Abstract
Smoking remains prevalent among U.S. youth despite decades of antismoking efforts. Effects from exposure to prevention programs at national level may provide informative and compelling data supporting better planning and strategy for tobacco control.
A national representative sample of youth 12–17 years of age from the National Survey on Drug Use and Health was analyzed. A 3-stage model was devised to estimate smoking behavior transitions using cross-sectional data and the Probabilistic Discrete Event System method. Cigarette smoking measures (prevalence rates and odds ratios) were compared between exposed and non-exposed youth.
More than 95% of the sample was exposed to prevention programs. Exposure was negatively associated with lifetime smoking and past 30-day smoking with a dose-response relation. Reduction in smoking was related to increased quitting in 2000–02, to increased quitting and declined initiation in 2003–05, and to initiation, quitting and relapse in 2005–08.
Findings of this analysis suggest that intervention programs in the United States can reduce cigarette smoking among youth. Quitting smoking was most responsive to program exposure and relapse was most sensitive to funding cuts since 2003. Health policy and decision makers should consider these factors in planning and revising tobacco control strategies.
Keywords: Adolescents, Community, Probabilistic Discrete Event System, Tobacco use prevention, United States
1. Introduction
A majority of adult smokers in the United States (US) report that they tried their first cigarette before the age of 18, and more than 80% of established smokers initiated smoking prior to high school graduation (US Department of Health and Human Services, 1994). Moreover, earlier smoking initiation is associated with greater smoking frequency and number of cigarettes smoked per day (Everett, et al., 1999). Overall, it is estimated that only 5% of established smokers are ever able to quit smoking completely (Chassin, Presson, Pitts, & Sherman, 2000). Thus, preventing adolescents from smoking is a critical and strategic priority for tobacco control.
2. Smoking prevention programs
A number of theory-based behavioral prevention programs have been devised and evaluated through randomized controlled trials (National Institute on Drug Abuse, 2003a; Thomas & Perera, 2006; US Department of Education, 2001; US Department of Health and Human Services, 2000). Typical examples of these programs include “Life Skills Training” (LST) (Botvin, Baker, Dusenbury, Botvin, & Diaz, 1995; Zollinger, et al., 2003), Midwestern Prevention Project (MPP) (Pentz, et al., 1989), “Project Towards No Tobacco Use” (TNT) (Dent, et al., 1995; Sussman, et al., 1993), “Know Your Body” (KYB) (Walter, 1989), “The Tobacco and Alcohol Prevention Project” (TAPP) (Hansen, Johnson, Flay, Graham, & Sobel, 1988), “Class of 1989 Study of the Minnesota Heart Health Program” (MHHP) (Perry, Kelder, Murray, & Klepp, 1992) and “Project Adolescent Learning Experience In Resistance Training” (ALERT) (Ellickson, Bell, & McGuigan, 1993), to name a few. A review of 94 randomized trials to assess various smoking prevention programs indicated the efficacy of behavioral interventions in delaying and preventing smoking initiation among children (aged 5–12) and adolescents (12–18) in the US (Thomas & Perera, 2006). With the guidance of the CDC, prevention programs have been implemented in a variety of settings across the nation, including schools and communities.
2.1. Approaches to smoking prevention
Smoking prevention programs have been implemented in various settings, particularly schools and communities. School-based programs were developed early in prevention efforts and continue to be among the most commonly used (Dobbins, DeCorby, Manske, & Goldblatt, 2008; National Institute on Drug Abuse, 2003a; Sherman & Primack, 2009; United Nations Office on Drugs and Crime, 2004). Schools are a place where students spend most of their time interacting with each other, representing an ideal venue for diffusion of information and for intervention programs targeting the influence of peers (Roberts-Gray, Gingiss, & Boerm, 2007; United Nations Office on Drugs and Crime, 2004).
The broader community may also serve as a forum for prevention efforts. Community organizations are able to mobilize resources to reach adolescents after school, and to spread anti-tobacco norms through social interactions and directly target tobacco outlets (National Institute on Drug Abuse, 2003a). Family, as a core part of community, may provide one of the most effective approach to reach youth because of the role of parents in tobacco use prevention (Ashery, Robertson, & Kumpfer, 1998; Bauman, et al., 2001). Mass media provides another venue for smoking prevention because of the potential for wide-reaching coverage, message promotion (Bala, Strzeszynski, & Cahill, 2008) and high cost-effectiveness (Secker-Walker, Worden, Holland, Flynn, & Detsky, 1997). For instance, highly visible nationwide anti-tobacco campaigns have utilized posters and billboards to spread the anti-smoking messages (National Institute on Drug Abuse, 2003a).
2.2. Challenges in evaluating prevention programs
Although substance use prevention programs recommended by the CDC have been shown to be effective (Thomas & Perera, 2006; US Department of Health and Human Services, 2000), how to evaluate the effect of these programs in practice is challenging. First, the settings to implement the recommended program may differ from the settings in which the evidence-based program was developed. Therefore, we cannot simply assume that a program that has been found to be effective in a controlled research setting will be effective in a practical setting. Second, many prevention practice programs lack a clearly defined, randomly assigned comparison group to effectively demonstrate that changes in behaviors are attributed to the intervention. It is also difficult to compare the efficacy of a program across different settings (e.g., across different communities) with and without the intervention. Furthermore, a program that has been found to be effective in one community may not necessarily prove to be as effective when implemented in another community. Lastly, historical pre- and post- comparisons can be used as an alternative for program effect evaluation, such as the data regarding the historical trends in tobacco use among US adolescents (Centers for Disease Control and Prevention, 2010; Johnston, 2010; US Department of Health and Human Services, 2000). However, this type of trend analysis often does not distinguish between youth who have been exposed to substance use interventions and youth who have not, so it is difficult to attribute improvements to program implementation.
In addition to evaluation of specific programs, it is also important to assess the impact of changes in funding for tobacco use prevention and control. For example, there was a progressive increase in funding for tobacco control up to 2002, after the signature of the Master Settlement Agreement between the Attorneys General of 46 US states and the largest tobacco companies in 1998. However, the funding was substantially cut since 2003 (Dietz, et al. 2010). A few studies have examined the impact of this funding cut at the local levels (Dietz, et al. 2010; Gingiss & Boerm, 2009; Ibrahim & Glantz, 2007; Niederdeppe, et al., 2008; Pizacani, et al., 2009; Sly, et al., 2005). However, information is lacking regarding the overall impact of this funding cut on prevention programs and the effect of tobacco control at the national level.
In addition to methodological challenges described above, transitional and dynamic measures are needed to quantify adolescent smoking behavior in addition to static prevalence measures. Unlike adults, smoking behavior in adolescents tends to changes rapidly (Chassin, et al., 2000; Chen, Li et al. 2001; Chen and Unger 1999; Kandel, Kiros, Schaffran, & Hu, 2004). When assessing program effect, prevalence rates (e.g., past 30-day smoking and lifetime smoking prevalence) are often used. Although prevalence data are useful to assess number of smokers during a specific period, there are limitations. Prevalence data do not provide information about the type of smoker (e.g., just initiated smoking vs. relapsed smoker) or the process of transitioning from one type of smoker to another that may be of great significance to program effect evaluation (Cavana & Tobias, 2008; Chen, Li et al. 2003; Chen, Stanton et al. 2011; Levy, Hyland, Higbee, Remer, & Compton, 2007). For example, among youth who are classified as current smokers (smoked on at least one day in the past month), some may just tried the first cigarette (initiator), some may have smoked regularly for years (regular smoker) after initiation, while some others may begin smoking again after quitting (relapsed smoker) (Chen, Li et al. 2003; Lin and Chen 2010; Chen, Stanton et al. 2011; Tobias, Cavana, & Bloomfield, 2010).
To overcome these challenges, new methodologies/analytical approaches are needed. Recently, we devised a method for such purpose. The method was developed based on the Probabilistic Discrete Event System (PDES) Theory, and it is capable of extracting longitudinal information from cross-sectional survey data (Author et al; Lin, F. & X. Chen, 2010; Shu, S., F. Lin, et al., 2008). This method requires only one wave of data from a cross-sectional survey to assess behavior progression. It treats individual cross-sectional surveys as a series of snapshots of a stable system, overcoming a number of challenges described above for program evaluation at the macro levels.
3. Objectives of this study
This study was conducted to better inform tobacco control planning and evaluation. We utilized a random sample of youth 12–17 years of age from the National Survey on Drug Use and Health (NSDUH, formally the National Household Survey on Drug Abuse). Since 1999, the NSDUH has been collecting data regarding substance use program exposure using a set of questions asking participants to report the locations (in school, out of school, in the community, at home, etc) and types of program exposure (lectures, billboards, movies) they have experienced (details of these questions are presented in Section 4.3 later in this paper).
Previous research has demonstrated that behavioral intervention programs targeting substance use in general are effective in reducing tobacco use among youth at the state and the national levels (Torre, Chiaradia, & Ricciardi, 2005; US Department of Health and Human Services, 2000). Thus, we had a unique opportunity to examine the potential effect of substance use prevention programs at the national level by comparing smoking behavior of the exposed youth with the non-exposed youth. We calculated the intensity of exposure to prevention programs and compared smoking behavior—as both static prevalence and dynamic transitions—for youth exposed to prevention programs and those not exposed. We then used the PDES method to compute smoking behavioral transitions using the cross-sectional data and used the estimated transitional probabilities to evaluate the responsiveness of smoking behavior to program exposure as well as funding cut for tobacco control since 2003 (Shu et al., 2008; Lin & Chen, 2010).
4. Data source and study sample
Data used for this analysis were derived from the 2000–08 NSDUH. Participants 12–17 years of age were included because data on exposure to community and school-based prevention programs were available only for participants in this age range. We selected the years from 2000 to 2008 because this period represents a time when significant changes occurred in tobacco use prevention in the United States, including sudden cuts in funding for tobacco control programs (Dietz, et al. 2010; Gingiss & Boerm, 2009; Ibrahim & Glantz, 2007; Niederdeppe, et al., 2008; Pizacani, et al., 2009; Sly, et al., 2005). To assess the association between exposure to substance use programs and changes in smoking behavior, participants were included if they had complete data on all questions assessing program exposure.
NSDUH is an annual household survey with a representative sample of around 70,000 civilian, non-institutionalized U.S. individuals aged 12 and older. Data collected through NSDUH are one of the primary sources for assessing the national levels of substance use in the US, including prevalence of cigarette smoking, overall and by ethnic groups (National Institute on Drug Abuse, 2003b). The survey is sponsored by the Substance Abuse and Mental Health Services Administration (SAMHSA), and conducted by the Research Triangle Institute (RTI) under contract since 1988. Households are randomly chosen using a multi-stage cluster sampling method to ensure the representativeness of the sample. Researchers were dispatched to the sampled households to collect data. The Computer-Assisted Personal Interviewing (CAPI) technique was used for questionnaire administration. More details about survey methodology are provided by the official technical reports (Substance Abuse and Mental Health Services Administration, 2006) and other related studies (Grucza, Abbacchi, Przybeck, & Gfroerer, 2007; Rodu & Cole, 2009).
One issue with the NSDUH data was a revision of the survey protocol in 2002 with the introduction of incentives of $30 to adolescent participants to enhance participation (Substance Abuse and Mental Health Services Administration, 2003). Although this revision showed an enhanced response rate than the previous version, findings from our analysis in this and other studies show no significant differences in the time trends in the prevalence of lifetime smoking and current smoking prior to and post 2002 when the survey protocol was revised (Chen et al., 2011).
4.1. Demographic characteristics
Basic demographic variables were assessed, including chronological age (in years), gender (male and female), and race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and Others). These variables were used to describe the characteristics of the study sample.
4.2. Measurement and modeling of smoking behavior
Four variables were defined and used to assess smoking behavior: never-smokers, lifetime smokers, current smokers, and ex-smokers. Participants were classified either as never-smokers (or NS) if they responded negatively to the question “Have you ever smoked part or all of a cigarette?” or lifetime smokers (or LS) if they responded positively to the same question. Participants were classified as current smokers (or CS) if they reported that the last time they smoked was within the past 30 days, based on their responses to the question: “How long has it been since you last smoked part or all of a cigarette?” (Answer options: 1 = within the past 30 days, 2 = before 30 days but within past 12 months, 3 = a year ago but within two years, and 4 = two years ago.) Participants were classified as ex-smokers (or XS) if they were classified as lifetime smokers and did not smoke in the past 30 days. The smoking types LS and CS were used to compute and compare prevalence rates of smoking between youth exposed to prevention programs with youth not exposed to any program; the smoking types NS, CS and XS were used for modeling as described below. Overall, LS were those who had never smoked in their lifetime, CS were those who smoked at least one day in the past month, and XS were those who had ever smoked, but had not smoked in the past month. These definitions allowed this study to model behavioral progression using the PDES method (Shu et al., 2008; Lin & Chen 2010).
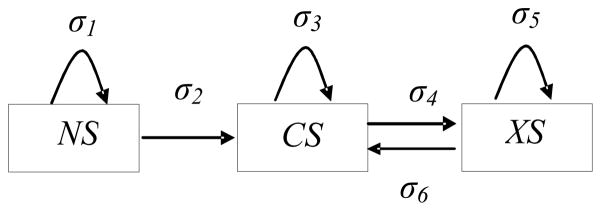
To model smoking progression using the PDES method and cross-sectional data, the proportion of three of the defined smoking types (e.g., NS, CS and XS, refer to Figure 1) were computed by age as the state probabilities. Although a number of other progression-based smokers can theoretically be defined (e.g. smoking experimenters, self-stoppers, addicted smokers) for more detailed modeling analysis, these types of smokers could not be operationally defined using the available NSDUH data. Despite this limitation, the types of smokers included reflect three key stages (NS, CS and XS) of adolescent smoking behavior progression as described in Figure 1. Such data are adequate for this study to assess the association between exposure to prevention programs and reductions in smoking behavior transition.
Figure 1. PDES Model of Smoking Behavior Progression for NSDUH Survey.
Note: NS = Never-smoker, CS = Current smoker, and XS = Ex-smoker. σi (i=1, 2, …6) are probabilities describing the rapidity at which one type of smokers remaining at the same stage or progress from one stage to another during one year period.
4.3. Assessment of exposure to prevention programs
Exposure to prevention programs in the past 12 months was assessed based on answers (Yes =1/No = 0) to a set of 6 questions included in the annual NSDUH: (1) “Have you had a special class about drugs or alcohol in school?” (2) “Have you had films, lectures, discussions, or printed information about drugs or alcohol in one of your regular school classes such as health or physical education?” (3) “Have you had films, lectures, discussions, or printed information about drugs or alcohol outside of one of your regular classes such as in a special assembly?” (4) “During the past 12 months have you seen or heard any alcohol or drug prevention messages from sources such as posters, pamphlets, radio, or TV?” (5) “Have you participated in an alcohol, tobacco or drug prevention program outside of school, where you learn about the dangers of using, and how to resist using, alcohol, tobacco, or drugs?” (6) “Have you talked with at least one of your parents about the dangers of tobacco, alcohol, or drug use?”
Although no specific prevention program was targeted, the content covered by these six questions provides a measure of the extent to which a participant was exposed to substance use prevention programs in the past year. Therefore we created a program exposure index (PEI) by summing up responses to all the questions with participants who scored 0 on PEI as the comparison group. In our data, 2.9% of participants scored 0 on the PEI measure. Although PEI = 0, in an exact sense, does not necessarily mean no any program exposure at all, the index provides a good proxy of program exposure. A preliminary analysis of the PEI indicated that only 3% of the participants scored 6, so they were combined with those who scored 5 for analysis. Subjects with PEI = 0 were used as references in analysis. Since only 2.9% of the participants received a zero score on PEI, the multi-year data were divided into three groups (to increase number of participants with PEI=0) with data in 2000–02 as Group 1, data in 2003–05 as Group 2 and data in 2006–08 as Group 3.
5. Statistical Analysis
5. 1. Computation and comparison of the smoking prevalence rates
To assess if exposure to substance use programs was associated with fewer number of smokers, we calculated and compared the prevalence rates of lifetime smoking and current smoking. The prevalence rates were computed as the ratio of the number of smokers over the number of the total participants included in the analysis. To account for the sampling error from the multi-level cluster random sampling scheme used in NSDUH, sampling weights were used in computing the rates. The computed prevalence rates for the exposed youth with PEI scores 1 to 5+ were then compared with youth with a PEI score of 0 using Odds Ratio (OR). The criterion of 95% confidence interval (CI) was used to assess the between group differences. A significantly lower prevalence rate among the exposed youth than among the non-exposed youth (OR < 1.0, p < 0.05) was used as evidence supporting the study hypothesis that exposure to prevention programs discouraging substance use was associated with reductions in cigarette smoking.
5. 2. Estimation and comparison of transitional probabilities
Transitional probabilities for smoking behavior progression were assessed using the following three-stage model (Figure 1) and the Probabilistic Discrete Event System (PDES)-based method (Lin & Chen, 2010).
Figure 1 depicts the transition of smoking behavior progression during a one-year period. The parameter σi (i = 1, 2, …6) represents the probability by which an adolescent either remains in the same progression stage (e.g., σ1 = the probability for an NS remaining as an NS) or progresses from one stage to another (σ2 = the probability for an NS to progress to CS) during a one-year period. To solve for these probabilities, the following equation set was used (Lin & Chen, 2010):
| (1) |
| (2) |
| (3) |
| (4) |
| (5) |
| (6) |
Where “a” = age; and “ ”, also known as “old ex-smokers”, who were current smokers a year ago and progressed to XS in the past year. XXS refers to ex-smokers remaining as ex-smokers in the year. Both and XXS were also estimated from the NSDUH data.
To computer the six transitional probabilities σi (i = 1, 2, …6), we first compute the state probabilities or the proportion of the defined five types of smokers (e.g., NS, CS, XS, , XXS) by age group using the NSDUH data. The computed state probabilities were thus used as data to solve the six equations as a set using the software Matlab (Mathworks, Natick, Massachusetts).
Among the six transitional probabilities, three were selected and compared between the exposed and the non-exposed participants. These probabilities were σ2 (transition from never smoker to current smoker), σ4 (transition from current smoker to ex-smoker) and σ6 (relapse from ex-smoker to current smoker). Odds ratio (OR) with 95% CI (Bland & Altman, 2000) was used to assess whether exposure prevention programs was associated with progressions in these steps of smoking behavior progression leading to the reductions in smoking. The prevalence rates and the state probabilities of the defined types of smokers were computed using SAS (SAS Institute, Inc, Cary, NC).
6. Results
6. 1. Sample characteristics
Data for a total of 142,913 participants 12–17 years of age were included in this analysis (Table 1). Demographically, slightly more than half (51.1%, 95% CI: 50.8%, 51.4%) of the sample were male, 65.2% (95% CI: 65.0%, 65.5%) non-Hispanic White, 12.9% (95% CI: 12.7%, 13.1%) non-Hispanic Black, 14.2% (95% CI: 14.0%, 14.4%) Hispanic, with the remaining (7.7%, 95% CI: 7.5%, 7.8%) classified as others. The number of participants and the gender and racial/ethnic compositions varied slightly across the three time periods. The number of youth with PEI = 0 (responded negatively to all six program exposure questions) was 1825 (4.1%, 95% CI: 3.9%, 4.2%) in 2000–02, 1807 (3.7%) in 2003–05 and 2332 (4.8%) in 2006–08; the number of youth with PEI = 5+ (responded positively to at least 5 questions) was 8385 (18.6%, 95% CI: 18.2%, 19.0%) in 2000–02, 9512 (19.3%, 95% CI: 19.0%, 19.7%) in 2003–05 and 8933 (18.4%, 95% CI: 18.1%, 18.8%) in 2006–08. The NSDUH sample represented approximately 24 – 27 million of the US adolescent population per year.
Table 1.
Demographic Characteristics (%) of the Study Sample, the National Survey on Drug Use and Health (2000–08), United States
| Variable | 2000–02 % (95%CI) (n=45087) |
2003–05 % (95% CI) (n=49271) |
2006–08 % (95% CI) (n=48555) |
Total % (95% CI) (N=142913) |
|---|---|---|---|---|
| Gender | ||||
| Male | 50.8 (50.3, 51.3) | 51.1 (50.6, 51.5) | 51.4 (51.0, 51.9) | 51.1 (50.8, 51.4) |
| Female | 49.2 (48.8, 49.7) | 48.9 (48.5, 49.4) | 48.6 (48.1, 49.0) | 48.9 (48.7, 49.2) |
| Age (in years) | ||||
| 12- | 15.2 (14.9, 15.5) | 14.5 (14.2, 14.9) | 13.9 (13.6, 14.2) | 14.5 (14.3, 14.7) |
| 13- | 16.5 (16.2, 16.9) | 16.4 (16.1, 16.8) | 15.8 (15.5, 16.1) | 16.2 (16.1, 16.4) |
| 14- | 17.6 (17.2, 17.9) | 17.1 (16.7, 17.4) | 16.5 (16.2, 16.9) | 17.0 (16.9, 17.2) |
| 15- | 17.2 (16.8, 17.5) | 17.7 (17.4, 18.0) | 17.9 (17.5, 18.2) | 17.6 (17.4, 17.8) |
| 16- | 17.2 (16.8, 17.5) | 17.4 (17.0, 17.7) | 18.4 (18.0, 18.7) | 17.7 (17.5, 17.9) |
| 17- | 16.4 (16.0, 16.7) | 16.9 (16.6, 17.3) | 17.6 (17.2, 17.9) | 17.0 (16.8, 17.2) |
| Race | ||||
| White | 69.1 (68.7, 69.6) | 65.3 (64.9, 65.7) | 61.5 (61.1, 62.0) | 65.2 (65.0, 65.5) |
| Black | 12.4 (12.1, 12.7) | 12.9 (12.6, 13.2) | 13.3 (13.0, 13.6) | 12.9 (12.7, 13.1) |
| Hispanic | 12.5 (12.2, 12.8) | 13.8 (13.5, 14.1) | 16.2 (15.9, 16.6) | 14.2 (14.0, 14.4) |
| Others | 6.0 ( 5.8, 6.2) | 7.9 ( 7.7, 8.2) | 8.9 ( 8.7, 9.2) | 7.7 ( 7.5, 7.8) |
| Program exposure index (PEI) | ||||
| PEI = 0 | 4.1( 3.9, 4.2) | 3.7( 3.5, 3.8) | 4.8( 4.6, 5.0) | 4.2( 4.1, 4.3) |
| PEI = 1 | 11.4(11.1, 11.7) | 11.6(11.3, 11.9) | 12.3(12.0, 12.6) | 11.8(11.6, 11.9) |
| PEI = 2 | 18.2(17.8, 18.5) | 18.1(17.8, 18.4) | 18.6(18.3, 19.0) | 18.3(18.1, 18.5) |
| PEI = 3 | 23.5(23.1, 23.8) | 22.6(22.2, 23.0) | 22.1(21.7, 22.4) | 22.7(22.5, 22.9) |
| PEI = 4 | 24.4(24.0, 24.8) | 24.8(24.4, 25.1) | 23.9(23.5, 24.2) | 24.3(24.1, 24.6) |
| PEI = 5+ | 18.6(18.2, 19.0) | 19.3(19.0, 19.7) | 18.4(18.1, 18.8) | 18.8(18.6, 19.0) |
6.2. Program exposure and the prevalence rates of cigarette smoking
Data in the upper panel of Table 2 indicate a negative association between PEI and the prevalence rates of lifetime smoking. As PEI increased from 0 to 5+, the smoking rates decreased progressively, and this pattern existed for participants in each of the three periods, implying the existence of a dose-response relation. Likewise, compared to youth with PEI = 0, the ORs for youth in all other groups with PEI ≥ 1 were less than 1.00 with 95% CI excluding 1.00, indicating significant reduction along with increases in PEI. Cochran-Armitage Trend Test indicated that this trend was statistically significant for all three periods (p < 0.001 for all). Consistent with the reductions in prevalence rates of smoking in all three periods, a greater PEI value was associated with a smaller OR in each of the periods, further supporting the dose-response relation. For example, compared to students with PEI = 0, the OR was 0.54 (95% CI: 0.48, 0.59) for youth with PEI ≥ 5 in 2000–02.
Table 2.
Associations (Odds Ratio) of Prevention Program Exposure Index (PEI) with the Prevalence Rates of Cigarette Smoking among US youth, the National Survey on Drug Use and Health (NSDUH), 2000–08, United States
| PEI | Year 2000–02 | Year 2003–05 | Year 2006–08 | |||
|---|---|---|---|---|---|---|
| % (95%CI) | OR (95%CI) | % (95%CI) | OR (95%CI) | % (95%CI) | OR (95%CI) | |
| Lifetime smoking | ||||||
| 0 | 44.1(41.8, 46.4) | 1.00 (n/a) | 40.8(38.5, 43.0) | 1.00 (n/a) | 35.0(33.0, 36.9) | 1.00 (n/a) |
| 1 | 40.1(38.8, 41.5) | 0.85(0.76, 0.95) | 35.8(34.5, 37.0) | 0.81(0.73, 0.90) | 30.6(29.5, 31.8) | 0.82(0.74, 0.91) |
| 2 | 37.1(36.1, 38.2) | 0.75(0.67, 0.83) | 33.5(32.6, 34.5) | 0.73(0.66, 0.81) | 26.6(25.7, 27.5) | 0.67(0.61, 0.74) |
| 3 | 34.8(33.9, 35.7) | 0.67(0.61, 0.75) | 29.7(28.8, 30.5) | 0.61(0.55, 0.68) | 23.4(22.6, 24.2) | 0.57(0.52, 0.62) |
| 4 | 31.6(30.7, 32.5) | 0.58(0.53, 0.65) | 27.1(26.3, 27.9) | 0.54(0.49, 0.60) | 22.6(21.8, 23.4) | 0.54(0.49, 0.60) |
| 5+ | 29.8(28.8, 30.7) | 0.54(0.48, 0.59) | 25.2(24.4, 26.1) | 0.49(0.44, 0.54) | 21.5(20.7, 22.4) | 0.51(0.46, 0.56) |
| Current smoking | ||||||
| 0 | 21.3(19.5, 23.2) | 1.00 (n/a) | 21.6(19.7, 23.5) | 1.00 (n/a) | 16.5(15.0, 18.0) | 1.00 (n/a) |
| 1 | 16.8(15.8, 17.8) | 0.74(0.65, 0.85) | 14.6(13.7, 15.5) | 0.62(0.54, 0.71) | 13.4(12.5, 14.2) | 0.78(0.68, 0.89) |
| 2 | 14.7(14.0, 15.5) | 0.64(0.56, 0.72) | 13.4(12.7, 14.1) | 0.56(0.49, 0.64) | 10.2( 9.6, 10.8) | 0.57(0.50, 0.65) |
| 3 | 13.2(12.5, 13.8) | 0.56(0.49, 0.63) | 11.6(11.0, 12.2) | 0.48(0.42, 0.54) | 9.1( 8.6, 9.7) | 0.51(0.45, 0.57) |
| 4 | 11.4(10.8, 12.0) | 0.47(0.42, 0.54) | 10.2( 9.7, 10.7) | 0.41(0.36, 0.47) | 9.0( 8.5, 9.5) | 0.50(0.44, 0.57) |
| 5+ | 11.0(10.3, 11.7) | 0.45(0.40, 0.52) | 10.0(9.4, 10.6) | 0.40(0.35, 0.46) | 8.5( 7.9, 9.0) | 0.47(0.41, 0.53) |
Note: PEI: Program exposure index; OR: Odds ratio, computed using data for participants with PEI = 0 as the reference group (OR = 1.00). Cochran-Armtage Trend test indicated a significant dose-response relation between PEI and the prevalence of lifetime smoking and current smoking at all three periods (p<0.0101) for all.
The associations between PEI and the prevalence rates of current smoking for the three periods are presented in the lower panel of Table 2. Data in the table indicate a negative association between the two variables. The prevalence rates were the highest among youth with PEI = 0 and the lowest with PEI = 5+. Compared to youth with PEI = 0, the ORs were less than 1.0 for all youths with PEI ≥1 and none of the 95% CIs containing 1.0, suggesting a significant negative association. Likewise, the negative trend between PEI and current smoking was statistically significant for participants in all three periods (p < 0.01 for all). A comparison of the ORs and 95% CI among youth with PEI >0 indicates no significant further reductions (overlap of the 95% CIs for two comparisons groups) in current smoking after the PEI increased to 3 for the 2000–02 and the 2003–05 periods respectively and after the PEI increased from 1 to 2 for the 2005–08 period.
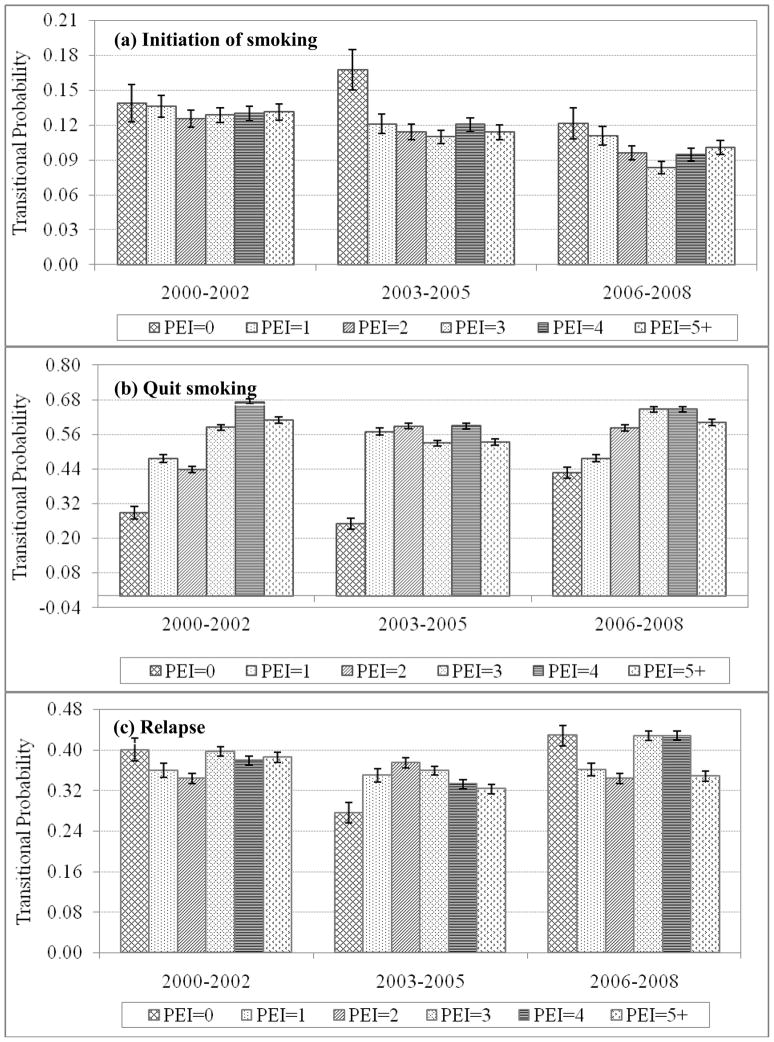
Figure 2 presents the results regarding the association between PEI and the three steps of smoking behavior transitions - smoking initiation (transition from NS to CS), quitting (transition from CS to XS) and relapsing (transition from XS back to CS) that were estimated using the PDES method and the same NSDUH data. The transitional probabilities with the 95% CIs in Figure 2(a) indicate that compared to youth with PEI = 0, youth with PEI ≥1 was associated with significant reductions in the rate of smoking initiation during the 2002–05 period and the 2006–08 period respectively. In addition, for youth in the 2006–08 period, further increases in PEI from 1 to 2 and from 2 to 3 were associated with additional reductions in the rate of smoking initiation.
Figure 2.
Association of the Program Exposure Index (PEI) with the Probabilities of Smoking Behavior Progression among US Youth, the Probabilistic Discrete Event System Method and the National Survey on Drug Use and Health (NSDUH) Data, 2000–08, United States
Note: Any two transitional probabilities with their 95% CI not overlapping with each other were statistically significantly different at p<0.05 level.
Data in Figure 2(b) indicate that compared to youth with PEI = 0, youth with PEI ≥ 1was associated with significant increases in quitting smoking in all three periods. For example, the quitting rate was 0.29 (95% CI: 0.27, 0.31) for youth in 2000–02 with a PEI = 0, the quitting was 0.48 (95% CI: 0.47, 0.49) for youth with PEI = 1. In addition, a dose-response relation was revealed between PEI and quitting rates among youth in 2000–02 (with the PEI values up to 4) and in 2006–08 (with the PEI values up to 3); and no such relation was observed for quitting during the 2003–05 period. The quitting rates during the 2006–08 tended to reach the 2000–02 level. However, the high quitting rates for participants in the group with program exposure also increased, suggesting the impact of other factors beyond the funding cut for school-based programs.
Data in Figure 2(c) indicate that the relapse rates were significantly lower for youth with PEI = 1 and 2 compared to youth with PEI = 0 in 2000–02 and in 2006–08. Youth with PEI=5+ in 2006–08 also showed a significant reduction in relapse rate compared to youth with PEI = 0. However, for youth assessed during 2003–05, a reverse relation between PEI and replace was observed. This is the period in the United States when tobacco control programs experienced a substantial cut in funding at the national and local levels.
7. Discussion
In this study, we examined the association between exposure to school and community-based behavioral prevention programs and cigarette smoking among adolescents in the United States using annual data from the National Survey on Drug Use and Health conducted during the 2000–08. Exposure to behavioral preventions programs was assessed using an index PEI that reflected the intensity of program exposure. In addition to the prevalence rates of lifetime and current smoking, rates of smoking initiation, quit and relapse were assessed using the PDES method and the same cross-sectional NSDUH data. The transitional probabilities add new data on progression step or steps that could explain reductions, if any, in cigarette smoking along with the exposure to prevention interventions. In addition, 2000–08 were included in this analysis so that potential impacts of the sudden funding cut since 2003 on smoking behavior could be assessed. Findings of this study support the conclusion that behavioral interventions are effective in postponing smoking initiation, stopping smoking and encouraging quitting as previously reported (Thomas & Perera, 2006; US Department of Health and Human Services, 2000)
7.1. Implications of exposure to behavioral interventions
Findings of this analysis indicate that exposure to behavioral interventions (as measured by PEI) was associated with significant reduction in lifetime smoking and current smoking during the 2000–02, 2003–05 and 2006–08 periods, respectively. Furthermore, a dose-response relation was revealed between PEI and the prevalence rates of life time smoking (all three periods) and current smoking (up to different PEI levels in different periods). In addition to confirming the results of earlier studies that behavioral intervention programs targeting substance use in general are effective in reducing tobacco use among youth at the state and the national levels (Torre, et al., 2005; US Department of Health and Human Services, 2000), findings from our study indicate the existence of a ceiling effect of the impact of program exposure on current smoking. Up to PEI = 3 or 4, further increases in PEI (intensity of program exposure) resulted in no significant reductions in current smoking, particularly during the 2003–05 period when funding for tobacco control was cut substantially.
The findings of the negative association between PEI and the prevalence rates of smoking in our study highlight the need to not only maintain but also strengthen the efforts of behavioral prevention intervention at all levels, including national and the state levels. According to the US census, every year approximately 4.3–4.5 million children enter adolescence with an estimate of 24–27 million youth 12–17 years of age (U.S. Census Bureau, 2010). Based on findings of this study, we estimated that approximately 23–26 million US youth (96% of the total) have been exposed to prevention programs, which eventually may prevent 2.3 – 2.6 million lifetime smokers and 2.0–2.3 million current smokers. Extending the coverage of the prevention programs will likely increase the number of children who refrain from using tobacco.
7.2. Unique aspects of the study
Findings unique for our study are the relation between prevention program exposure and smoking behavior transition that was estimated using the PDES method and cross-sectional data (Lin & Chen, 2010). The association between PEI and the three transitions (initiation, quitting and relapsing) in this study indicate that not only can the PDES be used to assess program exposure on smoking behavior change, it also can provide data strengthening the findings from the conventional method of comparisons of prevalence rates. For example, findings of our study indicate that reductions in smoking prevalence during the 2000–02 period were primarily due to increases in quitting (with an obvious program exposure dose effect); however, changes were rather limited in relapse and initiation. Reductions in smoking during the 2003–05 (funding cut period) were more complex. In addition to reductions in initiation and increases in quitting (no obvious program exposure dose effect), the smoking relapse rates for ex-smokers during this period was increased. The lack of program dose effect and the increased relapse rates could be a reflection of the funding cut for tobacco control as has been observed in several states in the U.S. (Dietz et al., 2010; Gingiss & Boerm, 2009; Niederdeppe, et al., 2008; Pizacani, et al., 2009; Sly, et al., 2005). Such important information has never been extracted and reported in previous research with cross-sectional data, including data from the NSDUH (Jordan, Karg, Batts, Epstein, & Wiesen, 2008; Winstanley, et al., 2008). If this result can be directly verified using longitudinal data, it is likely that the PDES method will be more sensitive than the conventional rate comparison (Table 2) for program effect evaluation at the macro levels as the inventors of this method anticipated (Lin & Chen, 2010).
7.3. Study limitations
There are some limitations to this study. First, although data from our analysis indicated that exposure to behavioral prevention programs was associated with significant reductions in cigarette smoking, results from our analysis cannot replace a randomized controlled design in which whether a subject receives the intervention is determined totally at random. Second, since the data used for this analysis are cross-sectional in nature, and an index was used as a proxy of program exposure, caution is advised when drawing any causal conclusion. Third, findings of this study suggest the utility of the PDES method to study smoking behavior using cross-sectional data, but it cannot be used to replace longitudinal data for program evaluation. Third, data used to measure smoking behaviors were self-reported, therefore, response bias cannot be ruled out without verification of biological markers (including CO in breath air and cotinine in body fluids). Lastly, the increases in the quitting rate during the 2006–08 period after the 2003 funding cut need further research. Although the findings of increased quitting among those who reported no program exposure during this period suggest that some other compensation mechanisms might have come into play after 2003, such effect could not be assessed. Despite these limitations, this study added to existing data on the effect of community and school-based behavioral prevention programs.
8. Lessons learned
Findings of this study suggest that reduction in adolescent smoking in the United States may be associated with exposure to substance use prevention programs. Health policy and decision makers should consider these factors in planning and revising tobacco control strategies. Given the financial difficulties the nation is facing, policy makers should consider the potential powerful impact offered by relatively low-cost nationwide substance use prevention campaigns.
HIGHLIGHTS.
Probabilistic Discrete Event Systems is a powerful tool to estimate transitional probability with cross-sectional data.
Exposure to substance abuse prevention programs was associated with reduced lifetime smoking and current smoking in youth with a dose-response relation.
Smoking in adolescents tends to change rapidly. Thus, different transitional stages (smoking initiation, quitting and relapsing) should be used for assessing smoking behavior (e.g., to increased quitting in 2000–02).
During a period of decreased federal funding for substance prevention programs, the smoking relapse rate for ex-smokers increased.
Sustained funding for nationwide substance prevention campaigns plays an important role in facilitating the tobacco control movement.
Biographies
Xinguang Chen, MD, PhD, is a professor from Pediatric Prevention Research Center at Wayne State University. Dr. Chen has been doing smoking-related research for 30 years and has publication on many renowned journals. His recent interests are methodology designing, dynamic model for behavior research and international health in China.
Feng Lin, PhD, is a professor from Wayne State University Department of Electrical and Computer Engineering. He contributed to PDES modeling.
Yuanjing Ren, MS., is a research assistant. With formal training in Health Management and Policy, she joined this project in 2010. She participated in statistical analysis and manuscript development.
Karen MacDonell, PhD., is an assistant professor with formal training in Developmental Psychology and Applied Statistics. She contributed to manuscript development.
Yifan Jiang, M.S., in Mathematical Statistics. Her major contributions include data processing and PDES modeling analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashery RS, Robertson EB, Kumpfer KL. Drug Abuse Prevention through Family Interventions. US Department of Health and Human Services, National Institute on Drug Abuse; Rockville, MD: 1998. [Google Scholar]
- Bala M, Strzeszynski L, Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev. 2008;(1):CD004704. doi: 10.1002/14651858.CD004704.pub2. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Foshee VA, Ennett ST, Pemberton M, Hicks KA, King TS, et al. The influence of a family program on adolescent tobacco and alcohol use. Am J Public Health. 2001;91(4):604–610. doi: 10.2105/ajph.91.4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland JM, Altman DG. Statistics notes. The odds ratio. BMJ. 2000;320(7247):1468. doi: 10.1136/bmj.320.7247.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Dusenbury L, Botvin EM, Diaz T. Long-term follow-up results of a randomized drug abuse prevention trial in a white middle-class population. JAMA. 1995;273(14):1106–1112. [PubMed] [Google Scholar]
- Cavana R, Tobias M. Integrative System Dynamics: Analysis of Policy Options for Tobacco Control in New Zealand. Systems Research and Behavioral Science. 2008;25(5):675–694. [Google Scholar]
- Centers for Disease Control and Prevention. Surveillance Summaries: Youth Risk Behavior Surveillance - United States, 2009. MMWR; 2010. [Google Scholar]
- Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- Chen X, Li G, et al. Secular trends in adolescent never smoking from 1990 to 1999 in California: an age-period-cohort analysis. Am J Public Health. 2003;93(12):2099–104. doi: 10.2105/ajph.93.12.2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Li Y, et al. Hazard of smoking initiation by age among adolescents in Wuhan, China. Prev Med. 2001;32(5):437–45. doi: 10.1006/pmed.2001.0826. [DOI] [PubMed] [Google Scholar]
- Chen X, Stanton B, et al. APC-Modeling of smoking prevalence among US adolescents and young adults. American Journal of Health Behavior. 2011 doi: 10.5993/ajhb.35.4.4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Unger JB. Hazards of smoking initiation among Asian American and non-Asian adolescents in California: a survival model analysis. Prev Med. 1999;28(6):589–99. doi: 10.1006/pmed.1999.0487. [DOI] [PubMed] [Google Scholar]
- Dent CW, Sussman S, Stacy AW, Craig S, Burton D, Flay BR. Two-year behavior outcomes of project towards no tobacco use. J Consult Clin Psychol. 1995;63(4):676–677. doi: 10.1037//0022-006x.63.4.676. [DOI] [PubMed] [Google Scholar]
- Dietz NA, Westphal L, Arheart KL, Lee DJ, Huang Y, Sly DF, et al. Changes in youth cigarette use following the dismantling of an antitobacco media campaign in Florida. Prev Chronic Dis. 2010;7(3):A65. [PMC free article] [PubMed] [Google Scholar]
- Dobbins M, DeCorby K, Manske S, Goldblatt E. Effective practices for school-based tobacco use prevention. Prev Med. 2008;46(4):289–297. doi: 10.1016/j.ypmed.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, Bell RM, McGuigan K. Preventing adolescent drug use: long-term results of a junior high program. Am J Public Health. 1993;83(6):856–861. doi: 10.2105/ajph.83.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett SA, Warren CW, Sharp D, Kann L, Husten CG, Crossett LS. Initiation of cigarette smoking and subsequent smoking behavior among U.S. high school students. Prev Med. 1999;29(5):327–333. doi: 10.1006/pmed.1999.0560. [DOI] [PubMed] [Google Scholar]
- Gingiss PM, Boerm M. Influence of funding cuts on Texas school tobacco programs. J Sch Health. 2009;79(8):361–368. doi: 10.1111/j.1746-1561.2009.00422.x. quiz 388–390. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Abbacchi AM, Przybeck TR, Gfroerer JC. Discrepancies in estimates of prevalence and correlates of substance use and disorders between two national surveys. Addiction. 2007;102(4):623–629. doi: 10.1111/j.1360-0443.2007.01745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen WB, Johnson CA, Flay BR, Graham JW, Sobel J. Affective and social influences approaches to the prevention of multiple substance abuse among seventh grade students: results from project SMART. Prev Med. 1988;17(2):135–154. doi: 10.1016/0091-7435(88)90059-x. [DOI] [PubMed] [Google Scholar]
- Ibrahim JK, Glantz SA. The rise and fall of tobacco control media campaigns, 1967 2006. Am J Public Health. 2007;97(8):1383–1396. doi: 10.2105/AJPH.2006.097006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2009. National Institute on Drug Abuse; Bethesda, MD: 2010. [Google Scholar]
- Jordan BK, Karg RS, Batts KR, Epstein JF, Wiesen C. A clinical validation of the National Survey on Drug Use and Health assessment of substance use disorders. Addict Behav. 2008;33(6):782–798. doi: 10.1016/j.addbeh.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Kiros GE, Schaffran C, Hu MC. Racial/ethnic differences in cigarette smoking initiation and progression to daily smoking: a multilevel analysis. Am J Public Health. 2004;94(1):128–135. doi: 10.2105/ajph.94.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Hyland A, Higbee C, Remer L, Compton C. The role of public policies in reducing smoking prevalence in California: results from the California tobacco policy simulation model. Health Policy. 2007;82(2):167–185. doi: 10.1016/j.healthpol.2006.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin F, Chen X. Estimation of Transitional Probabilities of Discrete Event Systems from Cross-Sectional Survey and its Application in Tobacco Control. Inf Sci (Ny) 2010;180(3):432–440. doi: 10.1016/j.ins.2009.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Preventing drug use among children and adolescents: A research-based guide for parents, educators and community leaders. US Department of Health and Human Services; Bethesda, Maryland: 2003a. [Google Scholar]
- National Institute on Drug Abuse. Drug use among racial/ethnic minorities (revised) National Institute on Drug Abuse; Bethesda, MD: 2003b. [Google Scholar]
- Niederdeppe J, Farrelly MC, Hersey JC, Davis KC. Consequences of dramatic reductions in state tobacco control funds: Florida, 1998–2000. Tob Control. 2008;17(3):205–210. doi: 10.1136/tc.2007.024331. [DOI] [PubMed] [Google Scholar]
- Pentz MA, MacKinnon DP, Dwyer JH, Wang EY, Hansen WB, Flay BR, et al. Longitudinal effects of the midwestern prevention project on regular and experimental smoking in adolescents. Prev Med. 1989;18(2):304–321. doi: 10.1016/0091-7435(89)90077-7. [DOI] [PubMed] [Google Scholar]
- Perry CL, Kelder SH, Murray DM, Klepp KI. Communitywide smoking prevention: long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. Am J Public Health. 1992;82(9):1210–1216. doi: 10.2105/ajph.82.9.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizacani BA, Dent CW, Maher JE, Rohde K, Stark MJ, Biglan A, et al. Smoking patterns in Oregon youth: effects of funding and defunding of a comprehensive state tobacco control program. J Adolesc Health. 2009;44(3):229–236. doi: 10.1016/j.jadohealth.2008.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts-Gray C, Gingiss PM, Boerm M. Evaluating school capacity to implement new programs. Eval Program Plann. 2007;30(3):247–257. doi: 10.1016/j.evalprogplan.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Rodu B, Cole P. Smoking prevalence: a comparison of two American surveys. Public Health. 2009;123(9):598–601. doi: 10.1016/j.puhe.2009.07.014. [DOI] [PubMed] [Google Scholar]
- Secker-Walker RH, Worden JK, Holland RR, Flynn BS, Detsky AS. A mass media programme to prevent smoking among adolescents: costs and cost effectiveness. Tob Control. 1997;6(3):207–212. doi: 10.1136/tc.6.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman EJ, Primack BA. What works to prevent adolescent smoking? A systematic review of the National Cancer Institute’s Research-Tested Intervention Programs. J Sch Health. 2009;79(9):391–399. doi: 10.1111/j.1746-1561.2009.00426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shu S, Lin F, et al. State Estimation and Detectability of Probabilistic Discrete Event Systems. Automatica (Oxf) 2008;44(12):3054–3060. doi: 10.1016/j.automatica.2008.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sly DF, Arheart K, Dietz N, Trapido EJ, Nelson D, Rodriguez R, et al. The outcome consequences of defunding the Minnesota youth tobacco-use prevention program. Prev Med. 2005;41(2):503–510. doi: 10.1016/j.ypmed.2004.11.027. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2002 National Survey on Drug Use and Health: National Findings, Appendix C: NSDUH Changes and Their Impact on Trend Measurement. US DHHS, Office of Applied Studies; Rockville, MD: 2003. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2006. Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06–419.4. [Google Scholar]
- Sussman S, Dent CW, Stacy AW, Sun P, Craig S, Simon TR, et al. Project towards no tobacco use: 1-year behavior outcomes. Am J Public Health. 1993;83(9):1245–1250. doi: 10.2105/ajph.83.9.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas R, Perera R. School-based programmes for preventing smoking. Cochrane Database Syst Rev. 2006;3:CD001293. doi: 10.1002/14651858.CD001293.pub2. [DOI] [PubMed] [Google Scholar]
- Tobias MI, Cavana RY, Bloomfield A. Application of a system dynamics model to inform investment in smoking cessation services in New Zealand. Am J Public Health. 2010;100(7):1274–1281. doi: 10.2105/AJPH.2009.171165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torre GL, Chiaradia G, Ricciardi G. School-based smoking prevention in children and adolescents: review of the scientific literature. J Public Health 2005 [Google Scholar]
- U.S. Census Bureau, P. D. Table 1. Annual Estimates of the Resident Population by Sex and Five-Year Age Groups for the United States: April 1, 2000 to July 1, 2009 (NC-EST2009–01) 2010. Retrieved October 2010. [Google Scholar]
- United Nations Office on Drugs and Crime. 2004 Schools: school-based education for drug abuse prevention. United Nations; New York: 2004. [Google Scholar]
- US Department of Education. Safe, Disciplined, and Drug-Free Schools. US Department of Education, Office of Special Education Research and Improvement, Office of Reform Assistance and Dissemination; Washington, DC: 2001. [Google Scholar]
- US Department of Health and Human Services. Preventing Tobacco Use among Young People: A Report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 1994. [Google Scholar]
- US Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2000. [Google Scholar]
- Walter HJ. Primary prevention of chronic disease among children: the school-based “Know Your Body” intervention trials. Health Educ Q. 1989;16(2):201–214. doi: 10.1177/109019818901600205. [DOI] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend. 2008;92(1–3):173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zollinger TW, Saywell RM, Jr, Muegge CM, Wooldridge JS, Cummings SF, Caine VA. Impact of the life skills training curriculum on middle school students tobacco use in Marion County, Indiana, 1997–2000. J Sch Health. 2003;73(9):338–346. doi: 10.1111/j.1746-1561.2003.tb04190.x. [DOI] [PubMed] [Google Scholar]