Abstract
Objective. To incorporate cultural competency in a Pharmacy Skills and Application course series and assess the level of cultural competency in students who did and did not complete the courses.
Design. The course series focused on cultural competency throughout the PharmD curriculum and included such activities as self-reflection, lecture, diversity service-learning, case studies, and discussion.
Assessment. The Inventory for Assessing the Process of Cultural Competence Among Healthcare Professionals – Revised (IAPCC-R) was used to measure cultural competence in 2 cohorts: the last class preceding implementation of the new course series and the first class after its implementation. Overall scores between the 2 cohorts were not significantly different; however, 2 subscale scores were significantly higher among students who completed the course series: cultural skills (p = 0.021) and cultural encounters (p = 0.048).
Conclusions. The Pharmacy Skills and Application course series appears to improve some aspects of cultural competence in pharmacy students, but may not be sufficient to elicit change in all areas.
Keywords: cultural competency, curriculum, assessment
INTRODUCTION
Ethnic minorities constitute over one-third of the US population.1 Although ethnicity is just one element of culture, health care is affected by the increasing diversity in our country. Health care providers are more likely than they were in the past to interact with patients who speak a different language or have different health beliefs.2,3
Cultural competence is defined by the Office of Minority Health as “a set of congruent behaviors, attitudes, and policies that come together in a system, agency, or among professionals that enables effective work in cross-cultural situations.”4 Culturally competent care has been linked to improved health outcomes and the elimination of health disparities.5 Consequently, pharmacy students should undergo adequate training so they are prepared to interact with and serve the needs of culturally diverse patients.6-9 The current ACPE Accreditation Standards emphasize that each “college or school must ensure that the curriculum addresses patient safety, cultural appreciation, health literacy, health care disparities, and competencies needed to work as a member of or on an interprofessional team.”10 The CAPE outcomes also state that pharmacy curricula should teach students to provide “culturally and linguistically appropriate pharmaceutical care services to diverse patient populations.”11
In a 2007 survey of US colleges and schools of pharmacy,12 93.9% of respondents agreed that cultural competency topics needed to be added to required courses. Nearly half of the respondents had plans to implement new topics and/or courses.
A variety of strategies to address cultural competency within the curriculum have been published. Although one study described an elective course for pharmacy students,13 the majority of studies describe required courses that incorporate cultural competency content into the curriculum.14-17 Although the studies implemented slightly different teaching approaches, the majority of assessment strategies focused on student satisfaction with the course and assignments, or students’ self-perceived level of cultural competency. Only Poirier and colleagues used the IAPCC-R to measure cultural competence.16
The Drake University College of Pharmacy and Health Sciences revised its doctor of pharmacy (PharmD) curriculum to better address cultural competency. The previous curriculum included only a patient counseling practicum on cultural competency consisting of a 1-hour lecture and 2-hour laboratory on verbal counseling skills for diverse cultural populations. In the new curriculum, the Pharmacy Skills and Applications series consists of 6 courses (18 credits) across the first 3 years of the PharmD program. One of the core areas within the course series is cultural competence.
The objectives of this study were to assess the level of cultural competency among pharmacy students, as well as to describe and assess the impact of the Pharmacy Skills and Application series on pharmacy students’ self-assessed level of cultural competence using the IAPCC-R. The paper provides examples and data on how other colleges can implement and measure cultural competency outcomes in pharmacy students using a validated instrument.
DESIGN
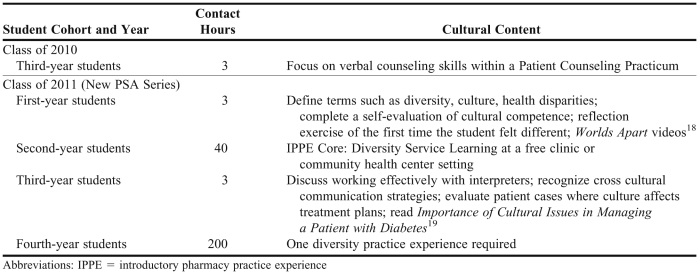
The new Pharmacy Skills and Application course series was first offered to the 2007-2008 first year (P1) class. In the series, lecture material is integrated with weekly laboratories and experiential learning opportunities. Each year students build on learning and skill development from the previous year, moving from basic to intermediate to advanced over the course of 3 years. The objective of the course series is to promote student development in 8 core skill areas, 1 of which is cultural competence. All of the skill areas are repeated throughout the series. Students attend lectures and complete laboratory activities that expose them to the importance of cultural competency in health care. An outline of cultural competency topics in the previous curriculum and in the course series is shown in Table 1 below.
Table 1.
Pharmacy Skills and Applications Course Series in a Doctor of Pharmacy Curriculum
The required resources to implement cultural competency topics within the Pharmacy Skills and Applications Series were manageable. Two faculty members, who also teach other topics within the course series, were involved in delivering the lecture and laboratory content. The Worlds Apart videos were purchased for class, but will not be repeat expenses from year to year.
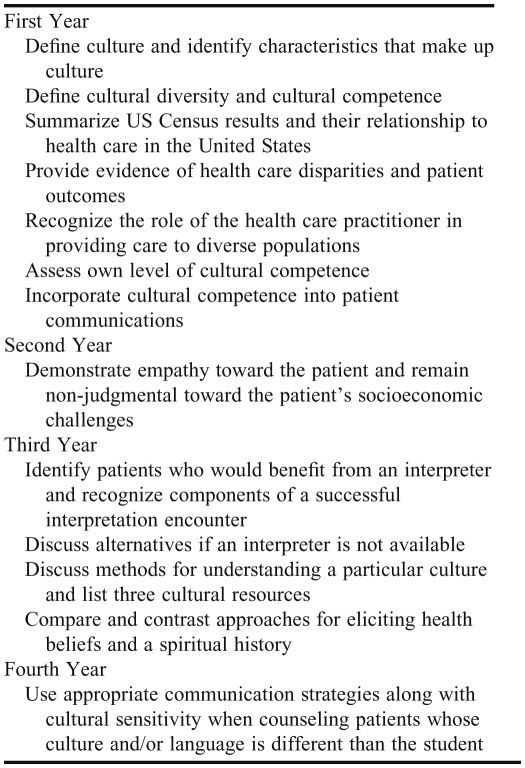
The cultural competency modules were designed based on published literature on the topic.13-17 The expertise of the instructors, gained through faculty development and training programs, also shaped the development of the course content. The learning objectives for these modules can be found in Table 2. The cultural competency topics for the graduates of the new curriculum (2007-2008 P1 class) were comprised of 2 hours of lecture and 4 hours of laboratory, spaced across the first 3 years of the program.
Table 2.
Objectives of Cultural Competency Topics in the Pharmacy Skills and Applications Course Series
In the P1 year, students attended a 1-hour lecture that defined key terms (culture, ethnicity, race), introduced evidence of health disparities, and explored strategies for communicating with culturally diverse patient populations. A self-reflection on cultural competence was completed by the students to assist with the introspective component of reflection and learning. Students also spent time in a 2-hour laboratory session in which they drew a picture of the first time they remembered feeling different from others and watched video vignettes that documented the effects of cultural issues on patient health. These activities were followed by a discussion on culture and health which was facilitated by the instructors. Using specific communication strategies to respect a particular patient’s culture was also emphasized in this section.
In the P2 year, students completed a diversity service-learning component as part of their experiential hours. They spent 40 to 42 hours interacting in medical settings with diverse patient populations, such as non-English speaking patients or indigent patients. Students completed this requirement in free clinics or community health centers around Central Iowa and then wrote a reflection paper about their experiences that addressed the following questions: How did a particular patient interaction and overall experience affect you? How were you able to help patients? How did patient differences impact the care provided by health providers? How will this experience affect your future practice?
The final lecture topic was presented in the P3 year. Students learned about working with interpreters and eliciting patients’ health beliefs through a lecture session. They also completed an assignment during a 2-hour laboratory section that required them to research a particular healthcare dilemma that might occur in a specific patient culture. Twenty-four students broke into teams of 4 and spent 20 minutes discussing the dilemma and answering the following questions: What additional questions do you have for the patient and why? What is your perception of the problem and potential treatment strategy(s)? How would you acknowledge the dilemma to the patient? What is your final recommendation? What are your plans for negotiating an agreement on a treatment strategy with the patient? After students finished the research component of the activity, each team presented their findings to the rest of the class. The class then discussed the particular culture and the healthcare dilemma that was faced.
Once students reached their P4 year and began clinical practice experiences, they were required to choose at least one that was classified as a “diversity” practice experience. This classification is based on the patient population served at the site and may include various types of patient diversity, such as race, economic status, age, certain disease states, regional location, or sexual orientation. Approximately 28% of advanced pharmacy practice experiences (APPEs) available to our students qualify as diversity practice experiences.
EVALUATION AND ASSESSMENT
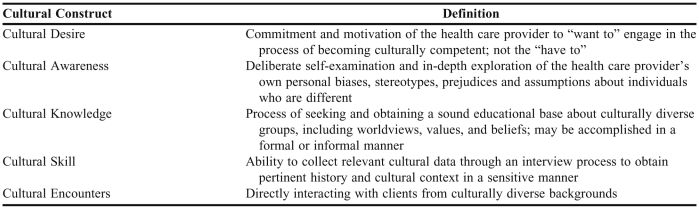
The IAPCC-R was used to measure cultural competence at the end of the PharmD program. The IAPCC-R is a self-assessment tool developed in 2002 to measure cultural competence in healthcare delivery.20 Consisting of 25 items and using a 4-point Likert scale, the IAPCC-R measures the 5 cultural constructs of desire, awareness, knowledge, skill, and encounters (Table 3). Completion time is approximately 10-15 minutes. The results range from 25-100 points, with a higher score correlating with a higher level of cultural competence. The levels of cultural competence are defined as: culturally incompetent (25-50 points), culturally aware (51-74 points), culturally competent (75-90 points), and culturally proficient (91-100 points). The tool has been used to assess cultural competence in a variety of healthcare professionals and has been studied in the United States and internationally.21-25 The IAPCC-R has been successfully used to evaluate pharmacy students in another college of pharmacy.16 Although not specifically for pharmacy students, the IAPCC-R has shown good reliability and validity20 and has also been used to test student nurses, nurses, medical students, and residents.26 This project was granted exempt status by the Drake Institutional Review Board.
Table 3.
Components of the Process of Cultural Competence in the Delivery of Health Care Services
The cultural competency portion of the Pharmacy Skills and Applications course series was assessed by comparing the IAPCC-R total competency scores and 5 subscale scores of students in 2 classes: the 2010 class who completed the PharmD curriculum before the Pharmacy Skills and Applications course series was added, and the 2011 class who were the first to complete the entire Pharmacy Skills and Applications course series. The IAPCC-R was administered using the online survey tool, Qualtrics (Qualtrics Labs Inc., Provo, UT). E-mail invitations were sent to the 2010 class in February 2010 and the 2011 class in February 2011, with follow-up reminders sent 1 week later.
All data were analyzed using SPSS (SPSS Inc., Chicago, IL) and an a priori alpha level of 0.05. Incomplete surveys instruments were addressed in 2 ways. Survey instruments were dropped from the analysis if 20% or more of the questions (5 questions) were not answered. For survey instruments that had less than 20% of the responses missing, the missing data were imputed using SPSS’s median of nearby points for that year’s cohort of students.
Based on the IAPCC-R scoring rubric, questions were scored from 1 to 4. A score of 4 was given if the most positive option of cultural competence was chosen. Survey item score were summed to generate a total cultural competency score for each respondent. Scores were also calculated for the 5 subscales of cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desire.
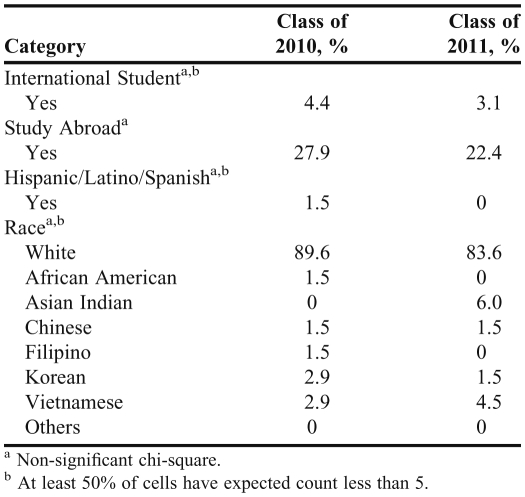
Demographic questions related to race, Hispanic/Latino/Spanish heritage, nationality, and study abroad experiences were compared across the 2 years of students using chi-square analysis. Study abroad was defined as educational opportunities outside of the United States that may have included courses or experiential learning (practice experiences) of ≥ 4 weeks in either high school or college. Independent samples t tests were used to compare the 2 years of data on cultural competency and the 5 subscales, as well as to compare cultural competency scores between those that had and had not studied abroad.
Two hundred six students were invited to participate and 143 submitted a survey instrument. Eight students (5.6%) failed to complete 80% of the survey instrument and were dropped from subsequent analyses. Of these, 5 students did not attempt any questions and 3 students skipped an entire page of the survey tool. The overall usable response rate was 69.4% (68/103 in 2010, 67/103 in 2011).
Imputing or assigning values to missing data was infrequent (usually 1 random question) and was required for only 0.5% (17) of the questions posed to the 2 cohorts. At most, a single question was left blank by 2 of the 135 student responders. Thus, we chose to include the adjusted data rather than disregard the nearly complete survey instruments.
Table 4 shows the general demographics of the sample. There was no difference between the 2 years based on the number of international students in the class, the number studying abroad, or the number with Hispanic/Latino/Spanish heritage or race.
Table 4.
Demographics of Pharmacy Students Who Completed the Inventory for Assessing the Process of Cultural Competence Among Healthcare Professionals
Over the 2 years of students surveyed, the majority (72%) scored at the culturally aware level of overall cultural competence. An additional 27% were culturally competent, and 1 student was culturally proficient. None of the students were culturally incompetent.
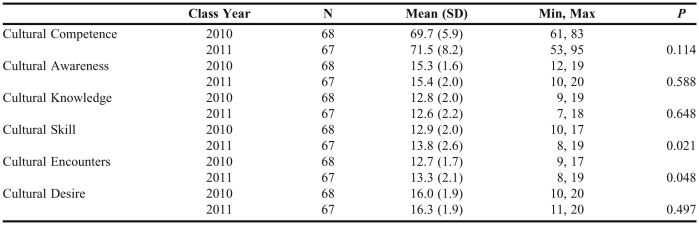
Table 5 includes the mean scores of cultural competence and its 5 subscales across each of the 2 years of data. There was no significant difference between the 2 cohorts in overall cultural competency score (p = 0.114). Only the cultural skills (p = 0.021) and the cultural encounters (p = 0.048) subscales showed a significant improvement in students’ scores under the new curriculum.
Table 5.
Pharmacy Students Cultural Competence and Subscale Scores on the Inventory for Assessing the Process of Cultural Competence Among Healthcare Professionals
Within each cohort, the range of competence scores varied dramatically. In 2010, 22 points separated the highest and lowest cultural competence score (61 vs. 83). In 2011, the range was 42 points (lowest score of 53, highest of 95).
As a post-hoc analysis, students with study abroad experience were compared to those without on the cultural competence score. No significant difference in cultural competence scores was found.
DISCUSSION
The average cultural competency score of the 2 cohorts of pharmacy students was at the upper limit of culturally aware (51-74 points). In reviewing various approaches to teaching cultural competence to US nursing students, Kardong-Edgren and colleagues suggested that “…cultural awareness, rather than cultural competency, may be a reasonable and appropriate goal for graduating students.”27 This would resonate with those who believe attainment of cultural competence is a lifelong process. They also concluded from their surveys that the range of curricular approaches used by each institution to teach cultural competence yielded similar results. If colleges and schools desire higher levels of cultural competence for graduates, a more intense, concentrated effort may be necessary. Programs with less curricular and co-curricular aspects of cultural competency should be cognizant of the amount of exposure to these topics necessary to produce long-term improvement in cultural competence or proficiency. Although the PSA series more than doubled the student contact hours (Table 1) for this topic, it did not result in a significant improvement in overall cultural competence.
Unlike our study which looked at a long-term (4-year) approach to teaching cultural competency and compared 2 separate cohorts of students, Poirier and colleagues looked at the short-term effect of a 3-credit hour course on a single cohort of pharmacy students.16 Using a pre/post comparison to identify cultural competency changes, their students’ scores improved from culturally “aware” to culturally “competent” on the IAPCC-R. Unfortunately, the timeframe of testing was short and the long-term effect of a targeted course was not assessed.
There was a significant improvement in 2 of the IAPCC-R subscales: cultural encounters and cultural skills. Encounters and skills both center on interviewing patients and interacting directly with patients who are culturally diverse. The introductory pharmacy practice experiences with Diversity Service Learning and the patient case scenarios that were added to the Pharmacy Skills and Applications course series help prepare students for these experiences. These specific components of the course series curriculum may account for the 2 subscales that showed improvement.
Of the 5 IAPCC-R subscales, students had the highest score for cultural desire (16.3/20 points) and the lowest for cultural knowledge (12.6/20 points). These findings help direct course revisions and suggest that more emphasis could be placed on content and experiences that relate to obtaining a sound educational base about culturally diverse groups, including worldviews, values, and beliefs. The relatively high score on cultural desire suggests that students already see the value of being culturally competent and have the commitment and motivation to engage in the process of becoming culturally competent.
Among the 2 cohorts, students had a wide range of cultural competence scores (53 to 95 points). This suggests that even after going through the Pharmacy Skills and Applications curriculum, there is still a substantial amount of variation in competence. Use of the IAPCC-R could help identify students in need of further instruction in this area, particularly prior to entering APPEs.
Surprisingly, the post hoc analysis comparing study abroad students to other students did not identify a difference in cultural competency scores. This might be explained in a variety of ways. The definition of study abroad in the survey instrument allowed for experiences that were as short as 4 weeks, which may not have been intensive enough to impact students’ cultural competence. Also, the students who had a study abroad experience may have had relatively low cultural competence scores at baseline and the experience had the effect of increasing their cultural competence level to that of their peers. Another explanation of the lack of difference in these subgroups of students could be related to the location of the study abroad experience. International experiences in developed countries may not have the same impact on students as experiences in undeveloped countries. Further research would be needed to suggest a more definitive relationship as other authors point to improvements in cultural competence levels following international study abroad by nursing students.28,29
The level of cultural competence of pharmacy students was measured using a self-assessment survey instrument, the IAPCC-R. Although one way to determine the impact of the new Pharmacy Skills and Applications course series, students’ scores may have been influenced by a social desirability effect and the student’s selection of the culturally correct answer even if it did not represent their true belief. Another way to evaluate cultural competence is to observe student interactions and counseling with diverse patients. Although this approach would require substantial resources, including patients, evaluators, and time, it may be an alternate way to evaluate the impact of the course series on direct patient care so that appropriate curricular revisions could target specific areas in need of improvement.
The lack of cultural diversity of the student population within our college of pharmacy was a limitation for the study. The majority of students in both cohorts identified themselves as white (2010, 89.6% and 2011, 83.6%). This may limit the generalizability of our findings to other institutions with different student demographics. It also limited our ability to analyze any difference in level of cultural competence by race. In addition, a small number of missing survey answers were replaced based on other responses and could have a slight effect on individual competency scores. This effect is likely to be minimal because only 0.5% of the questions had an imputed value.
It was not possible to account for all of the variables that could have impacted students’ cultural competence; therefore, there may have been factors outside of the Pharmacy Skills and Applications course series and aside from study abroad experiences, international student status, and race and/or ethnicity that influenced IAPCC-R scores. Students did not have the same practice sites for diversity service learning experiences in the P2 year, so the impact of that variation should also be considered.
Because 2 different cohorts were compared rather than individual students, we do not know whether and how the average student improved over the course of the curriculum. Including the class of students who completed the previous curriculum as a control group had some validity, as the general admissions process did not change between cohorts and the admissions profiles of the students in each cohort were similar. Regardless of the level of cultural competence students had prior to starting the Pharmacy Skills and Applications course series, additional changes to the curriculum may be necessary to achieve higher levels of cultural competence in students.
CONCLUSIONS
As colleges and schools of pharmacy explore the best methods for implementing cultural competence training into their curricula, this research offers an objective approach to teaching and measuring students’ cultural competence. Using a variety of activities, such as self-reflection, lecture, diversity service-learning, case studies, and discussion, seemed to be effective in improving certain areas of pharmacy students’ cultural competence. The course content and experiences in the Pharmacy Skills and Applications course series may not be sufficient to improve all aspects of students’ cultural competence, but this needs to be explored further by tracking individual student progress over the course of the curriculum. In light of these findings, the college will review the course and investigate lecture material and co-curricular activities that may aid in enhancing student cultural competence.
ACKNOWLEDGMENTS
Funding for this research project was provided by a Drake University Research Grant and a Drake University Faculty Development Grant.
REFERENCES
- 1.US Census Bureau. 2010 Census Shows America's Diversity. http://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn125.html. Accessed January 18, 2012.
- 2.US Census Bureau. United States S1601: Language Spoken at Home. http://factfinder.census.gov/servlet/STTable?_bm=y&-qr_name=ACS_2009_1YR_G00_S1601&-geo_id=01000US&-ds_name=ACS_2009_1YR_G00_&-_lang=en. Accessed January 18, 2012.
- 3.National Center for Cultural Competence. The compelling need for cultural and linguistic competence. http://nccc.georgetown.edu/foundations/need.html. Accessed January 18, 2012.
- 4.US Department of Health and Human Services. Office of Minority Health. http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=11. Accessed January 18, 2012.
- 5.O’Connell MB, Korner EJ, Rickles NM, Sias JJ. Cultural competency in health care and its implications for pharmacy. Pharmacotherapy. 2007;27(7):1062–1079. doi: 10.1592/phco.27.7.1062. [DOI] [PubMed] [Google Scholar]
- 6.Shaya FT, Gbarayor CM. The case for cultural competence in health professions education. Am J Pharm Educ. 2006;70(6):Article 124. doi: 10.5688/aj7006124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services. Health Resources and Services Administration. Transforming the face of health professions through cultural and linguistic competence education. http://www.hphnet.org/attachments/article/50/US%20HRSA.pdf. Accessed January 18, 2012.
- 8.Assemi M, Cullander C, Hudmon KS. Implementation and evaluation of cultural competency training for pharmacy students. Ann Pharmacother. 2004;38(5):781–786. doi: 10.1345/aph.1D402. [DOI] [PubMed] [Google Scholar]
- 9.Vess Halbur K, Halbur DA. Essentials of Cultural Competence in Pharmacy Practice. Washington DC: American Pharmacists Association; 2008. [Google Scholar]
- 10.Accreditation Council for Pharmacy Education (ACPE) Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed January 18, 2012.
- 11.American Association of Colleges of Pharmacy. CAPE Educational Outcomes. http://www.aacp.org/resources/education/Documents/SocialandAdminDEC06.pdf. Accessed January 18, 2012.
- 12.Onyoni EM, Ives TJ. Assessing implementation of cultural competency content in the curricula of colleges of pharmacy in the United States and Canada. Am J Pharm Educ. 2007;71(2):Article 24. doi: 10.5688/aj710224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Evans E. An elective course in cultural competence for healthcare professionals. Am J Pharm Educ. 2006;70(3):Article 55. doi: 10.5688/aj700355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westberg SM, Bumgardner MA, Lind PR. Enhancing cultural competency in a college of pharmacy curriculum. Am J Pharm Educ. 2005;69(5):Article 82. [Google Scholar]
- 15.Muzumdar JM, Holiday-Goodman M, Black C. Cultural competence knowledge and confidence after classroom activities. Am J Pharm Educ. 2010;74(8):Article 150. doi: 10.5688/aj7408150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Poirier TI, Bulter LM, Devraj R, et al. A cultural competency course for pharmacy students. Am J Pharm Educ. 2009;73(5):Article 81. doi: 10.5688/aj730581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vyas D, Caligiuri FJ. Reinforcing cultural competency concepts during introductory pharmacy practice experiences. Am J Pharm Educ. 2010;74(7):Article 129. doi: 10.5688/aj7407129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green A, Betancourt J, Carrillo JE. Facilitator’s Guide: Worlds Apart: A Four-Part Series on Cross-Cultural Healthcare. Boston: Mass: Fanlight Productions; 2003. [Google Scholar]
- 19.Shane-McWhorter L, Oderda LH. Importance of cultural issues in managing a patient with diabetes. Consult Pharm. 2007;22(5):431–437. doi: 10.4140/tcp.n.2007.431. [DOI] [PubMed] [Google Scholar]
- 20.Campinha-Bacote J. The Process of Cultural Competence in the Delivery of Healthcare Services. 5th ed. Cleveland: Ohio: Transcultural C.A.R.E. Associates; 2007. [DOI] [PubMed] [Google Scholar]
- 21.Noble LM, Noble A, Hand IL. Cultural competence of healthcare professionals caring for breastfeeding mothers in urban areas. Breastfeed Med. 2009;4(4):221–224. doi: 10.1089/bfm.2009.0020. [DOI] [PubMed] [Google Scholar]
- 22.Hunter JL, Krantz S. Constructivism in cultural competence education. J Nurs Educ. 2010;49(4):207–214. doi: 10.3928/01484834-20100115-06. [DOI] [PubMed] [Google Scholar]
- 23.Olt H, Jirwe M, Gustavsson P, Emami A. Psychometric evaluation of the Swedish adaptation of the inventory for assessing the process of cultural competence among healthcare professionals – revised (IAPCC-R) J Transcult Nurs. 2010;21(1):55–64. doi: 10.1177/1043659609349064. [DOI] [PubMed] [Google Scholar]
- 24.Musolino GM, Babitz M, Burkhalter ST, Thompson C, Harris R, Ward RS, Chase-Cantarini S. Mutual respect in healthcare: assessing cultural competence for the University of Utah Interdisciplinary Health Sciences. J Allied Health. 2009;38(2):e54–e62. [PubMed] [Google Scholar]
- 25.Capell J, Dean E, Veenstra G. The relationship between cultural competence and ethnocentrism of health care professionals. J Transcult Nurs. 2008;19(2):121–125. doi: 10.1177/1043659607312970. [DOI] [PubMed] [Google Scholar]
- 26.Inventory for Assessing the Process of Cultural Competence Among Healthcare Professionals-Revised (IAPCC-R) http://www.transculturalcare.net/iapcc-r.htm. Accessed January 18, 2012. [DOI] [PubMed]
- 27.Kardong-Edgren S, Cason CL, Walsh Brennan AM, Reifsnider E, Hummel F, Mancini M, Griffin C. Cultural competency of graduating BSN nursing students. Nurs Educ Perspect. 2010;31(5):278–285. [PubMed] [Google Scholar]
- 28.Larson KL, Ott M, Miles JM. International cultural immersion: en vivo reflections in cultural competence. J Cult Divers. 2010;17(2):44–50. [PubMed] [Google Scholar]
- 29.Inglis A, Rolls C, Kristy S. The impact on attitudes towards cultural difference of participation in a health focused study abroad program. Contemp Nurse. 2000;9(3-4):246–255. doi: 10.5172/conu.2000.9.3-4.246. [DOI] [PubMed] [Google Scholar]