Abstract
Objectives
To investigate the association of caregivers’ oral health literacy (OHL) with their children's oral health related-quality of life (C-OHRQoL) and explore literacy as a modifier in the association between children's oral health status (COHS) and C-OHRQoL.
Methods
We relied upon data from structured interviews with 203 caregivers of children ages 3-5 from the Carolina Oral Health Literacy (COHL) Project. Data were collected for OHL using REALD-30, caregiver-reported COHS using the NHANES-item, and COHRQoL using the Early Childhood Oral Health Impact Scale (ECOHIS). We also measured oral health behaviors (OHBs) and socio-demographic characteristics and calculated overall/stratified summary estimates for OHL and C-OHRQoL. We computed Spearman's rho and 95% confidence limits (CL) as measures of correlation of OHL/COHS with C-OHRQoL. To determine whether OHL modified the association between COHS and C-OHRQoL, we compared literacy-specific summary and regression estimates.
Results
Reported COHS was: excellent—50%, very good—28%, good—14%, fair—6%, poor—2%. The aggregate C-OHRQoL mean score was 2.0 (95% CL:1.4, 2.6), and the mean OHL score 15.9 (95% CL:15.2, 16.7). There was an inverse relationship between COHS and C-OHRQoL: rho=-0.32 (95% CL:-0.45, -0.18). There was no important association between OHL and C-OHRQoL; however, deleterious OHBs were associated with worse C-OHRQoL. Literacy-specific linear and Poisson regression estimates of the association between COHS and C-OHRQoL departed from homogeneity (Wald X2 P<0.2).
Conclusion
In this community-based sample of caregiver/child dyads, we found a strong correlation between OHS and C-OHRQoL. The association's magnitude and gradient were less pronounced among caregivers with low literacy.
Keywords: Oral Health Literacy, Oral Health-related Quality of Life, Children, Early Childhood, Subjective Oral Health, REALD-30
Introduction
The significance of multi-level consequences of childhood oral diseases is gaining the acknowledgment of professional societies and other stakeholders [1-6]. Above and beyond their clinical sequelae, early childhood caries (ECC) and orofacial trauma are the most prevalent dental conditions that confer well-documented psychological, social, and financial impacts on both the child and the family [2,7]. Despite improvements in many oral health indicators over the last decades, ECC in particular has increased among vulnerable pediatric populations in the US and beyond [8,9]. This is a major public health issue because dental caries may affect children's social and psychological well-being and has been linked to missed school days, parental lost work time, direct and indirect costs, and more [10-13].
Caregivers’ perceptions of their young children's oral health status (COHS) are uniquely valuable when considering childhood oral health because vulnerability to ECC has been linked to family- and parent-level factors [14-17]. Early childhood oral health behaviors, such as nighttime bottle feeding, snacking, and juice consumption, have been linked to parental level of education and at the same time, oral hygiene, decisions about utilization of dental services, and dental care are the exclusive domain of the caregiver [14,18,19]. Consequently, determinants of dental care-seeking behaviors are likely to include family-level characteristics such as awareness and recognition of oral conditions or symptoms, as well as the extent to which parents value oral health [20-24]. Although there is a dearth of evidence in this dimension, Talekar and colleagues [25] found a good correlation between parental reports and actual clinical dental status of children.
Measures of child oral health related quality of life (C-OHRQoL) encompass the broad spectrum of childhood oral disease impacts [26-27]. Instruments that are age-specific for children have been developed only recently and include versions of the parent and child components of the Child Oral Health Quality of Life Questionnaire [28-29] and the Early Childhood Oral Health Impact Scale (ECOHIS) [30]. Due to the inclusivity of a variety of child- and family-level impacts, C-OHRQoL instruments are considered valid and sensitive measures of the sequelae of oral disease [27]. For example, they have been employed to measure the impact of oral conditions and diseases [31], assess the effect of parental factors [32] and assess C-OHRQoL changes after various treatments [33-36].
Oral health literacy (OHL) has emerged as an important determinant of oral health [37]. OHL has been defined by the National Institutes of Dental and Craniofacial Research (NIDCR) as “the degree to which individuals have the capacity to obtain, process, and understand basic oral health information and services needed to make appropriate health decisions” [38]. Recent research has confirmed an association of low OHL with a plethora of outcomes such as worse oral health status, dental neglect, increased OHRQoL impacts, and sporadic use of dental services [39-41]. Because of its pivotal role in one's ability to recognize oral health information and act upon it, we anticipate that OHL may affect the manner in which caregivers’ report their children's oral status, as well as their perception and experience of oral health-related child- and family-level impacts. Specifically, we hypothesized that low caregiver OHL would be associated with worse C-OHRQoL, but also with decreased caregiver perception/report of C-OHRQoL impacts. Accordingly, the aims of this investigation were 1) investigate the association of OHL with C-OHRQoL and 2) explore the role of OHL as a modifier in the association between early childhood OHS and C-OHRQoL.
Materials and methods
Study design and population
We relied upon interview data from the Carolina Oral Health Literacy (COHL) project [39], a prospective study examining the OHL's relationship with health behaviors and health outcomes among caregivers, infants, and children enrolled in the Women, Infants and Children's (WIC) Supplemental Food Program in seven counties of North Carolina (NC) in the United States of America. COHL used purposeful quota sampling [42] to ensure adequate study sample representation of minority groups (African Americans and American Indians). To minimize potential non-random data missingness associated with low literacy two trained research assistants undertook all data collection via structured interviews.
After excluding men (N=49, 3.5% of total), Asians (N=12, 0.9% of total) and those who did not have English as their primary language (N=79, 5.6% of total), there were 1,280 caregiver/child dyads in the COHL cohort. A detailed description of the caregiver/child dyads cohort, as well as the association of OHL with early childhood oral health outcomes, has been reported by Vann and colleagues [18].
The analytical sample for the present investigation was limited to a subset of the previously reported COHL project dyads [18] that included all caregivers with children ages 3-5 who completed the Early Childhood Oral health Impact Scale (ECOHIS) instrument because ECHOHIS has been validated only in the preschool-age population [30]. Due to a protocol deviation, the instrument was administered to four caregivers with children younger than 36 months (two were 33, one was 34 and one was 35mos). We included these observations in the final analytical sample that included 203 caregiver/child dyads.
Variables and instruments
We measured OHL with REALD-30, a validated word recognition literacy test [43], where 0=lowest literacy and 30=highest literacy. To date there are no norms established to indicate a score for “adequate” OHL. As in a previous investigation, we relied upon an arbitrary cutoff of <13 to indicate “low” OHL [18]. This cutoff point also represented the lowest quartile of OHL scores distribution among our analytical sample and therefore, using this threshold, 25% of our sample (N=51) was classified as “low” OHL. The children's oral health status was assessed with the National Health and Nutrition Examination Survey (NHANES) item: “How would you describe the condition of your child's teeth?” Answers to this question were coded as: 5=“excellent”, 4=“very good”, 3=“good”, 2=“fair” and 1=“poor”.
We measured C-OHRQoL with ECOHIS, an instrument designed to capture oral health impacts on preschool children and their families [30]. ECOHIS has been validated in a convenience sample of mostly high-income parents of 5 year-old children and has been shown to possess good psychometric properties and internal consistency. The range of aggregate ECOHIS score is 0-52; 0-36 for the child (CS) and 0-16 for the family scale (FS). Cronbach's alpha was 0.95 for the FS and 0.91 for the CS, and these scales correlated well among themselves with a Spearman's rho of 0.36 [30].
The authors of ECHOIS recommended [30] that the instrument be tested among parents of younger children and other study groups to establish its external validity. Subsequently, ECOHIS has been adapted and validated in several other languages including French [44], Portuguese [45], Chinese [46], and Farsi [47]. Although the two distinct ECOHIS sub-scales were originally proposed to measure child- and family-level impacts, other authors have considered the aggregate ECOHIS score as a measure of overall impact [31,34,35,48]. In this study we computed both total and sub-scale OHS-specific estimates but for analytical purposes, we focused only upon the total (aggregate) ECOHIS score.
We assessed children's oral health behaviors (OHBs) for nighttime bottle feeding, frequency of juice intake, and consumption of sweets. The range of responses for nighttime bottle feeding were “never”, “sometimes”, and “usually”, whereas for feeding behaviors they were “never/occasionally”, “once a day”, and “more than once a day”. Demographic variables included caregiver's age, education, and race, which was self-reported and defined as White, African American (AA) or American Indian (AI), and coded as an indicator variable. Age was measured in years and coded as a quartile-categorical variable. Education was coded as a four-level categorical variable where 1=less than high school, 2=high school or GED, 3=some technical or college, and 4=college degree or higher.
Analytical approach
Our analyses relied on descriptive, graphical, parametric, and non-parametric methods. We examined the internal consistency of ECOHIS instrument by obtaining Cronbach's alphas for the entire scale, as well as for FS and CS. We computed descriptive statistics (means, standard errors, and ranges) of C-OHRQoL and OHL scores for strata of demographic and behavior variables. We examined the distribution of OHL and C-OHRQoL scores with histograms and tested the assumption of normality using a combined skewness and kurtosis test [49] and a P<0.05 criterion. To quantify the association of OHL and COHS with C-OHRQoL, we used Spearman's rho and 95% confidence limits (CL), estimated using bootstrapping (n=1,000 repetitions). We embraced Spearman's rho and ANOVA-based R2 to obtain estimates of correlation between the two subscales of the C-OHRQoL measure.
To determine whether OHL modified the association between COHS and COHRQoL, first we empirically inspected literacy-stratified C-OHRQoL mean scores for categories of OHS, as well as bar graphs. Next we utilized multivariate linear regression to model the association between OHS and C-OHRQoL, including race, education, and age as a priori confounders. We used a Wald X2 test (with a conservative P-value threshold of <0.2) to test formally the hypothesis of a common estimate (homogeneity) of the association between OHS and C-OHRQoL between strata of literacy [50]. Because previous investigators [31,32] employed Poisson regression to model the particularly skewed distribution of C-OHRQoL scores, we repeated the evaluation of effect measure modification (EMM) using multivariate Poisson regression models. For both contrasts of estimates, the homogeneity statistic was distributed with one degree of freedom (number of strata – 1) and computed as follows: X2= [(βlow-βcommon]2 + [(βhigh-βcommon)2/sehigh2]. For all analyses, we relied upon the statistical program Stata 11.1 (Stata Corp LP, College Station, TX, USA) for all analyses.
Results
The distribution of OHL and C-OHRQoL scores by demographic and behavior variables is presented in Table 1. The total C-OHRQoL score was right-skewed (D’Agostino X2 P<0.05) with mean=2.0 (95% CL= 1.4, 2.6) and range=0-28. Cronbach's alpha was 0.86. The child scale revealed a mean of 1.2 (95% CL= 0.8, 1.5) with a range of 0-19 and an alpha of 0.79. The family scale revealed a mean of 0.8 (95% CL: 0.5, 1.1) with a range of 0-12 and alpha of 0.75. The two scales were strongly correlated with Spearman's rho of 0.46 (95% CL=0.32, 0.61) and R2=0.64. The OHL score was distributed normally (D’Agostino X2 P>0.05) with a mean of 15.9 (95% CL= 15.2, 16.7) and range of 2-29.
Table I.
Distribution of Early Childhood Oral Health- Related Quality of Life (C-OHRQoL-ECOHIS) and Oral Health Literacy (REALD-30) scores [(mean and 95% confidence limits (CL)] by caregiver demographic characteristics and Child Oral Health Behaviors among the COHL-ECOHIS study caregiver-child dyads (n=203).
| C-OHRQoL | OHL | |||
|---|---|---|---|---|
| Demographics | n | % | ECOHIS total score (95% CL) | REALD-30 score (95% CL) |
| Entire sample | 203 | 100 | 2.0 (1.4, 2.6) | 15.9 (15.2, 16.7) |
| Race | ||||
| White | 84 | 41.4 | 1.8 (1.1, 2.6) | 17.6 (16.6, 18.7) |
| African American | 73 | 36.0 | 1.7 (0.7. 2.6) | 15.2 (14.1, 16.3) |
| American Indian | 46 | 22.7 | 2.7 (0.9, 4.4) | 14.0 (12.4, 15.7) |
| Education | ||||
| Did not finish high school | 61 | 30.0 | 2.2 (1.1, 3.3) | 12.8 (11.6, 13.9) |
| High school diploma of GED | 72 | 35.5 | 2.3 (0.9, 3.6) | 15.9 (14.9, 16.9) |
| Some technical or college | 58 | 28.6 | 1.4 (0.8, 2.1) | 17.8 (16.6, 18.9) |
| College degree or higher | 12 | 5.9 | 1.4 (0.0, 2.8) | 23.5 (20.9, 26.1) |
| Age quartiles (years) | Mean(SD) | |||
| Q1 (range: 18.3-23.7) | 51 | 21.8(1.4) | 2.9 (1.3, 4.4) | 14.7 (13.3, 16.1) |
| Q2 (range: 23.7-27.1) | 51 | 25.0(1.0) | 1.5 (0.4, 2.7) | 16.8 (15.6, 18.0) |
| Q3 (range: 27.1-30.7) | 51 | 28.8(1.1) | 1.2 (0.5, 1.9) | 15.5 (13.9, 17.2) |
| Q4 (range: 30.8-57.1) | 50 | 36.1(5.4) | 2.2 (0.9, 3.5) | 16.8 (15.3, 18.3) |
| Child Oral Health Behaviors | ||||
| Have put the child in bed with bottle | ||||
| Never | 132 | 65.0 | 1.2 (0.8, 1.6) | 16.3 (15.4, 17.3) |
| Sometimes | 38 | 18.7 | 2.8 (1.0, 4.6) | 14.6 (12.9, 16.2) |
| Usually | 33 | 16.3 | 4.0 (1.4, 6.6) | 15.9 (14.4, 17.5) |
| Frequency of juice consumption | ||||
| Never/Occasionally | 59 | 29.1 | 2.0 (0.9, 3.1) | 15.6 (14.4, 16.9) |
| Once a day | 59 | 29.1 | 1.6 (0.7, 2.5) | 16.1 (14.6, 17.6) |
| More than once a day | 85 | 41.9 | 2.2 (1.1, 3.2) | 16.0 (15.0, 17.1) |
| Frequency of sweet snacks consumption | ||||
| Never/Occasionally | 122 | 60.1 | 1.2 (0.7, 1.7) | 16.1 (15.2, 17.1) |
| Once a day | 50 | 24.6 | 2.7 (1.3, 4.1) | 15.8 (14.3, 17.3) |
| More than once a day | 31 | 15.3 | 3.7 (1.1, 6.3) | 15.4 (13.6, 17.2) |
Caregivers’ and children's median age was 27 years (range=18-57) and 43 months (range=33-59), respectively. Two-thirds of caregivers had high school diploma, GED, or less, 41% were Whites, 36% AAs and 23% AIs. One-third reported a history of nighttime bottle use and more than 40% reported the child's juice consumption as greater than once daily. Pronounced gradients were noted in literacy scores between racial and age groups, as well as levels of education. The caregivers’ educational level was inversely related to C-OHRQoL scores, which varied by caregivers’ age. The examination of deleterious child oral health practices, particularly nighttime bottle feeding and frequency of sweets consumption, revealed these OHBs to be associated with lower OHL and worse C-OHRQoL.
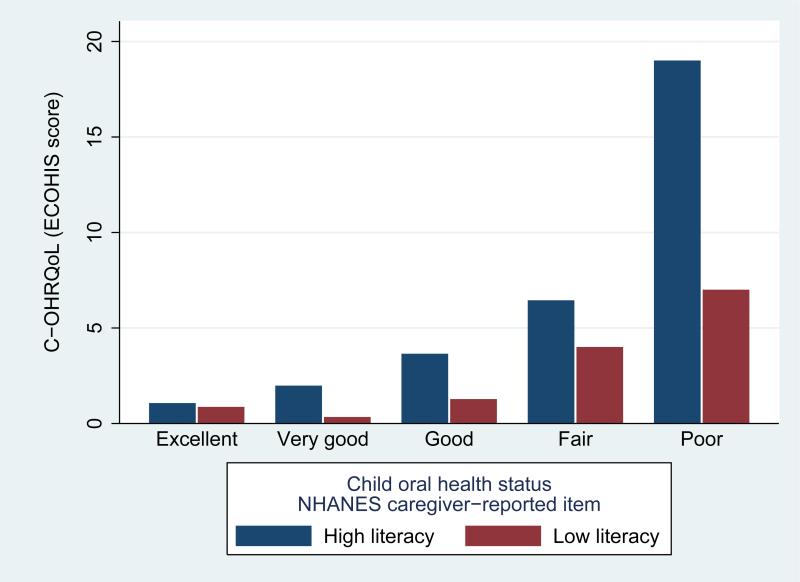
The distribution of caregiver-reported COHS was: excellent—50%, very good—28%, good—14%, fair—6 %, and poor—2 % (Table 2). Better C-OHS was associated with decreased ECOHIS scores: rho=-0.32 (95% CL= -0.45, -0.18) while OHL was weakly correlated with C-OHRQoL: rho=0.10 (95% CL= -0.03, 0.23). Comparison of literacy-specific estimates in Table 2 indicated that OHL, despite its weak association with C-OHRQoL, has the properties of an effect modifier. This is illustrated as well with the stratified bar graphs in Figure 1, where it is evident that among caregivers with “low” literacy (<13 REALD-30), the magnitude and gradient of the association between OHS and C-OHRQoL was less pronounced.
Table II.
Early Childhood Oral Health- Related Quality of Life (C-OHRQoL-ECOHIS) scores [(mean and standard deviation (SD)] by caregiver-reported Child Oral Health Status (COHS) for the entire study sample (n=203) and stratified by oral health literacy (OHL) level (“high” OHL: ≥13 REALD-30; “low” OHL: <13 REALD-30 score).
| Child OH Status | C-OHRQoL-ECOHIS | |||||
|---|---|---|---|---|---|---|
| n | % | Total score (SD) | Family scale (SD) | Child scale (SD) | ||
| Entire sample | ||||||
| Excellent | 101 | 49.7 | 1.0(3.1) | 0.4 (1.2) | 0.6 (2.1) | |
| Very good | 57 | 28.1 | 1.6(2.6) | 0.8 (1.6) | 0.9 (1.4) | |
| Good | 28 | 13.8 | 2.7(5.6) | 0.8 (1.9) | 0.8 (4.1) | |
| Fair | 13 | 6.4 | 5.7(6.3) | 2.4 (2.7) | 1.1 (3.9) | |
| Poor | 4 | 2.0 | 13(11.1) | 6.8 (5.1) | 3.1 (6.3) | |
| “High” OHL | ||||||
| Excellent | 79 | 52.0 | 1.1(3.2) | 0.4 (1.2) | 0.7 (2.2) | |
| Very good | 45 | 29.6 | 2.0(2.9) | 1.0 (1.8) | 1.0 (1.5) | |
| Good | 17 | 11.2 | 3.6(6.8) | 1.1 (2.3) | 2.6 (5.1) | |
| Fair | 9 | 5.9 | 6.4(6.3) | 2.8 (2.6) | 3.7 (4.1) | |
| Poor | 2 | 1.3 | 19.0(11.3) | 9.0 (4.2) | 10.0 (7.1) | |
| “Low” OHL | ||||||
| Excellent | 22 | 43.1 | 0.9(2.8) | 0.4 (1.1) | 0.5 (1.7) | |
| Very good | 12 | 23.5 | 0.3(0.7) | 0.0 (0.0) | 0.3 (0.7) | |
| Good | 11 | 21.6 | 1.3(2.2) | 0.5 (0.9) | 0.8 (1.6) | |
| Fair | 4 | 7.8 | 4.0(6.7) | 1.5 (3.0) | 2.5 (3.8) | |
| Poor | 2 | 3.9 | 7.0(9.9) | 4.5 (6.4) | 2.5 (3.5) | |
Figure.
Bar graphs illustrating the mean child oral health related quality of life scores (ECOHIS) by caregiver-reported child oral health status, for strata of caregiver oral health literacy (OHL; “low” literacy: <13 REALD-30; “high” literacy: ≥13 REALD-30) among the 203 caregiver-child dyads participating in the Carolina Oral Health Literacy (COHL) project.
The multiple linear regression estimates of the association between COHS and C-OHRQoL were: entire sample: β=-1.6 (95% CL=-2.2, -1.0)]; “low” literacy (<13 REALD-30 score): β=-0.9 (95% CL=-1.7, -0.1)]; “high” literacy (≥13 REALD-30 score): β=-2.0 (95% CL=-2.7, -1.3)]. We rejected the assumption of homogeneity (X2=4.1, df=1, P<0.2). The modifying role of OHL was again evident when comparing crude (unadjusted) linear regression estimates of the association between COHS and C-OHRQoL (data not shown). Similarly, effect measure modification was confirmed with the contrast of Poisson derived Incidence Rate Ratio (IRR) estimates: entire sample: IRR=0.55 (95% CL=0.51, 0.59)]; “low” literacy (<13 REALD-30 score): IRR =0.63 (95% CL=0.52, 0.75)]; “high” literacy (≥13 REALD-30 score): IRR =0.54 (95% CL=0.50, 0.59)]; homogeneity X2=2.0, df=1, P<0.2.
Discussion
This is the first investigation to examine the role of caregivers’ oral health literacy juxtaposed to their children's oral health status and C-OHRQoL. Oral health literacy was weakly associated with C-OHRQoL, however, as hypothesized it emerged as a significant modifier of the association between COHS and C-OHRQoL. We found a strong association between children's oral health status and C-OHRQoL in our sample of female caregivers and their preschool aged children. Deleterious behaviors such as nighttime bottle feeding and frequent sweet snacking were also associated with increased C-OHRQoL impacts.
Our study sample was comprised of non care-seeking community-based caregivers of 3-5 year olds and minority groups were well-represented, with 36% AA and 23% AI caregivers, factors that offer advances over previous investigations and increase the external validity of our findings. Of special note is the lower internal consistency of ECOHIS in our sample versus the validation study reported for high-income caregivers of 5-year old children [30].
We acknowledge that a potential study limitation of our findings is the inclusion of only female caregivers; additionally, only less than 10% of our caregivers reported fair or poor child oral health status. By contrast, 23% of parents rated their 0-5 year old children's oral health status as poor in a study that used a modified version of ECOHIS by Wandera and colleagues [51]. This limits our inferential potential for these strata. Furthermore, the cross-sectional nature of this investigation limits our potential to make any causal inferences with regard to pathways that may link low caregiver literacy with early childhood oral health outcomes and C-OHRQoL. However, the COHL project is prospective in nature, and upon analyses of follow up data of children's dental utilization, type of dental services and related costs, we anticipate gaining more insights into these hypothesized pathways.
The estimate of C-OHRQoL impacts (mean=2.0) in the present investigation is lower but comparable to the one reported by Goettems and colleagues [32] among non-care seeking samples of pre-school children. These authors reported a mean total score of 3.3 among a group of children (mean age= 43 months) participating in a national immunization campaign. In the Klaasen trial [35] among parents and children (mean age=48 months) referred for comprehensive treatment in specialized clinic, the baseline mean ECOHIS score was high, with a mean of 12.7. Care-seeking parents of children 2-5 years old attending a dental school screening program revealed a mean ECOHIS of 9.2 [31] while Lee and colleagues [34] reported caregivers of caries-free children to have a mean ECOHIS score of 2.9 versus 15.0 among parents of children with ECC. Du and colleagues [48] calculated ECOHIS scores on a 13-65 range; had these investigators used conventional scoring, mean ECOHIS score for healthy and cerebral palsy children would be 3.1 and 6.0 respectively.
Poor COHS was associated with increased C-OHRQoL impacts. Indeed, deleterious oral health behaviors such as nighttime bottle feeding and increased frequency of sweets consumption (that were associated with worse C-OHRQoL) can be considered a link in the causal chain that links literacy with poor oral health outcomes [18], although this effect may be weak [52]. It should be acknowledged that the accuracy of caregivers’ reports in all domains of their children's quality of life can be questioned [53]. Further, it must be underscored that caregivers’ perceptions are pivotal in initiating and sustaining oral health care for their children [54]. Evidence of marked differences in ECOHIS scores between care-seeking and non-care-seeking subjects is in concordance with a problem-initiated dental attendance pattern. Moreover, as an oral health-specific measure, ECHOHIS has been shown to perform better than generic child quality of life instruments in the oral health context [48,55].
Addressing children's unmet dental needs is an under-appreciated problem that warrants a systemic approach [56]. Watt and colleagues [57] recognized that oral health promotion efforts often are constrained by the lack of appropriate and high quality outcome measures. In the health context, literacy [58] is a recognized threat to the validity and performance of measures typically used in oral health research. In the present study, we hypothesized and confirmed that caregivers with low literacy may perceive or report subjective C-OHRQoL impacts differently versus those with higher literacy. In particular, the modifying effect of OHL corresponded to less pronounced gradient of the association between OHS and C-OHRQoL. This is consistent with Wilson and Cleary's modified conceptual model of patient outcomes [59] on which Wandera et al. [51] based their examination of the relationship of psychosocial factors with C-OHRQoL. This finding can be attributed to a different threshold of caregiver recognition or report of C-OHRQoL impacts relative their children's oral health status and one potential implication for oral health research is that low literacy may be associated with under-reporting of symptoms or quality of life impacts. To strengthen this link, the validity of caregivers’ reports of COHS should be examined across literacy levels.
Recently Mejia and colleagues [60] reported an inverse association between low parental functional health literacy and the presence of sealants on their third-grade children. Because OHL is been increasingly recognized as component of oral health disparities and is regarded as a vehicle to reduce them [61], further investigations are warranted to examine the potential role of OHL as a modifier of caregivers’ self-reports among larger and more diverse population-based samples. Based on this study's findings we recommend that participants’ OHL be considered in the design and interpretation of studies that examine health behaviors, outcomes, and quality of life impacts. We envision that the widespread reliance on OHL as a valuable component in clinical practice [62] and research [63] will be facilitated with the development of short, easily administered OHL screening instruments.
Acknowledgments
The COHL Project is supported by NIDCR Grant #RO1DE018045.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.American Academy of Pediatric Dentistry (AAPD) [April 12 2011];Definition of dental disability. 2008 Available at: http://www.aapd.org/media/Policies_Guidelines/D_DentalDisability.pdf.
- 2.American Academy of Pediatric Dentistry (AAPD) [April 12 2011];Policy on early childhood caries (ECC): Classification, consequences, and preventive strategies. 2008 Available at: http://www.aapd.org/media/Policies_Guidelines/P_ECCClassifications.pdf. [PubMed]
- 3.Hale KJ, American Academy of Pediatrics Section on Pediatric Dentistry Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 Pt 1):1113–6. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- 4.Mouradian WE. The face of a child: children's oral health and dental education. J Dent Educ. 2001;65:821–31. [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services . In: Oral Health in America: A Report of the Surgeon General. Rockville Md., editor. Vol. 7. National Institute of Dental and Craniofacial Research, National Institutes of Health, US Dept of Health and Human Services; 2000. pp. 158–68. [Google Scholar]
- 6.US Department of Health and Human Services . Healthy People 2010: Understanding and improving health. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 7.Lee JY, Divaris K. Hidden consequences of dental trauma: the social and psychological effects. Pediatr Dent. 2009;31:96–101. [PubMed] [Google Scholar]
- 8.Tomar SL, Reeves AF. Changes in the oral health of US children and adolescents and dental public health infrastructure since the release of the Healthy People 2010 Objectives. Acad Pediatr. 2009;9:388–95. doi: 10.1016/j.acap.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 9.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;248:1–92. [PubMed] [Google Scholar]
- 10.Cunnion DT, Spiro A, 3rd, Jones JA, Rich SE, Papageorgiou CP, Tate A, et al. Pediatric oral health-related quality of life improvement after treatment of early childhood caries: a prospective multisite study. J Dent Child (Chic) 2010;77:4–11. [PMC free article] [PubMed] [Google Scholar]
- 11.Blumenshine SL, Vann WF, Jr, Gizlice Z, Lee JY. Children's school performance: impact of general and oral health. J Public Health Dent. 2008;68:82–7. doi: 10.1111/j.1752-7325.2007.00062.x. [DOI] [PubMed] [Google Scholar]
- 12.Locker D, Jokovic A, Stephens M, Kenny D, Tompson B, Guyatt G. Family impact of child oral and oro-facial conditions. Community Dent Oral Epidemiol. 2002;30:438–48. doi: 10.1034/j.1600-0528.2002.00015.x. [DOI] [PubMed] [Google Scholar]
- 13.Ramos-Gomez FJ, Shepard DS. Cost-effectiveness model for prevention of early childhood caries. J Calif Dent Assoc. 1999;27:539–44. [PubMed] [Google Scholar]
- 14.Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, Bramlett MD, et al. Influences on children's oral health: a conceptual model. Pediatrics. 2007;120:e510–20. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 15.Mattheus DJ. Vulnerability related to oral health in early childhood: a concept analysis. J Adv Nurs. 2010;66:2116–25. doi: 10.1111/j.1365-2648.2010.05372.x. [DOI] [PubMed] [Google Scholar]
- 16.Weintraub JA, Prakash P, Shain SG, Laccabue M, Gansky SA. Mothers’ caries increases odds of children's caries. J Dent Res. 2010;89:954–8. doi: 10.1177/0022034510372891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mouradian WE, Huebner CE, Ramos-Gomez F, Slavkin HC. Beyond access: the role of family and community in children's oral health. J Dent Educ. 2007;71:619–31. [PubMed] [Google Scholar]
- 18.Vann WF, Jr, Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: impact on oral health outcomes in early childhood. J Dent Res. 2010;89:1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mouradian WE, Wehr E, Crall JJ. Disparities in children's oral health and access to dental care. JAMA. 2000;284:2625–31. doi: 10.1001/jama.284.20.2625. [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Zhang Y, Yang R, Zhang Q, Zou J, Kang D. Associations of social and behavioural factors with early childhood caries in Xiamen city in China. Int J Paediatr Dent. 2011;21:103–11. doi: 10.1111/j.1365-263X.2010.01093.x. [DOI] [PubMed] [Google Scholar]
- 21.Gussy MG, Waters EB, Riggs EM, Lo SK, Kilpatrick NM. Parental knowledge, beliefs and behaviours for oral health of toddlers residing in rural Victoria. Aust Dent J. 2008;53:52–60. doi: 10.1111/j.1834-7819.2007.00010.x. [DOI] [PubMed] [Google Scholar]
- 22.Qin M, Li J, Zhang S, Ma W. Risk factors for severe early childhood caries in children younger than 4 years old in Beijing, China. Pediatr Dent. 2008;30:122–8. [PubMed] [Google Scholar]
- 23.Finlayson TL, Siefert K, Ismail AI, Sohn W. Psychosocial factors and early childhood caries among low-income African-American children in Detroit. Community Dent Oral Epidemiol. 2007;35:439–48. doi: 10.1111/j.1600-0528.2006.00352.x. [DOI] [PubMed] [Google Scholar]
- 24.Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatr Dent. 2003;25:431–40. [PubMed] [Google Scholar]
- 25.Talekar BS, Rozier RG, Slade GD, Ennett ST. Parental perceptions of their preschool-aged children's oral health. J Am Dent Assoc. 2005;136:364–72. doi: 10.14219/jada.archive.2005.0179. [DOI] [PubMed] [Google Scholar]
- 26.Jokovic A, Locker D, Guyatt G. What do children's global ratings of oral health and well-being measure? Community Dent Oral Epidemiol. 2005;33:205–11. doi: 10.1111/j.1600-0528.2005.00210.x. [DOI] [PubMed] [Google Scholar]
- 27.McGrath C, Broder H, Wilson-Genderson M. Assessing the impact of oral health on the life quality of children: implications for research and practice. Community Dent Oral Epidemiol. 2004;32:81–5. doi: 10.1111/j.1600-0528.2004.00149.x. [DOI] [PubMed] [Google Scholar]
- 28.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Measuring parental perceptions of child oral health-related quality of life. J Public Health Dent. 2003;63:67–72. doi: 10.1111/j.1752-7325.2003.tb03477.x. [DOI] [PubMed] [Google Scholar]
- 29.Jokovic A, Locker D, Stephens M, Guyatt G. Agreement between mothers and children aged 11-14 years in rating child oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:335–43. doi: 10.1034/j.1600-0528.2003.00012.x. [DOI] [PubMed] [Google Scholar]
- 30.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children's oral health: the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 2007;5:6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abanto J, Carvalho TS, Mendes FM, Wanderley MT, Bönecker M, Raggio DP. Impact of oral diseases and disorders on oral health-related quality of life of preschool children. Community Dent Oral Epidemiol. 2011;39:105–14. doi: 10.1111/j.1600-0528.2010.00580.x. [DOI] [PubMed] [Google Scholar]
- 32.Goettems ML, Ardenghi TM, Romano AR, Demarco FF, Torriani DD. Influence of maternal dental anxiety on oral health-related quality of life of preschool children. Qual Life Res. 2010 doi: 10.1007/s11136-010-9816-0. In Press. [DOI] [PubMed] [Google Scholar]
- 33.Thomson WM, Malden PE. Assessing change in the family impact of caries in young children after treatment under general anaesthesia. Acta Odontol Scand. 2011 doi: 10.3109/00016357.2011.554862. In Press. [DOI] [PubMed] [Google Scholar]
- 34.Lee GH, McGrath C, Yiu CK, King NM. Sensitivity and responsiveness of the Chinese ECOHIS to dental treatment under general anaesthesia. Community Dent Oral Epidemiol. 2011 doi: 10.1111/j.1600-0528.2010.00604.x. In Press. doi: 10.1111/j.1600-0528.2010.00604.x. [DOI] [PubMed] [Google Scholar]
- 35.Klaassen MA, Veerkamp JS, Hoogstraten J. Young children's Oral Health-Related Quality of Life and dental fear after treatment under general anaesthesia: a randomized controlled trial. Eur J Oral Sci. 2009;117:273–8. doi: 10.1111/j.1600-0722.2009.00627.x. [DOI] [PubMed] [Google Scholar]
- 36.Li S, Malkinson S, Veronneau J, Allison PJ. Testing responsiveness to change for the early childhood oral health impact scale (ECOHIS). Community Dent Oral Epidemiol. 2008;36:542–8. doi: 10.1111/j.1600-0528.2008.00434.x. [DOI] [PubMed] [Google Scholar]
- 37.Horowitz AM, Kleinman DV. Oral health literacy: the new imperative to better oral health. Dent Clin North Am. 2008;52:333–44. doi: 10.1016/j.cden.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 38.National Institute of Dental and Craniofacial Research. National Institute of Health. U.S. Public Health Service. Department of Health and Human Services The invisible barrier: Literacy and its relationship with oral health. A report of a workgroup sponsored by the national institute of dental and craniofacial research, national institute of health, U.S. public health service, department of health and human services. J Public Health Dent. 2005;65:174–182. doi: 10.1111/j.1752-7325.2005.tb02808.x. [DOI] [PubMed] [Google Scholar]
- 39.Lee JY, Divaris K, Baker AD, Rozier RG, Lee SY, Vann WF., Jr Oral health literacy levels among a low income population. J Public Health Dent. 2011 doi: 10.1111/j.1752-7325.2011.00244.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Divaris K, Lee JY, Baker D, Vann WF., Jr Oral health literacy and subjective oral health. J Dent Res. 2010;89:873. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Baker D, Lee JY, Divaris K, Vann WF., Jr Do health literacy and self-efficacy beliefs affect dental behaviors? J Dent Res. 2010;89:1389. [Google Scholar]
- 42.Kalton G. Models in the practice of survey sampling. International Statistical Review. 1983;51:175–88. [Google Scholar]
- 43.Lee JY, Rozier RG, Lee SY, Bender D, Ruiz RE. Development of a word recognition instrument to test health literacy in dentistry: the REALD-30 -- a brief communication. J Public Health Dent. 2007;67:94–8. doi: 10.1111/j.1752-7325.2007.00021.x. [DOI] [PubMed] [Google Scholar]
- 44.Li S, Veronneau J, Allison PJ. Validation of a French language version of the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual Life Outcomes. 2008;6:9. doi: 10.1186/1477-7525-6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tesch FC, Oliveira BH, Leão A. [Semantic equivalence of the Brazilian version of the Early Childhood Oral Health Impact Scale]. Cad Saude Publica. 2008;24:1897–909. doi: 10.1590/s0102-311x2008000800018. [DOI] [PubMed] [Google Scholar]
- 46.Lee GH, McGrath C, Yiu CK, King NM. Translation and validation of a Chinese language version of the Early Childhood Oral Health Impact Scale (ECOHIS). Int J Paediatr Dent. 2009;19:399–405. doi: 10.1111/j.1365-263X.2009.01000.x. [DOI] [PubMed] [Google Scholar]
- 47.Jabarifar SE, Golkari A, Ijadi MH, Jafarzadeh M, Khadem P. Validation of a Farsi version of the early childhood oral health impact scale (F-ECOHIS). BMC Oral Health. 2010;10:4. doi: 10.1186/1472-6831-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Du RY, McGrath C, Yiu CK, King NM. Health- and oral health-related quality of life among preschool children with cerebral palsy. Qual Life Res. 2010;19:1367–71. doi: 10.1007/s11136-010-9693-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.D'Agostino RB, Balanger A, D'Agostino RB., Jr A suggestion for using powerful and informative tests of normality. American Statistician. 1990;44:316–321. [Google Scholar]
- 50.Greenland S, Rothman KJ. Introduction to stratified analysis. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. Lippincott, Williams and Wilkins; New York: 2008. pp. 258–82. [Google Scholar]
- 51.Wandera M, Kayondo J, Engebretsen IM, Okullo I, Astrøm AN. Factors associated with caregivers’ perception of children's health and oral health status: a study of 6- to 36-month-olds in Uganda. Int J Paediatr Dent. 2009;19:251–62. doi: 10.1111/j.1365-263X.2009.00969.x. [DOI] [PubMed] [Google Scholar]
- 52.Miller E, Lee JY, DeWalt DA, Vann WF., Jr Impact of caregiver literacy on children's oral health outcomes. Pediatrics. 2010;126:107–14. doi: 10.1542/peds.2009-2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jokovic A, Locker D, Guyatt G. How well do parents know their children? Implications for proxy reporting of child health-related quality of life. Qual Life Res. 2004;13:1297–307. doi: 10.1023/B:QURE.0000037480.65972.eb. [DOI] [PubMed] [Google Scholar]
- 54.Brickhouse TH. Family oral health education. Gen Dent. 2010;58:212–9. [PubMed] [Google Scholar]
- 55.Lee GH, McGrath C, Yiu CK, King NM. A comparison of a generic and oral health-specific measure in assessing the impact of early childhood caries on quality of life. Community Dent Oral Epidemiol. 2010;38:333–9. doi: 10.1111/j.1600-0528.2010.00543.x. [DOI] [PubMed] [Google Scholar]
- 56.Kopelman LM, Mouradian WE. Do children get their fair share of health and dental care? J Med Philos. 2001;26:127–36. doi: 10.1076/jmep.26.2.127.3026. [DOI] [PubMed] [Google Scholar]
- 57.Watt RG, Harnett R, Daly B, Fuller SS, Kay E, Morgan A, et al. Evaluating oral health promotion: need for quality outcome measures. Community Dent Oral Epidemiol. 2006;34:11–7. doi: 10.1111/j.1600-0528.2006.00257.x. [DOI] [PubMed] [Google Scholar]
- 58.Al-Tayyib AA, Rogers SM, Gribble JN, Villarroel M, Turner CF. Effect of low medical literacy on health survey measurements. Am J Public Health. 2002;92:1478–80. doi: 10.2105/ajph.92.9.1478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273:59–65. [PubMed] [Google Scholar]
- 60.Mejia GC, Weintraub JA, Cheng NF, Grossman W, Han PZ, Phipps KR, et al. Language and literacy relate to lack of children's dental sealant use. Community Dent Oral Epidemiol. 2010 doi: 10.1111/j.1600-0528.2010.00599.x. In Press. doi: 10.1111/j.1600-0528.2010.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Allukian M., Jr The neglected epidemic and the surgeon general's report: a call to action for better oral health. Am J Public Health. 2008;98:S82–5. doi: 10.2105/ajph.98.supplement_1.s82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jackson RD, Coan LL, Hughes E, Eckert GJ. Introduction of health literacy into the allied dental curriculum: first steps and plans for the future. J Dent Educ. 2010;74:318–24. [PubMed] [Google Scholar]
- 63.Jackson RD, Eckert GJ. Health literacy in an adult dental research population: a pilot study. J Public Health Dent. 2008;68:196–200. doi: 10.1111/j.1752-7325.2007.00063.x. [DOI] [PubMed] [Google Scholar]