Abstract
Background
According to extensive epidemiological data, infertility is associated with increased ovarian cancer risk. Previous studies showed that both women with infertility and those with ovarian cancer have autoantibodies to ovarian antigens. The objective was to determine if women with infertility have antibodies to mesothelin, a well characterized ovarian cancer antigen.
Methods
Sera were obtained from women with infertility (n=109), ovarian cancer (n=28), benign ovarian tumors or cysts (n=24) and from healthy women (n=152). Infertility included those with a risk for ovarian cancer; endometriosis (n=23), ovulatory dysfunction (n=17), premature ovarian failure (n=25) and unexplained infertility (n=44). Sera were assayed for mesothelin antibodies and for circulating mesothelin antigen by immunoassay and compared to assay control sera (n=16) to determine a positive result.
Results
Mesothelin antibodies were significantly more frequent in women with prematurely reduced ovarian function including ovulatory dysfunction (59%), ovarian failure (POF) (44%) and unexplained infertility (25%) compared to controls. In contrast, women with endometriosis, who also have a high risk for ovarian cancer, did not have mesothelin antibodies. Serum levels of mesothelin were rarely elevated in women with infertility but were high in most patients with ovarian cancer.
Conclusions and Significance
We show for the first time that antibodies to mesothelin, a well characterized ovarian cancer antigen, occur in some women with epidemiologic risk for ovarian cancer. The results suggest it may be possible to identify which women with infertility have ovarian cancer risk.
Keywords: Autoantibodies, Mesothelin, Infertility, Ovarian Cancer
INTRODUCTION
Numerous epidemiologic studies indicate that there is an association between infertility and ovarian cancer (1–5), independent of infertility drug treatment. In a recent study of infertility using a cancer registry in Sweden, the odds ratio (OR) for ovarian cancer was 3.93 (6). According to a 25-year longitudinal investigation of over 12,000 women in the United States, the standardized incidence ratio (SIR) for ovarian cancer risk in infertile women is double that of the general population (SIR=1.98) (7, 8).
Infertility affects over 11% of reproductive age women and is defined as the failure to conceive during one year of unprotected intercourse (9, 10). Diagnostic categories of female infertility may involve endometriosis (uterine cells outside the uterus), tubal factors (inflamed or mechanically blocked Fallopian tubes), uterine factors (e.g., failed implantation) and ovarian factors such as ovulatory dysfunction, diminished ovarian reserve (reduced or absent oocyte content which includes premature ovarian failure), unexplained infertility and multiple causes (9–11). Unexplained infertility is a diagnosis of exclusion used when the standard clinical and laboratory data are normal. Premature ovarian failure (POF) is defined as spontaneous menopause before age 40 (12–14) and may be induced or idiopathic.
Different categories of infertility have different ovarian cancer risk. In the longitudinal infertility study, the highest risk factors for ovarian cancer compared to the general population were nulliparity (never conceived) (SIR=1.98) and endometriosis (SIR=2.48) followed by anovulation (SIR=1.94) (7, 8). Some factors are additive; for example, the SIR for women with endometriosis who never conceived was 4.19. A relationship between POF and ovarian cancer has not been examined systematically although there is evidence that early age at menopause (15–17) or follicle depletion and early ovarian failure (18, 19) is associated with ovarian cancer risk. In cross-sectional studies, unexplained infertility is associated with an increased risk for ovarian cancer (e.g., SIR=2.94 (20) or OR=1.19 (4)).
The etiologies for infertility are multi-factorial and include genetic, environmental, endocrine and autoimmune factors. We showed that some patients with unexplained infertility or POF (21–23) have anti-ovarian antibodies that indicate an autoimmune disorder targeting the ovary (22, 24–26). In addition, a subset of women from all categories undergoing treatment for infertility have poor ovarian estrogen responses to follicle stimulating hormone (FSH); this is also associated with anti-ovarian antibodies (27). While FSH levels are the gold standard for assessing ovarian function (28), anti-ovarian antibodies appear to be independently associated with subclinical changes in ovarian function (29).
Cancer patients often make antibodies to antigens that are expressed in tumor cells even though some of the antigens are also expressed by normal cells (30–35). Women with ovarian cancer also have anti-ovarian antibodies similar to women with infertility (36) indicating they have a similar autoimmune response (30, 36, 37). This is congruent with reports of anti-tumor antibodies to a variety of antigens in ovarian cancer (30, 37, 38). It has been hypothesized that autoimmunity increases the risk for cancer (32, 35, 39, 40) and that a weak tumor-directed immune response can stimulate tumor growth (41, 42).
To gain more insight into the relationship among autoantibodies, infertility and ovarian cancer we tested sera from women with infertility for mesothelin antibodies. Mesothelin expression is elevated in ovarian tumors (43), is shed into the circulation (44) and circulating mesothelin has relatively high specificity for ovarian cancer (45, 46). Previous studies showed that mesothelin antibodies occur in women with ovarian cancer (47, 48) and pelvic inflammatory disease (48). Thus, mesothelin was chosen because it is one of the best characterized ovarian cancer antigens and has relatively high specificity for malignant cells (43).
MATERIALS AND METHODS
Patients
A total of 329 sera were assessed from healthy controls, infertility patients and cancer patients. All sera were collected according to protocols approved by the relevant Institutional Review Boards.
Infertility patient sera (n=109) were collected from infertility clinics at Rush University Medical Center (n=26), the Center for Human Reproduction (courtesy of Dr Carolyn Coulam) (n=16) and the University of Ulm (courtesy of Dr Cosima Brucker) (n=67). Sera represented idiopathic premature ovarian failure (POF; n=25), endometriosis (n=23), ovulatory dysfunction (n=17) and unexplained infertility (n=44). The evaluation included semen analysis, a postcoital test, ovulation (luteal phase progesterone), tubal patency (open and unobstructed fallopian tubes) and measurement of FSH and estrogen. The average duration of infertility was 3.6±1.5 (range 2–8) years for all study patients. The average number of prior in vitro fertilization treatment (IVF) cycles was minimal (less than one per patient).
Patients with idiopathic POF experienced menopause at an average of age of 26.6±9.1 years and had elevated, menopausal day 3 FSH levels (i.e, > 10mIU/mL) (Table 1). Endometriosis patients were obtained from the infertility clinic (n=14) or from the gynecology clinic (n=9) and had surgically confirmed endometriosis without other conditions. Hormone levels were not available for the later group. For endometriosis patients obtained through the infertility clinic, day 3 FSH was in the normal range (Table 1). Ovulatory dysfunction was defined as oligomenorrhea (35–90 days between cycles) or anovulation (no evidence of ovulation) and excluded polycystic ovary syndrome (49). Women with ovulatory dysfunction had slightly elevated, but near normal, day 3 FSH levels (Table 1). Patients with unexplained infertility had normal clinical and laboratory results (Table 1).
Table 1.
Summary of Patient Characteristics
| n | Age | FSH | |
|---|---|---|---|
| PATIENT CATEGORY | mean±SD (range), years | mean±SD (range), mIU/mL | |
| NORMAL | |||
| group I | 31 | 38.7±15.9 (18–65) | nd |
| group II | 121 | nd | nd |
| INFERTILITY PATIENTS | |||
| ENDOMETRIOSIS (infertility clinic) | 14 | 38.3±7.7 (28–60) | 7.1±2.6 (4.9–12.1) |
| ENDOMETRIOSIS (gynecology clinic) | 9 | 46.0±11.1 (36–70) | nd |
| OVULATORY DYSFUNCTION | 17 | 31.7±4.7 (24–40) | 16.9±24.9 (1.2–72) |
| PREMATURE OVARIAN FAILURE | 25 | 30.1±6.6 (19–42) | 60.4±37.8 (19.1–123) |
| UNEXPLAINED INFERTILITY | 44 | 33.2±4.7 (21–49) | 7.4±3.1 (1.9–16.5) |
| BENIGN TUMOR OR CYST | 24 | 56.5±15.7 (26–85) | nd |
| OVARIAN CANCER | 28 | 56.5±15.7 (26–85) | nd |
| ASSAY SERUM CONTROLS | 16 | 56.5±15.7 (26–85) | nd |
| TOTAL | 329 | ||
nd= not determined; FSH: Follicle Stimulating Hormone
Sera from patients with ovarian cancer or benign gynecological conditions were obtained at entry into the clinic for evaluation of a pelvic mass at Rush University Medical Center. Patients had no prior treatment or surgery for cancer. Study patients had ovarian cancer (n=28; n=21 stages III–IV with 15 serous, 5 endometrioid and 1 mucinous histology; n=7 stages I–II with 4 endometrioid, 1 mixed, 1 clear cell and 1 serous histology), benign conditions (n=24; ovarian cysts or fibroids) or surgically confirmed endometriosis (described above).
Controls for assay background (“serum controls”) (n=16) were obtained at Rush University Medical Center from healthy women without a history of diagnosed infertility, autoimmune disease or a history of cancer and were collected at the same time as the experimental sera. The assay controls were used to assess non-specific serum reactions and to determine a cutoff value for a positive result. Also, experimental comparison groups were used. Sera (n=31) from healthy women were obtained from a commercial source (ProMedDx, Norton, MA) (designated “Normal-I”). A second set (“Normal-II”; n=121) contributed by I.H. were originally obtained from Dr O. Nilsson at Fujirebio Diagnostics, Inc, and were used as normal controls for assay development. The age of the Normal-II group is not known. Information regarding fertility for both normal groups was not available.
Serum
Blood was collected into a red top tube, the serum separated and aliquots stored at −80°C.
Recombinant mesothelin
A modification of a mammalian expression vector was used to produce recombinant mesothelin (50). Mesothelin cDNA fragment fused with CMV promoter was amplified by PCR using Pfx50™ DNA polymerase (Invitrogen, CA) with sense primer (5′-AAATTTCTCGAGCGATGTACGGGCCAGAT ATA-3′) and antisense primer (5′-AAAAAACCTGCAGGCTACGTGTCTGCA GGGGGCAT-3′). The PCR product was purified with a QIAquick® PCR Purification Kit (QIAGEN) according to the manufacturer’s protocol. The recombinant plasmid CIHDpa-mesothelin was constructed by replacing IFNγ with mesothelin fragment in the CIHDpa plasmid (50), which was in-licensed from the National University of Singapore. The plasmid was verified by restriction enzyme digestion and by sequencing the completely inserted cDNA.
CIHDpa and mesothelin fragments were digested with XhoI and SbfI restriction enzymes. CIHDpa and mesothelin fragments were extracted from 1% agarose electrophoresis gels using QIAquick® Gel Extraction Kit (Qiagen, CA). Fragments were ligated by T4 DNA ligase (Invitrogen, CA) (16°C, overnight), transformed into E. coli OneShot® TOP10 competent cells (Invitrogen, CA) and plated on LB agar containing ampicillin. For confirmation of the target gene, the plasmid DNA was extracted with a MiniPrep kit (Qiagen, CA) and then examined for inserts of the expected sizes by enzyme digestion (XhoI and SbfI), PCR and sequencing.
Endotoxin-free mesothelin recombinant plasmid was prepared with an Endo-free Maxi kit (Qiagen, CA). 2ug plasmid was added into 2 ul of Lipofactamine and incubated (20 minutes). DNA-Lipofectamine complexes were added into 1 million CHO-DG44 cells. The cells were grown in suspension in 125 ml Corning® plastic cell culture flasks and incubated (37°C; 5% CO2–95% air; 24 hours). The cells were transferred into selection medium (CHO medium without HT supplement). The number of transfected cells was greater than 95% after 30 days.
Culture media were tested for mesothelin using a sandwich ELISA (51, 52). Supernatants were diluted in phosphate buffered saline (PBS) containing 1% BSA in a ratio of 1:10. The data showed that mesothelin was highly expressed by the CHO cells and was released into the culture media. Mesothelin was purified from the culture supernatants by an antibody affinity chromatography column and the purified mesothelin was verified by protein sequencing.
Antibody Tests
Sera were tested at a dilution of 1:20 for antibodies to recombinant human mesothelin and selected sera were retested at a dilution of 1:100 using a modified assay (48).
Briefly, plates (Medisorp; Fisher Scientific, Waltham, MA) were coated (100ul/well, 16 hours, 4°C) with recombinant mesothelin in PBS (10mM, pH 7.4). For each serum, control wells without antigen (coating buffer only) were similarly incubated as a control for nonspecific binding of serum to plastic. Nonspecific binding was blocked with 3% BSA in PBS (15 minutes, 22°C) and serum (100ul/well, 1:20 or 1:100 diluted in PBS+1% BSA) was added (1 hour, 22°C). Wells were washed in PBS containing 0.1% Tween. Goat anti-human IgG-HRP (Invitrogen, Carlsbad, CA) in PBS containing 3% BSA (100ul/well; 1 hour, 22°C) was added. After washing, SureBlueTM TMB peroxidase substrate (KPL, Gaithersburg, MD) was added (100 ul/well; 15 minutes in darkness), and then STOP solution (100ul/well; KPL, Gaithersburg, MD). Plates were read at 450 nm with a Dynatech MR5000 plate reader (Dynatech Laboratories, San Diego, CA). For each serum sample, optical density values in wells without antigen were subtracted from the optical density value in wells with mesothelin. Data was analyzed either by comparison of optical density values or using a cutoff value to determine an antibody positive result. The cutoff value was equivalent to the mean optical value for the serum assay controls (n=16) plus two standard deviations (95% confidence level) or three standard deviations (99% confidence level).
Measurement of circulating mesothelin
Mesothelin levels in sera were measured using a standard sandwich immunoassay (R&D Systems, Minneapolis, MN). Rat anti-human mesothelin capture antibody and biotinylated rat anti-human mesothelin detection antibody were used according to the manufacturer’s instructions. Mesothelin was measured in sera diluted 1:40 in Reagent Diluent (R&D Systems, Minneapolis, MN). The recombinant human mesothelin standard curve range was 62.5 to 8,000 pg/mL. The analytic limit of detection (negative control mean + 2SD) was 79.3 pg/mL.
Statistical analysis
The Mann U Whitney test was used to compare the optical density values and the mesothelin levels. Significant differences in the proportion of mesothelin antibody positive sera were determined using the Fishers exact test. The correlation between mesothelin levels and anti-mesothelin optical density values was compared and significance was determined using Pearson’s or Spearman’s rank correlation as appropriate. For all tests p<0.05 was considered significant.
RESULTS
In an initial analysis of mesothelin antibody levels the two comparison groups (normal-I and normal-II) were evaluated separately and in combination. Since there was no difference between normal-I and normal-II (p>0.6) using either the optical density values or a cutoff value to determine the number of antibody positive sera, and since results were similar when the groups were combined, all further analysis used the combined normal sera group for comparisons.
The mean levels of antibody measured as the optical density at 1:20, were significantly higher in women with POF (p=0.00001), ovulatory dysfunction (p=0.0003), unexplained infertility (p=0.038) and endometriosis (p=0.041) compared to normal sera (Figure 1 and Table 2). Optical density values for sera from women with ovarian cancer or benign tumors did not differ and they did not differ from normal sera (p>0.2).
Figure 1.
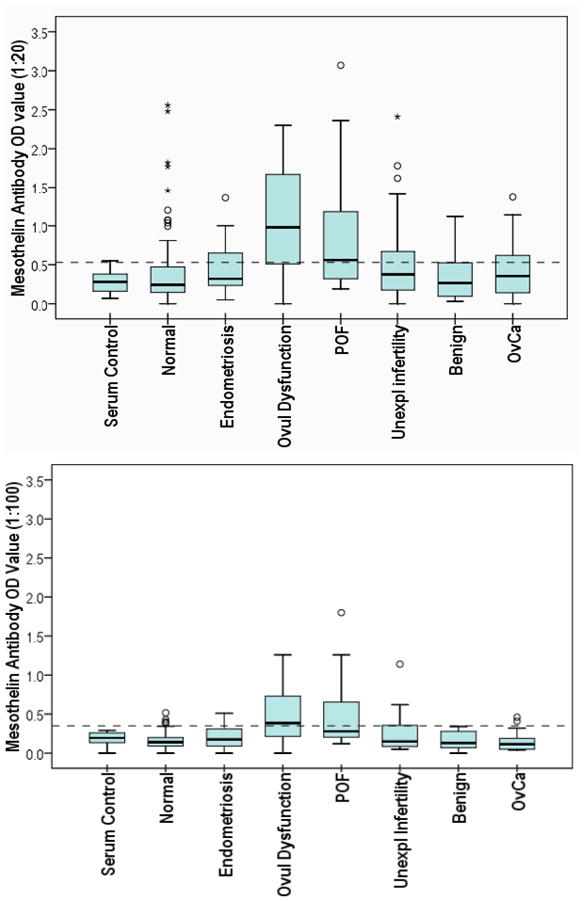
Box plots of mesothelin antibody shown as optical density (OD) values by study group. Sera were tested at 1:20 (upper graph) and 1:100 (lower graph). Each box plot shows the median (50th percentile; dark bar), values to the 1.5 interquartile range (whiskers), 25th–75th percentile range (box) and outliers (○, ★). The horizontal dotted line shows the cutoff value (mean serum control OD + 2SD) used to determine antibody positive results as summarized in Table 2.
Table 2.
Summary of Mesothelin Antibody and Antigen in Infertility
| ANTIBODY | (1:20) | ANTIBODY | (1:100) | ANTIGEN LEVEL | ||
|---|---|---|---|---|---|---|
| OD VALUE | % POS (2SD) | % POS (3SD) | OD VALUE | % POS (2SD) | (ng/mL) | |
| Mean ± SD | % (n/total) | % (n/total) | Mean ± SD | % (n/total) | Mean ± SD (range) | |
| NORMAL | 0.37 ± 0.4 | 19% (29/152) | 11% (17/152) | 0.16 ± 0.10 | 6% (5/82) | 18.6 ± 8.5 (10.2–49.6) |
| INFERTILITY PATIENTS | ||||||
| ENDOMETRIOSIS | 0.47 ± 0.34* | 35% (8/23) | 26% (4/23) | 0.19 ± 0.14 | 14% (3/22) | 16.9 ± 7.7 (8.3–37.8) |
| OVULATORY DYSFUNCTION | 1.01 ± 0.74*** | 65% (11/17)*** | 59% (10/17)*** | 0.49 ± 0.38*** | 50% (8/16)*** | 24.1 ± 8.4 (11.7–33.3) |
| PREMATURE OVARIAN FAILURE | 0.88 ± 0.78*** | 52% (13/25)** | 44% (11/25)** | 0.53 ± 0.51*** | 33% (5/15)** | 20.5 ± 9.9 (10.8–45.6) |
| UNEXPLAINED INFERTILITY | 0.53 ± 0.51* | 32% (14/44) | 25% (11/44)* | 0.24 ± 0.21 | 26% (10/38)** | 24.7 ± 12.3 (12.6–59.1)* |
| BENIGN TUMOR OR CYST | 0.38 ± 0.35 | 21% (5/24) | 21% (5/24) | 0.16 ± 0.11 | 0 (0/18) | 14.1 ± 6.9 (6.0–32.5) |
| OVARIAN CANCER | 0.41 ± 0.33 | 36% (10/28) | 14% (4/28) | 0.15 ± 0.13 | 11% (2/18) | 102.9 ± 113.9 (12.1–434.7)*** |
| ASSAY SERUM CONTROL | 0.27 ± 0.13 | ref | ref | 0.19 ± 0.09 | ref | 12.0 ± 5.6 (5.3–38.1) |
Significance is indicated as
P=0.05–0.01;
P=0.01–0.001;
P<0.001
When a cutoff value (95% confidence level) was used (Table 2), the number of positive sera was significantly higher in women with POF (p=0.002) and ovulatory dysfunction (p=0.0002) compared to normal sera. The number of positive sera in unexplained infertility, endometriosis or benign conditions did not differ from normal sera (p>0.2). The number of positive sera in ovarian cancer (p=0.077) and unexplained infertility approached significance (p=0.097) compared to normal sera. Within the ovarian cancer group, mesothelin antibody occurred in 50% (8 of 16) sera from women with serous histology tumors, only 11% (1 of 9) sera from patients with endometrioid tumors and 1 serum from a patient with mixed clear cell and endometrioid tumor.
Two more stringent conditions for determining the number of positive sera were used. A higher cutoff value (99% confidence level) reduced the proportion of positive sera in all groups (Table 2). Using the higher cutoff value, sera from women with POF (p=0.0005) or ovulatory dysfunction (p=0.0001) remained significantly different from normal sera.
Similarly, when sera were tested at a higher dilution of 1:100, only the optical density values for POF (p=0.0001) and ovulatory dysfunction (p=0.00008) differed significantly compared to normal sera (Table 2). However the number of positive sera (95% confidence level) in unexplained infertility (p=0.005) became significant and the number of antibody positive sera remained significant in POF (p=0.007) and ovulatory dysfunction (p=0.0001).
Overall, the decrease in the proportion of positive sera associated with dilution of sera from 1:20 to 1:100 was greater than 75% for benign conditions, endometriosis, normal and ovarian cancer, while the relative decrease of antibody positive sera in infertility groups was less than 40%. Taken together the results show that mesothelin antibodies in the infertility groups, particularly POF and ovulatory dysfunction, have a higher titer and possibly a higher affinity than anti-mesothelin detected in normal, benign or ovarian cancer sera.
Mesothelin antigen levels in serum were significantly higher in women with ovarian cancer (p=0.00003), benign conditions (p=0.01) or unexplained infertility (p=0.01) compared to normal women (Figure 2 and Table 2). Based on optical density values, mesothelin antibody and antigen were not correlated (Spearman’s correlation coefficient, 0.06, p=0.4). Within individual categories, mesothelin antigen and antibody were not significantly correlated except in ovarian cancer (correlation coefficient = 0.49, p=0.015). However, as seen in Figure 3, the association is scattered; some individuals have elevated mesothelin, some have mesothelin antibody and some have both.
Figure 2.
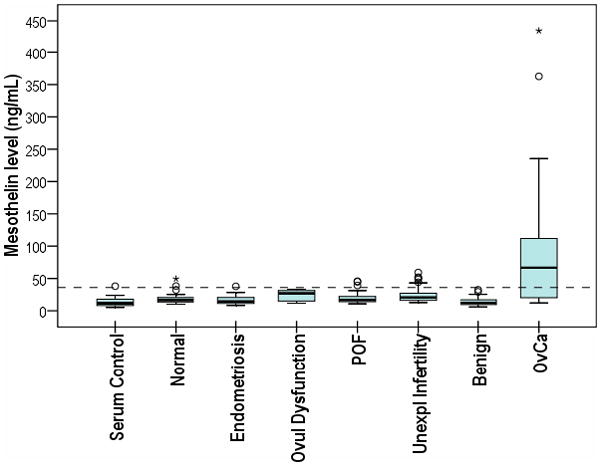
Box plot of circulating mesothelin antigen levels (ng/mL) by study group. The box plot is described in Figure 1. The horizontal dotted line shows the mean normal value + 2SD for reference. Mean values for each group are summarized in Table 2.
Figure 3.
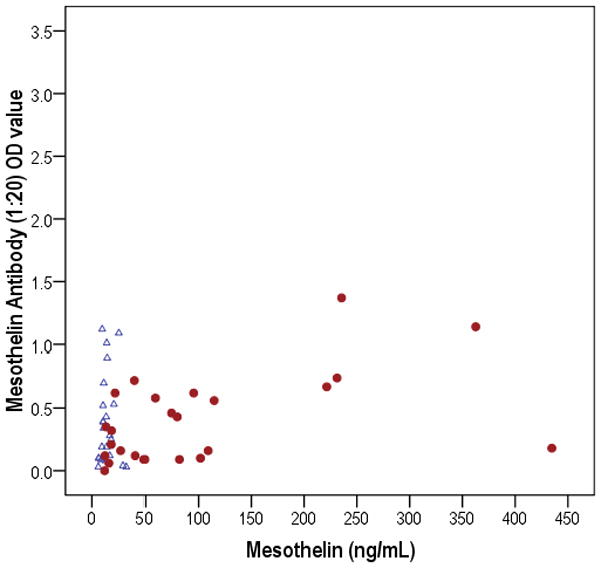
Comparison of mesothelin antibody and circulating antigen in ovarian cancer (●) and benign tumor (△) groups. Mesothelin and anti-mesothelin were correlated in ovarian cancer (correlation coefficient corrected for age = 0.49, p=0.02). However, not all individuals with elevated mesothelin had anti-mesothelin antibodies.
Although the age range of the study groups and normal controls overlapped, the mean ages were not the same. Mesothelin antibody (correlation coefficient = −0.17, p=0.02) was negatively correlated, while mesothelin antigen (correlation coefficient = 0.26, p=0.001) was positively correlated with age. When corrected for age, the relationships between anti-mesothelin and circulating mesothelin remained unchanged (correlation coefficient = 0.1, p=0.2) including the correlation within the ovarian cancer group (correlation coefficient corrected for age = 0.49, p=0.018). Thus, circulating antigen was detected more often in ovarian cancer and anti-mesothelin was detected more often in patients with evidence of ovarian failure.
DISCUSSION
This study extends previous studies which showed that women with infertility and women with ovarian cancer have antibodies to ovarian antigens and shows for the first time that women with specific categories of infertility have antibodies to a well known ovarian cancer biomarker. Originally, we identified anti-ovarian (microsomal) antibodies indicative of ovarian autoimmunity in women with POF, unexplained infertility or sub-optimal response to exogenous hormone (21–27, 29, 53–55). Furthermore, in women with low ovarian responsiveness, anti-ovarian antibodies occur predominantly in younger women differentiating them from older women transitioning into a normal, age-related menopause (53). Since women with infertility have increased risk for ovarian cancer (4, 6, 8) and since anti-tumor antibodies are common in cancer (30, 35, 38, 56–58) we also evaluated the possibility that ovarian cancer patients have anti-ovarian antibodies. We found that women with ovarian cancer, but not endometrial cancer or benign tumors have anti-ovarian antibodies (36).
In the current study, we show that there is an autoantibody response to mesothelin, a well defined biomarker of ovarian carcinoma (51, 59, 60), in women with POF, ovulatory dysfunction or unexplained infertility. This is consistent with the presence of an autoimmune disease of the ovary (22, 24–26, 61) and with the established risk of ovarian cancer associated with infertility (4, 6, 8). This raises the possibility that an autoimmune process precedes or contributes to development and progression of malignant ovarian tumors. Shared autoantibody repertoires in autoimmunity and cancer have been reported (32). Although there is a relationship between autoimmunity and immunity to tumors, the nature of the relationship remains to be determined (39). Nonetheless, the results of this study suggest that early autoantibody responses could identify which women with infertility have a high risk for ovarian cancer.
Interestingly, although endometriosis is associated with a high risk for ovarian cancer (62, 63), women with endometriosis did not have anti-mesothelin antibodies. Although there was a difference in the initial, least stringent analysis of optical density values, there was no difference in the number of positive sera compared to normal sera. The absence of mesothelin antibodies in patients with endometriosis was also noted in a small group in a previous study (48). A history of endometriosis is more often associated with endometrioid and clear cell ovarian carcinoma (62) while serous histology tumors are thought to arise from epithelial cells shed onto the ovary from the fallopian tubes (64, 65). Similarly the risk for sub-types of ovarian tumors may vary; among women with infertility in a population study of infertility in Denmark (66), the major contribution to ovarian cancer risk was associated with serous tumors (SIR=2.1) followed by endometrioid tumors (SIR=1.35) with mucinous tumors contributing little to the risk for ovarian cancer (SIR=0.81). This is also consistent with differences in expression profiles among different tumor subtypes (67, 68). Thus it is possible that tumors arising in women with endometriosis do not involve autoantibody reactions or do not involve the same autoantibody reactions as other infertility categories.
Evidence for different autoantibodies associated with different histological subtypes (30, 69–71) is congruent with the concept that mesothelin antibodies may be associated with some types of infertility and not others. We found the majority of mesothelin antibody positive sera in ovarian cancer were associated with serous rather than endometrioid tumor histology, consistent with the more frequent expression of mesothelin in serous ovarian tumors (72). Hence it is possible that antibodies to mesothelin reflect a risk for serous ovarian tumors.
In addition, we found a higher titer of anti-mesothelin antibodies in infertility than in ovarian cancer. This suggests they may have a higher affinity, or that in ovarian cancer in the presence of excess antigen, antibody-antigen complexes form reducing detection of anti-mesothelin. Antigen-antibody complexes have been reported for CA125 (73) and MUC1(74). It is also possible that excess antigen or some other mechanism suppresses the antibody response in ovarian cancer. Although mesothelin antibodies were reported previously (47, 48) our group of ovarian carcinoma patients may have been too small to reach statistical significance compared to normal sera. However, the group used in this study had a lower proportion of serous ovarian cancer than in prior studies (47, 48) and this may have contributed to the lower proportion of mesothelin antibodies. While none of the normal or benign comparison groups had significant levels of anti-mesothelin, there were occasional women with mesothelin antibodies. This is not surprising since over 11% of the population may have infertility (9) and thus it is possible that a subset of women in the normal group may have infertility associated with autoantibodies. It is also possible that among older women in this group a subset have undetected early stage tumors. Thus, the magnitude of differences between women with identified infertility and those in the normal group may be slightly underestimated. However, further study is needed to determine the significance of mesothelin antibodies in apparently healthy women.
We also tested sera for circulating mesothelin and found, as expected, that most patients with ovarian carcinoma had circulating antigen (45). However, with the exception of unexplained infertility, circulating antigen was not significantly higher in the infertility groups compared to normal women. Since there are no standard clinical cutoff values for circulating mesothelin, it is not clear if the slightly elevated levels of circulating mesothelin in unexplained infertility are clinically relevant.
The precise function of antibodies in tumor progression remains to be determined and may involve multiple roles (75). Antibodies to cell surface antigens can promote the growth of tumor cells both in vitro and in vivo (76–78). Antibodies to tumor antigens can also inhibit tumor growth, e.g. via antibody-dependent cellular cytotoxicity, complement dependent cytotoxicity and by interfering with growth controlling signals. Also, a weak tumor-directed immune response can stimulate tumor growth (41, 42) and it has been hypothesized that autoimmunity increases the risk for cancer (32, 35, 39, 40). However, in contrast to the extensive evidence for anti-tumor antibodies, MUC1antibodies, another antigen which is overexpressed in ovarian cancer (79–81) are detected more frequently in women with a lower risk of ovarian cancer (80, 81) than in patients with cancer (82, 83) Clearly, anti-tumor antibodies may provide specific biomarkers of cancer risk and of early stage cancer, but much remains to be determined regarding their functional role in cancer.
In summary, the results of this study showed for the first time that circulating mesothelin antibodies occur in women with increased epidemiologic risk for ovarian cancer. One may speculate that antibodies may arise in response to very early neoplastic processes in infertile women that may or may not progress to malignant tumors depending on additional triggering events. On the other hand antibodies may bind to normal cells in the ovary and cause ovarian dysfunction which leads to infertility and in a subpopulation of infertile women, to the development of ovarian cancer. On the other hand, antibodies may simply reflect an inflammatory response to mesothelin.
Further studies are needed to establish the relative risk for ovarian cancer in infertile women who have mesothelin antibody. Useful information on the relationship of autoantibodies to tumor progression may also be derived from an appropriate animal model. For example, we showed that egg-laying hens have a high frequency of ovarian carcinoma (84) associated with ovarian autoantibodies similar to humans (85). Ovarian tumors in hens express a homologue of human mesothelin (86). Use of this model may facilitate clarification of the relationship between anti-mesothelin antibodies and ovarian cancer formation.
Acknowledgments
The authors thank Dr N. Kiviat for her generous support and Jee Hang Tse for excellent technical help.
Abbreviations
- SIR
standardized incidence ratio
- OR
odds ratio
- POF
premature ovarian failure
- FSH
follicle stimulating hormone
Footnotes
Studies were supported by NIH R01AI055060-01 (JL), Ovarian Cancer SPORE (P50CA83636) Development Award (JL), NIH R01CA134487 (JL, subcontract), Rush University Segal award (JL), NIH 1RO1CA1344867 (IH) and a grant from Fujirebio Diagnostics, Inc (IH).
There are no conflicts of interest to declare.
References
- 1.Tortolero-Luna G, Mitchell MF. The epidemiology of ovarian cancer. J Cell Biochem Suppl. 1995;23:200–7. doi: 10.1002/jcb.240590927. [DOI] [PubMed] [Google Scholar]
- 2.Venn A, Healy D, McLachlan R. Cancer risks associated with the diagnosis of infertility. Best Pract Res Clin Obstet Gynaecol. 2003;17:343–67. doi: 10.1016/s1521-6934(02)00128-1. [DOI] [PubMed] [Google Scholar]
- 3.Runnebaum IB, Stickeler E. Epidemiological and molecular aspects of ovarian cancer risk. J Cancer Res Clin Oncol. 2001;127:73–9. doi: 10.1007/s004320000153. [DOI] [PubMed] [Google Scholar]
- 4.Ness RB, Cramer DW, Goodman MT, Kjaer SK, Mallin K, Mosgaard BJ, et al. Infertility, fertility drugs, and ovarian cancer: a pooled analysis of case-control studies. Am J Epidemiol. 2002;155:217–24. doi: 10.1093/aje/155.3.217. [DOI] [PubMed] [Google Scholar]
- 5.Rossing MA, Tang MT, Flagg EW, Weiss LK, Wicklund KG. A case-control study of ovarian cancer in relation to infertility and the use of ovulation-inducing drugs. Am J Epidemiol. 2004;160:1070–8. doi: 10.1093/aje/kwh315. [DOI] [PubMed] [Google Scholar]
- 6.Kallen B, Finnstrom O, Lindam A, Nilsson E, Nygren KG, Otterblad Olausson P. Malignancies among women who gave birth after in vitro fertilization. Hum Reprod. 2011;26:253–8. doi: 10.1093/humrep/deq307. [DOI] [PubMed] [Google Scholar]
- 7.Brinton LA, Westhoff CL, Scoccia B, Lamb EJ, Althuis MD, Mabie JE, et al. Causes of infertility as predictors of subsequent cancer risk. Epidemiology. 2005;16:500–7. doi: 10.1097/01.ede.0000164812.02181.d5. [DOI] [PubMed] [Google Scholar]
- 8.Brinton LA, Lamb EJ, Moghissi KS, Scoccia B, Althuis MD, Mabie JE, et al. Ovarian cancer risk associated with varying causes of infertility. Fertil Steril. 2004;82:405–14. doi: 10.1016/j.fertnstert.2004.02.109. [DOI] [PubMed] [Google Scholar]
- 9.Kamel RM. Management of the infertile couple: an evidence-based protocol. Reprod Biol Endocrinol. 2010;8:21. doi: 10.1186/1477-7827-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sunderam S, Chang J, Flowers L, Kulkarni A, Sentelle G, Jeng G, et al. Assisted reproductive technology surveillance--United States, 2006. MMWR Surveill Summ. 2009;58:1–25. [PubMed] [Google Scholar]
- 11.Molinaro TA, Shaunik A, Lin K, Sammel MD, Barnhart KT. A strict infertility diagnosis has poor agreement with the clinical diagnosis entered into the Society for Assisted Reproductive Technology registry. Fertil Steril. 2009;92:2088–90. doi: 10.1016/j.fertnstert.2009.05.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Luborsky J, Sowers M, Gold E, Meyers P, Eckhold H, Santoro N. Premature menopause (POF) in a multi-ethnic population study of the menopause transition. 4th International Symposium on Women’s Health and Menopause; Washington, DC USA. 2001. abstract. [Google Scholar]
- 13.Goswami D, Conway GS. Premature ovarian failure. Hum Reprod Update. 2005;11:391–410. doi: 10.1093/humupd/dmi012. [DOI] [PubMed] [Google Scholar]
- 14.Santoro N. Research on the mechanisms of premature ovarian failure. J Soc Gynecol Investig. 2001;8:S10–2. doi: 10.1016/s1071-5576(00)00097-6. [DOI] [PubMed] [Google Scholar]
- 15.Cramer DW. Epidemiologic aspects of early menopause and ovarian cancer. Ann N Y Acad Sci. 1990;592:363–75. doi: 10.1111/j.1749-6632.1990.tb30347.x. [DOI] [PubMed] [Google Scholar]
- 16.Cramer DW, Hutchison GB, Welch WR, Scully RE, Ryan KJ. Determinants of ovarian cancer risk. I. Reproductive experiences and family history. J Natl Cancer Inst. 1983;71:711–6. [PubMed] [Google Scholar]
- 17.Cramer DW, Welch WR, Cassells S, Scully RE. Mumps, menarche, menopause, and ovarian cancer. Am J Obstet Gynecol. 1983;147:1–6. doi: 10.1016/0002-9378(83)90073-x. [DOI] [PubMed] [Google Scholar]
- 18.Smith ER, Xu XX. Ovarian ageing, follicle depletion, and cancer: a hypothesis for the aetiology of epithelial ovarian cancer involving follicle depletion. Lancet Oncol. 2008;9:1108–11. doi: 10.1016/S1470-2045(08)70281-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vanderhyden BC. Loss of ovarian function and the risk of ovarian cancer. Cell Tissue Res. 2005;322:117–24. doi: 10.1007/s00441-005-1100-1. [DOI] [PubMed] [Google Scholar]
- 20.Venn A, Watson L, Bruinsma F, Giles G, Healy D. Risk of cancer after use of fertility drugs with in-vitro fertilisation. Lancet. 1999;354:1586–90. doi: 10.1016/S0140-6736(99)05203-4. [DOI] [PubMed] [Google Scholar]
- 21.Luborsky J, Llanes B, Davies S, Binor Z, Radwanska E, Pong R. Ovarian autoimmunity: greater frequency of autoantibodies in premature menopause and unexplained infertility than in the general population. Clin Immunol. 1999;90:368–74. doi: 10.1006/clim.1998.4661. [DOI] [PubMed] [Google Scholar]
- 22.Luborsky J. Ovarian autoimmune disease and ovarian autoantibodies. J Womens Health Gend Based Med. 2002;11:585–99. doi: 10.1089/152460902760360540. [DOI] [PubMed] [Google Scholar]
- 23.Luborsky JL, Visintin I, Boyers S, Asare T, Caldwell B, DeCherney A. Ovarian antibodies detected by immobilized antigen immunoassay in patients with premature ovarian failure. J Clin Endocrinol Metab. 1990;70:69–75. doi: 10.1210/jcem-70-1-69. [DOI] [PubMed] [Google Scholar]
- 24.Pires ES, Khole VV. A block in the road to fertility: autoantibodies to heat-shock protein 90-beta in human ovarian autoimmunity. Fertil Steril. 2009;92 doi: 10.1016/j.fertnstert.2008.08.068. [DOI] [PubMed] [Google Scholar]
- 25.Sundblad V, Bussmann L, Chiauzzi VA, Pancholi V, Charreau EH. Alpha-enolase: a novel autoantigen in patients with premature ovarian failure. Clin Endocrinol (Oxf) 2006;65:745–51. doi: 10.1111/j.1365-2265.2006.02661.x. [DOI] [PubMed] [Google Scholar]
- 26.Forges T, Monnier-Barbarino P, Faure GC, Bene MC. Autoimmunity and antigenic targets in ovarian pathology. Hum Reprod Update. 2004;10:163–75. doi: 10.1093/humupd/dmh014. [DOI] [PubMed] [Google Scholar]
- 27.Meyer WR, Lavy G, DeCherney AH, Visintin I, Economy K, Luborsky JL. Evidence of gonadal and gonadotropin antibodies in women with a suboptimal ovarian response to exogenous gonadotropin. Obstet Gynecol. 1990;75:795–9. [PubMed] [Google Scholar]
- 28.Creus M, Penarrubia J, Fabregues F, Vidal E, Carmona F, Casamitjana R, et al. Day 3 serum inhibin B and FSH and age as predictors of assisted reproduction treatment outcome. Hum Reprod. 2000;15:2341–6. doi: 10.1093/humrep/15.11.2341. [DOI] [PubMed] [Google Scholar]
- 29.Luborsky J, Roussev R, Coulam C. Ovarian antibodies, FSH and inhibin are independent markers associated with unexplained infertility. Human Reprod. 2000;15:1046–1051. doi: 10.1093/humrep/15.5.1046. [DOI] [PubMed] [Google Scholar]
- 30.Gnjatic S, Ritter E, Buchler MW, Giese NA, Brors B, Frei C, et al. Seromic profiling of ovarian and pancreatic cancer. Proc Natl Acad Sci U S A. 2010;107:5088–93. doi: 10.1073/pnas.0914213107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reuschenbach M, von Knebel Doeberitz M, Wentzensen N. A systematic review of humoral immune responses against tumor antigens. Cancer Immunol Immunother. 2009;58:1535–44. doi: 10.1007/s00262-009-0733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bei R, Masuelli L, Palumbo C, Modesti M, Modesti A. A common repertoire of autoantibodies is shared by cancer and autoimmune disease patients: Inflammation in their induction and impact on tumor growth. Cancer Lett. 2009;281:8–23. doi: 10.1016/j.canlet.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 33.Stockert E, Jager E, Chen YT, Scanlan MJ, Gout I, Karbach J, et al. A survey of the humoral immune response of cancer patients to a panel of human tumor antigens. J Exp Med. 1998;187:1349–54. doi: 10.1084/jem.187.8.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nesterova M, Johnson N, Cheadle C, Cho-Chung YS. Autoantibody biomarker opens a new gateway for cancer diagnosis. Biochim Biophys Acta. 2006;1762:398–403. doi: 10.1016/j.bbadis.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 35.Tan EM, Zhang J. Autoantibodies to tumor-associated antigens: reporters from the immune system. Immunol Rev. 2008;222:328–40. doi: 10.1111/j.1600-065X.2008.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barua A, Bradaric MJ, Kebede T, Espinosa S, Edassery SL, Bitterman P, et al. Anti-ovarian and anti-tumor antibodies in women with ovarian cancer. Am J Reprod Immunol. 2007;57:243–249. doi: 10.1111/j.1600-0897.2007.00470.x. [DOI] [PubMed] [Google Scholar]
- 37.Luborsky JL, Barua A, Shatavi SV, Kebede T, Abramowicz J, Rotmensch J. Anti-tumor antibodies in ovarian cancer. Am J Reprod Immunol. 2005;54:55–62. doi: 10.1111/j.1600-0897.2005.00287.x. [DOI] [PubMed] [Google Scholar]
- 38.Erkanli A, Taylor DD, Dean D, Eksir F, Egger D, Geyer J, et al. Application of Bayesian modeling of autologous antibody responses against ovarian tumor-associated antigens to cancer detection. Cancer Res. 2006;66:1792–8. doi: 10.1158/0008-5472.CAN-05-0669. [DOI] [PubMed] [Google Scholar]
- 39.Ramirez-Montagut T, Turk MJ, Wolchok JD, Guevara-Patino JA, Houghton AN. Immunity to melanoma: unraveling the relation of tumor immunity and autoimmunity. Oncogene. 2003;22:3180–7. doi: 10.1038/sj.onc.1206462. [DOI] [PubMed] [Google Scholar]
- 40.Uchi H, Stan R, Turk MJ, Engelhorn ME, Rizzuto GA, Goldberg SM, et al. Unraveling the complex relationship between cancer immunity and autoimmunity: lessons from melanoma and vitiligo. Adv Immunol. 2006;90:215–41. doi: 10.1016/S0065-2776(06)90006-6. [DOI] [PubMed] [Google Scholar]
- 41.Prehn RT, Prehn LM. The flip side of immune surveillance: immune dependency. Immunol Rev. 2008;222:341–56. doi: 10.1111/j.1600-065X.2008.00609.x. [DOI] [PubMed] [Google Scholar]
- 42.Prehn RT. An immune reaction may be necessary for cancer development. Theor Biol Med Model. 2006;3:6. doi: 10.1186/1742-4682-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rosen DG, Wang L, Atkinson JN, Yu Y, Lu KH, Diamandis EP, et al. Potential markers that complement expression of CA125 in epithelial ovarian cancer. Gynecol Oncol. 2005;99:267–77. doi: 10.1016/j.ygyno.2005.06.040. [DOI] [PubMed] [Google Scholar]
- 44.Scholler N, Fu N, Yang Y, Ye Z, Goodman GE, Hellstrom KE, et al. Soluble member(s) of the mesothelin/megakaryocyte potentiating factor family are detectable in sera from patients with ovarian carcinoma. Proc Natl Acad Sci U S A. 1999;96:11531–6. doi: 10.1073/pnas.96.20.11531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McIntosh MW, Drescher C, Karlan B, Scholler N, Urban N, Hellstrom KE, et al. Combining CA 125 and SMR serum markers for diagnosis and early detection of ovarian carcinoma. Gynecol Oncol. 2004;95:9–15. doi: 10.1016/j.ygyno.2004.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Palmer C, Duan X, Hawley S, Scholler N, Thorpe JD, Sahota RA, et al. Systematic evaluation of candidate blood markers for detecting ovarian cancer. PLoS ONE. 2008;3:e2633. doi: 10.1371/journal.pone.0002633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ho M, Hassan R, Zhang J, Wang QC, Onda M, Bera T, et al. Humoral immune response to mesothelin in mesothelioma and ovarian cancer patients. Clin Cancer Res. 2005;11:3814–20. doi: 10.1158/1078-0432.CCR-04-2304. [DOI] [PubMed] [Google Scholar]
- 48.Hellstrom I, Friedman E, Verch T, Yang Y, Korach J, Jaffar J, et al. Anti-mesothelin antibodies and circulating mesothelin relate to the clinical state in ovarian cancer patients. Cancer Epidemiol Biomarkers Prev. 2008;17:1520–6. doi: 10.1158/1055-9965.EPI-08-0039. [DOI] [PubMed] [Google Scholar]
- 49.Broekmans FJ, Fauser BC. Diagnostic criteria for polycystic ovarian syndrome. Endocrine. 2006;30:3–11. doi: 10.1385/ENDO:30:1:3. [DOI] [PubMed] [Google Scholar]
- 50.Ng SK, Wang DI, Yap MG. Application of destabilizing sequences on selection marker for improved recombinant protein productivity in CHO-DG44. Metab Eng. 2007;9:304–16. doi: 10.1016/j.ymben.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 51.Hellstrom I, Raycraft J, Kanan S, Sardesai NY, Verch T, Yang Y, et al. Mesothelin variant 1 is released from tumor cells as a diagnostic marker. Cancer Epidemiol Biomarkers Prev. 2006;15:1014–20. doi: 10.1158/1055-9965.EPI-05-0334. [DOI] [PubMed] [Google Scholar]
- 52.Johnston FM, Tan MC, Tan BR, Jr, Porembka MR, Brunt EM, Linehan DC, et al. Circulating mesothelin protein and cellular antimesothelin immunity in patients with pancreatic cancer. Clin Cancer Res. 2009;15:6511–8. doi: 10.1158/1078-0432.CCR-09-0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luborsky JL, Thiruppathi P, Rivnay B, Roussev R, Coulam C, Radwanska E. Evidence for different aetiologies of low estradiol response to FSH: age-related accelerated luteinization of follicles or presence of ovarian autoantibodies. Hum Reprod. 2002;17:2641–9. doi: 10.1093/humrep/17.10.2641. [DOI] [PubMed] [Google Scholar]
- 54.Shatavi SV, Llanes B, Luborsky JL. Association of unexplained infertility with gonadotropin and ovarian antibodies. Am J Reprod Immunol. 2006;56:286–91. doi: 10.1111/j.1600-0897.2006.00428.x. [DOI] [PubMed] [Google Scholar]
- 55.Edassery SL, Shatavi SV, Kunkel JP, Hauer C, Brucker C, Penumatsa K, et al. Autoantigens in ovarian autoimmunity associated with unexplained infertility and premature ovarian failure. Fertil Steril. 2010;94:2636–41. doi: 10.1016/j.fertnstert.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Taylor DD, Gercel-Taylor C, Parker LP. Patient-derived tumor-reactive antibodies as diagnostic markers for ovarian cancer. Gynecol Oncol. 2009;115:112–20. doi: 10.1016/j.ygyno.2009.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 57.Jager E, Stockert E, Zidianakis Z, Chen YT, Karbach J, Jager D, et al. Humoral immune responses of cancer patients against "Cancer-Testis" antigen NY-ESO-1: correlation with clinical events. Int J Cancer. 1999;84:506–10. doi: 10.1002/(sici)1097-0215(19991022)84:5<506::aid-ijc10>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 58.Gnjatic S, Wheeler C, Ebner M, Ritter E, Murray A, Altorki NK, et al. Seromic analysis of antibody responses in non-small cell lung cancer patients and healthy donors using conformational protein arrays. J Immunol Methods. 2009;341:50–8. doi: 10.1016/j.jim.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 59.Hassan R, Remaley AT, Sampson ML, Zhang J, Cox DD, Pingpank J, et al. Detection and quantitation of serum mesothelin, a tumor marker for patients with mesothelioma and ovarian cancer. Clin Cancer Res. 2006;12:447–53. doi: 10.1158/1078-0432.CCR-05-1477. [DOI] [PubMed] [Google Scholar]
- 60.Hellstrom I, Hellstrom KE. SMRP and HE4 as biomarkers for ovarian carcinoma when used alone and in combination with CA125 and/or each other. Adv Exp Med Biol. 2008;622:15–21. doi: 10.1007/978-0-387-68969-2_2. [DOI] [PubMed] [Google Scholar]
- 61.Monnier-Barbarino P, Forges T, Faure GC, Bene MC. Ovarian autoimmunity and ovarian pathologies: antigenic targets and diagnostic significance. J Gynecol Obstet Biol Reprod (Paris) 2005;34:649–57. doi: 10.1016/s0368-2315(05)82897-2. [DOI] [PubMed] [Google Scholar]
- 62.Nezhat F, Datta MS, Hanson V, Pejovic T, Nezhat C. The relationship of endometriosis and ovarian malignancy: a review. Fertil Steril. 2008;90:1559–70. doi: 10.1016/j.fertnstert.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 63.Mandai M, Yamaguchi K, Matsumura N, Baba T, Konishi I. Ovarian cancer in endometriosis: molecular biology, pathology, and clinical management. Int J Clin Oncol. 2009;14:383–91. doi: 10.1007/s10147-009-0935-y. [DOI] [PubMed] [Google Scholar]
- 64.Salvador S, Gilks B, Kobel M, Huntsman D, Rosen B, Miller D. The fallopian tube: primary site of most pelvic high-grade serous carcinomas. Int J Gynecol Cancer. 2009;19:58–64. doi: 10.1111/IGC.0b013e318199009c. [DOI] [PubMed] [Google Scholar]
- 65.Piek JM, van Diest PJ, Verheijen RH. Ovarian carcinogenesis: an alternative hypothesis. Adv Exp Med Biol. 2008;622:79–87. doi: 10.1007/978-0-387-68969-2_7. [DOI] [PubMed] [Google Scholar]
- 66.Jensen A, Sharif H, Frederiksen K, Kjaer SK. Use of fertility drugs and risk of ovarian cancer: Danish Population Based Cohort Study. BMJ. 2009;338:b249. doi: 10.1136/bmj.b249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kobel M, Kalloger SE, Boyd N, McKinney S, Mehl E, Palmer C, et al. Ovarian carcinoma subtypes are different diseases: implications for biomarker studies. PLoS Med. 2008;5:e232. doi: 10.1371/journal.pmed.0050232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Marquez RT, Baggerly KA, Patterson AP, Liu J, Broaddus R, Frumovitz M, et al. Patterns of gene expression in different histotypes of epithelial ovarian cancer correlate with those in normal fallopian tube, endometrium, and colon. Clin Cancer Res. 2005;11:6116–26. doi: 10.1158/1078-0432.CCR-04-2509. [DOI] [PubMed] [Google Scholar]
- 69.Draghici S, Chatterjee M, Tainsky MA. Epitomics: serum screening for the early detection of cancer on microarrays using complex panels of tumor antigens. Expert Rev Mol Diagn. 2005;5:735–43. doi: 10.1586/14737159.5.5.735. [DOI] [PubMed] [Google Scholar]
- 70.Gunawardana CG, Memari N, Diamandis EP. Identifying novel autoantibody signatures in ovarian cancer using high-density protein microarrays. Clin Biochem. 2009;42:426–9. doi: 10.1016/j.clinbiochem.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 71.Tang L, Yang J, Ng SK, Rodriguez N, Choi PW, Vitonis A, et al. Autoantibody profiling to identify biomarkers of key pathogenic pathways in mucinous ovarian cancer. Eur J Cancer. 2010;46:170–9. doi: 10.1016/j.ejca.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Frierson HF, Jr, Moskaluk CA, Powell SM, Zhang H, Cerilli LA, Stoler MH, et al. Large-scale molecular and tissue microarray analysis of mesothelin expression in common human carcinomas. Hum Pathol. 2003;34:605–9. doi: 10.1016/s0046-8177(03)00177-1. [DOI] [PubMed] [Google Scholar]
- 73.Cramer DW, O’Rourke DJ, Vitonis AF, Matulonis UA, Dijohnson DA, Sluss PM, et al. CA125 immune complexes in ovarian cancer patients with low CA125 concentrations. Clin Chem. 2010;56:1889–92. doi: 10.1373/clinchem.2010.153122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Croce MV, Isla-Larrain MT, Price MR, Segal-Eiras A. Detection of circulating mammary mucin (Muc1) and MUC1 immune complexes (Muc1-CIC) in healthy women. Int J Biol Markers. 2001;16:112–20. doi: 10.1177/172460080101600205. [DOI] [PubMed] [Google Scholar]
- 75.de Visser KE. Spontaneous immune responses to sporadic tumors: tumor-promoting, tumor-protective or both? Cancer Immunol Immunother. 2008;57:1531–1539. doi: 10.1007/s00262-008-0501-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.de Visser KE, Korets LV, Coussens LM. De novo carcinogenesis promoted by chronic inflammation is B lymphocyte dependent. Cancer Cell. 2005;7:411–23. doi: 10.1016/j.ccr.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 77.de Visser KE, Eichten A, Coussens LM. Paradoxical roles of the immune system during cancer development. Nat Rev Cancer. 2006;6:24–37. doi: 10.1038/nrc1782. [DOI] [PubMed] [Google Scholar]
- 78.Shearer WT, Philpott GW, Parker CW. Stimulation of cells by antibody. Science. 1973;182:1357–9. doi: 10.1126/science.182.4119.1357. [DOI] [PubMed] [Google Scholar]
- 79.Vlad AM, Diaconu I, Gantt KR. MUC1 in endometriosis and ovarian cancer. Immunol Res. 2006;36:229–36. doi: 10.1385/IR:36:1:229. [DOI] [PubMed] [Google Scholar]
- 80.Cramer DW, Titus-Ernstoff L, McKolanis JR, Welch WR, Vitonis AF, Berkowitz RS, et al. Conditions associated with antibodies against the tumor-associated antigen MUC1 and their relationship to risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2005;14:1125–31. doi: 10.1158/1055-9965.EPI-05-0035. [DOI] [PubMed] [Google Scholar]
- 81.Terry KL, Titus-Ernstoff L, McKolanis JR, Welch WR, Finn OJ, Cramer DW. Incessant ovulation, mucin 1 immunity, and risk for ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:30–5. doi: 10.1158/1055-9965.EPI-06-0688. [DOI] [PubMed] [Google Scholar]
- 82.Hermsen BB, Verheijen RH, Menko FH, Gille JJ, van Uffelen K, Blankenstein MA, et al. Humoral immune responses to MUC1 in women with a BRCA1 or BRCA2 mutation. Eur J Cancer. 2007;43:1556–63. doi: 10.1016/j.ejca.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 83.Rabassa ME, Croce MV, Pereyra A, Segal-Eiras A. MUC1 expression and anti-MUC1 serum immune response in head and neck squamous cell carcinoma (HNSCC): a multivariate analysis. BMC Cancer. 2006;6:253. doi: 10.1186/1471-2407-6-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fredrickson TN. Ovarian tumors of the hen. Environ Health Perspect. 1987;73:35–51. doi: 10.1289/ehp.877335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barua A, Bradaric MJ, Kebede T, Espionosa S, Edassery SL, Bitterman P, et al. Anti-tumor and anti-ovarian autoantibodies in women with ovarian cancer. Am J Reprod Immunol. 2007;57:243–9. doi: 10.1111/j.1600-0897.2007.00470.x. [DOI] [PubMed] [Google Scholar]
- 86.Yu Y, Edassery S, Barua A, Abramowicz J, Bahr J, Hellstrom I, Luborsky JL. The hen model of human ovarian cancer develops anti-mesothelin autoantibodies in response to mesothelin expressing tumors submitted. 2011 doi: 10.1186/1757-2215-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


