Abstract
Study design
Case report.
Objective
To report a case of cervical instability from an os odontoideum that presented as posterior thoracic pain and to present a review of the literature.
Background
Thoracic posterior paraspinal spasms and pain are common chief complaints in individuals with spinal abnormalities.
Methods
A 19-year-old man presented with posterior thoracic pain for nearly 1 year following a college sports-related injury (lacrosse). Computed tomography and magnetic resonance imaging did not reveal any significant thoracic or lumbar spinal cord or nerve root pathology, but did reveal an incidental finding of an os odontoideum.
Results
Surgical stabilization of the atlantoaxial instability resulting from the os odontoideum resulted in complete resolution of the patient's thoracic pain.
Conclusions
Thoracic back pain without a clear thoracic spine etiology warrants further workup to rule out the possibility of spinal instability.
Keywords: Atlantoaxial instability, Os odontoideum, Surgery, Spinal, Pain, Thoracic, Injuries, Sports
Introduction
Os odontoideum is a rare disorder in which an ossicle with smooth circumferential cortical margins represents the odontoid process that has no osseous continuity with the body of C2.1 Both acquired and congenital etiologies have been proposed.2–5 It may present with a wide range of clinical symptoms, ranging from mild neurological symptoms to myelopathy to paralysis.1
Methods
A 19-year-old man presented with progressively increasing posterior thoracic pain for nearly 1 year following an injury sustained while playing lacrosse. Physical examination revealed a nonfocal neurological examination. The patient had a mild loss of cervical and thoracic range of motion due to pain.
Plain radiographs of the thoracic spine were unremarkable. Computed tomography and magnetic resonance imaging (MRI) revealed a small to moderate-sized left paracentral disk herniation at the T8–T9 level, without spinal cord or nerve root compression.
Nonoperative treatment, including physical therapy, epidural injections, and anti-inflammatories, provided minimal relief of these symptoms. Due to the refractory nature of this patient's symptoms, the patient was re-examined and all imaging studies were reviewed on follow-up. Upon further review of the thoracic MRI, the scout images revealed an abnormality at the region of C2. Cervical radiographs showed this abnormality to be an os odontoideum. Further inquiry into the patient's history revealed a fall at 27 months of life that resulted in bilateral arm fractures and a prolonged period of sustained torticollis that ultimately resolved. The patient had no known congenital or developmental spinal abnormalities with his os odontoideum.
Results
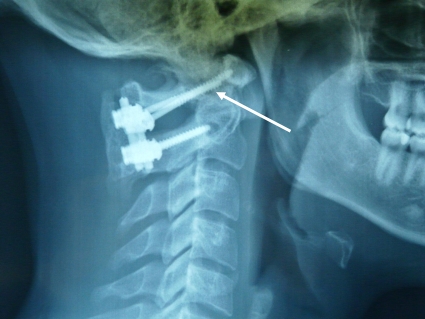
Radiographs demonstrated a greater than 12-mm anterior subluxation of C1 on C2 and flexion–extension films revealed significant atlantoaxial instability. A posterior C1–C2 lateral mass instrumented fusion with iliac crest bone autograft was performed (Fig. 1). In the immediate postoperative period, the patient reported complete resolution of his thoracic pain. At 2-year follow-up, the patient was neurologically intact and without complaints of thoracic pain.
Figure 1.
Posterior C1–C2 instrumented fusion (C2 pars and C1 lateral mass). Follow-up radiographs at 3 months post-operation showed a solid fusion. Note os odontoideum with sclerotic margin (arrow).
Discussion
Individuals who present with thoracic pain refractory to nonoperative treatment and no obvious causative thoracic pathology are difficult to manage clinically. This patient showed no signs of myelopathy or radiculopathy, and imaging studies showed only a minor thoracic spondylosis. Fortunately, the identification of an os odontoideum on the patient's scout MRI image led to a further evaluation with cervical radiographs.
Although this is an atypical presentation, os odontoideum are commonly an incidental finding and are frequently diagnosed in individuals in their late teens and 20s.6–8
The etiology of os odontoideum is poorly understood, with proposed theories ranging from traumatic to congenital to some combination of both. A congenital etiology is supported by the argument that these lesions are commonly associated with other congenital anomalies such as Klippel–Feil and Down's syndrome. Additionally, there are cases of os odontoideum without significant history of trauma.2 However, an acquired etiology is also supported by cases in which pre-trauma cervical radiographs were normal and post-trauma radiographs show an os odontoideum.3 It is common for patients presenting with os odontoideum to also have a remote or recent history of trauma. Klimo et al.6 reported that 50% of patients with os odontoideum had a history of significant previous trauma and 56% of patients with os odontoideum presented after acute trauma.
Menezes further documented that 15% of patients with os odontoideum had a history of cervical trauma in early childhood, and another 14% had a previous history of ‘neck problems in early childhood,’ such as neck pain or torticollis.5 This acquired etiology is also supported by the argument that os odontoideum have similar radiographic features to chronic nonunited fracture of the odontoid process.4 A third theory of pathogenesis considers a congenital disease activated by acquired factors. Brecknell and Malham9 explain that recent or presenting trauma may be viewed as the precipitating event for the development of a symptomatic os odontoideum, but that trauma is not responsible for the disorder itself.
The presence of an os odontoideum often coincides with atlantoaxial instability. With any sagittal plane deformity there can be a compensatory increase in paraspinal musculature activity. Abnormally increased paraspinal muscle activity that compensates for a deficiency in spinal strength or stability, termed guarding behavior, may be one nonvoluntary consequence of spinal injury.10 In a case of cervical instability, it seems intuitive that a patient could exhibit compensatory increase in cervical paraspinal musculature activity; however, in this case the patient presented with spasms and increased paraspinal musculature activity in the thoracic region. It is debatable as to whether the cervical instability caused this patient's symptoms of thoracic paraspinal muscle spasms, but the cause and effect relationship is very likely given the patient's resolution of symptoms after surgical arthrodesis and stabilization of the atlantoaxial instability. Therefore, in this case cervical instability likely caused the paraspinal muscle spasms that caused this patient to present with posterior thoracic pain. This case illustrates the fact that in patients with os odontoideum and thoracic pain, stabilization of the ossicle may cause improvement of the patient's lower thoracic and paraspinal pains.
Conclusion
Thoracic back pain without apparent thoracic etiology may be caused by atlantoaxial instability. Os odontoideum, although rare, should be considered in the differential diagnosis of thoracic pain without obvious thoracic pathology. Finally, posterior atlantoaxial fusion can stabilize the dynamic sagittal plane deformity, thereby effectively treating posterior thoracic pain from thoracic paraspinal muscle spasms.
References
- 1.Hadley MN. Os odontoideum. Neurosurgery 2002;50(3 Suppl.):S148–S155 [DOI] [PubMed] [Google Scholar]
- 2.Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: the case for a multifactorial etiology. Spine (Phila Pa 1976) 2006;31(9):979–84 [DOI] [PubMed] [Google Scholar]
- 3.Schuler TC, Kurz L, Thompson DE, Zemenick G, Hensiger RN, Herkowitz HN. Natural history of os odontoideum. J Pediatr Orthop 1991;11(2):222–5 [DOI] [PubMed] [Google Scholar]
- 4.Stevens JM, Chong WK, Barber C, Kendall BE, Crockard HA. A new appraisal of abnormalities of the odontoid process associated with atlanto-axial subluxation and neurological disability. Brain 1994;117(Part 1):133–48 [DOI] [PubMed] [Google Scholar]
- 5.Menezes AH. Pathogenesis, dynamics, and management of os odontoideum. Neurosurg Focus 1999;6(6):e2. [DOI] [PubMed] [Google Scholar]
- 6.Klimo P, Jr, Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine 2008;9(4):332–42 [DOI] [PubMed] [Google Scholar]
- 7.Watanabe M, Toyama Y, Fujimura Y. Atlantoaxial instability in os odontoideum with myelopathy. Spine (Phila Pa 1976) 1996;21(12):1435–9 [DOI] [PubMed] [Google Scholar]
- 8.Dai L, Yuan W, Ni B, Jia L. Os odontoideum: etiology, diagnosis, and management. Surg Neurol 2000;53(2):106–8, discussion:108–109 [DOI] [PubMed] [Google Scholar]
- 9.Brecknell JE, Malham GM. Os odontoideum: report of three cases. J Clin Neurosci 2008;15(3):295–301 [DOI] [PubMed] [Google Scholar]
- 10.Fryer G, Morris T, Gibbons P. Paraspinal muscles and intervertebral dysfunction: part two. J Manipulative Physiol Ther 2004;27(5):348–57 [DOI] [PubMed] [Google Scholar]