and little to no control was taken to prevent participants seeking outside treatment or medication. Whilst small to moderate improvements in anxiety symptoms were identified, the overall quality of the studies was poor. Consequently, all the evidence must be interpreted with caution.
Nevertheless, some important aspects of self-help interventions have been identified from the adult literature. Motivation of the user appears to be a very important aspect, with interventions that incorporate motivating tools, such as therapist or automatic reminders, having better outcomes than those that rely solely on the user.71,72,80,96 In particular, self-help programs that incorporate some form of therapist contact result in increased completion rates and improved outcomes when compared to pure self-help treatments,96–98 and traditional face-to-face interventions.70,76,99–103 It is possible that the improved outcomes occur because the user is more likely to be using a treatment that is appropriate for their individual issue.72 Only minimal therapeutic input appears to be required, however, to provide appropriate advice and encouragement,96 and this does not require the resources of highly skilled mental health professionals such as clinical psychologists.68,88,90 Little to no improvements in anxiety symptoms have been noted by increasing therapist support to more than once weekly contact.70,104 Furthermore, fewer, shorter, more frequent modules appear to produce better outcomes as rewards may occur more frequently.17,80
Reviews with adults generally conclude that the best outcomes appear to be achieved by combining self-help treatments with some form of face-to-face therapy.98,105 Self-help interventions might be best utilized in stepped-care plans with some form of face-to-face interaction as a source of motivation, and initial assessment by a mental health professional.
Finally, it is important to note that the self-help interventions available to the public are unlikely to have undergone rigorous research testing, and those that have undergone testing are unlikely to be widely available for public use. The current review showed that self-help books and commercially available self-help resources for young people had not been the subject of research evaluation. The best research evidence was for university-designed and administered interventions that are not widely available to the public.
Recommendations
There is an urgent need for effective prevention and early intervention for anxiety disorders in children, adolescents, and young adults to prevent the widespread debilitating effects of such mental health problems and progression to more serious illness. A great deal of further research is needed, however, and attention needs to focus on reasons for the lack of rigorous research in the field and high attrition rates in the few research studies. Foremost, the many self-help interventions that are already available to the public need to be the subject of good quality outcome-based research. Furthermore, self-help interventions that are developed through university research trials need to be able to be publicly available if they are shown to be efficacious. The role of support in the use of self-help interventions also needs to be examined. Using self-help as an adjunct to therapy, or in a guided manner with the support of skilled or semi-skilled mental health professionals, is beginning to receive research attention. The role of parents in self-help for young people also needs to be investigated, however, particularly for children and younger adolescents, but also in relation to encouraging older adolescents to effectively use self-help interventions. Receiving appropriate and effective treatment as early as possible in the development of anxiety disorders is essential to improving the mental health and well-being of young people as they grow into adulthood. Ways to encourage research attention to this important area of early intervention need to be found.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 3.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-Month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Arch Gen Psychiatry. 2003;60(11):1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- 6.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med. 1997;27(2):93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 7.Duchesne S, Vitaro F, Larose S, Tremblay R. Trajectories of anxiety during elementary-school years and the prediction of high school noncompletion. J Youth Adolesc. 2008;37(9):1134–1146. [Google Scholar]
- 8.Flannery-Schroeder EC. Reducing anxiety to prevent depression. Am J Prev Med. 2006;31(6 Suppl 1):136–142. doi: 10.1016/j.amepre.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, Berglund PA, Foster CL, Saunders WB, Stang PE, Walters EE. Social consequences of psychiatric disorders, II: Teenage parenthood. Am J Psychiatry. 1997;154(10):1405–1411. doi: 10.1176/ajp.154.10.1405. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. Am J Psychiatry. 1995;152(7):1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 11.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry. 2002;59(3):225–231. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 12.Strauss CC, Frame CL, Forehand R. Psychosocial impairment associated with anxiety in children. J Clin Child Psychol. 1987;16(3):235–239. [Google Scholar]
- 13.Frydenberg E, Lewis R. Teaching coping to adolescents: When and to whom? Am Educ Res J. 2000;37(3):727–745. [Google Scholar]
- 14.Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. AeJAMH. 2005;4(3 Suppl):218–251. [Google Scholar]
- 15.Cunningham M, Wuthrich VM, Rapee RM, Lyneham HJ, Schniering CA, Hudson JL. The Cool Teens CD-ROM for anxiety disorders in adolescents: a pilot case series. Eur Child Adolesc Psychiatry. 2009;18(2):125–129. doi: 10.1007/s00787-008-0703-y. [DOI] [PubMed] [Google Scholar]
- 16.Campbell LF, Smith TP. Integrating self-help books into psychotherapy. J Clin Psychol. 2003;59(2):177–186. doi: 10.1002/jclp.10140. [DOI] [PubMed] [Google Scholar]
- 17.Hirai M, Clum GA. Self-help therapies for anxiety disorders. In: Watkins KE, Clum GA, editors. Handbook of Self-Help Therapies. New York, NY: Routledge; 2008. pp. 77–108. [Google Scholar]
- 18.Albano AM, Kendall PC. Cognitive behavioural therapy for children and adolescents with anxiety disorders: clinical research advances. Int Rev Psychiatry. 2002;14:129–134. [Google Scholar]
- 19.Herbert JD, Gaudiano BA, Rheingold AA, et al. Cognitive behavior therapy for generalized social anxiety disorder in adolescents: a randomized controlled trial. J Anxiety Disord. 2009;23(2):167–177. doi: 10.1016/j.janxdis.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. Br J Clin Psychol. 2004;43(Pt 4):421–436. doi: 10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- 21.Tanielian T, Jaycox LH, Paddock SM, Chandra A, Meredith LS, Burnam MA. Improving treatment seeking among adolescents with depression: understanding readiness for treatment. J Adolesc Health. 2009;45(5):490–498. doi: 10.1016/j.jadohealth.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Slade T, Johnston A, Teesson M, et al. The Mental Health of Australians 2: Report on the 2007 National Survey of Mental Health and Wellbeing. Canberra Australia: Department of Health and Ageing; 2009. [Google Scholar]
- 23.Cheung AH, Dewa CS. Mental health service use among adolescents and young adults with major depressive disorder and suicidality. Can J Psychiatry. 2007;52(4):228–232. doi: 10.1177/070674370705200404. [DOI] [PubMed] [Google Scholar]
- 24.Oakley Browne MA, Wells JE, Scott KM, McGee MA. Lifetime prevalence and projected lifetime risk of DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):865–874. doi: 10.1080/j.1440-1614.2006.01905.x. [DOI] [PubMed] [Google Scholar]
- 25.Australian Bureau of Statistics. National Survey of Mental Health and Wellbeing: Summary of Findings. Canberra, Australia: Australian Bureau of Statistics; 2007. [Google Scholar]
- 26.US Surgeon General. Mental Health: Culture, Race and Ethnicity – A Supplement to Mental Health: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2001. [PubMed] [Google Scholar]
- 27.Zhang AY, Snowden LR, Sue S. Differences between Asian and White Americans’ help seeking and utilization patterns in the Los Angeles area. J Community Psychol. 1998;26(4):317–326. [Google Scholar]
- 28.Essau CA. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress Anxiety. 2005;22(3):130–137. doi: 10.1002/da.20115. [DOI] [PubMed] [Google Scholar]
- 29.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gould MS, Velting D, Kleinman M, Lucus C, Thomas JG, Chung M. Teenager’s attitudes about coping strategies and help-seeking behavior for suicidality. J Am Acad Child Adolesc Psychiarty. 2004;43(9):1124–1133. doi: 10.1097/01.chi.0000132811.06547.31. [DOI] [PubMed] [Google Scholar]
- 31.Wilson CJ, Deane FP, Ciarrochi J. Can hopelessness and adolescents’ beliefs and attitudes about seeking help account for help negation? J Clin Psychol. 2005;61(12):1525–1539. doi: 10.1002/jclp.20206. [DOI] [PubMed] [Google Scholar]
- 32.Eisenberg D, Downs MF, Golberstein E, Zivin K. Stigma and help seeking for mental health among college students. Med Care Res Rev. 2009;66(5):522–541. doi: 10.1177/1077558709335173. [DOI] [PubMed] [Google Scholar]
- 33.Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- 34.Deane FP, Wilson CJ, Ciarrochi J. Suicidal ideation and help-negation: Not just hopelessness or prior help. J Clin Psychol. 2001;57(7):901–914. doi: 10.1002/jclp.1058. [DOI] [PubMed] [Google Scholar]
- 35.Fallon BJ, Bowles T. Adolescent help-seeking for major and minor problems. Aust J Psychol. 1999;51(1):12–18. [Google Scholar]
- 36.Valkenburg PM, Sumter SR, Peter J. Gender differences in online and offline self-disclosure in pre-adolescence and adolescence. Br J Dev Psychol. 2011;29(2):253–269. doi: 10.1348/2044-835X.002001. [DOI] [PubMed] [Google Scholar]
- 37.Angst J, Gamma A, Gastpar M, Lepine JP, Mendlewicz J, Tylee A. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci. 2002;252:201–209. doi: 10.1007/s00406-002-0381-6. [DOI] [PubMed] [Google Scholar]
- 38.Korp P. Health on the internet: implications for health promotion. Health Educ Res. 2006;21(1):78–86. doi: 10.1093/her/cyh043. [DOI] [PubMed] [Google Scholar]
- 39.Kelly CM, Jorm AF, Wright A. Improving mental health literacy as a strategy to facilitate early intervention for mental disorders. Med J Aust. 2007;187(7):S26–S30. doi: 10.5694/j.1326-5377.2007.tb01332.x. [DOI] [PubMed] [Google Scholar]
- 40.Rickwood D, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust. 2007;187(7):S35–S39. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- 41.Ciarrochi J, Heaven PC, Supavadeeprasit S. The link between emotion identification skills and socio-emotional functioning in early adolescence: a 1-year longitudinal study. J Adolesc. 2008;31(5):565–582. doi: 10.1016/j.adolescence.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 42.Buston K. Adolescents with mental health problems: what do they say about health services? J Adolesc. 2002;25(2):231–242. doi: 10.1006/jado.2002.0463. [DOI] [PubMed] [Google Scholar]
- 43.Sayal K. Annotation: Pathways to care for children with mental health problems. J Child Psychol Psychiatry. 2006;47(7):649–659. doi: 10.1111/j.1469-7610.2005.01543.x. [DOI] [PubMed] [Google Scholar]
- 44.Sawyer MG, Arney FM, Baghurst PA, et al. The mental health of young people in Australia: key findings from the child and adolescent component of the national survey of mental health and well-being. Aust N Z J Psychiatry. 2001;35(6):806–814. doi: 10.1046/j.1440-1614.2001.00964.x. [DOI] [PubMed] [Google Scholar]
- 45.Holmes JM, March S, Spence SH. Use of the internet in the treatment of anxiety disorders with children and adolescents. Counselling, Psychotherapy, and Health. 2009;5(1):187–231. [Google Scholar]
- 46.Steinberg L, Silverberg SB. The vicissitudes of autonomy in early adolescence. Child Dev. 1986;57(4):841–851. doi: 10.1111/j.1467-8624.1986.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 47.Griffiths KM, Christensen H. Internet-based mental health programs: a powerful tool in the rural medical kit. Aust J Rural Health. 2007;15(2):81–87. doi: 10.1111/j.1440-1584.2007.00859.x. [DOI] [PubMed] [Google Scholar]
- 48.Moritz S, Wittekind CE, Hauschildt M, Timpano KR. Do it yourself? Self-help and online therapy for people with obsessive-compulsive disorder. Curr Opin Psychiatry. 2011;24(6):541–548. doi: 10.1097/YCO.0b013e32834abb7f. [DOI] [PubMed] [Google Scholar]
- 49.Calear AL, Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med J Aust. 2010;192(11 Suppl):S12–S14. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- 50.Barak A, Klein B, Proudfoot JG. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009;38(1):4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- 51.Tate DF, Zabinski MF. Computer and Internet applications for psychological treatment: update for clinicians. J Clin Psychol. 2004;60(2):209–220. doi: 10.1002/jclp.10247. [DOI] [PubMed] [Google Scholar]
- 52.Bower P, Richards D, Lovell K. The clinical and cost-effectiveness of self-help treatments for anxiety and depressive disorders in primary care: a systematic review. Br J Gen Pract. 2001;51(471):838–845. [PMC free article] [PubMed] [Google Scholar]
- 53.Pantalon MV. Use of self-help books in the practice of clinical psychology. In: Salkovskis P, editor. Adults: Clinical Formulation and Treatment. Vol. 6. New York, NY: Elsevier Science; 1998. pp. 265–276. [Google Scholar]
- 54.Elgar FJ, McGrath PJ. Self-administered psychosocial treatments for children and families. J Clin Psychol. 2003;59(3):321. doi: 10.1002/jclp.10132. [DOI] [PubMed] [Google Scholar]
- 55.Lewis G, Anderson L, Araya R, et al. Report to the Department of Health R&D Programme. London, UK: 2004. Self-help interventions for mental health problems. [Google Scholar]
- 56.Brantley J. Calming Your Anxious Mind: How Mindfulness and Compassion Can Free You From Anxiety, Fear and Panic. Oakland, CA: New Harbinger Publications; 2003. [Google Scholar]
- 57.Rapee RM, Wignall A, Spence SH, Cobham V, Lyneham HJ. Helping Your Anxious Child: A Step-by-Step Guide for Parents. 2nd ed. Oakland, CA: New Harbinger Publications; 2008. [Google Scholar]
- 58.Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: A randomized controlled trial. J Consult Clin Psychol. 2006;74(3):436–444. doi: 10.1037/0022-006X.74.3.436. [DOI] [PubMed] [Google Scholar]
- 59.Chansky TE. Freeing Your Child From Anxiety: Powerful, Practical Solutions to Overcome Your Child’s Fears, Worries, and Phobias. New York, NY: Broadway Books; 2004. [Google Scholar]
- 60.Carter F, Cheesman P. Anxiety in Childhood and Adolescence. New York, NY: Croom Helm; 1988. [Google Scholar]
- 61.Hirai M, Clum GA. A meta-analytic study of self-help interventions for anxiety problems. Behav Ther. 2006;37(2):99–111. doi: 10.1016/j.beth.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 62.Marks I, Cavanagh K. Computer-aided psychological treatments: evolving issues. Ann Rev Clin Psychol. 2009;5:121–141. doi: 10.1146/annurev.clinpsy.032408.153538. [DOI] [PubMed] [Google Scholar]
- 63.Cavanagh K, Shapiro DA. Computer treatment for common mental health problems. J Clin Psychol. 2004;60(3):239–251. doi: 10.1002/jclp.10261. [DOI] [PubMed] [Google Scholar]
- 64.Edwards-Hart T, Chester A. Online mental health resources for adolescents: overview of research and theory. Aust Psychol. 2010;45(3):223–230. [Google Scholar]
- 65.Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J. A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety. Health Technol Assess. 2003;6(22):1–100. doi: 10.3310/hta6220. [DOI] [PubMed] [Google Scholar]
- 66.Coull G, Morris PG. The clinical effectiveness of CBT-based guided self-help interventions for anxiety and depressive disorders: a systematic review. Psychol Med. 2011;41(11):2239–2252. doi: 10.1017/S0033291711000900. [DOI] [PubMed] [Google Scholar]
- 67.Marrs R. A meta-analysis of bibliotherapy studies. Am J Community Psychol. 1995;23(6):843–870. doi: 10.1007/BF02507018. [DOI] [PubMed] [Google Scholar]
- 68.Menchola M, Arkowitz HS, Burke BL. Efficacy of self-administered treatments for depression and anxiety. Prof Psychol Res Pr. 2007;38(4):421–429. [Google Scholar]
- 69.Scogin F, Bynum J, Stephens G, Calhoon S. Efficacy of self-administered treatment programs: meta-analytic review. Prof Psychol Res Pr. 1990;21(1):42–47. [Google Scholar]
- 70.Newman MG, Erickson T, Przeworski A, Dzus E. Self-help and minimal-contact therapies for anxiety disorders: Is human contact necessary for therapeutic efficacy? J Clin Psychol. 2003;59(3):251–274. doi: 10.1002/jclp.10128. [DOI] [PubMed] [Google Scholar]
- 71.Mains JA, Scogin FR. The effectiveness of self-administered treatments: a practice-friendly review of the research. J Clin Psychol. 2003;59(2):237–246. doi: 10.1002/jclp.10145. [DOI] [PubMed] [Google Scholar]
- 72.Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of internet-based psychotherapeutic inteventions. J Technol Human Serv. 2008;26(2–4):109–160. [Google Scholar]
- 73.Cuijpers P, Marks IM, van Straten A, Cavanagh K, Gega L, Andersson G. Computer-aided psychotherapy for anxiety disorders: a meta-analytic review. Cogn Behav Ther. 2009;38(2):66–82. doi: 10.1080/16506070802694776. [DOI] [PubMed] [Google Scholar]
- 74.Fletcher J, Lovell K, Bower P, Campbell M, Dickens C. Process and outcome of a non-guided self-help manual for anxiety and depression in primary care: a pilot study. Behav Cogn Psychother. 2005;33(3):319–331. [Google Scholar]
- 75.Holdsworth N, Paxton R, Seidel S, Thomson D. Parallel evaluations of new guidance materials for anxiety and depression in primary care. J Ment Health. 1996;5(2):195–207. [Google Scholar]
- 76.Carr AC, Ghosh A, Marks IM. Computer-supervised exposure treatment for phobias. Can J Psychiatry. 1988;33(2):112–117. doi: 10.1177/070674378803300208. [DOI] [PubMed] [Google Scholar]
- 77.Nordin S, Carlbring P, Cuijpers P, Andersson G. Expanding the limits of bibliotherapy for panic disorder: randomized trial of self-help without support but with a clear deadline. Behav Ther. 2010;41(3):267–276. doi: 10.1016/j.beth.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 78.Febbraro GA. An investigation into the effectiveness of bibliotherapy and minimal contact interventions in the treatment of panic attacks. J Clin Psychol. 2005;61(6):763–779. doi: 10.1002/jclp.20097. [DOI] [PubMed] [Google Scholar]
- 79.Watkins PL. Manualized treatment of panic disorder in a medical setting: two illustrative case studies. J Clin Psychol Med Settings. 1999;6(4):353–372. [Google Scholar]
- 80.Carlbring P, Ekselius L, Andersson G. Treatment of panic disorder via the Internet: a randomized trial of CBT vs applied relaxation. J Behav Ther Exp Psychiatry. 2003;34(2):129–140. doi: 10.1016/s0005-7916(03)00026-0. [DOI] [PubMed] [Google Scholar]
- 81.Lidren DM, Watkins PL, Gould RA, Clum GA, Asterino M, Tulloch HL. A comparison of bibliotherapy and group therapy in the treatment of panic disorder. J Consult Clin Psychol. 1994;62(4):865–869. doi: 10.1037//0022-006x.62.4.865. [DOI] [PubMed] [Google Scholar]
- 82.National Collaborative on Workforce and Disability (NCWD) For Youth. 2002. [Accessed November 11, 2011]. Available from: http://www.ncwd-youth.info/taxonomy/term/865.
- 83.Sethi S, Campbell AJ, Ellis LA. The use of computerized self-help packages to treat adolescent depression and anxiety. J Technol Human Serv. 2010;28(3):144–160. [Google Scholar]
- 84.Kenardy J, McCafferty K, Rosa V. Internet-delivered indicated prevention for anxiety disorders: a randomized controlled trial. Behav Cogn Psychother. 2003;31(3):279–289. [Google Scholar]
- 85.Kenardy J, McCafferty K, Rosa V. Internet-delivered indicated prevention for anxiety disorders: six-month follow-up. Clin Psychol. 2006;10(1):39–42. [Google Scholar]
- 86.Tillfors M, Andersson G, Ekselius L, et al. A randomized trial of internet-delivered treatment for social anxiety disorder in high school students. Cogn Behav Ther. 2011;40(2):147–157. doi: 10.1080/16506073.2011.555486. [DOI] [PubMed] [Google Scholar]
- 87.Cukrowicz KC, Joiner TE., Jr Computer-based intervention for anxious and depressive symptoms in a non-clinical population. Cogn Ther Res. 2007;31(5):677–693. [Google Scholar]
- 88.Wolitzky-Taylor KB, Telch MJ. Efficacy of self-administered treatments for pathological academic worry: a randomized controlled trial. Behav Res Ther. 2010;48(9):840–850. doi: 10.1016/j.brat.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 89.Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. J Med Internet Res. 2002;4(1):e3. doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cunningham M, Wuthrich V. Examination of barriers to treatment and user preferences with computer-based therapy using the Cool Teens CD for adolescent anxiety. E J Appl Psychol. 2008;4(2):12–17. [Google Scholar]
- 91.Sears HA. Adolescents in rural communities seeking help: who reports problems and who sees professionals? J Child Psychol Psychiatry. 2004;45(2):396–404. doi: 10.1111/j.1469-7610.2004.00230.x. [DOI] [PubMed] [Google Scholar]
- 92.Spence SH, Donovan CL, March S, et al. Online CBT in the treatment of child and adolescent anxiety disorders: Issues in the development of BRAVE-ONLINE and two case illustrations. Behav Cogn Psychother. 2008;36(4):411–430. [Google Scholar]
- 93.March S, Spence SH, Donovan CL. The efficacy of an internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J Pediatr Psychol. 2009;34(5):474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- 94.Khanna M, Aschenbrand SG, Kendall PC. New frontiers: computer technology in the treatment of anxious youth. Behav Ther. 2007;30(1):22–25. [Google Scholar]
- 95.Khanna MS, Kendall PC. Computer-assisted CBT for child anxiety: the coping cat CD-ROM. Cogn Behav Pract. 2008;15(2):159–165. [Google Scholar]
- 96.Ghosh A, Marks IM, Carr AC. Therapist contact and outcome of self-exposure treatment for phobias. A controlled study. Br J Psychiatry. 1988;152:234–238. doi: 10.1192/bjp.152.2.234. [DOI] [PubMed] [Google Scholar]
- 97.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37(3):319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 98.Klein B, Richards JC, Austin DW. Efficacy of internet therapy for panic disorder. J Behav Ther Exp Psychiatry. 2006;37(3):213–238. doi: 10.1016/j.jbtep.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 99.Carlbring P, Nilsson-Ihrfelt E, Waara J, et al. Treatment of panic disorder: live therapy vs. self-help via the Internet. Behav Res Ther. 2005;43(10):1321–1333. doi: 10.1016/j.brat.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 100.Richards A, Barkham M, Cahill J, Richards D, Williams C, Heywood P. PHASE: A randomised, controlled trial of supervised self-help cognitive behavioural therapy in primary care. Br J Gen Pract. 2003;53:764–770. [PMC free article] [PubMed] [Google Scholar]
- 101.Kiropoulos LA, Klein B, Austin DW, et al. Is internet-based CBT for panic disorder and agoraphobia as effective as face-to-face CBT? J Anxiety Disord. 2008;22(8):1273–1284. doi: 10.1016/j.janxdis.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 102.Kenwright M, Liness S, Marks I. Reducing demands on clinicians by offering computer-aided self-help for phobia/panic. Br J Psychiatry. 2001;179(5):456–459. doi: 10.1192/bjp.179.5.456. [DOI] [PubMed] [Google Scholar]
- 103.Greist JH, Marks IM, Baer L, et al. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. J Clin Psychiatry. 2002;63(2):138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- 104.Klein B, Austin D, Pier C, et al. Internet-based treatment for panic disorder: does frequency of therapist contact make a difference? Cogn Behav Ther. 2009;38(2):100–113. doi: 10.1080/16506070802561132. [DOI] [PubMed] [Google Scholar]
- 105.Farrand P. Development of a supported self-help book prescription scheme in primary care. Primary Care Mental Health. 2005;3(1):61–66. [Google Scholar]