Abstract
Objectives. To develop, pilot test, and evaluate a continuous professional development (CPD) process for first-year pharmacy (P1) students.
Design. Students and faculty members were introduced to the important elements of the CPD process via a live training program. Students completed the year-long 4-step CPD cycle by identifying a learning objective, creating a plan, completing the learning activity, evaluating their learning outcome, documenting each step, and meeting with their faculty advisor for feedback and advice.
Assessment. Seventy-five first-year students (100%) successfully completed the CPD process during the 2009-2010 academic year. The students spent an average of 7 hours (range 2 to 20 hours) on the CPD process. The majority of faculty members (83%) completing the survey instrument found the process valuable for the students and would like to see the program continued.
Conclusion. Integrating a CPD requirement for students in a college or school of pharmacy is feasible and valuable to students’ developing life-long learning skills. Effective and frequent training of faculty members and students is a key element in the CPD process.
Keywords: continuous professional development, continuing pharmacy education, pharmacy students
INTRODUCTION
The Institute of Medicine (IOM), in a 2009 report, acknowledged that the current continuing education system for health professionals is not ideal.1 The report mentions several reasons why the healthcare professions should change to a continuous professional development (CPD) process. One of the IOM’s concerns was that “health professionals and their employers tend to focus on meeting regulatory requirements rather than identifying personal knowledge gaps and finding programs to address them.” This deficiency is overcome in a straightforward manner when following a continuous professional development model because the CPD process requires self-reflection and identification of a personal plan.
Pharmacists are incorporating CPD into their practice in several countries including Canada, the United Kingdom, and New Zealand.1 Pharmacy organizations supporting the CPD process include the American Pharmacists Association,2 American Society of Health-Systems Pharmacists,3 American Association of Colleges of Pharmacy,4 and the National Association of Boards of Pharmacy.5 The Accreditation Council for Pharmacy Education (ACPE) describes continuous professional development as: “the lifelong process of active participation in learning activities that assists individuals in developing and maintaining continuing competence, enhancing their professional practice, and supporting achievement of their career goals.”6
Several studies involving use of the CPD process by United States’ pharmacists have been published. A study from Colorado by McConnell and colleagues compared self-reports of pharmacists who undertook a 10-month CPD process to those of pharmacists who were instructed to follow the traditional continuing pharmacy education (CPE) process.7 The pharmacists who participated in the CPD process reported significant improvements in their practice compared to the pharmacists who followed the traditional format. However, the study also found that the CPD pharmacists reported more often that time was a barrier to completing educational activities. A study that compared live and online CPD training for first-year pharmacy students found that students who participated in the live training were significantly better at writing learning objectives than the students who participated in the online training.8 The literature also contains some limited information on the training of pharmacists and pharmacy students on the CPD process. A search of the Journal using the search terms “continuing/continuous professional development” in the title identified 5 articles. Janke and colleagues stated that “Our biggest opportunity to influence the next phase of CPD development is through work with our students.”9 In another study, Canadian pharmacists were concerned about their lack of skills in self-identification of learning needs.10 No articles were found in the Journal that related to teaching the CPD process in the curriculum. A search of abstracts in the Allacademic using the terms “continuing professional development” and “pharmacy curriculum” identified 18 abstracts, but only 1 related to teaching CPD in the curriculum.11 That abstract describes a process for second-year pharmacy students creating a CPD document, whereas our project uses first-year pharmacy students in creating a CPD document.
According to the ACPE 2007 Standards, faculty members in accredited colleges and schools of pharmacy are required to implement a CPD process for their learning activities. The North Carolina Board of Pharmacy allowed pharmacists to use a CPD process in addition to the traditional continuing professional education documentation process. However, pharmacists who wish to participate in the continuous professional development process as a means to maintain licensure must participate in specialized training offered by the state.12
The number of learning approaches or activities that a pharmacist can use when using a CPD process is more diverse than in the traditional CPE format. The CPD learning process incorporates traditional learning formats as well as additional learning activities that are customized to the user; thus, the learning activities vary depending on the interest and preferred learning style of the pharmacist. Whereas, traditional CPE requires a more formal approach to learning such as attending a live seminar or completing a home study course. Another difference is that in the CPD model, educational needs are identified through self-directed personal assessment or peer assessment; thus, the relevance to practice is high. Unlike CPE which is measured only by credit hours earned, CPD is measured by credit hours earned and/or learning objectives achieved.7
Because continuing to obtain pharmacy knowledge after entering pharmacy practice may be just as important as the learning that occurs in pharmacy school, developing lifelong learning skills in pharmacy students is critical. ACPE Guideline 25.4 states: “Faculty should provide students both content and perspectives unique to their discipline and critical to problem solving and lifelong learning.”13 Most students are in pharmacy school for only 4 years, whereas their career may span more than 30 years. Thus, imparting lifelong learning skills to pharmacy students may be beneficial to their professional success.
Our main goal was to evaluate the feasibility, eg, the impact on workload from a student and faculty perspective, of implementing a CPD process for first-year pharmacy students. This manuscript describes the design and implementation of the program. The programmatic objectives were: (1) to train students and faculty in the CPD process and their respective roles in the implementation process; (2) to implement a student-driven process that required students to choose a topic of interest, design a plan, implement the plan, and reflect on the process; and (3) to help students recognize the value of the CPD process to their pharmacy careers.
DESIGN
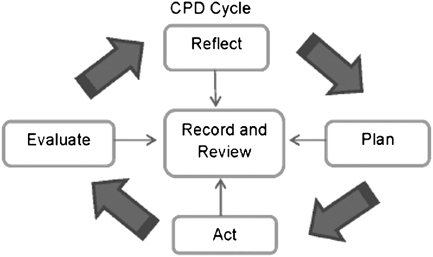
In 2009, the Wegmans School of Pharmacy implemented the CPD program for P1 students. The process was developed by an ad hoc faculty CPD committee. Faculty advisor training sessions were conducted in the summer of 2009, during which the concept and relevant importance of CPD were explained, as well as the planned process for implementation at St. John Fisher College. The assistant dean of student affairs conducted a 90-minute session on the CPD 4-step process (Figure 1)14 and use of student documentation forms. Faculty advisors were assigned to oversee the CPD process for 8 to 12 students during the pilot year, in addition to fulfilling their usual student advising responsibilities.
Figure 1.
Continuous Professional Development Cycle14
The P1 students were given a 1-hour training session during the fall 2009 orientation on the CPD process and its long-term benefits to their careers. The assistant dean of student affairs reviewed the 4-step model (Figure 1) and presented a sample of a CPD paper and provided suggestions on how the “action” step could be accomplished. The documents used in the training sessions were posted to a shared computer drive accessible by students and faculty members.
Following the faculty and student training, the students began the first step of the CPD process, which was to reflect on a learning goal or objective based on personal interests.14 The students were assisted with this process by faculty advisors who conducted one-on-one meetings with students to review their understanding of the CPD process and to discuss possible learning interests. During this meeting, the faculty advisor mentored the student on self-reflection and identifying one specific, measurable, attainable, relevant, and time bound (SMART) learning objective for the year, ranging from a learning outcome from a class syllabus to a personal volunteer activity. The goal for students was to complete 1 CPD cycle and achieve their personal learning objective by April 1st of the academic year.
The learning objectives were student selected and varied considerably from student to student. For example, a student who wanted to learn more about diversity might state the following: “I would like to work in an inner city pharmacy upon graduation and so my objective is to enhance my understanding of patient diversity as it relates to pharmacy practice.” The advisor had to ensure that the objective was doable within the semester, so there was some give and take when constructing the objective.
The advisors then helped students with the second step of the CPD cycle, forming a plan, which in the case of the diversity example could be to shadow an inner city pharmacist and research literature on the services available in inner city pharmacies. The CPD committee recommended that a minimum of 2 activities be included in the plan and that realistic deadlines be established to ensure the plan was completed by April 1st. Other examples of learning activities that were shared with the students included: shadowing an expert to attain skills and knowledge; attending one or more professional development programs; reading books/journals; and completing volunteer work that was related to the learning objective. Students could choose other learning activities but they had to be approved by their advisor.
The third step in the CPD cycle was for students to perform the learning activities discussed with their advisor and document their progress through various means of communication (ie, e-mail, verbally, written report to the advisor).
The final step of the CPD cycle, was for the students to evaluate their accomplishments. Students were instructed to answer the following questions in writing: (1) Was the learning activity of adequate content and was the method appropriate for achieving my learning objective? (2) Was my learning plan effective? Describe. (3) How well did I meet my own deadlines? (4) Based on this experience how would I change my approach to learning for the future?
Deadlines for completion of each of the 4 steps of the CPD cycle were established prior to beginning the process (Objective by September 1; Plan by October 1, Action by January 31, and Evaluation by April 1). Students had to obtain approval from their advisors using a documentation form after completing each step and before proceeding with the next step. The advisors had the flexibility to adjust the dates for deadlines if a student needed to redo one of the steps in the process. As an incentive to complete the process on time, students were told that those who failed to do so would not be able to register for the next semester’s courses until the process was completed. This delay in registration is an incentive to complete the process on time as students may not get their preferred elective course or preferred laboratory section time. This study was approved by the college’s Institutional research Board as exempt research.
EVALUATION AND ASSESSMENT
The initial CPD program was conducted from August 2009-March 2010. Twenty-four faculty members completed advisor training on the CPD process in the summer of 2009 prior to the arrival of P1 students. During orientation, all 75 students in the P1 pharmacy class attended the training session on the CPD process.
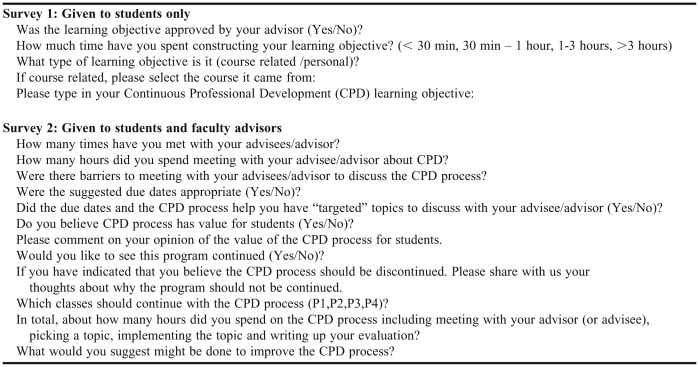
Seventy-five (100%) students in the first-year pharmacy class successfully completed the CPD process as documented by faculty advisor sign-off. In November 2009, a survey instrument was administered using the E*Value online survey system to assess students’ opinions regarding the CPD process and their engagement in the pilot program (Appendix 1).
This midpoint survey instrument was completed by 42 (56%) students, all but one of whom reported having their learning objective approved by their advisor at the time of the survey, indicating they were on schedule. The data collected were analyzed using descriptive statistics.
Fifteen (36%) respondents spent between 30 minutes and 1 hour constructing their learning objective, while 17 (40%) spent between 1 and 3 hours. Regarding the origin of their learning objective, 17 (40%) reported it was related to a pharmacy course they were taking that year. Of those 17 students, 14 (70%) chose a topic related to the Top 200 Drugs I course. The remaining 24 (57%) students chose a topic that was more personal or was identified through sources outside of their coursework.
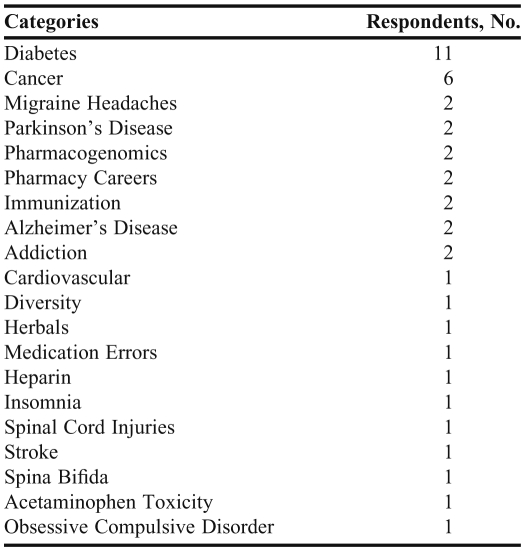
Students’ learning objectives reflected more than 20 different subjects (Table 1) ranging from disease states such as migraine headaches and Parkinson’s disease, to topics of a more personal nature such as pharmacy careers and diversity. The 2 most common subjects were diabetes and cancer.
Table 1.
Categories of Learning Objectives Chosen by First-Year Pharmacy Students Participating in a Continuous Professional Development Program (N = 42)
At the completion of the CPD process, a second survey was administered to students and faculty advisors using the Qualtrics online system to assess the time and effort spent during the process, their perceptions about the process, and its value. The purpose of this second survey instrument was not to assess the learning outcome of the CPD process, but rather to assess the process itself.
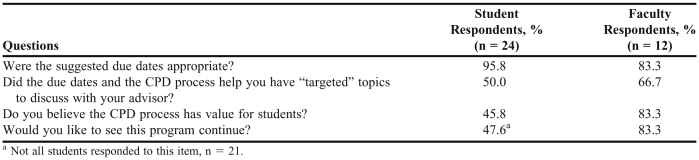
Twenty-four (32%) students completed the second survey instrument. Students reported having met with their advisor an average of 2 to 3 times during the process, for a total of 1.3 hours. Students reported that the most significant barrier to meeting with their advisors was the students’ inability to make it a priority. Ten of the 21 students who responded to this question (48%) would like to see the program continued throughout the 4-year curriculum. Students spent an average of 7 hours on the overall CPD process, with total time ranging from 2 to 20 hours. Student responses to selected survey questions, including how they valued the CPD process, are presented in Table 2. In response to the open-ended questions, students provided positive feedback as well as constructive criticism. Students suggested providing a list of sample topics that students could choose from and better educating both students and faculty members on the entire CPD process.
Table 2.
Respondents’ Positive (Yes) Responses to Selected Survey Questions Regarding Participation in a Continuous Professional Development Program for First-Year Pharmacy Students
Twenty-four (100%) faculty members successfully served as advisors for the students throughout the CPD process. Twelve (50%) faculty members completed the survey instrument, providing similar responses to those of the students (Table 2). Faculty members reported meeting with their advisees an average of 2 to 3 times throughout the process, and spending a total of 1.1 hours with each student. Both faculty and students reported that the most significant barrier to meeting was a lack of prioritizing the CPD project. Ten faculty respondents (83.3%) respondents would like to see the program continued throughout the 4-year curriculum. The faculty advisors reported spending between 1 and 20 hours on the entire CPD process but did not specify whether this was the average time spent with each advisee or total time spent with all advisees.
DISCUSSION
The Wegmans School of Pharmacy believes that creating lifelong learning principles in students that will last beyond graduation day is critical in an ever-changing field such as pharmacy. The purpose of our study was to evaluate the feasibility of implementing a CPD process with first-year pharmacy students. Our CPD process modeled how to identify educational needs through self-directed personal assessment and assisted participants in addressing weaknesses in knowledge, skills, and/or abilities specific to pharmacy practice. By developing, implementing, and assessing a continuous professional development program at the Wegmans School of Pharmacy, we oriented our new pharmacy students to the IOM’s perspective and began training them and our faculty members in the principles of continuing professional development.
Of the P1 class, 75 (100%) students and 24 (100%) advisors completed the CPD process. After completing the pilot CPD program, P1 students suggested that future offerings of the program provide sample CPD topics to students. For the following year, the CPD committee suggested the following topics: focused therapeutic topic or disease state, leadership, diversity, service, work-life balance, and career goals.
The amount of time spent on the CPD process varied significantly. For example, the amount of time spent on writing learning objectives ranged from 30 minutes to 3 hours. Perhaps additional education on the definition and creation of SMART learning objectives will decrease the time that students’ spend creating objectives and the time that advisors’ spend reviewing and editing them.
The diversity of faculty roles may account for some of the inconsistency in faculty time spent advising. Most of the P1 teaching is done by the 6 faculty members in the pharmaceutical sciences department who are routinely available in their offices and laboratories, which are located within the pharmacy building. On the other hand, the pharmacy practice faculty members who teach later in the pharmacy curriculum and are frequently off-site may have little interaction with P1 students. This lack of routine contact, in combination with off-campus responsibilities, makes these faculty advisors less accessible to students.
College or schools considering the CPD process should consider matching students to appointed “CPD faculty consultants” rather than to their academic advisors. These consultants could be selected based on the frequency of student contact in required coursework or on student interests and faculty expertise. For instance, P1 students could complete the CPD process with P1 course faculty members and P4 students with advanced pharmacy practice experience faculty preceptors.
Although 45.8% of the students recognized the value of the CPD process, more than 54% did not, suggesting that supplementary training on the importance of CPD is required. Brief discussions held periodically throughout their pharmacy student career would reinforce the importance of the process and help to establish lifelong learning behaviors. Also, extending the CPD program into the P4 year with preceptors may help correlate the CPD process to pharmacy practice. After 3 years of CPD training, students may have adopted a philosophy of life-long learning. Discontinuing the process in the P4 year may have unintended effects, such as sending a message that experiential education is a replacement for CPD. Incorporating the CPD process into the P1 to P3 years will familiarize the students with the method of CPD and permit them to become more proficient in applying it, and hopefully, realizing its benefit to their professional development. Continuing the CPD process during the P4 year and APPEs mimics its integration into actual pharmacy practice. As a result, students would be able to easily incorporate CPD principles into their professional lives postgraduation. In addition, requiring students to complete the process throughout APPEs would allow our preceptors to be introduced to this new practice of continuing education, perhaps causing them to self-reflect on their continuing education habits.
Whether the students’ successfully completed the CPD process was determined by their faculty advisor. Although the advisor had a significant role throughout the process, our survey results showed that the time that each faculty member dedicated to the process varied. It is unknown whether this variation in faculty advising time affected the quality of the CPD process for the individual student. Perhaps future changes in the program should include the assessment of a sampling of completed CPDs to ensure that students have a more consistent experience.
To improve the process for the future, students suggested providing a list of sample topics that from which students could choose, and better educating students and faculty members on the entire CPD process. Faculty responses to the open-ended questions included positive feedback regarding the benefits and value of the program to students and suggestions to provide more structured training for faculty members and students.
Since the initial implementation of the CPD process, we continue to analyze, identify, and correct problems as they appear (ie, providing sample topics, updating faculty training yearly, etc). Also, after compiling the survey results, we have identified additional areas of concern (ie, variation in time spent on the process, additional educational needs, etc) and expansion (ie, including P4 students in the process, identifying CPD faculty consultants, APPE preceptor training, etc).
The findings presented here may vary from those of colleges or schools with different programs or different faculty member and student characteristics. For example, we have a relatively small PharmD program that is taught exclusively by our faculty. Our school offers no other degrees. This focus on PharmD students permits more regular and intimate contact with students.
CONCLUSION
Implementation of a CPD process in the pharmacy curriculum for first-year pharmacy students was feasible and contributed to students’ development of lifelong learning skills. In our pilot project, students followed the traditional 4-step cycle (Figure 1) of composing a learning objective, creating a plan, performing the action, and self-assessing their own process. Each step was documented and required approval from the student’s advisor. The feedback we received indicated that effective and frequent training of faculty members and students is one of the key elements that should be included when requiring students to learn about and complete the CPD cycle.
Appendix 1. Survey Questions
REFERENCES
- 1. Redesigning Continuing Education in the Health Professions. Washington, DC: IOM (Institute of Medicine) 2010. The National Academies Press. www.nap.edu/catalog.php?record_id=12704. Accessed January 5, 2012.
- 2. American Pharmacists Association House of Delegates 2005, Policies web page. http://www.pharmacist.com/AM/Template.cfm?Section=House_of_Delegates&Template=/CM/ContentDisplay.cfm&ContentID=10542. Accessed January 5, 2012.
- 3. American Society of Health Systems Pharmacist Position Statement web page. https://www.ashp.org/DocLibrary/BestPractices/EducationPositions.aspx. Accessed January 5, 2012.
- 4. American Association of Colleges of Pharmacy, review of Policies 1980-2010. http://www.aacp.org/governance/HOD/Documents/Cumulative%20Policy%201980%20-%202010.pdf. Accessed January 5, 2012.
- 5. National Association of Boards of Pharmacy, Continuing Competency Resolutions 2003. http://www.nabp.net/news/continuing-pharmacy-practice-competency-resolution-no-99-7-03/. Accessed January 5, 2012.
- 6. Accreditation Council for Pharmacy Education. http://www.acpe-accredit.org/deans/cpd.asp. Accessed January 5, 2012.
- 7.McConnell KJ, Newlon CL, Delate T. The impact of continuing professional development versus traditional pharmacy education on pharmacy practice. Ann Pharmacother. 2010;44(10):1585–1595. doi: 10.1345/aph.1P161. [DOI] [PubMed] [Google Scholar]
- 8.Tofade T, Franklin B, Noell B, et al. Evaluation of a continuing professional development program for first year student pharmacists undergoing an introductory pharmacy practice experience. Innovations Pharm. 2011;2(2):1–13. http://www.pharmacy.umn.edu/innovations/prod/groups/cop/@pub/@cop/@innov/documents/article/cop_article_337972.pdf. Accessed January 5, 2012. [Google Scholar]
- 9.Janke KK. Continuous professional development: don’t miss the obvious. Am J Pharm Educ. 2010;74(2):Article 31. doi: 10.5688/aj740231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Austin Z, Marini A, Glover N, et al. Continuous professional development: a qualitative study of pharmacists’ attitudes, behaviors, and preferences in Ontario, Canada. Am J Pharm Educ. 2005;69(1):Article 4. [Google Scholar]
- 11.Evans J, Hamilton R, Dominelli A, et al. Introduction of continuing professional development to the pharmacy curriculum [abstract]. 108th Annual Meeting of the American Association of Colleges of Pharmacy, Orlando, Florida, July 14-17, 2007. Am J Pharm Educ. 2007;71(3):Article 60. [Google Scholar]
- 12. North Carolina Board of Pharmacy CPD web page. http://www.ncbop.org/CPD.htm. Accessed January 5, 2012.
- 13. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (“Standards 2007, version 2.0”). http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed January 5, 2012.
- 14.Rouse MJ. Continuing professional development in pharmacy. Am J Health-Syst Pharm. 2004;61:2069–2076. doi: 10.1093/ajhp/61.19.2069. [DOI] [PubMed] [Google Scholar]