Abstract
Objectives. To measure Croatian community pharmacists’ progress in competency development using the General Level Framework (GLF) as an educational tool in a longitudinal study.
Methods. Patient care competencies of 100 community pharmacists were evaluated twice, in 2009 and in 2010 in a prospective cohort study. During this 12-month period, tailored educational programs based on the GLF were organized and conducted, new services and standard operating procedures were implemented, and documentation of contributions to patient care in the pharmacist’s portfolio became mandatory.
Results. Pharmacists’ development of all GLF patient care competencies was significant with the greatest improvements seen in the following competencies: patient consultation, monitoring drug therapy, medicine information and patient education, and evaluation of outcomes.
Conclusions. This study, which retested the effectiveness of an evidence-based competency framework, confirmed that GLF is a valid educational tool for pharmacist development.
Keywords: competency development, pharmacist, general level framework, continuing education, continuing professional development, community pharmacy
INTRODUCTION
Competency in pharmacy is the ability of the pharmacist to make deliberate choices from a repertoire of behaviors for handling situations and tasks in the specific context of professional pharmacy practice by using and integrating knowledge and personal values in accordance with professional role and responsibilities.1 Knowledge can be assessed using various tools eg, examinations and questionnaires.2 However, more sophisticated methods of testing are needed to assess skills, judgment, and attitudes in the context of clinical performance, eg, direct observation and objective structured clinical examinations (OSCEs). The assessment methods may include observation, review of documentation, surveys of those using pharmacy services, or role-playing using standardized or real patients.3,4 It is also possible to assess competency by comparing pharmacists’ behavior to documented, effective actions of other pharmacists in real pharmaceutical care situations.
By assessing the differences between the current and desired levels of pharmacist competencies, it is possible to develop an individual education plan aimed at achieving the desired level of competency.5 Knowledge, skills, attitudes, and personal pharmacist values thereby receive real significance through experience in practice. Educational programs therefore should focus on integrating knowledge and practice.6 In this way, education should be tailored to suit individual needs, taking into account the pharmacist’s desire for advancement and professional development.7 However, educational needs pertaining to the development of competency can be assessed at the level of the organization, and with regard to national or international plans or movements within the profession.8 In 2007, the Global Education Taskforce, established by the International Pharmaceutical Federation (FIP), United Nations Educational, Scientific and Cultural Organization (UNESCO), and the World Health Organization (WHO), called for increased testing of competencies, additional educational programs and tools for their improvement, as well as international cooperation.9 In attempting to sum up the common educational needs related to the development of competencies, various models for competency testing have been examined at the global level.10
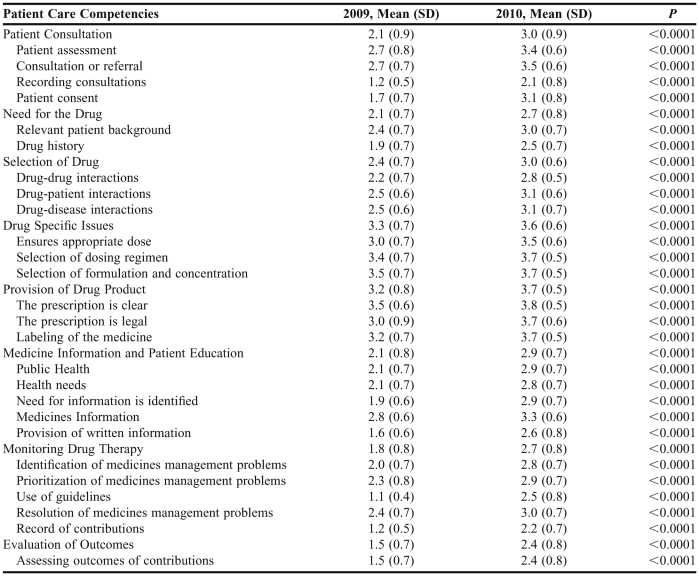
In 2005, the Competency Development and Evaluation Group developed the General Level Framework (GLF).11 The GLF is in use for competency testing of pharmacists in hospital and community settings in Great Britain,12 Australia,13 Croatia,14 Singapore, and Serbia.15 The GLF contains a detailed description of knowledge, actions, and skills that should be applied by a pharmacist in delivering competent pharmaceutical patient care. There are 4 competency clusters: delivery of patient care, problem-solving competencies, personal competencies, and management and organization competencies. The delivery of patient care cluster is comprised of 8 different competencies (Table 1), and was selected by researchers to evaluate and develop the community pharmacists’ professional competence level in Croatia. Each of these competencies has several statements that define the competency, known as behavioral statements (Table 1). All 26 behavioral statements can be evaluated through a monitoring method, ie, observation of performance in real situations involving the delivery of pharmaceutical care.
Table 1.
Comparison of Competencies and Behavioral Statement in 2009 and 2010
Croatia has a population of 4.5 million. Pharmacies are a part of the primary health care system, and there are 2,773 registered pharmacists working in community pharmacies. Pharmacist licenses are renewed every 6 years by the Croatian Chamber of Pharmacists based on points collected through CPD programs or mentoring. It is not an obligation for pharmacists in Croatia to keep a learning portfolio, and it is not yet part of the licensing process. In Croatia, like in other Eastern European countries, the primary role of community pharmacists remains the traditional role of dispensing, supplying, and compounding medicines, with few structured clinical engagements and little advanced collaborative practice.16
The objective of this study was to measure Croatian community pharmacists’ progress in competency development using the GLF in a longitudinal study. Croatian pharmacists undergo traditional continuing education, which usually involves only passive learning. Implementation of the GLF was Croatian pharmacists’ first exposure to a continuing education system that first identified their individual training and development needs and then provided the education and training required to attain competency in those areas.
METHODS
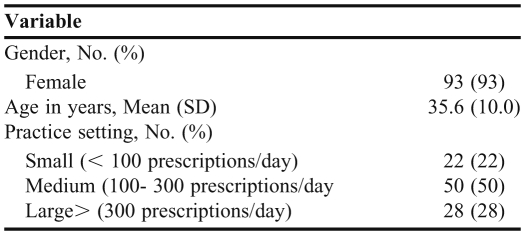
The study involved 100 pharmacists (Table 2) employed in Croatia's largest pharmacy chain who were included in the evaluation of pharmaceutical care competencies that was conducted in 2009. The pharmacies ranged from small to large and were situated in small and large towns, in different regions throughout Croatia. At that time, the pharmacy chain consisted of 38 pharmacies. Prior to their participation in this research, none of the participants were familiar with the precise content of the GLF program. They were informed that the document was already in use in Great Britain and Australia, that it was translated into Croatian and validated by Croatian experts and adapted for the purposes of the study. Participants signed an informed consent form to participate in the study to evaluate their competencies and educate them about their professional development needs. Ethics approval was obtained from Farmacia’s Health Department Ethics Committee.
Table 2.
Demographics of Participants (N = 100)
The initial assessment was conducted from March to June 2009, through structured, overt observation of the participants in community pharmacies during regular working hours in a single visit, using the behavioral statement checklist and rating scale. The initial data on pharmacist performance in community pharmacies in Croatia were provided in an earlier study (Table 1) as a starting point in which the competencies that Croatian pharmacists needed to develop to improve their professional contributions in community settings were identified.14 Improvement was most needed in the following competencies: monitoring drug therapy, patient consultation, and evaluation of outcomes. Developing forms, templates, or computer programs to record those actions in pharmacist’s practice was essential. Large variance in assessments ratings among pharmacists was found in: prioritizing medicine management problems, ensuring that the prescription is legal, and identifying drug-drug interactions. Pharmacists’ best performance was recorded in the following competencies: drug specific issues and provision of drug product.
After the initial evaluation of competencies, the results were presented to participants in the Farmacia Education Centre. All participants were given a detailed explanation of their individual assessment, as well as general statistical data from the study. The competencies in which participants achieved the highest and lowest levels, both individually and collectively, were identified, as were the competencies in which the greatest differences in the level of performance were found.14,17
For participants to use the feedback provided to them to develop professional competencies, it was necessary for them first to better understand the concept of competency in pharmacy practice. Lectures were organized to acquaint the participants with the GLF program in detail. Workshops were also held in which participants discussed the significance and importance of individual competencies and tried individually to assess their own competencies. Those results are not included in the present study.
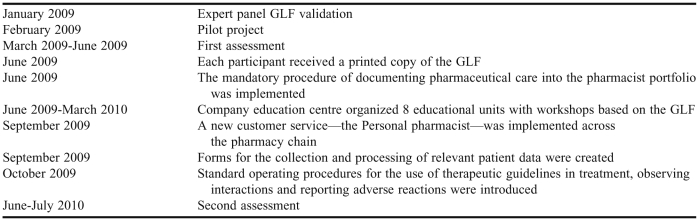
In June 2009, a printed copy of the GLF was sent to each participant outlining the competencies in which they required further training and guidelines on how they could achieve a higher level of competency. From June 2009 to March 2010, the pharmacy chain’s education center organized 8 workshops on the following topics: documentation methods, observation of interactions, observations of side effects and adverse reactions, communication skills, literature searches, provision of written information, use of guidelines, and taking medication histories. Documenting pharmaceutical care in the pharmacist’s portfolio became mandatory procedure within the pharmacy chain in June 2009, with the objective of collecting evidence of pharmacist contributions to improved patient outcomes. During practice hours, pharmacists documented the following: observed side effects, adverse reactions of medicines, interactions between medicines, errors in dosage, cases of polypharmacy and other drug related problems, and pharmacists’ actions. To improve patient adherence and therapy outcomes, a new customer service, the Personal Pharmacist, was implemented in September 2009 throughout the pharmacy chain. The service was aimed at providing personal guidance and support to patients with drug-related problems. Obtaining a medication history and conducting a structured interview with the patient served as the starting point for the pharmacist to develop an individualized pharmaceutical care plan for the patient.18 Forms for the collection and processing of relevant patient data were created in September 2009 and were designed to be easy to complete and ensure comparability of data. A protocol was created that included a template for the review of medications, correspondence with physicians, and instructions for a structured interview with patients. Standard operating procedures were introduced in October 2009 for the use of therapeutic guidelines in treatment, observing interactions, and reporting adverse reactions.
Pharmacists applied the knowledge obtained in the workshops by conducting short-term projects, and monitoring their development through tests and survey tools. By following the instructions of the GFL, they self-assessed the extent to which they were meeting the expected standards and whether further practice in specific skills or behaviors was needed to raise the level of competency.
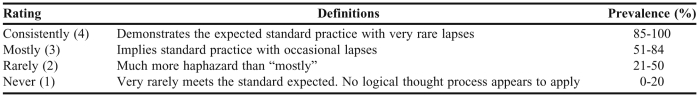
After the 12-month period in which participants used the GLF as an educational tool, the main researcher reevaluated the same 100 pharmacists, now employed in 55 Farmacia community pharmacies (June 2010 to July 2010). All pharmacists were assessed at work in their community pharmacy by a single assessor, using the overt observation method. Each assessment took an average of 4 hours to complete. In addition to monitoring the participant’s interaction with patients, a review of the documented expert work from each portfolio was also conducted, and the number of pharmacist’s contributions (as defined by the GLF program) was recorded. The performance of the pharmacists’ was evaluated by rating their performance on the 26 behavioral statements in the Framework on a 4-point scale, as in the initial evaluation(Table 3).
Table 3.
Scale Used With the General Level Framework to Assess Pharmacists' Competencies
Mean and standard deviation were used as statistical indicators. Parametric tests were used to determine significant differences. Statistical processing and analysis of data were carried out using STATISTICA, version 6.1 (StatSoft Inc, Tulsa, OK). Statistical testing was conducted at a significance level of 95% (α = 0.05).
RESULTS
The study included 100 pharmacists, 93% of whom were women, which corresponds to the Croatian average.19 Community pharmacies were divided by size into small (up to 100 prescriptions per day), medium (100-300 prescriptions per day), and large (300+ prescriptions per day). Half of the participants practiced in medium-sized community pharmacies (Table 2). During the study period, none of the participants left the study, however, 2 pharmacists moved from a medium to a small pharmacy, and 1 moved from a medium to a large pharmacy. All other pharmacists either remained in the same pharmacy or moved to a pharmacy of the same size.
The values of the behavioral statements from 2009 and 2010 show the competencies in which the participants performed the best and poorest during the first and second testing sessions (Table 1). A comparison was made of participants’ performance on individual behavioral statements in 2009 and 2010, showing their progress in individual competencies. There was a significant difference between the values of behavioral statements in 2009 and 2010 for all competencies. The majority of data exhibited normal distribution profiles.
Pharmacists demonstrated the best performance development in the following competencies: patient consultation, monitoring drug therapy, medicine information and patient education, and evaluation of outcomes. While participants’ poorest performance in 2010 was in the patient care behavioral statements on recording consultations and contributions and assessing outcomes of contributions (Table 1), their performance levels were significantly higher than in 2009.
The best performance levels in 2010 were seen in the following competencies: drug specific issues and provision of drug product, according to the behavioral statements: selection of formulation and concentration, the prescription is clear, selection of dosing regimen, labeling of the medicine, and ensures appropriate dose. These results were similar to those from 2009; however, the levels increased significantly, ranging from 3.7 to 3.8, ie, near the maximum values (Table 1).
A significant difference was found between the mean behavioral statement scores. The greatest progress was achieved in the behavioral statements: patient consent and use of guidelines , and the least in the previously mentioned behavioral statements that had the highest values in 2009.
There was still a significant difference between the values of the behavioral statements in 2010 (p <0.05). However, a comparison of the differences between behavioral statements in 2009 and 2010 showed that the difference between behavioral statements in 2010 (F = 54,56) was nearly half that in 2009 (F = 114,65).
The calculated values of differences in the level of pharmacist’s performance in 2010 and 2009 for the following behavioral statements were significantly dependent on the age of the participant, with values of differences increasing with age: health needs (p = 0.011), identification of medicines management problems (p = 0.029), and use of guidelines (p = 0.033).
A significant difference was found between pharmacy locations with regard to score on the following behavioral statements: recording consultations (p = 0.013), drug-drug interactions (p = 0.023), provision of written information (p = 0.022) and assessing outcomes of contributions (p = 0.012). The greatest improvement in scores on behavior statements were found in rural environments. The values of the remaining behavioral statements were relatively uniform in all observed pharmacy locations.
A significant difference in the scores on the following behavioral statements was also found in: health needs (p = 0.024), medicines information (p = 0.011) and provision of written information (p = 0.022) with regard to pharmacy size. These differences in pharmacist’s performance decreased with pharmacy size. Pharmacists working in small pharmacies showed the biggest improvement in performance level.
DISCUSSION
Pharmacists demonstrated the best performance development in the following competencies: patient consultation, monitoring drug therapy, evaluation of outcomes, medicine information, and patient education (Table 1). All except the latter were identified in the initial evaluation as the main competencies needing improvement, and the education program evaluated in this study was designed based on those results.
The most substantial progress was achieved in the mean assessment rating for use of guidelines and patient consent, which were the 2 behavioral statements with the poorest rating in 2009 (Table 1). During the educational intervention, special attention was paid to these 2 topics; thus, progress was expected. The mean assessment rating for the behavioral statement regarding patient consent significantly increased. The need for development of an ethical covenant between the pharmacist and the patient has been proposed by several authors.20,21
Because consent is principal in the patient-pharmacist relationship, and informed consent papers have been rare in pharmacy practice research to date, attempts have been made to resolve the ethical dilemmas pharmacists need to cope with while attaining informed consent.22 Roche and Kelliher proposed a framework by which ethical guidelines might facilitate the resolution of the dilemma faced by the pharmacist, who is expected to simultaneously maintain the legal and duty of care responsibilities in the patient consent process. A new approach to communicating with patients, supported through the GLF, requires asking the patient a series of questions. The increase in ratings suggest that the pharmacists understood the importance of the patient consent process and took a more responsible approach in obtaining such consent.
Another behavioral statement that rated poorly in 2009, use of guidelines, improved by more than an entire grade (+1.4) in 2010 (Table 1). This was a positive result that use of guidelines raises pharmaceutical care to a higher level and makes pharmacists’ contributions more evidence based.
The rating of the behavioral statements on relevant patient background and drug history also improved significantly (Table 1). The behavioral statements on recording consultations and recording contribution received the lowest assessment ratings in 2010, although significant performance development was achieved (Table 1). The mean scores show that the participants conduct these activities in their daily work in more than 50% of situations.
Despite implementation of official standard operating procedures developed by the company, raising scores in these competencies requires greater personal engagement on the part of pharmacists, and spending additional time with patients is not always possible. The Croatian healthcare system does not support assessment of pharmacist performance through the use of nationwide tools such as the medication action plan, which facilitates the documentation of medication-related problems in other countries.23 Documentation of pharmacist contributions is a useful tool in enhancing communication with other healthcare providers, justifying the workload, and identifying opportunities for focused drug use review.24 Although several studies reported that most hospital pharmacists document their contributions, there is virtually no evidence as to how this information is collected or used.25,26 As greater emphasis is placed on demonstrating individual competency, pharmacist documentation will continue to serve a key role. Although this may appear to be a relatively easy task, experience is required to know what information to include and how to communicate it in a manner appropriate for the patient medication record.27
The present study demonstrated significant improvements in all competencies evaluated. This finding supports other studies that used the GLF to assess competencies,12,23 though the results presented here show even greater improvement in pharmacist competencies. Coombes and colleagues demonstrated improvements in 57% of the competencies evaluated (35 of 61), and none of the remaining competencies demonstrated a decrease in performance between evaluations.23 The South of England competency study was designed as a controlled study, and demonstrated that junior pharmacist competencies developed using the Framework improved in 24 of 25 areas assessed at 6 months and that this improvement was sustained at 12 months.12 In both the above studies, the sample consisted of hospital/clinical pharmacists. Therefore, the greater improvement in competencies found in this study may have been due to the use of the GLF to evaluate community pharmacists. There are barriers preventing community pharmacists from practicing as clinical pharmacists, such as a lack of reimbursement for clinical services, functions associated with medication order fulfillment, provider status,27 and lack of access to clinical information about the patient. All of these barriers could influence the lower initial scores, and subsequent use of the GLF as an educational tool may have resulted in greater improvement.
Mills and colleagues compared the use of the GLF in clinical practice pharmacists and community pharmacists and found that the desired performance levels for clinical pharmacists in the delivery of patient care competencies were significantly higher than for community pharmacists, although there was no difference in the probability of either group achieving their desired performance level. Their performance level was based on self-assessment and demonstrated the applicability of the GLF to the different sectors of practice.28 According to this study, the average competency performance level of UK community pharmacists was 3 (mostly) and the desired level was set at 4 (consistently) for all 8 patient care competencies. The Croatian pharmacists’ assessment from 2009, due to the mean of behavioral statements (according to rounded up levels), shows an average level of 3 in the areas of drug-specific issues and provision of drug product competencies. All other competencies in Croatia were rated 2 (rarely). Following the tailored educational intervention in Croatia, in 2010 all competencies were rated 1 level higher, with pharmacists even achieving the highest level 4 (consistently) for the competency areas of drug specific issues and provision of drug product.
Another possible explanation for the greater improvement in pharmacist competencies in this study is cultural and educational differences. Unlike the United Kingdom and Australia, Croatia is in the initial stages of developing clinical pharmacy and pharmaceutical care. Even so, the first patient-centered subjects (pharmacotherapy, communication skills, pharmacy practice) were introduced at the Croatian School of Pharmacy between 2006 and 2009. Therefore, most practicing pharmacists did not attend these courses as part of their undergraduate education.
An interesting result from our study is certainly the variability found among pharmacists’ ratings on the behavioral statements in 2010. These differences were half of those found among pharmacists’ competency ratings in 2009, indicating that the behavior forms were more uniform in individual situations and that the differences between individual pharmacies decreased at the level of individual competencies. This is certainly an excellent indicator that the GLF, as a tool, has an educational role in setting standards and contributing to the uniform provision of services in pharmaceutical care.
One of the results deserving special mention is the difference in the level of performance in 2009 and 2010 for behavioral statements regarding the following: health needs, identification of medicines management problems, and use of guidelines. The analysis indicated that there was a significant difference in ratings based on the age of participants. This proves that experience is one of the key preconditions for improving competency, and that the educational interventions raised pharmacists’ awareness and encouraged them to apply their professional knowledge and skills obtained through experience in practice, particularly in complex situations, such as in recognizing and identifying drug-related problems.
The significant difference between pharmacy locations with regard to the scores of certain behavioral statements requiring additional time and effort, such as recording consultations, drug-drug interactions, provision of written information, and assessing outcomes of contributions, indicates that these differences may be influenced by the work environment, atmosphere, and cooperation with physicians in the rural environment. This was expected, as a smaller number of patients allows for more time for patient communication, which resulted in greater and faster progress.
Working with the same sample of mutually connected participants was considered an organizational strength of the study. Educational interventions were conducted at the same time for all participants (Table 4), so they had the opportunity to exchange experiences and compare their work. Pharmacists were evaluated by the same assessor during 2 visits, thereby excluding inter-rater variability. The researcher also assessed pharmacist portfolios to ensure as objective a rating of participant contributions to patient care as possible.
Table 4.
Time Line for Study Using the General Level Framework to Educate and Improve Competencies in Croatian Pharmacists
Because of the lack of pharmacists in Croatia, pharmacy teams often work at minimum capacity. In some pharmacies there is only 1 pharmacist present, working with numerous patients per day. Therefore, their consultations with some patients are often limited. For that reason, some participants did not succeed in achieving the set standard, particularly in competencies in more time-consuming processes such as recording consultations and contributions, assessing outcomes of contributions, etc. This difference in work environments could be considered a limitation.
The study limitations are also related to the fact that the first exposure of Croatian pharmacists to the GLF was, for many, also their first exposure to clinically oriented education as previously explained. We found that the learning curve for pharmacists in this study was quite steep and they advanced far above their initial level of performance.
Using virtual cases in the assessment process could also be considered a limitation. Virtual performance could include lack of empathy and feedback from the real patient. Furthermore, questions can be tailored to the level of skill to be assessed, and the patient variable in examination is uniform across participants.29 As many studies have reported, this kind of investigation, including overt observation, could have caused some pharmacists to feel uncomfortable, which may have resulted in deviations from their regular behavior. On the other hand, some of the participants’ performance may have more accurately reflected their performance in daily practice.30
Competencies that still need to be developed to improve patient care in community settings were identified (Table 1). Those findings served as a starting point for future research and education plans and actions. Future work should explore professional and personal competencies according to the GLF. Also, self-assessment in competency evaluation will be implemented and considered a valuable indicator in tailoring education for pharmacist practitioners in a community setting. Those pharmacists whose behavioral statements scores increased to the highest levels were recognized as potential future project leaders, mentors, or specialists in some areas. This evaluation and education model could be implemented at the national level, and regulatory bodies have shown interest in such a possibility.31
CONCLUSIONS
The General Level Framework tool, an evidence-based competency framework, assisted with the development of pharmacists’ training needs, which are constitutive to their professional development. The Framework can be used to evaluate pharmacists’ current level of practice, thus allowing them to progress independently by participating in individually tailored education programs.
This study provides the first data on pharmacist competency development in Croatia and serves as a starting point for future education plans, studies, and transnational actions in Eastern European countries. Because it was founded in the outcomes of education and training, the GLF is applicable for managers/administrators, educators, regulators, and practitioners working towards global harmonization of practice-based expectations for practitioners. This could have important applications for fostering transnational collaboration and enhancing all aspects of our professional scope of practice, across all sectors and settings.32
REFERENCES
- 1.Govaerts MJB. Educational competencies or education for professional competence? Med Educ. 2008;42(3):234–236. doi: 10.1111/j.1365-2923.2007.03001.x. [DOI] [PubMed] [Google Scholar]
- 2.Patel J, West D, Bates IP, Eggleton A, Davies G. Early experiences of the mini-PAT (Peer Assessment Tool) amongst hospital pharmacists in South East London. Int J Pharm Pract. 2009;17(2):123–126. [PubMed] [Google Scholar]
- 3.Wass V, Van der Vleuten C, Shatzer J, Jones R. Assessment of clinical competence. Lancet. 2001;357(9260):945–949. doi: 10.1016/S0140-6736(00)04221-5. [DOI] [PubMed] [Google Scholar]
- 4.McRobbie D, Fleming G, Ortner M, Bates I, Davies JG. Evaluating skills and competencies of pre-registration pharmacists using objective structured clinical examinations (OSCEs) Pharm Educ. 2006;6(2):133–138. [Google Scholar]
- 5.Mills E, Farmer D, Bates I, Davies JG, Webb D, McRobbie D. Development of an evidence led competency framework for primary care and community pharmacists. Pharm J. 2005;275:48–52. [Google Scholar]
- 6.Dall-Alba G, Sandberg J. Educating for competence in professional practice. Instr Sci. 1996;24(6):411–437. [Google Scholar]
- 7.Webb DG, Davies JG, McRobbie D, Bates IP, Wright J. Adopting a strategy for practitioner development. Hospital Pharm. 2004;11(2):104–108. [Google Scholar]
- 8.Anderson C, Bates I, Beck D, et al. FIP roundtable consultation on pharmacy education: developing a global vision and action plan. Int Pharm J. 2006;20(2):12–13. [Google Scholar]
- 9.Anderson C, Bates I, Beck D, et al. Action! Update on the global pharmacy education consultation. Int Pharm J. 2008;22(1):6–8. [Google Scholar]
- 10.Bruno A, Bates I, Brock T, Anderson C. Towards a global competency framework. Am J Pharm Educ. 2010;74(1):Article 3. doi: 10.5688/aj740356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Competency Development Evaluation Group. GLF – General Level Framework. A Framework for Pharmacist evelopment in General Pharmacy Practice. 2nd ed. London: Competency Development Evaluation Group; 2007. [Google Scholar]
- 12.Antoniou S, Webb DG, McRobbie D, Davies JG, Wright J, Quinn J, Bates IP. A controlled study of the general level framework: results of the South of England competency study. Pharm Educ. 2005;5(3-4):201–207. [Google Scholar]
- 13.Coombes I. A Competency Framework for Pharmacy Practitioners to Provide Minimum Standard of Pharmaceutical Review - The General Level Framework Handbook. 2nd ed. Safe Medication Practice Unit Queensland Health. Adapted from NHS London and South East - CoDEG; Herston: 2009. [Google Scholar]
- 14.Meštrović A, Staničić Z, Bates I, et al. Evaluation of Croatian community pharmacists’ patient care competencies using the general level framework. Am J Pharm Educ. 2011;75(2):Article 36. doi: 10.5688/ajpe75236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Competency Development & Evaluation Group. London: www.codeg.org . Accessed February 2, 2012. [Google Scholar]
- 16.Proposal of National Strategy in Developing Health System in Croatia 2006–2011. Zagreb, Croatia: Croatian Government, Ministry of Health; 2006. [Google Scholar]
- 17.Meštrović A, Ortner M, Mucalo I, Stanicic Z, Bates I, Duggan C, Carter S. International Pharmaceutical Federation 69th Congress; Istanbul: 2009. Community pharmacists’ development using General Level Framework. CPS1-P-008, page 94. [Google Scholar]
- 18.Wiedenmayer K, Summers RS, Mackie AC, et al. Hague, The Netherlands: International Pharmaceutical and Federation World Health Organization; 2006. Developing pharmacy practice: a focus on patient care. [Google Scholar]
- 19.Register of pharmacists. Zagreb, Croatia: Croatian Chamber of Pharmacists; 2010. [Google Scholar]
- 20.Latif DA. Ethical cognition and selection-socialization in retail pharmacy. J Bus Ethics. 2000;25(4):343–357. doi: 10.1023/a:1006097521228. [DOI] [PubMed] [Google Scholar]
- 21.Wingfield J, Bissell P, Anderson C. The scope of pharmacy ethics-an evaluation of the international research literature, 1990-2002. Soc Sci Med. 2004;58(12):2383–2396. doi: 10.1016/j.socscimed.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Roche C, Kelliher F. Exploring the patient consent process in community pharmacy practice. J Bus Ethics. 2008;86(1):91–99. [Google Scholar]
- 23.Burke JM, Miller WA, Spencer AP, et al. Clinical pharmacists' competencies. Pharmacotherapy. 2008;28:806–815. doi: 10.1592/phco.28.6.806. [DOI] [PubMed] [Google Scholar]
- 24.Mills E, Farmer D, Bates I, Davies G, Webb D. The General Level Framework – use in primary care and community pharmacy to support professional development. Int J Pharm Pract. 2008;16(5):325–331. [Google Scholar]
- 25.Wallace J, Rao R, Haslam R. Simulated patients and objective structured clinical examinations: review of their use in medical education. Adv Psych Treat. 2002;8:342–348. [Google Scholar]
- 26.Prihhastuti Puspitasari H, Aslani P, Krass I. A review of counseling practices on prescription medicines in community pharmacies. Res Social Admin Pharm. 2009;5(3):197–210. doi: 10.1016/j.sapharm.2008.08.006. References and further reading may be available for this article. To view references and further reading you must purchase this article. [DOI] [PubMed] [Google Scholar]
- 27.Meštrović A. Veliki uspjeh konferencije o kompetencijama u ljekarništvu (Great success – Pharmacy Competency Conference) Farm Glas. 2009;65(3):180–183. [Google Scholar]
- 28.FIP Pharmacy Education Taskforce. A Global Competency Framework. Draft Version, August 2010.
- 29.Wallace J, Rao R, Haslam R. Simulated patients and objective structured clinical examinations: review of their use in medical education. Advances in Psychiatric Treatment. London. The Royal College of Psychiatrists. 2002;8:342–348. [Google Scholar]
- 30.Prihhastuti Puspitasari H, Aslani P, Krass I. A review of counseling practices on prescription medicines in community Pharmacies. Res Social Admin Pharm. 2009;5(3):197–210. doi: 10.1016/j.sapharm.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Meštrović A. Veliki uspjeh konferencije o kompetencijama u ljekarništvu (Great success – Pharmacy Competency Conference) Farm Glas. 2009;65(3):180–183. [Google Scholar]
- 32.FIP Pharmacy Education Taskforce. A Global Competency Framework. Draft Version. August 2010 [Google Scholar]