Abstract
Objective. To assess the impact of team-based learning (TBL) in a foundational pharmacokinetics course.
Design. The course was arranged into 5 modules based on the TBL format. Each module contained preclass preparation; readiness-assurance process; and in-class, clinical cases. Survey instruments on professionalism and attitudes of team learning were administered pre- and post-course.
Assessment. Examination grades focused at the evaluation/creation level were significantly higher in the TBL format compared with the previous year. Professionalism scores increased over the course of the semester, particularly in altruism and honesty. Other measures of team-learning attitudes significantly increased over time, although there was no change in major subscales. End-of-semester course evaluations showed improvements in active engagement and in various areas of skill development.
Conclusion. The TBL format can be used successfully in a foundational pharmacokinetics course to increase higher levels of learning, team-learning skills, and professionalism in pharmacy students.
Keywords: self-directed learning, cooperative learning, team-based learning, active learning, professionalism, pharmacokinetics
INTRODUCTION
Pharmacokinetics is often considered to be a quantitative discipline that involves the application of mathematical principles to describe drug behavior within the body1; however, there is a large conceptual component to the discipline that goes beyond the calculation aspects. Because the brain processes exact mathematical calculations, mathematical estimations, and conceptual concepts using different regions,2it is important to use instructional techniques that foster learning in all 3 modalities.
There are 2 important realities in medical education: differentiating subtle differences between 2 diseases and being able to quickly diagnose the correct form of that disease suffered by a patient.3 These concepts translate directly to pharmacy education, as students need to recognize subtle differences among medications in pharmacotherapy practice and quickly apply that information to a patient. Within pharmacokinetics, the important competencies are the ability to calculate dosing regimens, recover patient specific parameters, and apply pharmacokinetics concepts in lieu or in support of mathematical calculations. This may be an especially challenging task in a community pharmacy setting that relies more on the conceptual framework than on mathematical constructs based on measured drug concentrations, as often seen in the hospital setting.
In traditionally structured pharmacokinetics courses, the content is typically taught in a lecture-based format, with students subsequently using the content in either an applied pharmacokinetic course, therapeutics course, or during experiential training. Delaying students’ opportunity to learn how to use the content does not fit well with how adults learn best.3 Adults tend to learn what is most immediately important to them because it is relevant and has high value; they consequently will pay minimal attention to information not perceived to be valuable based on lack of immediate relevance.4Authentic problem-solving is one of the well-supported instructional techniques to promote critical thinking, as are step-by-step guided practice, structured collaboration, communication, and formative feedback.5 These are all components of team-based learning (TBL).
According to a 2011 survey by the National Association of Colleges and Employers, the top 5 skills desirable to future employers are verbal communication skills and the ability to make decisions, solve problems, plan and organize work, and obtain and process information.6 The 2010 survey tool included work ethic, initiative, interpersonal skills, and teamwork within their top 10 skills. These findings are congruent with the beliefs of pharmacy educators7 and current accreditation standards. TBL is 1 strategy that may facilitate student development of the skills necessary to meet the needs of the job market. This strategy also may address the aforementioned modalities to learn calculations, estimations, and concepts.
Previous attempts have been made to design a pharmacokinetics course to promote critical thinking and increase the amount of self-directed learning.1 In a previous course design, students prepared before class, their class time was used for discussion of important concepts in a recitation-type approach. This approach used smaller groups (ie, groups of no more than 50 students) attending class only once a week instead of the more traditional format of the full cohort attending class 3 times a week. Examinations focused more on application and higher-order cognitive abilities compared with the traditional lecture format used in previous years. Although examination performance did not change, there was an increase in higher-order questions, suggesting that it was successful in developing higher-order thinking and self-directed learning. Limitations of this format include inefficiency: each session was repeated 3 times a week for each subset of the cohort, and the format did not promote some of the desired skills, such as teamwork or communication. The recitation format also is limited with respect to ensuring individual accountability for preclass preparation.
This manuscript describes the initial results of transitioning a large-enrollment pharmacokinetics course to a TBL format. Goals of this transition were to provide opportunities to develop skills beyond that of content knowledge and to provide an educational setting to facilitate a more natural physiologic path of learning not accomplished through a traditional, linear instructional model.
DESIGN
Pharmacokinetics instruction in the doctor of pharmacy (PharmD) program at the School of Pharmacy at The University of North Carolina at Chapel Hill consists of a 2-semester sequence beginning in the fall of the second year. The foundational pharmacokinetics course is a 3-credit course that is offered in the fall semester. Students from 2 sites, Chapel Hill and Elizabeth City, participated in the course, and all classes were video-teleconferenced synchronously.
In 2010, the 154 students enrolled in the course (143 at Chapel Hill and 11 at Elizabeth City) were randomly divided into groups of 6 by campus but balanced for gender. One faculty member served as the leader/facilitator for both campuses originating from the Chapel Hill campus. There were 5 TBL modules within the course: pharmacodynamics, single-dose pharmacokinetics, infusion and multiple-dose pharmacokinetics, violations of the 1-compartment model (ie, nonlinear behavior, multiple-compartment behavior), and physiologic concepts in pharmacokinetics (ie, renal and hepatic clearance). Each TBL module consisted of 3 phases: pre-class preparation, readiness-assurance testing, and application of concepts to patient cases.
The first phase occurred prior to the TBL session and was completed by students individually. The second and third phases occurred during the class session and involved individuals, teams, and the entire class. A fourth component of student reflection occurred before each examination and was completed by individual students.8 A group project also was incorporated, consisting of 6 clinically focused cases, the purpose of which was for students to review major concepts within the course prior to the final examination. Cases were reviewed the week prior to the final examination.
Prior to each TBL session, students were given defined objectives for the assigned study materials, which included an e-book and an interactive, online-learning object, both designed by the instructor.8 Problem sets, practice quizzes, and old examinations were made available to students but were designated for self-assessment purposes only.
The class was scheduled for two 1.5-hour sessions. For the second phase of TBL, the first 30 minutes of the 1.5-hour session were devoted to assessing students' preparation. Students first took an individual readiness-assurance test (iRAT) consisting of 10 to 15 multiple-choice items based on content from the preclass assignments. Students then completed the same assessment within their teams, ie, a group readiness-assurance test (gRAT). After the iRAT and gRAT were completed, the facilitator reviewed the answers with the class and clarified any concepts that students did not understand relating to the quiz and the precourse assignments. The first day of class within the semester, students negotiated with their instructor how much the iRAT and gRAT would contribute to their total quiz grade. Boundaries for this negotiation were that the iRAT could contribute a maximum of 60% and a minimum of 40% to the final quiz score and that the gRAT would constitute the remaining percentage. An additional stipulation was that individual students were required to achieve at least a 60% on the iRAT score in order to receive the full credit of team scores. Total quiz points from the 5 quizzes were equivalent to 1 examination. On days when the readiness assurance process was not used, the class session was considered a voluntary help session.
The third phase occurred during the second 1.5-hour session. Patient cases with 3 to 6 corresponding questions were used for students to practice applying the foundational concepts. Case questions used real medications to reinforce foundational concepts and calculations. Each question was written in multiple-choice format with 3 to 5 plausible options to provoke discussion among the team members.The faculty facilitator began by reviewing 1 case and its related question with the entire class. Then, each team considered the options and the available information and selected the best answer. All the teams worked on the same question during the 5 to 15 minutes allotted for team discussion. Teams used the precourse study materials, laptops, and any other references they chose to bring to class to assist them in the selection and defense of their response.
Each team was assigned a flag, which was placed on their desk prior to the group deliberations. Raising the team flag indicated to the facilitator that the team had finished deliberating and was ready to discuss the case. When all the flags had been raised, the faculty facilitator asked the teams to simultaneously post their respective answer cards. At that point, facilitated discussion among the groups occurred. The facilitator devoted 5 to 10 minutes for the class discussion of each question within the case. The entire process was repeated throughout the class period until all case questions were completed. Approximately 2 cases could be discussed during the allotted 90 minutes of class time.
At the end of the course, students were required to complete a peer assessment of each team member's contribution using a published instrument.9 Peers rated team members on preparation, participation, leadership, attitude, confidence, and professionalism during the TBL sessions. The students also performed an interim peer-assessment to familiarize themselves with the process and provide formative feedback to individuals.10
Student learning was assessed using a midterm and final examination, which consisted of multiple-choice questions presented in an answer-until-correct format using immediate feedback forms.11 This examination format had been used for the previous 5 years within the course. Questions were constructed to assess student level of learning according to Bloom's Taxonomy, consistent with the stated learning objectives for the course. The levels of learning were separated into 2 categories to facilitate classification of questions and were consistent with curriculum mapping efforts: level 1 = application and analysis; level 2 = creation and evaluation. This method differs from that in previous years when knowledge/comprehension level questions were on the examination rather than on quizzes.
The impact of the TBL format was assessed in several ways. The first method was to compare examination performance, end-of-semester course evaluations, and student attitudes1 with those of students who completed the course the previous year. In the previous year's format, class met once a week for 75 minutes in smaller groups of 40 to 50 students and a recitation-style approach to learning was used. Class time for the course was used for discussion, problem solving, case studies, and other types of active-learning activities. Although in previous years students were asked to prepare for class either through reading the e-book or completing the online, interactive learning object, there was no assessment of their preparation.
The second method of assessment was to examine the impact of course-format changes on the subsequent clinical pharmacokinetics course. The rationale was that an increase in clinical application training within the foundational course could impact subsequent learning, which might reveal itself in the clinical pharmacokinetics course. The format of the clinical pharmacokinetics course has been explained elsewhere.11
The third method of assessing the impact of the course format was to use previously published survey instruments to measure team learning attitudes12 and professionalism.13 Both instruments were completed before the course and after the course to examine changes over time. The university's institutional review board classified this study as exempt from review.
EVALUATION AND ASSESSMENT
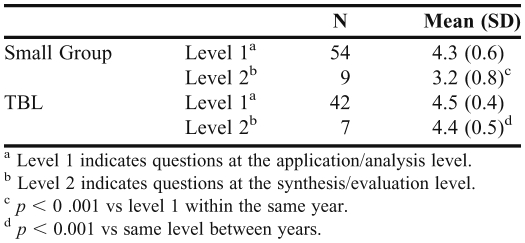
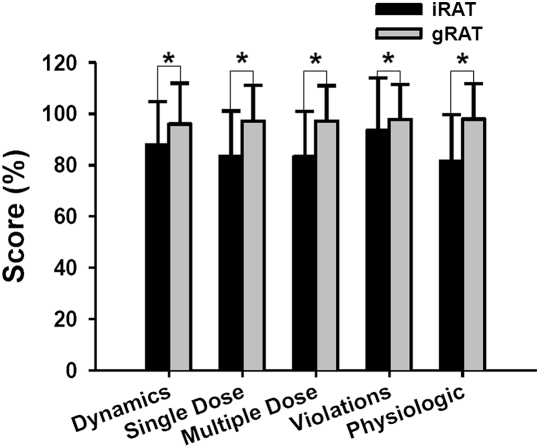
Admissions data over the study period were constant in grade-point average (3.5 / 4.0), Pharmacy College Admissions Test (PCAT) scores (top 85%), and number of students with previous degrees (68% to 73%). A retrospective comparison of examination scores was made between the prior year when the recitation-style format was used and the current TBL year. This was accomplished using a 2-way ANOVA, for course format (smaller group, recitation-style vs TBL) and level of learning (application/analysis vs evaluation/creation), with a Tukey's post-hoc comparison. The criterion for significance was set at p < 0.05. There was a class format-by-level difference (Table 1). In the smaller-group format, there were significantly lower scores at the level of synthesis/evaluation compared with application/analysis; however, the difference between the 2 levels of learning was not significant in the TBL year. A paired t test was used to compare quiz scores from the individual and team quizzes from the readiness-assessment process (Figure 1). There was significant improvement in the team scores for each module. The iRAT scores averaged over 80% for any given module (median 83%, average 86%, range 82%- 94%), whereas the gRAT scores averaged over 95% for any given module (median 97%, mean 97%, range 96%-98%)
Table 1.
Comparison of Examination Scores Between the Team-Based Learning Year and the Previous Year's Small-Group Format
Figure 1.
Comparison of individual and team quizzes from the readiness-assessment process. Data presented as mean and standard deviations. Abbreviations: iRAT = individual quiz; gRAT = team quiz. * p < 0.001.
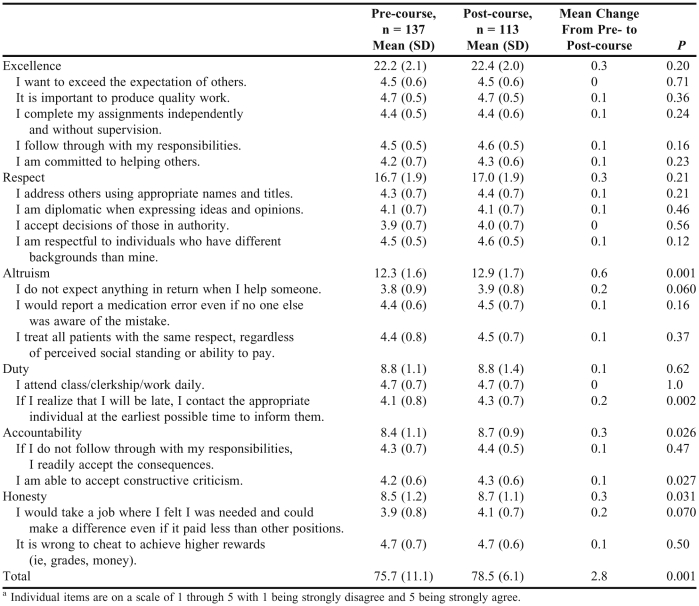
During the TBL year, professionalism was assessed using a survey instrument. Data were analyzed using a paired t test based on a pre- and post-course for individual items on the survey tool in the categories of excellence, respect, altruism, duty, accountability, and honesty (Table 2). Aggregate scores for each of the categories are also listed in Table 2. These scores were calculated by summing the individual items in each category. There was a significant increase in overall professionalism score and the mean scores on the subscales for altruism, duty, and honesty. Although there was no mean change in the accountability subscale, there was a significant improvement in students’ feelings toward accepting constructive criticism.
Table 2.
Changes in Attitudes Toward Various Aspects of Professionalisma
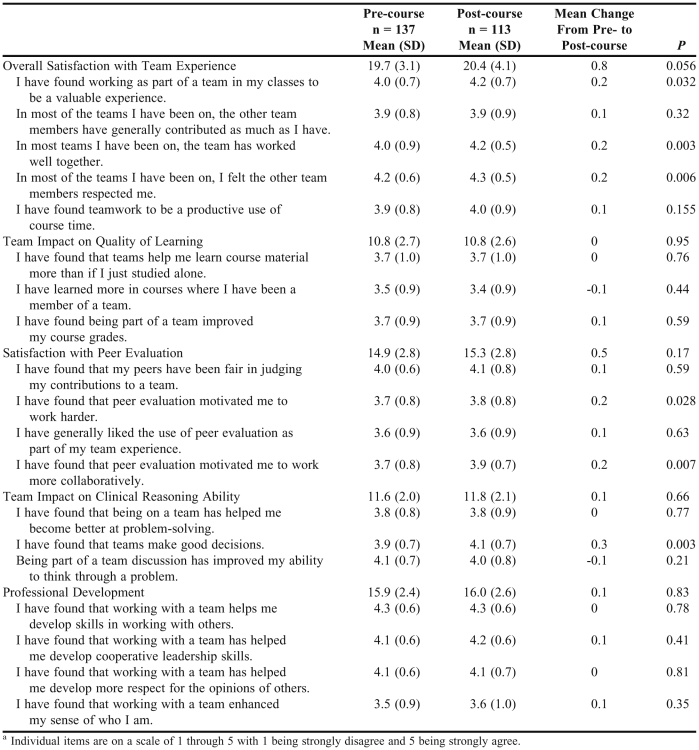
Data were analyzed using a paired t test based on a pre- and post-course survey instrument for mean scores and individual items on the survey tool in the categories of overall satisfaction with team experience, team impact on quality of learning, satisfaction with peer evaluation, team impact on clinical reasoning ability, and professional development (Table 3). Aggregate scores were calculated by averaging the means for the individual items in each category. There were no significant changes in attitudes in any category, although overall satisfaction with team experience was nearly significant (p = 0.056). Within overall satisfaction with the team experience, there were significant improvements in feelings toward working as part of team being a valuable experience, team members working well together, and mutual respect among team members. In the subscale of satisfaction with peer evaluation, there were significant improvements in students’ attitudes regarding the role of peer evaluation in motivating students to work harder and more collaboratively. Finally, there was a significant improvement in the attitude that teams make good decisions within the team impact-on-clinical-reasoning subscale.
Table 3.
Changes in Attitudes Toward Various Aspects of Team Learninga
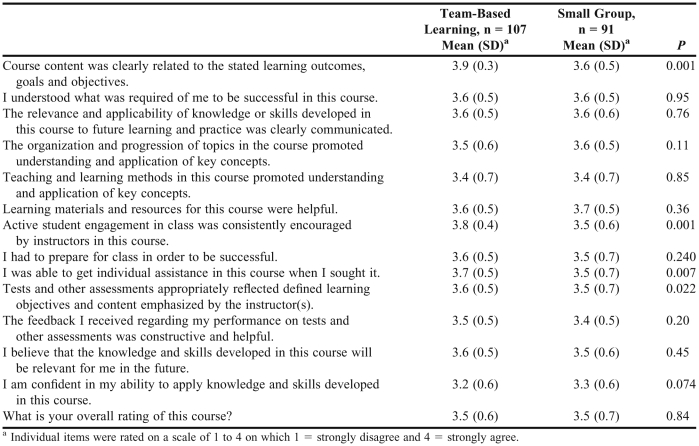
End-of-semester attitudinal survey instruments were used to collect information on student perceptions of the course and the learning experience. Mean responses were compared between the TBL year and smaller-group year using a t test with 1 indicating strong disagreement, 3 indicating neutral, and 5 indicating strong agreement. During the TBL year, 74% of students favored the e-book as a resource for class preparation compared with12% who favored the online learning object; the remaining 14% of students indicated no preference. The mean score during the TBL year was not significantly different from the smaller-group year, during which 62% preferred the e-book, 19% preferred the Web-based material, and 19% were neutral.
Approximately 81% of the students in the TBL format felt it was necessary to attend class to understand the material, 12% disagreed, and 7% were neutral. The mean score was significantly higher compared with the smaller-group format, in which 37% of students felt coming to class was necessary, 30% disagreed, and 33% were neutral (p < 0.001). Twenty-eight percent of students agreed that they missed out on instructor contact because of the TBL format, 54% disagreed, and 18% were neutral. The mean score was significantly larger than that of the previous year when 20% agreed, 66% disagreed, and 14% were neutral (p = 0.013), suggesting that students in the TBL year felt they missed out on instructor contact time more than with the previous format. When asked if they felt they missed out on learning, 26% agreed, 55% disagreed, and 18% were neutral. The mean score was significantly higher than in the previous year when 17% agreed, 67% disagreed, and 16% were neutral (p = 0.005), suggesting that students in the TBL year felt that they missed out on some learning compared with that of the previous format. Forty-eight percent of students agreed that the TBL format was better than a traditional lecture, 35% were neutral, and 18% disagreed. These responses were not different from those from the year of the smaller-group format, when 70% agreed, 21% were neutral, and 9% disagreed.
Approximately 45% of students felt they did not spend any more or less time preparing for this class than for other classes, although 30% felt they spent more time preparing for this particular course. These responses were not different from those of the previous year, when 41% of students felt they did not spend more or less time compared with that for other classes while 40% felt they spent more time.
End-of-semester course evaluations were used to compare information on student perceptions of the course and the learning experience. Students’ responses were compared between the TBL year and smaller group year using a t test. When examining end-of-semester course evaluations between the TBL year and the previous year, there were significant improvements in feelings that course content was related to course objectives, active student engagement was encouraged, assessments were aligned with course objectives, and students were able to get individual assistance when needed (Table 4).
Table 4.
Comparison of End-of-the-Semester Course Evaluations for the Team-Based Learning Format and the Previous Year's Smaller-Group Format
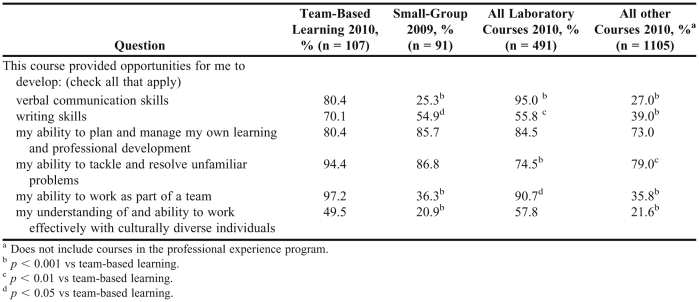
As learning goes beyond content knowledge, opportunities for development of other relevant skills were compared between the TBL format, other courses within the current year, and the previous version of the course (Table 5). Students checked all skills that applied within the end-of-year course evaluations, and the proportion of responses was compared. Students felt that the TBL format provided more opportunities for the development of verbal communication skills than did lecture-based courses and the previous year's course but that the pharmaceutical care laboratory provided more opportunities than did the TBL course. The TBL format provided more opportunities for developing writing skills and working as part of a team compared with the small-group format, other courses, and pharmaceutical care laboratory. The former course format and other didactic courses within the year provided fewer opportunities to develop skills to work with diverse populations The current course format provided more opportunities to develop the ability to tackle problems than did other courses within the year and pharmaceutical care laboratory but not when compared with the previous year's course. There were no differences between course formats with respect to students’ ability to plan and manage their own work.
Table 5.
Comparison of Course Formats on Providing Opportunities to Develop Various Skills
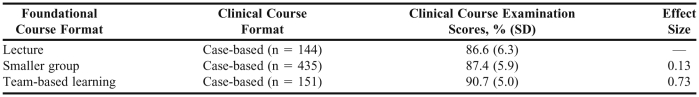
One purpose of using the smaller group format in prior years and the TBL format during the current year was to help with clinical applicability of material. By increasing the clinical applicability, there would be an increase in the level of meaningfulness to the student, leading to increases in long-term retention. The impact of these formats on transfer (ie, performance in the subsequent, clinical pharmacokinetics course) was investigated using examination grades as the primary metric. The effect size for lecture, the smaller-group format, and the current TBL format that was used in the foundational course can be found in Table 6. The effect size of the smaller-group format was small (d = 0.13) when compared to when lecture was used in the foundational course. The effect size of the TBL format was moderately large (d = 0.73) when compared with that of the lecture format, indicating that the TBL format had some effect on performance in the later, clinically applied pharmacokinetics courses. An alternative analysis was conducted using regression and taking into account baseline performance within the foundational course. Using this approach, the small-group standardized coefficient was 0.20 and the TBL standardized coefficient was 0.39, suggesting that the TBL format had a greater impact on examination performance in the clinical pharmacokinetics course than in the smaller-group or lecture format.
Table 6.
Impact of Foundational Course Format on Examinations Scores in the Clinical Course
DISCUSSION
The ability to develop both factual knowledge and higher-order skills that will assist students in the workforce are 2 important aspects to balance within a curriculum and individual courses. Large enrollment courses often dissuade instructors from addressing the higher-order skills and focus more on the transmission of factual information; however, use of smaller, recitation-type sessions within a large enrollment pharmacokinetics course can be used to enhance the focus on higher-order skills.1 This article reports on using a TBL format to elicit a similar effect.
According to the examination performance, the TBL format resulted in learning that was similar to that in a smaller-group format. The 1 advantage of TBL over the smaller-group format is efficiency. TBL can use the entire class at 1 time compared with the smaller-group format, which requires multiple sections, often taught by the same instructor. Although there is some evidence that TBL resulted in students performing better on examination questions focused at higher levels of learning (eg, synthesis and evaluation), it is difficult to draw firm conclusions from the data based on the relatively small sample sizes for these types of questions. However, students had comparable performance on application/analysis type questions. Some students noted in course evaluations that smaller group recitations may have been helpful when dealing with mathematical problems. Overall, the performance enhancement is consistent with that in a study by Koles and colleagues14 who found that students involved in TBL demonstrated a greater extent of content mastery than did other instructional approaches. Within the preparatory quizzes, the individual quiz score averaged above 80%, indicating that students were able to read and acquire foundational information on their own.
One goal of a change in instructional strategy is to better prepare students for future learning. This prospective view was investigated by auditing examination scores on the subsequent clinical pharmacokinetics course. This study found a moderate effect size of the TBL format on subsequent performance, which is comparable to the effect size in knowledge acquisition with other instructional interventions, such as self-directed learning (range -1.6 to 3.8, average 0.45),15 providing feedback (range 0.14 to 1.10, average 0.79)16 and reciprocal teaching (eg, collaborative or cooperative learning) (range 0.86 to 0.88, median 0.88).17These findings seem logical, as the framework of TBL incorporates self-directed learning, feedback, and cooperative learning. Further work would be needed to examine the consistency of the effect year to year and the duration of the effect (ie, whether the effect impacted performance on experiential training).
The National Association of Colleges and Employers found that skills such as analytical thinking, teamwork, work ethic, and communication are important for the job market. Course evaluations found that the TBL format provided more opportunities for teamwork compared with the small-group format and other large-enrollment courses during the semester and the pharmaceutical care laboratory. Similar results were found for writing skills, although the pharmaceutical care laboratory was the only course format that provided more opportunities for verbal communication skills. However, TBL did provide more writing opportunities than did the small-group format used in previous years of the course and other large-enrollment courses that are more lecture-based. There is evidence that students reported working harder based on the motivational effects of peer evaluation.
With the TBL format, measures of student professionalism significantly improved over the course of the semester, consistent with the findings of Beatty and colleagues.18 In this and the aforementioned studies, initial scores indicated that students perceived teamwork and professionalism skills as strong prior to the introduction of TBL. In both situations, significant educational change may not have occurred because of high initial scores. While there was statistical change, attributing these changes to a single course within a curriculum is problematic and the results should be interpreted with caution.
When using the TBL format, medical students showed significant improvements in attitudes toward satisfaction with peer evaluation and professional development from their first to their second year. This study did not find any significant changes over the semester. These differences may be attributable to the time scale (ie, 1 year vs 1 semester) or the amount of TBL in the medical curriculum vs the 1 course during the semester, as in the current study. Regardless, even though the major categories did not show changes, some of the individual questions showed significant changes.
There were other attitudinal differences between the TBL format and the smaller-group format used the prior year. Most notably, students in the TBL felt they missed out on learning to a greater extent compared with the smaller-group format cohort. This may be related to the perception of learning. Abrantes and colleagues19 found that factors of course organization, student-instructor interaction, instructor responsiveness, and instructor likeability all positively impact perceived learning. According to the course evaluations, there was no difference in attitudes toward course organization or the instructor's approachability between the current and previous year's courses. There was an improvement in attitudes in that students could get more individual assistance in the TBL format. Students felt they missed out less on instructor interaction during the smaller-group format than during the TBL year. Given that student-instructor interaction plays a smaller relative role in the perception of learning than does instructor responsiveness,19 it is surprising that students felt they missed out on learning. This lower extent of perceived learning may better relate to the intellectual development of students and the role peers play in the learning process. According to constructs by Perry and Baxter Magolda, students on one side of the continuum favor instructors as the experts, while on the other side of the continuum, they accept peers as experts in their own right.20,21 Given that TBL relies heavily on peer-instruction, some individuals may feel they are not getting adequate learning experiences.
As this was the inaugural year for this format, some changes were made during the semester. Teams were initially given a single copy of cases. During the course of the semester, students asked for additional copies. There was a perception by the instructor that this accommodation negatively impacted the team discussion because students started to work more individually or in pairs rather than as part of their 6-member team. During the next iteration, a single copy will be provided. This sharing of resources is an important part of the team process, as it increases the proximity of team members and forces more interaction.22 For the first 3 modules, calculations were included in the patient cases. Student feedback midsemester suggested there was large variability in the time allowed to complete the calculations within the group, which led to some level of frustration. During the day on which the readiness assurance process was complete, students requested that they be provided with a calculations overview and that the cases be more conceptual in nature. These changes were implemented during the semester and will be used during the next iteration.
The limitation to this report is that not all aspects of the course assessment, such as professionalism, could be compared with those of other courses or previous formats of the course. Also, the survey tools used may not be sensitive to changes that occur over 1 semester, and although the results of the survey instruments may be influenced by a single course, they may better reflect input from multiple courses. Examination questions were used as one metric of impact. The smaller number of questions at the synthesis/evaluation level and potential differences in item difficulty are limitations related to grades.
CONCLUSIONS
This study demonstrated that a mathematically based discipline, such as pharmacokinetics, in a large-enrollment course with multiple campuses synchronously video-teleconferenced, can be adapted to the TBL format. Students can successfully acquire course content outside of class and be held accountable for that acquisition through the readiness-assurance process. Class time could then be used to help develop the conceptual and calculation aspects of the discipline. In some cases, the breadth and depth of learning or skills were enhanced in that the format allowed for more examples or discussion of clinical application. Student performance on examinations indicates some improvement in scores, despite examinations being focused on higher orders of learning (eg, application, analysis, etc). Additionally, there is some indication that performance in latter coursework related to pharmacokinetics is enhanced. Finally, there was also evidence of an increase in favorable attitudes in areas of professionalism and teamwork. Further work is required to refine in-class cases and development of other, non-content skills such as problem solving.
ACKNOWLEDGEMENT
The author thanks Wendy Cox for her input during the preparation of this manuscript.
REFERENCES
- 1.Persky AM, Pollack GM. Transforming a large-class lecture course to a smaller-group interactive course. Am J Pharm Educ. 2010;74(9):Article 170. doi: 10.5688/aj7409170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zull JE. The art of changing the brain: enriching teaching by exploring the biology of learning. 1st ed. Sterling, VA: Stylus Publishing; 2002. [Google Scholar]
- 3.Parmelee DX, Michaelsen LK. Twelve tips for doing effective team-based learning (TBL) Med Teach. 2010;32(2):118–122. doi: 10.3109/01421590903548562. [DOI] [PubMed] [Google Scholar]
- 4.Ambrose SA. How Learning Works: Seven Research-Based Principles for Smart Teaching. 1st ed. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 5.Pascarella ET, Terenzini PT. How College Affects Students: Findings and Insights From Twenty Years of Research. 1st ed. San Francisco: Jossey-Bass Publishers; 1991. [Google Scholar]
- 6.NACE. Job Outlook 2011 Spring Update. Bethlehem: National Association of Colleges and Employers; 2011. [Google Scholar]
- 7.Blouin RA, Riffee WH, Robinson ET, et al. Roles of innovation in education delivery. Am J Pharm Educ. 2009;73(8):Article 154. doi: 10.5688/aj7308154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Persky AM. Multi-faceted approach to improve learning in pharmacokinetics. Am J Pharm Educ. 2008;72(2):Article 36. doi: 10.5688/aj720236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Michaelsen LK. Team-based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning. 1st ed. Sterling, VA: Stylus; 2008. [Google Scholar]
- 10.Sweet M, Pelton-Sweet LM. The social foundation of team-based learning: students accountable to students. New Directions for Teaching and Learning. 2008;2008(116):29–40. [Google Scholar]
- 11.Dupuis RE, Persky AM. Use of case-based learning in a clinical pharmacokinetics course. Am J Pharm Educ. 2008;72(2):Article 29. doi: 10.5688/aj720229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parmelee DX, DeStephen D, Borges NJ. Medical students' attitudes about team-based learning in a pre-clinical curriculum. Med Educ Online. 2009;14:1. doi: 10.3885/meo.2009.Res00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chisholm MA, Cobb H, Duke L, McDuffie C, Kennedy WK. Development of an instrument to measure professionalism. Am J Pharm Educ. 2006;70(4):Article 85. doi: 10.5688/aj700485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koles PG, Stolfi A, Borges NJ, Nelson S, Parmelee DX. The impact of team-based learning on medical students' academic performance. Acad Med. 2010;85(11):1739–17345. doi: 10.1097/ACM.0b013e3181f52bed. [DOI] [PubMed] [Google Scholar]
- 15.Murad MH, Coto-Yglesias F, Varkey P, Prokop LJ, Murad AL. The effectiveness of self-directed learning in health professions education: a systematic review. Med Educ. 2010;44(11):1057–1068. doi: 10.1111/j.1365-2923.2010.03750.x. [DOI] [PubMed] [Google Scholar]
- 16.Hattie J, Timperley H. The power of feedback. Rev Educ Res. 2007;77(1):81–112. [Google Scholar]
- 17.Rosenshine B, Meister C. Reciprocal teaching: a review of the research. Rev Educ Res. 1994;64(4):479–530. [Google Scholar]
- 18.Beatty SJ, Kelley KA, Metzger AH, Bellebaum KL, McAuley JW. Team-based learning in therapeutics workshop sessions. Am J Pharm Educ. 2009;73(6):Article 100. doi: 10.5688/aj7306100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abrantes J, Seabra C, Lages L. Pedagogical affect, student interest, and learning performance. J Bus Res. 2007;60(9):960–964. [Google Scholar]
- 20.Baxter Magolda MB. Knowing and Reasoning in College: Gender-Related Patterns in Students' Intellectual Development. 1st ed. San Francisco: Jossey-Bass; 1992. [Google Scholar]
- 21.Perry WG Harvard University. Forms of Intellectual and Ethical Development in the College Years: a scheme. New York: Holt; 1970. Bureau of Study Counsel. [Google Scholar]
- 22.Michaelsen LK, Knight AB, Fink LD. Team-based Learning: a Transformative Use of Small Groups. Westport, CT: Praeger; 2002. [Google Scholar]