Abstract
Objectives. To introduce a multiple-instructor, team-based, active-learning exercise to promote the integration of basic sciences (pathophysiology, pharmacology, and medicinal chemistry) and clinical sciences in a doctor of pharmacy curriculum.
Design. A team-based learning activity that involved pre-class reading assignments, individual-and team-answered multiple-choice questions, and evaluation and discussion of a clinical case, was designed, implemented, and moderated by 3 faculty members from the pharmaceutical sciences and pharmacy practice departments.
Assessment. Student performance was assessed using a multiple-choice examination, an individual readiness assurance test (IRAT), a team readiness assurance test (TRAT), and a subjective, objective, assessment, and plan (SOAP) note. Student attitudes were assessed using a pre- and post-exercise survey instrument. Students’ understanding of possible correct treatment strategies for depression improved. Students were appreciative of this true integration of basic sciences knowledge in a pharmacotherapy course and to have faculty members from both disciplines present to answer questions. Mean student score on the on depression module for the examination was 80.4%, indicating mastery of the content.
Conclusions. An exercise led by multiple instructors improved student perceptions of the importance of team-based teaching. Integrated teaching and learning may be achieved when instructors from multiple disciplines work together in the classroom using proven team-based, active-learning exercises.
Keywords: team-based learning, depression, team teaching, active learning, pharmacotherapy
INTRODUCTION
The revised Accreditation Council for Pharmacy Education (ACPE) standards place greater emphasis on the scientific foundation of practice competencies and their assessment. Specifically, ACPE standards 10 and 11 recommend integration of the curricular content and coordinated instruction across disciplines using appropriate assessment techniques, active-learning strategies, and other pedagogical approaches that enable students to transition from dependent to self-directed, lifelong learners.1 Active-learning techniques are also recommended by ACPE to help students achieve desired learning outcomes. As a result, curriculum committees in many pharmacy colleges and schools are implementing programs that integrate basic sciences (such as physiology, pharmacology, and medicinal chemistry) with pharmacotherapy to better deliver program outcomes. Various active-learning strategies have been developed that are useful for mastering material in an integrated manner.5
The concept of integration has been emphasized in pharmacy education for more than a decade.2 The benefits of integration have been recognized by pharmacy educators who have used various strategies to adapt their teaching to this approach.3,4 Because the range of sciences that are relevant to pharmacotherapy are diverse, we hypothesized that integrated teaching and learning in pharmaceutical education could be best accomplished when individuals with expertise in specific disciplines worked together in the classroom at the same time.
At Texas A & M Health Science Center, Rangel College of Pharmacy, all the pharmacotherapy courses are delivered in a format that integrates pathophysiology, pharmacology, medicinal chemistry, and pharmacotherapy content. These courses are taught in the second and third years of the PharmD curriculum. Two 2-credit hour integrated medicinal chemistry and pharmacology courses are taught in the first year. These preliminary courses cover functional groups and pharmacokinetic and pharmacodynamic principles, as well as adrenergic and cholinergic drugs. An introductory 4-credit-hour human physiology course is also required in the first year. Despite the adoption of an integrated curricular model, we have observed that basic sciences content has not been effectively used or appreciated by the pharmacy students when making clinical decisions. In order to more explicitly demonstrate the close integration of basic and clinical sciences in patient care, we designed the current study to involve faculty members from multiple disciplines in a single lesson that used active-learning exercises and emphasized the use of basic sciences knowledge in making effective clinical decisions.
The objective of this study was to effectively integrate basic sciences (physiology, pharmacology, and medicinal chemistry) with clinical sciences in a pharmacotherapy laboratory course using a multi-disciplinary, team-based, active-learning exercise. The desired outcome of this approach was to demonstrate the value of basic science concepts in making strategic and logical clinical decisions. In this paper we describe the implementation of a team-based teaching and learning exercise in a laboratory session of an integrated pharmacotherapy course in the subject area of depression in order to promote integration of basic sciences concepts with clinical sciences and to provide a platform to discuss multiple solutions for the same case, thereby achieving a higher level of learning. As team-facilitated content integration and active learning are 2 approaches that are central to the current pharmacy education culture, we also sought to determine whether the exercise altered student attitudes about the importance of these approaches to teaching and learning.
DESIGN
The project described here was exempted by the Texas A&M University Internal Review Board. The exercise was carried out in the Integrated Pharmacotherapy Rounds and Recitations course, which is a laboratory component of the Integrated Pharmacotherapy course. Pharmacotherapy laboratory courses are used to demonstrate the concepts learned in the integrated classroom lecture-based courses. The exercise used individual- and team-based active-learning activities that were based on techniques suggested at the 2010 AACP Active-Learning Institute.6 Team-based learning is an effective method of active learning that has been extensively used in medical education7-10 and is increasingly used in pharmacy education.11,12 Our team-based learning and teaching approach required individual and group accountability and was purposefully structured to guide student awareness of the relevance of basic science principles to clinical decision-making. The instructors used pre-assigned groups of 5 to 7 students for the team-based activities. Individual accountability for assigned reading outside of the class was tested by a two-part readiness assurance test (RAT) which consisted of an individual quiz comprised of 10 multiple-choice questions and a team readiness assurance test (TRAT) that required team members to work collaboratively to answer questions for a team grade. The RAT emphasized basic sciences concepts relevant to the clinical case, which was subsequently presented during the laboratory session. After the IRAT and TRAT were completed, the basic science and clinical faculty members discussed the quiz questions with the class and explained the clinical usefulness of the concepts covered. A clinical case was then presented, and the students worked in groups to construct an appropriate clinical assessment and treatment plan, which was submitted for a team grade. The clinical case was then discussed by the entire class, with the clinical and basic science instructors facilitating discussion, providing appropriate explanations, and emphasizing the multitude of possible diagnoses and treatment plans. At the end of the laboratory session, students were asked to evaluate their team members on their participation in group discussions.
The Integrated Pharmacotherapy course on psychiatry and addiction is the fifth course in a sequence of 8 integrated pharmacotherapy courses in the Pharm D curriculum. Integrated Pharmacotherapy Rounds and Recitations (PHAR 814) is a complementary course that allows for demonstration and application of the concepts learned in the more lecture-based Integrated Pharmacotherapy course (PHAR 810). In these courses, basic sciences (consisting of the disciplines pathophysiology, pharmacology, and medicinal chemistry) are presented in conjunction with therapeutics, and each science discipline is taught by a faculty member trained in a specific discipline. The college defines mastery as students achieving 70% or higher confidence or examination scores on the learning objectives provided.
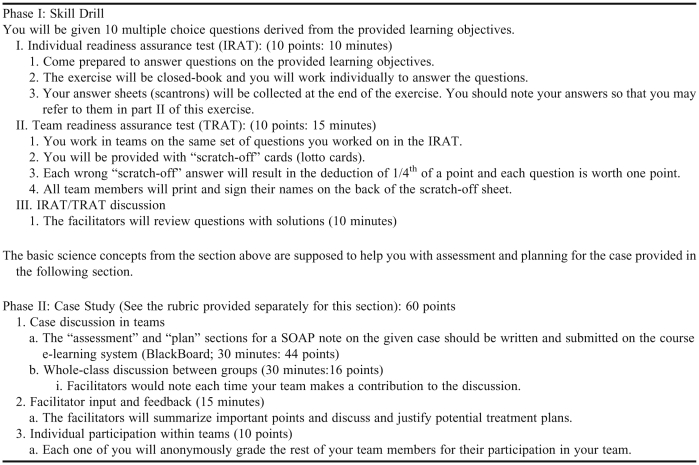
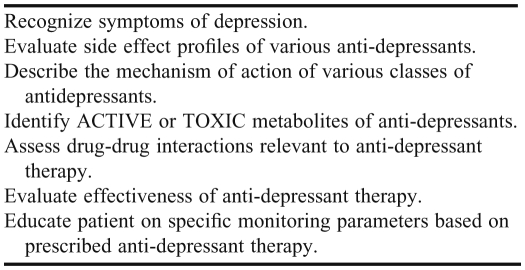
During their first year in the pharmacy program, students are assigned to teams of 5 to 7 students by the school for team-based learning activities. Students remain in the same teams throughout the first 3 years of the program. Integrated Pharmacotherapy V is a 3 credit-hour course delivered in the fall semester in the third year of the 4-year program. We used team-based learning methods to promote the integration of basic sciences knowledge with pharmacotherapy during a PHAR 814 laboratory session on depression. Ninety-one students (14 teams) participated in this exercise. The depression module of PHAR 810 was taught by 3 basic sciences faculty members (a pathophysiologist, a pharmacologist, and a medicinal chemist) and 1 clinical practitioner. During the integrated team-based active learning exercise for PHAR 814, a pharmacologist, medicinal chemist, and clinical practitioner conducted the session together as a team. One week prior to the laboratory session, the students were provided instructions on how the laboratory would be conducted (Table 1), and the students were instructed to come to the laboratory session having mastered the objectives presented in Table 2 .The assigned reading included lecture presentation slides and textbook chapters covering the pathophysiology, pharmacology, medicinal chemistry, and therapeutics of depression.
Table 1.
Instructions for Students on Rounds and Recitations (Laboratory Session) on the Topic of Depression
Table 2.
Objectives to Master Provided to Students Prior to the Team-based Learning Exercise
During phase I of the exercise, students were tested on the pre-assigned material using an IRAT and TRAT. The IRAT had 10 multiple-choice questions which the students answered independently. Students next worked on the same questions in teams (TRAT). For the TRAT portion, each team was given a “lotto” or “scratch-off card.” Using these cards, the team could “scratch-off” choices in sequence until they were able to scratch off the choice that was marked as the correct answer. Each incorrect choice that was scratched off resulted in the deduction of one-fourth of the question's points. Only basic sciences content was tested on the RATs; however, the questions in the RATs were written by basic sciences faculty members in consultation with the clinical faculty member to ensure that the questions were relevant to the concepts required in the assessment and treatment plan components of the clinical case. After the IRAT and TRAT were completed, all 3 faculty members discussed the questions with the students.
During phase 2 of the exercise, students were given a clinical case and instructed to work in their teams to discuss and write-up the assessment and planning portions of a subjective, objective, assessment, and plan (SOAP) note. The SOAP notes were submitted via the Internet to the Blackboard e-learning system. Assessing the case required application of basic sciences concepts that were covered in phase 1 of the activity. There were several potentially correct clinical strategies that could be used to treat the patient presented in the case. After the teams had submitted their clinical analyses and treatment plan, the case was opened up for full class discussion among all groups. All 3 instructors moderated the large group discussion, which was intended to encourage active participation and facilitate critical thinking among students. Students were given team participation points based on the frequency with which their team contributed to the discussion.
Following the class discussion, the clinical faculty member summarized the discussion points and provided preferred answers with justification. At the end of the activity, students within each team were asked to evaluate their fellow team members’ participation and involvement in the team-based exercise.
EVALUATION AND ASSESSMENT
Ninety-one students participated in the exercise. Mastery of the learning objectives was assessed through multiple-choice questions during the IRAT and TRAT sessions. These questions were prepared by the basic science instructors in consultation with the pharmacy practice faculty member and designed to emphasize concepts that would be useful in assessing the clinical case and designing an appropriate treatment plan. In addition, a subjective evaluation of the assessment and plan portions of the SOAP note was conducted by the clinical instructor using a grading rubric (available from the author by request) (Table 4). Each student's overall grade for the laboratory session was calculated from the following individual scoring components: IRAT, 10%; TRAT, 10%; the subjective evaluation of the assessment and plan portions of the SOAP note, 60%; the team participation grade derived from peer evaluation, 10%; and a grade for each team's participation in the full class discussion as evaluated by the faculty, 10%. The average score on the laboratory exercise was 77.2 ± 1.0%, indicating that students mastered the desired learning outcomes (Table 2) at the level set and expected by the school.
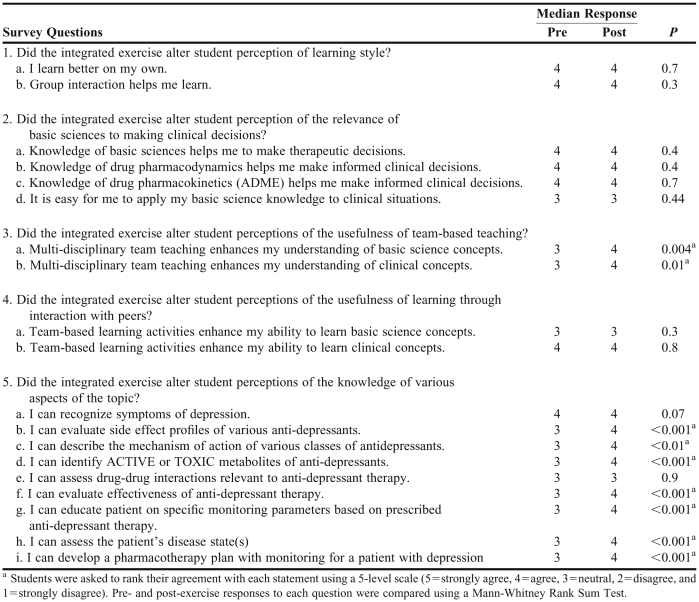
Students were also given pre- and post-exercise survey instruments to self-assess their mastery of the exercise's objectives, the relevance of basic sciences to making sound clinical decisions, and the usefulness of team-based teaching and learning techniques. The survey was administered using Blackboard. Eighty of the 91 students completed the survey instruments. In the post-exercise survey, 68% of the students agreed or strongly agreed that the IRAT/TRAT contributed to their ability to perform better during the SOAP note component of the exercise, and 66% agreed or strongly agreed that the team-based learning exercise helped them perform better on the end-of-module multiple-choice examination. Forty-four percent of students indicated that the full class SOAP notes discussion was the most beneficial portion of the exercise. A detailed comparison of pre- and post-survey responses is presented in Table 3. The topics addressed in the survey related to student perceptions of learning styles, importance of basic sciences to making clinical decisions, the benefit of team-based teaching, the educational value of team-based learning, and student perceptions of their mastery of the laboratory exercise's learning objectives. The survey tools demonstrated that students perceived that they benefited from the team-based teaching and that they had mastered the learning outcomes listed in Table 2.
Table 3.
Third-Year Pharmacy Students’ Responses to a Survey Regarding a Team-based Learning Exercise
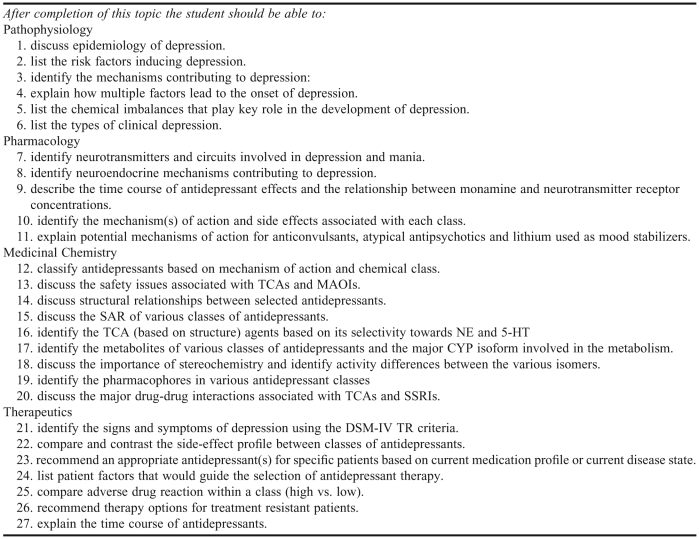
Student performance in the end-of-module multiple-choice examination on mental depression was also evaluated. The average examination score was 80.4 ± 1.7%, which indicated that mastery of the desired learning outcomes for the complete module on depression (Appendix 1) was attained.
DISCUSSION
We designed and implemented an integrated, team-based teaching and active-learning exercise with the objective of enhancing student awareness of the relevance of basic sciences concepts in making meaningful clinical decisions and the value of team-based teaching and team-based active-learning techniques. In the past, we had perceived that students did not appreciate the relevance or use their knowledge of basic sciences when making clinical decisions. We hypothesized that by directly demonstrating the connection between basic science concepts and clinical decision-making through the mechanisms described in this manuscript, students would better appreciate their interdependence and more willingly apply concepts of basic sciences when designing patient care plans. Although the pre- and post-exercise survey data did not show any change in student attitudes relative to the application of basic sciences concepts to making appropriate clinical decisions, they did confirm that students believe basic sciences concepts are important in making clinical decisions.
The majority of students (68%) felt that this team-based learning exercise positively contributed to their learning and provided better understanding and application of the material learned in an integrated classroom course. According to the post-exercise survey results on content mastery, students thought the team-based learning approach helped them achieve the desired learning outcomes for the exercise (Table 2). Moreover, the students scored an average of 80% on the end-of-module, multiple-choice examination, indicating that they achieved mastery of the comprehensive module objectives (Appendix 1). Together, these observations indicate that this type of exercise is effective for promoting mastery of the desired laboratory learning outcomes, and may contribute to mastery of the comprehensive module objectives. A weakness of the study is that we did not have a control group of students who did not receive exposure to this laboratory exercise. Such a control group is difficult to implement in an educational setting because students in the control group might feel disadvantaged.
One of the most significant findings of this report is that the exercise significantly improved student opinion of the effectiveness of team-based teaching. In our integrated course sequence, each disease state has typically been addressed in a discipline-specific manner. In other words, a student studying depression receives separate lectures on the pathophysiology, pharmacology, medicinal chemistry, and therapeutics of depression. While the juxtaposition of the approaches of each of these disciplines to the topic is a form of integration, we conducted this study to see whether, when instructors from multiple disciplines worked together on a single exercise, student perceptions of the usefulness of team based-instruction to their learning improved. The comparison of scores on the pre- and post-exercise attitude survey indicated that these students, who had already been receiving instruction that faculty considered integrated, saw the benefit of team-based teaching after participating in the exercise described. This finding indicates that there are still opportunities for improving the integrated nature of our curriculum and instruction.
Several students mentioned on the survey tools that contradictions occur when instructors from individual disciplines present content independently. Obviously, it would be impossible for all instructors to agree at all times, as there are often multiple appropriate treatment plans for the same patient, and this is important for the students to learn. However, if the instructors are in the classroom at the same time, the merits of various therapeutic approaches and the scientific rationale that supports them can be discussed with the students. This realization that there can be more than one right answer should strengthen the students’ ability to make sound patient care decisions, particularly in an interdisciplinary team environment where multiple perspectives must be taken into account.
Interestingly, the exercise did not alter student perceptions of the usefulness of interaction with peers in the learning process. The active-learning activities used in this exercise were team-based in nature. As we described earlier, students in our instructional program are assigned to a team beginning in their first year and they work together with these students throughout their tenure at the college. Because of these fixed and frequently used teams, students probably develop strong opinions about the usefulness of team-based, active-learning exercises. Assigning students with different skill sets to each team and assigning student roles within the team may prove useful for our instructional purposes.
The students felt that the class discussion of the clinical case (SOAP note) was the most beneficial component of the exercise. This suggests that it was really the interaction between the students and the instructors that was most beneficial to learning. The faculty members felt the discussion was engaging, and it was rewarding to see how students were able to discuss the various potential therapeutic plans with their classmates and to realize that several possible treatment plans existed for the same patient. When faculty members summarized the discussion with all possible answers to the case, it helped the students apply concepts learned in the classroom. It may not be enough to have the students work together in teams; they may benefit optimally from having an instructor guide the teamwork.
SUMMARY
Three instructors from different disciplines (physiology/pharmacology, medicinal chemistry, and clinical pharmacy) designed an exercise that consisted of individual- and team-answered multiple-choice questions, team-based development of the assessment and plan portions of a SOAP note on a clinical case on depression, and group discussions moderated by all of the instructors. The evaluation of the exercise indicated that students found the multiple-instructor moderated, team-based, active-learning exercise to be beneficial to their learning, and had mastered the desired learning outcomes at the level expected by the college. Most importantly, the exercise improved student appreciation for team-based teaching using instructors from multiple disciplines.
ACKOWLEDGEMENT
The authors thank Dr. Victoria F. Roche, Senior Associate Dean, School of Pharmacy and Health Professions, Creighton University, Omaha, NE, for expert editing in revising this manuscript.
Appendix 1. Depression Module in PHAR 810 Course Learning Objectives
REFERENCES
- 1.ACPE accreditation standards. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed January 18, 2012.
- 2.Stull R, Carter RA. Integrating the pharmacy curriculum: more to consider than improving learning. Am J Pharm Educ. 2002;66(4):407–410. [Google Scholar]
- 3.Conway S, Johnson J, Ripley T. Integration of team based learning strategies into cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ives T, Deloatch K, Ishaq K. Integration of medicinal chemistry and pharmacotherapeutics courses: a case-based, learner-centered approach. Am J Pharm Educ. 1998;62(4):406–411. [Google Scholar]
- 5.Stewart D, Brown S, Clavier C, Wyatt J. Active-learning processes used in US pharmacy education. Am J Pharm Educ. 2011;75(2):Article 68. doi: 10.5688/ajpe75468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AACP Institute on Active Learning and Pedagogical Change, Lansdowne, Virginia, May 24-26, 2010. http://www.aacp.org/meetingsandevents/othermeetings/2010Institute/Documents/Designing%20and%20Facilitating%20and%20Active%20Learning%20-%20Medina.pdf. Accessed January 18, 2012.
- 7.Parmelee DX, Michaelsen LK. Twelve tips for doing effective team-based learning (TBL) Med Teach. 2010;32(2):118–122. doi: 10.3109/01421590903548562. [DOI] [PubMed] [Google Scholar]
- 8.Parmelee DX. Team-based learning: moving forward in curriculum innovation: a commentary. Med Teach. 2010;32(2):105–107. doi: 10.3109/01421590903548554. [DOI] [PubMed] [Google Scholar]
- 9.Haidet P, Fecile ML. Team-based learning: a promising strategy to foster active learning in cancer education. J Cancer Educ. 2006;21(3):125–128. doi: 10.1207/s15430154jce2103_6. [DOI] [PubMed] [Google Scholar]
- 10.Rider EA, Brashers V. Team-based learning: a strategy for interprofessional collaboration. Med Educ. 2006;40(5):486–487. doi: 10.1111/j.1365-2929.2006.02434.x. [DOI] [PubMed] [Google Scholar]
- 11.Beatty SJ, Kelly KA, Metzger AH, et al. Team-based learning in therapeutics workshop sessions. Am J Pharm Educ. 2009;73(6):Article 100. doi: 10.5688/aj7306100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Letassy NA, Fugate SE, Medina MS, et al. Using team-based learning in an endocrine module taught across two campuses. Am J Pharm Educ. 2008;72(5):Article 103. doi: 10.5688/aj7205103. [DOI] [PMC free article] [PubMed] [Google Scholar]