INTRODUCTION
Adrenal rest tumor in liver is a very rare tumor. It originates from an adrenal rest, which is derived from the aberrant adrenocortical tissue. Adrenal rest tumor is an ectopic collection of adrenocortical cells in extra-adrenal sites.1,2 This tumor may be hormonally active and manifest endocrine syndromes.2 But, most tumors are non-functioning and benign. Histologically, hepatic adrenal rest tumors (HARTs) are composed of low columnar or cuboidal clear cells, similar to adrenocortical tumors. At imaging, HART is typically subcapsular tumor, demonstrating macroscopic fat and hypervascularity.3-5 Radiologically, adrenal rest tumor shows similar findings with those of hepatocellular carcinoma (HCC), adenoma or other hepatic tumors. Differentiation of HART from angiomyolipoma or HCC may be difficult at both radiologic and histologic analysis. Especially in case of HART without macroscopic fat component, preoperative radiologic diagnosis of adrenal rest tumor is confusing with HCC. So, differential diagnosis should be made with caution.
Here is a case of adrenal rest tumor with radiological imaging findings of HCC.
CASE
A 62-year-old man was referred from a local hospital. One month earlier, at a regular medical checkup, a hepatic mass was detected on ultrasound sonography (US). He had no family history of malignancy or significant past history. There were no symptoms related to the mass. General physical examinations were unremarkable. The laboratory findings showed leukocyte count of 5,600/mm3, hemoglobin level of 13.8 g/dL, and platelet count of 218,000/mm3. The aspartate aminotransferase was 19 IU/L, alanine aminotransferase was 15 IU/L, and alkaline phosphatase was 46 IU/L. The total bilirubin level was 0.9 mg/dL, albumin level was 3.7 g/dL, prothrombin time was 11.6 second (INR, 0.98). Serum hepatitis B surface antigen was negative, hepatitis B surface antibody was positive, and anti-hepatitis C virus was negative. Serum α-fetoprotein level was 3.9 ng/mL. Carcinoembryonic antigen was not checked. As we did not anticipate the possibility of hormonally functioning tumor, the hormone levels were not checked.
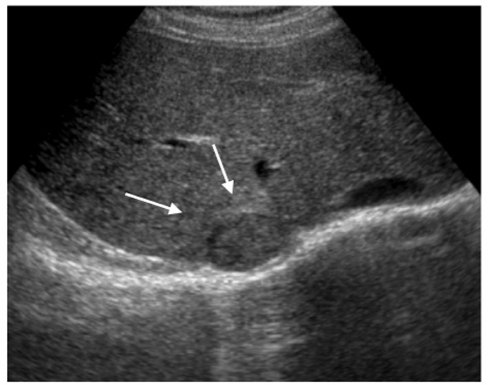
Trans-abdominal US revealed a 3 cm solid mass showing heterogeneous echogenicity at the periphery of the posterosuperior sub-segment of the right hepatic lobe with bulging contour (Fig. 1).
Figure 1.
Transabdominal ultrasonography of a 62-year-old man shows heterogenous echogenic mass (arrows) in liver right lobe posterior segment subcapsular area.
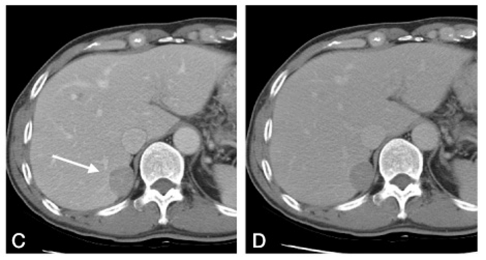
On unenhanced computed tomography (CT) images, the mass appeared to be hypodense with components of low CT numbers [30-40 housefield unit (HU)] (Fig. 2). Macroscopic fat component was not clearly detected on CT. On multiphase dynamic CT images, the mass was enhanced homogenously and appeared to be hyperdense in the arterial phase (110 HU) and hypodense in the portal and delayed phase (80 HU) (Fig. 3, 4). On ordinal axial CT images, the right adrenal gland was identified separately, but abutting against the hepatic mass.
Figure 2.
On pre-contrast scan, 3 cm size mass (arrow) showed slightly bulging contour in right lobe posterior segment of liver. The mass shows slight hypodense attenuation than liver parenchyma (HU 40).
Figure 3.
Arterial phase dynamic CT shows homogenous enhancement of the mass (arrow). In the other level, normal right side adrenal gland was visualized.
Figure 4.
On portal phase (A) and delayed phase (B) of dynamic CT, the mass turned to lower attenuation than surrounding liver parenchyma (arrow).
Based on above radiologic findings, HCC was suspected. The patient underwent a subsegmental resection of the liver. The resected specimen exhibited a well-demarcated mass with whitish tan and golden yellow streaks in cut section just beneath the capsule. At surgery, a hepatic tumor was seen to be abutted to the right adrenal gland at the surface of the liver, but the right adrenal gland was easily detached from the tumor and showed no abnormality.
Microscopic studies revealed a mass consisting of adrenal cortical cells, mainly clear cells with abundant lipid contents, confirming the diagnosis of adrenal rest tumor. There was no evidence of mitotic activity. Adrenal medulla was not found in the tumor. The postoperative course was uneventful, and the patient was subsequently discharged.
DISCUSSION
Adrenal rest is collections of aberrantly located adrenocortical tissue. Its incidence is reported to be very low. It has been described most commonly in abdominal and pelvic sites.1 The aberrant adrenal tissues are divided into the heterotopia and the accessory adrenal gland; the former is derived from adrenal primordium that has migrated to neighboring organs such as kidneys or the liver at an embryonic stage, whereas the latter is the ectopia of fragmented adrenal tissues into the celiac axis, retroperitoneal cavity, uterus broad ligament, or testis. Adrenal rest is a minute lesion with a diameter of less than 7 mm, and is incidentally detected at surgery or autopsy in various sites except for the limbs.3 Frequency of the adrenal rest is high in the celiac axis, testis and broad ligament which are related to the embryogenic development of the adrenal gland. Rarely it was found in lung, brain, pancreas, omentum, and transverse colon.6 They usually consist only of adrenal cortical cells, rarely containing adrenal medullar cells.1
Adrenal rest tumors are thought to arise from the aberrant adrenal tissues. Occasional adrenal rest tumors have been reported to occur in the liver.1-5 HART is considered to be derived from the adrenal rest in the liver and is very rare. This tumor is common in younger patients and equally distributed between both genders.4 HART has previously been called primary hypernephroma of the liver and hypernephroid carcinoma of the liver.4 Adrenal rest tumors are composed of cord-like arrangements of low columnar or cuboidal clear cells, containing light-colored transparent cytoplasms, which are partitioned by thin fibrous septum. Histologically, the lesions of HART are similar to adrenocortical tumors. As it is occasionally difficult to distinguish the adrenal rest tumor from hepatocellular adenoma or HCC due to histological similarity,4 reliable diagnostic methods are required to prove steroid hormone production or excretion. However, most tumors are clinically non-functioning. Even in such cases, immunohistochemical examinations with protein antigens related to adrenocortical steroidogenesis are useful to prove the steroidogenic capability of these tumors.2,3
The malignant transformation of HART is quite rare. There has been only one case report, a 17-month-old boy with malignant HART accompanied with adrenocortical hyperfunction.5 The case had no foci of atypical mitosis, necrosis, and capsular and venous invasion, so the tumor was considered to be benign.
An accurate preoperative radiological diagnosis is very difficult. HART usually appears as a round, well defined mass in the right hepatic lobe. Among the histological constituents of HART, the presence of fat within the tumor is the most characteristic feature.4 HART shows a fat containing and hypervascular mass on imaging. They often contain foci of calcification. To determine that the tumor is originated from the liver, it is necessary to demonstrate that the tumor is distinctly demarcated from the adrenal gland and the original adrenal gland is identified radiologically.
One specific radiological diagnostic character of HART is the presence of fat components. This will reflect intracytoplasmic lipid droplets of the tumor cells. The differential diagnoses of hepatic tumors containing fat components are as follows: HCC with fatty metamorphosis, focal nodular hyperplasia, hepatocellular adenoma, angiomyolipoma, lipoma, and liposarcoma.7 Another radiological diagnostic character is hypervascularity. The tumor is mainly supplied by the hepatic artery. Therefore, HCC with fatty metamorphosis and angiomyolipoma could be considered as a differential diagnosis. In cases of hypervascular or fat-containing hepatic tumors, HART should be added to the lists of radiological differential diagnoses.
In adrenocortical adenoma, on unenhanced scans, attenuation values vary from 34 HU in adenomas with low lipid levels to -20 HU in those with high lipid levels. The attenuation on unenhanced scans tends to be very low, often near that of water. Adrenal lesions with attenuation values of < 0 HU have been shown to represent adrenal adenomas. Korobkin et al.,8 using a threshold of 10 HU, found an overall sensitivity of 73% and a specificity of 96%. Thus, they concluded that further workup is unnecessary when the lesion has an attenuation of ≤10 HU. Likewise, if some components in the liver tumor show distinctive low attenuation of <10 HU on unenhanced CT, HART should be added to the lists of differential diagnoses.
However, in our case, the mass did not show definite macroscopic fatty component on CT. Magnetic resonance image (MRI) could have aided the detection of fatty component in the mass, but we did not perform MRI exam. So, in this case, the main radiological findings were hypervascularity on arterial phase and wash-out on delayed phase, which was similar to HCC.
SUMMARY
A case of HART in a man without clinical symptoms is described. HART shows the following radiologic features: a solitary hepatic mass containing distinct components of fat and soft tissue attenuation; a round, well demarcated mass of the right posterior hepatic lobe in the subcapsular region; radiologic recognition of the original adrenal glands; blood supply of the tumor by the hepatic artery. However, if this disease itself is not in the lists of differential diagnoses, correct diagnosis is difficult only with radiologic or pathologic exams. HART should be added to the lists of radiologic differential diagnoses of hypervascular or fat-containing hepatic tumors.
References
- 1.Schechter DC. Aberrant adrenal tissue. Ann Surg. 1968;167:421–426. doi: 10.1097/00000658-196803000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Contreras P, Altieri E, Liberman C, Gac A, Rojas A, Ibarra A, et al. Adrenal rest tumor of the liver causing Cushing's syndrome: treatment with ketoconazole preceding an apparent surgical cure. J Clin Endocrinol Metab. 1985;60:21–28. doi: 10.1210/jcem-60-1-21. [DOI] [PubMed] [Google Scholar]
- 3.Arai K, Muro H, Suzuki M, Oba N, Ito K, Sasano H. Adrenal rest tumor of the liver: a case report with immunohistochemical investigation of steroidogenesis. Pathol Int. 2000;50:244–248. doi: 10.1046/j.1440-1827.2000.01029.x. [DOI] [PubMed] [Google Scholar]
- 4.Tajima T, Funakoshi A, Ikeda Y, Hachitanda Y, Yamaguchi M, Yokota M, et al. Nonfunctioning adrenal rest tumor of the liver: radiologic appearance. J Comput Assist Tomogr. 2001;25:98–101. doi: 10.1097/00004728-200101000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Baba Y, Beppu T, Imai K, Masuda T, Iyama K, Sasano H, et al. A case of adrenal rest tumor of the liver: radiological imaging and immunohistochemical study of steroidogenic enzymes. Hepatol Res. 2008;38:1154–1158. doi: 10.1111/j.1872-034X.2008.00360.x. [DOI] [PubMed] [Google Scholar]
- 6.Yoon HJ, Kim, SH, Park JB, Jo HC, Son MY, Kim TB, et al. Adrenal rest tumor from the greater omentum mimicking exophytic hepatocellular carcinoma (HCC): A case report. J Korean Soc Radiol. 2010;63:45–48. [Google Scholar]
- 7.Prasad SR, Wang H, Rosas H, Menias CO, Narra VR, Middleton WD, et al. Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics. 2005;25:321–331. doi: 10.1148/rg.252045083. [DOI] [PubMed] [Google Scholar]
- 8.Korobkin M, Brodeur FJ, Yutzy GG, Francis IR, Quint LE, Dunnick NR, et al. Differentiation of adrenal adenomas from nonadenomas using CT attenuation values. AJR Am J Roentgenol. 1996;166:531–536. doi: 10.2214/ajr.166.3.8623622. [DOI] [PubMed] [Google Scholar]