Abstract
Objective. To compare empathy scores between health professions students (pharmacy and nursing) and non-health professions (law) students and between first- and third-year students.
Methods. The Jefferson Scale of Physician Empathy-Student Version was completed by 282 students.
Results. Nursing and pharmacy students had significantly more empathy than did law students. Third-year pharmacy students scored higher on empathy than did first-year pharmacy students, whereas the converse was true for nurses. There was no significant difference in empathy between first- and third-year law students. Across the study years, empathy increased among pharmacy students, decreased among nurses, and remained the same among law students. Women scored higher on empathy than did males.
Conclusions. Empathy scores among university students vary depending on discipline and year of study.
Keywords: empathy, pharmacy students, nursing students, law students
INTRODUCTION
Empathy has been viewed as an ambiguous concept.1 Although there is some variation regarding the concept of empathy, it is generally defined as the ability to “see the world as others see it, be nonjudgmental, understand another’s feelings, and communicate the understanding.”2 Empathy is viewed as an important attribute for medical caregivers.3 According to Spiro, “empathy is the foundation of patient care, and it should frame the skills of the profession.”3 Empathy is the cornerstone of patient-physician relationships4 and should characterize all healthcare relationships,5 including that between patients and pharmacists. In particular, empathy significantly influences adherence to medical recommendations,6,7 reduces medical errors,8 increases patient satisfaction,9 and increases physician well-being.10 The successful interaction between patient and healthcare provider is often dependent upon the empathic nature of the physician.5 Therefore, empathy is viewed as an important attribute for students in the medical and health professions to develop.
Despite the importance of empathy in the healthcare setting, empathy declines during medical training.11-13 A longitudinal study examining changes in medical students’ empathy during medical school2 found no significant change in the first 2 years of medical school but a significant decline in empathy by the third year that continued throughout the students’ medical training. This finding is consistent with that of earlier research.4 A systematic review of 18 studies found that student empathy decreased significantly during medical and residency training.14 These studies suggest that the primary reasons for this decline were the clinical practice phase and subsequent increased patient contact aspect of training. Another possible explanation is heightened exposure to morbidity and mortality, leading to disengagement and a reduction in empathy.14 In contrast, empathy increased in medical students in Japan.15 Differences in medical school admissions criteria and the medical curriculum between Japan and America may explain this difference. Compared with American students, Japanese students may have lower baseline levels of empathy because they are more science orientated. These findings, coupled with inclusion of humanities and arts in the Japanese medical curriculum, accounts for the increase in empathy scores as these students progress through medical school.
Empathy has also been explored in the context of pharmacy practice. Empathy is particularly important to pharmacists because they are the most accessible health professionals12 and provide a wide range of services; thus, pharmacists must be adept at communication and consultation. Although there are recognized challenges in both defining and developing professionalism in pharmacy students, empathy is considered an important part of professionalism within pharmacy in America16,17 and the United Kingdom.18 A review of pharmacy literature revealed that despite a lack of consensus in defining professionalism, empathy is a frequently named characteristic of professionalism.18 The importance of empathy suggests that pharmacists’ education and training should include the development of empathy as an objective. With respect to the pharmacy profession, Lonie and colleagues11 investigated pharmacy students’ self-reported empathy scores before and after empathy training and concluded that there is a possible association between training and change in attitudes and behaviors. For instance, communication-skills training in American medical students significantly increased the empathy dimensions of “respect of self and others” and “perceiving feelings and listening.”8 However, the study also found that there was a significant decrease in the dimensions of “openness, honesty and flexibility,” perhaps suggesting that, to be beneficial, empathy and communication skills training may need to be specifically designed. Lonie and colleagues suggest that pharmacy educators should be encouraged to expand their communication-skills education and training in pharmacy schools and colleges. Indeed, many pedagogic methods have been tried in an attempt to develop empathy in students.1,2 Medical and health professionals need the time to listen to their patients, as listening is an essential tool in empathy and, therefore, in medical practice.3
There are significant gender differences in empathy.1 Women are considered more inherently empathic, and women outscored men in empathy across all years of medical training. However, the decline in empathy during medical education and training was found to be similar for both men and women. Although medical students intending to pursue people-oriented specialties (ie, family medicine, padiatrics, psychiatry, and gynecology) scored higher on empathy than did medical students intending to pursue more technology-oriented specialties (ie, anesthesiology, pathology, radiology, and surgery), there was a decline in empathy scores in students by the third year, irrespective of specialty.1 However, the magnitude of decline was greater for men compared with women and for those pursuing technology- vs people-oriented careers.
Much of the research on empathy in the medical profession has concentrated on physicians. This study aimed to expand the research field through exploring other healthcare professional students (nurses and pharmacists) as well as a non-healthcare cohort (law students). With respect to lawyers and law students, there is a paucity of research regarding whether empathy is an important skill for lawyers. Gallacher argues that empathy, especially as it relates to communication skills, should be an important part of legal education and the practice of law in real-life situations. 19 Gallacher emphasizes the role that lawyers have in communicating with different and diverse audiences, such as judges, members of the jury, other professionals, and clients.19 In the current study, law was chosen as a discipline of study as it is a non-health equivalent to the other 2 disciplines, nursing and pharmacy. The purpose of this study was to investigate empathy in students with respect to 2 hypotheses: the 2 health professions student cohorts (nursing and pharmacy) would have higher empathy scores than would the non-health-related student cohort (law), and empathy scores would differ between first- and third-year students.
METHODS
Ethical approval for this study was granted by the Research Ethics Committee of the School of Pharmacy and Biomedical Sciences, University of Central Lancashire, UK. Participants were 282 undergraduate students from the university. Seventy-six percent (n = 190) were female and 24% (n = 60) male. Students were randomly chosen from 1 of 6 student cohorts; first-year pharmacy (n = 47) students, first-year nursing students (n = 49), first-year law students (n= 30), third-year pharmacy students (n = 44), third-year nursing students (n = 47), and third-year law students (n = 33) (32 participants were missing from the year of study or program of study). Students were recruited at the start of lectures, and randomization was achieved by the researchers asking every other student entering the lecture theatre if he/she would like to take part in the study. An explanation of the study was given and students were advised that consent was implied by completion of the measure. Participants ranged in age from 19 to 51 years, with the majority being ages 19 to 27 years.
The Jefferson Scale of Physician Empathy-Student Version (JSPE-S) was used to measure empathy. The JSPE is a self-report inventory with 20 items scored on a 7-point Likert scale ranging from 1 = strongly disagree to 7 = strongly agree. Higher scores represent greater empathic orientation. The scale, which was developed by the Jefferson Medical College, is both distributed from and analyzed at the college. It was originally developed for medical students20 and was later modified to be applicable to practicing physicians and other health professionals.21 The psychometric properties of this scale have been reported as satisfactory,20 and the construct validity of the scale has been confirmed with medical students and medicine residents. The internal consistency was found to be satisfactory (0.89 and 0.87) among medical students and internal medicine residents, respectively.20 Factor analysis supports the underlying components of the JSPE-S for pharmacy and nursing students.22
Examples of JSPE-S statements, which users rate on a Likert scale, include: “Patients feel better when their health care provider understands their feelings” and “Understanding body language is as important as verbal communication in health care provider-patient relationships.” An example of a reverse-score statement is “Attention to patients’ emotions is not important in patient interview.”
RESULTS
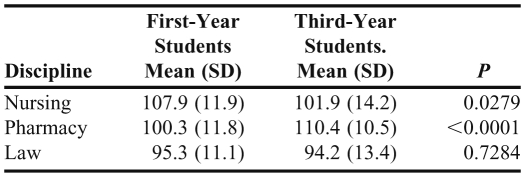
The comparison of empathy scores for groups in the study is reported in Table 1. Women had significantly higher empathy scores than did men (p < 0.001). Female participants had a mean score of 103 whereas male participants had a mean score of 97. Students in the third year of study had a slightly higher mean than did those in the first year of study. However, there was no significant difference in empathy scores between those in the first year and those in the third year of study (p = 0.41). There was no significant difference on empathy scores between those in the nursing and pharmacy programs; however, students in both of the health-related professions obtained significantly higher empathy scores than did the law students (p < 0.0001). There was a significant difference in the empathy scores of nursing students in the first year compared with the scores of those in the third year (p < 0.01). Students in the third year of study scored significantly lower than did those in the first year. There was no significant difference in empathy between participants in the first year of law school and those in the third year (p = 0.73), but empathy scores of pharmacy students in the third year of study were significantly higher compared with those of first-year students (p < 0.0001). Participants aged 27 years and older had significantly more empathy than did the younger participants (p < 0.001).
Table 1.
Levels of Empathy Among First- and Third-Year Students in Three Health and Non-Health Disciplines
DISCUSSION
The finding that women have more empathy than men is consistent with that of previous research.1 As a whole sample (nursing, pharmacy, and law students), there was no significant difference between students in the third year of study and those in the first year. This is in contrast to previous study findings, which suggest a decline in empathy between the first year and third year. 1,4 However, the studies that report a decline in empathy generally are studies conducted on samples of medical students. Because of the importance of empathy to health professionals and health professions, students in the 2 health professions (nursing and pharmacy) were expected to have significantly greater empathy than their counterparts studying law. The current study supports this assertion and may emphasize the importance of empathy in certain disciplines of study such as the health professions. People with more empathic attributes also may be drawn or attracted to the healthcare professions.
What is particularly interesting from the current study and how it contributes to the literature in a unique way is the differences found between the cohorts of students within the study. There was no significant difference in the empathy of first- and third-year law students, suggesting that, in this discipline, empathy neither increases or decreases during education. However, for the 2 health-related professions, empathy significantly declined among third-year nursing students compared with those in the first year; conversely, empathy significantly increased for third-year pharmacy students compared with first-year students. The results for the nursing students were similar to those for medical students in previous research. The increase in empathy among pharmacy students is an exception to the general findings. This study contributes to research in the field of empathy, especially with respect to the difference in empathy across disciplines and years of study. More research is needed to understand why pharmacists’ empathy scores were higher for third-year students compared with those of first-year students, whereas the converse was found for nursing students.
With respect to the current findings, the gender segregation of the subject disciplines warrants consideration. Only 4 of the nursing students were male compared with 88 who were female. Although there were more male students in pharmacy, female students were still in the majority (24 male students compared to 57 female students) in the total cohort. The genders were more equally represented among the law students (33 female and 21 male students). The gender segregation of the disciplines of study is important because empathy is viewed as a feminine trait and may therefore be more expected in more feminine-dominated disciplines such as healthcare. However, the gender composition of the disciplines in the current study does not minimize the importance of the key findings.
This study also highlights the Jefferson scale as a robust measure of empathy. The instrument is easily administered and time-efficient. More researchers and educators could use the tool to assess empathy and measure the effectiveness of empathy education and interventions to improve empathy in professional training; however, it is a commercial instrument and, therefore, not free.
Although the current study broadened the study of empathy to other disciplines, several limitations should be acknowledged. A longitudinal methodological design would have allowed the study to follow the same students throughout the study years in order to establish the differences in empathy scores more effectively. Additionally, students in the current study are from one UK university; future research should investigate students from various universities to increase the generalizability of research in this area.
More research is needed on how and why empathy changes during the education and training of all health and allied health professionals. Longitudinal research that takes into account educational interventions and their impact on different subject disciplines would aid the development of research in this field of study. A greater understanding of what students are taught at what point in the curriculum may highlight when empathy interventions would be most successful or influential. Future research might consider whether there is a significant link between work placement/patient contact during education and training and a decline in empathy. This type of research might have a significant impact on pharmacy students, particularly in the UK where pharmacy education is assessing a move toward more pharmacy practice placements in order to increase students’ practical experience.23
CONCLUSION
A finding of increased empathy scores among pharmacy students during their undergraduate education is in contrast to previous findings in the medical profession and highlights the potential importance of empathy training within education. The increasing public health role of the pharmacist in many international contexts and the potential reform of pharmacy education in the United Kingdom and beyond highlight the need for continued research into the development of empathy and professionalism within education and training.
ACKNOWLEDGEMENT
The authors thank the School of Pharmacy and Biomedical Sciences at the University of Central Lancashire for their funding support for this project.
REFERENCES
- 1.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 2.Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 3.Spiro H. The practice of empathy. Acad Med. 2009;84(9):1177–1179. doi: 10.1097/ACM.0b013e3181b18934. [DOI] [PubMed] [Google Scholar]
- 4.Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–1438. doi: 10.1007/s11606-007-0298-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005;293(9):1100–1106. doi: 10.1001/jama.293.9.1100. [DOI] [PubMed] [Google Scholar]
- 6.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther. 1998;26(5):31–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 7.Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36(8):1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Stepien KA, Baernstein A. Educating for empathy: a review. J Gen Intern Med. 2006;21(5):524–539. doi: 10.1111/j.1525-1497.2006.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim S, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Professionals. 2004;27(3):237–251. doi: 10.1177/0163278704267037. [DOI] [PubMed] [Google Scholar]
- 10.Haslam N. Humanizing medical practice: the role of empathy. Med J Aust. 2007;187(7):381–382. doi: 10.5694/j.1326-5377.2007.tb01305.x. [DOI] [PubMed] [Google Scholar]
- 11.Lonie JM, Aleman R, Dhing C, Mihm D. Assessing pharmacy self-reported empathic tendencies. Am J Pharm Educ. 2005;(2):69. Article 29. [Google Scholar]
- 12.Lonie JM. From counting and pouring to caring: the empathic developmental process of community pharmacists. Res Soc Admin Pharm. 2006;2(4):439–457. doi: 10.1016/j.sapharm.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Hojat M, Mangione S, Nasca TJ, Gonnella JS. Empathy scores in medical school and ratings of empathic behavior 3 years later. J Soc Psychol. 2005;145(6):663–672. doi: 10.3200/SOCP.145.6.663-672. [DOI] [PubMed] [Google Scholar]
- 14.Neumann M, Edelhauser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 15.Kataoka H, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009;84(9):1192–1197. doi: 10.1097/ACM.0b013e3181b180d4. [DOI] [PubMed] [Google Scholar]
- 16.Hammer DP, Mason HL, Chalmers RK, Popovich NG, Rupp MT. Developing and testing of an instrument to assess behavioural professionalism of pharmacy students. Am J Pharm Educ. 2000;64:141–151. [Google Scholar]
- 17.Hammer DP, Berger BA, Beardsley RS, Easton MR. Student professionalism. Am J Pharm Educ. 2003;67(3):1–29. [Google Scholar]
- 18.Wilson S, Tordoff A, Becket G. Pharmacy professionalism: a systematic analysis of contemporary literature (1998-2009) Pharm Educ. 2010;10(1):27–31. [Google Scholar]
- 19.Gallacher I. Thinking like non-lawyers: why empathy is a core lawyering skill and why legal education should change to reflect its importance 2011. Selected workers available at: http://works.bepress.com/ian_gallacher/14. Accessed February 1, 2012.
- 20.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. [Google Scholar]
- 21.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and speciality. Am J Psych. 2002;159(9):1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 22.Prescott J, Wilson S, Becket G. Factor analysis of the Jefferson scale of physician empathy student version. Assess Dev Matters. 2011;(4):3. [Google Scholar]
- 23.General Pharmaceutical Council. Initial education and training for pharmacists. http://pharmacyregulation.org/initial-training Accessed February 24, 2012.