The obesity epidemic in the United States is escalating, especially among persons of color (1), those living in poverty (2), and residents of rural communities (3). Obesity rates among children from racial and ethnic minority groups exceed those of white children by as many as 10 to 12 percentage points (4). In 2003–2004, Mexican-American children aged 6 to 11 years were 1.3 times as likely as non-Hispanic white children to be overweight, and American Indian/Alaskan Natives were 1.6 times as likely as non-Hispanic whites to be obese (5). Among youth aged 6 to 19 years, the obesity prevalence was at least 50% higher in the Mexican-American and African-American non-Hispanic populations than in the white non-Hispanic populations (5). According to the Healthy People 2010 Midcourse Review, obesity rates among all youth are increasing and moving away from target goals (6).
RISK FACTORS FOR OBESITY
Experts agree that when research is conducted on health disparities in areas such as obesity, ethnic variation should not be studied alone. Rather, demographic, social structure, and environmental variables should also be considered (7). Major disparities exist in different physical and social environments in the United States, and these factors account for 20% to 25% of the variations in obesity-related morbidity and mortality (8). Specifically, overweight and obesity inequities are experienced by lower income families and persons living in rural areas. Among youth aged 6 to 19 years of age, 20% of those in lower income households (ie, an income ≤130% of the poverty threshold) are overweight or obese, in contrast to 16% of youth in higher income households (>130% of poverty threshold) (9). Although no nationally representative data are available, Rural Healthy People 2010 reports findings from eight studies conducted across eight states, which indicate that childhood and adolescent obesity is more prevalent in rural communities than in other communities across the United States. (3). This is a change from previous findings that obesity is mainly found in urban environments (3).
There is substantial evidence that being an ethnic minority, being poor, and living in a rural community are unfavorable risk factors for obesity in childhood. Because the foundations of adult health, productivity, and well-being are established early on, childhood is an important time to intervene with the aim of improving population health and reducing health disparities (10). Given these risk factors for excess weight and what we know about the health effects of overweight and obesity, large scale public health approaches are required to eliminate these inequities.
EXISTING KNOWLEDGE ABOUT NUTRITION-RELATED POLICIES AND PRACTICES IN SCHOOLS
Policies are often more permanent than public health programs and are seen as having the greatest potential to eliminate obesity and health disparities. A recent national obesity prevention policy approach is the 2005 US Department of Agriculture School Wellness Initiative. This initiative requires schools to adopt, implement, and evaluate nutrition and activity policies.
Surveillance of Nutrition-Related Policies and Practices in Schools
Two major US public surveillance systems give us insight into the prevalence of school wellness policies and practices. These systems are the School Health Practices and Policies Study (11) and the School Health Profiles Study (12). Both have been sponsored by the Centers for Disease Control and Prevention since 1994.
The School Health Practices and Policies Study provides a nationally representative sample every 6 years. State-, district-, school-, and classroom-level data are collected from the person responsible for coordinating and/or delivering school health programs. Data are collected through computer-assisted telephone interviews and self-administered mailed questionnaires. Information about health education, physical education, health services, mental health and social services, nutrition services, and faculty and staff health promotion topics are collected across elementary, middle, and high schools. In 2006, 100% of states, 75% of districts (n = 538), 78% of schools (n = 1,103), and 94% of classrooms (n = 1,194) randomly selected for participation in the School Health Practices and Policies Study did so. The data are publicly available, with the state as the lowest level identifier.
The School Health Profiles Study is a state-driven and state-owned biennial survey of public school principals and lead health educators in secondary schools. This mailed, self-administered survey assesses school health policies and education related to many variables: physical activity, competitive foods, food service, reproductive health, tobacco prevention, violence prevention, and human immunodeficiency virus/acquired immunodeficiency syndrome prevention. State and school participation is voluntary and confidential. States use various methods to improve their response rate, including e-mail messages and telephone calls. States can choose to conduct a census (all schools participate) or sampling approach. In 2004, 32 states participated, resulting in a principal/school sample size of 6,101, with response rates of 71% to 100%. Most states give the Centers for Disease Control and Prevention permission to share their de-identified data set (participating schools not named).
These rich data sources will be helpful for determining the equity in distribution of school policies and practices by a limited number of demographic indictors.
Prevalence of Nutrition Standards, Healthful Eating Strategies, and Marketing Policies and Practices in Schools
In response to the US Department of Agriculture School Wellness Initiative, many federal, association, and industry agencies have made recommendations to schools on how they can help turn around the obesity trajectory (13). One consistently agreed upon recommendation is to establish nutrition standards for all foods and beverages available at school. The Institute of Medicine commissioned a study to review and provide recommendations for nutrition standards of foods and beverages available at school (14). Progress toward these recommendations can be monitored by the School Health Practices and Policies Study and School Health Profiles Study. For example, the 2006 School Health Practices and Policies Study data illustrate the common availability of cookies (78%), soda (98%), and chips (69%) in secondary schools. Moreover, the availability of these junk food venues has been negatively correlated with student fruit consumption (15). The School Health Practices and Policies Study 2006 results also indicate that only 30% to 39% of all districts require that schools prohibit junk foods in ala carte or vending venues; an additional 29% to 30% of districts recommend (but do not require) that schools do this (16). States vary widely in the prevalence of other nutrition policies and practices. For example, 7% to 37% of districts require or recommend that a fruit or nonfried vegetable be served when foods are offered at school celebrations (16).
There is evidence that strategies to encourage healthful eating in schools—pricing, energy posting, and student participation in taste testing—are feasible. New additions to the 2008 School Health Profiles Study questionnaires will allow assessment of policies and practices related to healthful eating strategies and school-based marketing and advertising. The Changing Individuals’ Purchase of Snacks study examined the effect of price reductions on sales of fresh fruit and vegetables in school cafeterias at 12 secondary schools in Minnesota (17). Fresh fruit and baby carrots were targeted for 50% price reductions. Results showed that during the price reduction period, sales of fresh fruit increased four-fold, and sales of baby carrots increased twofold. Evidence that energy content posting will affect purchasing behaviors is mixed, and the topic is controversial. One case study is underway in New York City, where a menu-labeling law was recently implemented that requires some restaurants to post energy content information on menus. The influence of this citywide policy is being evaluated. To highlight interest in this strategy, the American Dietetic Association recently recommissioned a work group to review the evidence and put forth a position on menu labeling (Diekman CB. American Dietetic Association’s stance on restaurant labeling. E-mail correspondence to Association members, April 10, 2008).
Involving students in taste testing and voting for school foods is another strategy to encourage healthful eating at school that has been used successfully (18). However, according to a limited data source provided by the School Nutrition Association’s 2007 Operations Report, fewer than 20% of school districts allow students to taste test “most new items” (19).
Ethnic, geographic, and age-related food marketing is well documented. Marketing can shape social values and influence personal preferences that favor high-energy-density foods and beverages (7). Schools are no safe haven. Marketing in schools has been described as product sales (eg, exclusive contracts, fast food on school grounds, food label rebate programs, and candy bar fundraising); direct advertising (eg, logos, posters, book covers, and score boards); media advertising (eg, bus, yearbook, newsletter, Channel One, and screen savers); and indirect advertising (eg, teaching/curriculum materials and industry sponsored kits) (20). Despite the evidence of pervasive marketing in schools, a survey of School Nutrition Association members showed that only 28% of school districts have formal policies in place that restrict advertising/marketing to students (19).
What we do not know is how policies and practices related to nutrition standards, healthful eating strategies, and marketing in schools are distributed across different race, income, and location strata for schools. Also unknown are the associations between disparities in policies and practices in schools that serve the most weight-vulnerable children (ie, minority, poor, and rural). Knowledge about equity or disparities in the distribution of these policies and practices is important for two major reasons. First, such knowledge will help identify the role of system-level policies/practices and demographic factors—and their interactions—that promote or inhibit weight-related disparities in school settings. Second, if disparities and/or associations in school wellness policies and practices do exist, then research can move beyond first and second generation studies (detecting disparities and understanding reasons for observed disparities) to include third generation studies (ie, interventions to reduce or eliminate disparities) (21).
FRAMEWORK AND GUIDELINES FOR IDENTIFYING DISPARITIES
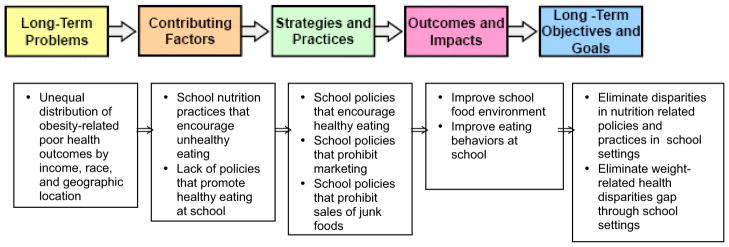
The nation is committed to reducing health disparities (8). Unfortunately, the Healthy People 2010 progress review found that obesity rates among all youth are moving away from, rather than toward, their target goals (6). A similar trend away from target goals is reported for obesity rates between lower and higher income adolescents (6). A conceptual framework to consider when evaluating the equity in distribution of school nutrition policies and practices is the Strategic Framework for Improving Racial and Ethnic Minority Health and Eliminating Racial and Ethnic Disparities (22). The framework is a product of the Health and Human Services Office of Minority Health. Its purpose is to help guide, organize, and coordinate the systematic planning, implementation, and evaluation of national efforts to improve the health of minority populations and reduce health disparities. The framework is useful for school policy research, because it emphasizes the role of system-level factors and approaches that promote or inhibit practices aimed at reducing health disparities. The Figure depicts the general structure of the framework (five components) and how school nutrition policies and practices might be incorporated.
Figure.
Applying the Strategic Framework for Improving Racial and Ethnic Minority Health and Eliminating Racial and Ethnic Disparities to school nutrition policies and practices.
Determining Meaningful Differences
When using large datasets like the School Health Practices and Policies Study or School Health Profiles Study it is easy to identify statistically significant differences for even small relative differences (2% to 3%) between most comparison groups. However, with large sample sizes, it is possible to obtain statistically significant differences that do not identify meaningful differences. For example, data from a large sample of schools may identify that 26% of rural, 28% of urban, and 29% of suburban schools have a policy prohibiting the advertisement of junk foods resulting in a statistically significant difference between them. However, judging whether a disparity exists is less clear. A 2007 Agency for Healthcare Research and Quality report (23) identifies the following criteria for determining meaningful differences among populations: “the difference is statistically significant at the α-0.05 level, two-tailed test and the relative difference is at least 10% different from the reference group when framed positively as a favorable outcome or negatively as an adverse outcome.” The Agency for Healthcare Research and Quality definition of an important difference in health care can be applied to school policy data.
In addition, the Centers for Disease Control and Prevention offer the following guidelines for measuring disparities between one or more group rates, including establishing a reference group (24).
When disparities are measured, the reference point should be explicitly identified.
If comparisons are made between two groups, the more favorable group rate should be used as the reference point.
Pairwise comparisons are called for when the objective is to describe disparities between one or more individual groups and a specific reference point.
The size of the groups and the number of persons affected in each group should be taken into account when assessing the influence of disparities.
Whenever possible, a confidence interval should accompany each measure of disparity.
The Framework and Agency for Healthcare Research and Quality and Centers for Disease Control and Prevention guidelines are helpful tools that can be applied to assessing wellness policies and practices to determine whether there is equity in the distribution of obesity prevention policies and practices among schools.
FUTURE WORK
Today, policies that focus on upstream determinants of population health remain more the exception than the rule (25). The US Department of Agriculture initiative is one response to the need for more environment-focused changes and less individual-focused behavior changes. Improving risk factors through policy approaches is an important lesson learned from both the tobacco and alcohol fields (25). A better understanding of whether the current distribution of school food policies and practices will create schools of opportunity for all children or contribute to the unequal burden of childhood obesity among some populations is needed. This evaluation approach is especially important because a national policy initiative has taken place.
One study supports the need to evaluate the equity in policy distribution among schools. Using 2006 Utah Profiles data (n = 209 schools), researchers identified that schools with the highest free and reduced lunch enrollment and those located in rural settings were significantly less likely to offer healthful snacks (eg, low-fat milk and baked chips) and more likely to serve unhealthful snacks during meal times (13). Schools with a low percentage of free and reduced lunch enrollments were 3.0 times more likely to report the availability of at least four of the six healthful items examined than schools with high free and reduced lunch enrollment. Schools in urban settings were 3.2 times more likely to offer more healthful choices than schools in rural settings. Schools with a high percentage of free and reduced lunch enrollment were 5.0 times more likely to allow the purchase of snacks during lunch than schools with a low enrollment (28.4% vs 7.6%; P = 0.01). This work also identified disparities in physical activity policies and practices among the schools with the highest percentage of free and reduced lunch enrollment and rural schools. Schools with the lowest participation in free and reduced lunch enrollment were 2.9 times more likely to report having intramural activities or physical activity clubs than high participation schools. Urban schools were 2.9 times more likely and suburban schools were 3.3 times more likely than rural schools to report intramural activities or physical activity clubs. Exploring the current balance of policies during this postwellness era will be important.
Current school nutrition policy and practice prevalence rates have not been reported by important obesity risk factors. This knowledge gap proposes the need to answer two key questions: are there differences in the prevalence of school nutrition policies and practices by school level, race, income, and geographic location? And, what are the associations between the nutrition policy and practice environments of schools and important obesity risk factors? These questions put forward the task to evaluate the distribution of nutrition practices and policies in school settings serving those already most at risk for obesity. Answers to these questions will provide clues to rapidly advance the field towards solutions, if needed. Targeted policy level interventions to reduce obesity-related health disparities in school settings may be needed.
Contributor Information
MARILYN S. NANNEY, University of Minnesota, Department of Family Medicine and Community Health, Program in Health Disparities Research, Minneapolis, MN.
CYNTHIA DAVEY, University of Minnesota, Office of Clinical Research, Biostatistical Design and Analysis Center, Minneapolis, MN.
References
- 1.Yancey AK, Kumanyika SK, Ponce NA, McCarthy WJ, Fielding JE, Leslie JP, Akbar J. Population-based interventions engaging communities of color in healthy eating and active living: A review. Prev Chron Dis. 2004;1:A09. [PMC free article] [PubMed] [Google Scholar]
- 2.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971–2004. JAMA. 2006;295:2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 3.Tae-Seale T, Chandler C. Rural Healthy People 2010: A Companion Document to Healthy People 2010. College Station, TX: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Center; 2003. Nutrition and overweight concerns in rural areas: A literature review; pp. 115–130. [Google Scholar]
- 4.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Children. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 5.CDC WONDER online databases. Centers for Disease Control and Prevention; [Accessed May, 16, 2008]. Web site. http://wonder.cdc.gov/ [Google Scholar]
- 6.Healthy People 2010 Midcourse Review. [Accessed May 16, 2008];Healthy People 2010. Web site. http://www.healthypeople.gov/data/midcourse/default.htm.
- 7.Kumanyika S. Environmental influences on childhood obesity: Ethnic and cultural influences in context. Physiol Behav. 2007;94:61–70. doi: 10.1016/j.physbeh.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Satcher D, Higginbotham EJ. The public health approach to eliminating disparities in health. Am J Public Health. 2008;98:400–403. doi: 10.2105/AJPH.2007.123919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Data/Statistics. US Department of Health and Human Services Office of Minority Health Web site; [Accessed May 16, 2008]. omhrc.gov/templates/browse.aspx?lvl=1&lvlID=2. [Google Scholar]
- 10.Acevedo-Garcia D, Osypuk TL, McArdle N, Williams DR. Toward a policy-relevant analysis of geographic and racial/ethnic disparities in child health. Health Affairs. 2008;27:321–333. doi: 10.1377/hlthaff.27.2.321. [DOI] [PubMed] [Google Scholar]
- 11.School Health Practices and Policies Study. Center for Disease Control and Prevention; [Accessed June 2, 2008]. Web site. http://www.cdc.gov/HealthyYouth/shpps/index.htm. [Google Scholar]
- 12.Centers for Disease Control and Prevention. School Health Profiles Study; [Accessed June 2, 2008]. Web site. http://www.cdc.gov/HealthyYouth/profiles/index.htm. [Google Scholar]
- 13.Nanney M, Bohner C, Friedrichs M. Poverty-related factors associated with obesity prevention policies in Utah secondary schools. J Am Diet Assoc. 2008;108:1210–1215. doi: 10.1016/j.jada.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stallings V, Yaktine A. Leading the Way Toward Healthier Youth. Washington, DC: The National Academies Press; 2007. Nutrition Standards for Foods in Schools. [Google Scholar]
- 15.Kubik MY, Lytle LA, Hannan PJ, Perry CL, Story M. The association of the school food environment with dietary behaviors of young adolescents. Am J Public Health. 2003;93:1168–1173. doi: 10.2105/ajph.93.7.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Toole TP, Anderson S, Miller C, Guthrie J. Nutrition services and foods and beverages available at school: Results from the School Health Policies and Programs Study 2006. J Sch Health. 2007;77:500–521. doi: 10.1111/j.1746-1561.2007.00232.x. [DOI] [PubMed] [Google Scholar]
- 17.French SA. Pricing effects on food choices. J Nutr. 2003;133(suppl):841S–843S. doi: 10.1093/jn/133.3.841S. [DOI] [PubMed] [Google Scholar]
- 18.Finn D, Nanney MS. Risk factors for frequent competitive food consumption at one suburban public middle school. Published abstract. American Public Health Association 133rd Annual Meeting; Philadelphia, PA. 2005. [Google Scholar]
- 19.School Nutrition Operations Report: The State of School Nutrition 2007. Alexandria, VA: School Nutrition Association; 2007. [Google Scholar]
- 20.McGinnis JM, Gootman J, Kraak, Vivica I, editors. Food Marketing to Children and Youth: Threat or Opportunity? Washington, DC: National Academy Press; 2006. [Google Scholar]
- 21.Fine MJ, Ibrahim SA, Thomas SB. The role of race and genetics in health disparities research. Am J Public Health. 2005;95:2125–2128. doi: 10.2105/AJPH.2005.076588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graham G. A strategic framework for improving racial/ethnic minority health and eliminating racial/ethnic health disparities. US Department Of Health And Human Services Office Of Minority Health; [Accessed May 16, 2008]. Web site. http://www.omhrc.gov/npa/images/78/PrintFramework.html. [Google Scholar]
- 23.Hebert PL, Sisk JE, Howell EA. When does a difference become a disparity? Conceptualizing racial and ethnic disparities in health. Health Affairs. 2008;27:374–382. doi: 10.1377/hlthaff.27.2.374. [DOI] [PubMed] [Google Scholar]
- 24.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Insun Kim, Mays V, Pearcy J, Schoenbach V, Weissman JS. Methodological issues in measuring health disparities. Vital Health Stat 2. 2005;141:1–16. [PMC free article] [PubMed] [Google Scholar]
- 25.Vartiainen E, Puska P, Pekkanen J, Tuomilehto J, Jousilahti P. Changes in risk factors explain changes in mortality from ischemic heart disease in Finland. BMJ. 1994;309:23–27. doi: 10.1136/bmj.309.6946.23. [DOI] [PMC free article] [PubMed] [Google Scholar]