Abstract
Objective. To evaluate the impact of a continuing pharmacy education (CPE) course on Spanish community pharmacists’ participation in a pharmacotherapy follow-up program.
Design. Participation in a CPE course offered 4 times over a 4-year period via satellite teleconferencing was monitored and the data analyzed to determine the course’s impact on community pharmacists’ participation in a pharmacotherapy follow-up program.
Assessment. Community pharmacists’ participation in the pharmaceutical care CPE course had a slightly positive impact on their participation in the pharmacotherapy follow-up program. In the best profiles, there was a probability of 7.3% that participants would participate in the pharmacotherapy follow-up program.
Conclusions. Completion of pharmaceutical care CPE courses did not have a significant impact on pharmacists’ participation in a pharmacotherapy follow-up program.
Keywords: continuing pharmacy education, distance education, pharmaceutical care, pharmacotherapy follow-up
INTRODUCTION
Pharmacotherapy follow-up is a service that was developed by community pharmacies1-3 in response to a need for ongoing treatment of medication-based health problems. Lack of medication effectiveness and/or safety results in a high rate of avoidable emergency department visits.4 The implementation of this service requires a radical change in practice, including a shift from a medicine-centered approach to a new approach focused on the effects of medication on the patient.5
Continuing pharmacy education is necessary for community pharmacists to develop new skills such as pharmacotherapy follow-up.3,5,6 A lack of adequate training is considered one of the obstacles to implementing pharmacotherapy follow-up.7 However, the credit-based CPE model that is most frequently implemented in Spain seems to be insufficient to radically change the behavior of pharmacists. This study proposes a shift to a more complex CPE model based on individualized and qualitative criteria specific to the learning needs of the pharmacist.8
There is considerable discussion within the field of CPE about barriers and facilitators to lifelong learning,9,10 the results obtained from face-to-face instruction and distance education,11-13 and the acceptability and effectiveness of instruction depending on the model employed.14-17 Hence, the use of new technologies has been advocated to provide a comprehensive and quality distance education program to a large number of individuals.11,18,19
This study analyzed the association between pharmacist attendance at CPE meetings and their participation in the Dader Program of Pharmacotherapy Follow-Up, which involves the submission of interventions for real patient cases. The Dader Program of Pharmacotherapy Follow-Up is the only national program dedicated to monitoring pharmacists’ clinical activity through a pharmacotherapy follow-up service. This service facilitates pharmaceutical interventions by pharmacists, communication, and actions aimed at changing aspects of the patient’s treatment or use of medication in an attempt to resolve drug-related problems and negative medication outcomes.
In pharmacy, the pharmacist is responsible for addressing the patient’s medication needs. This type of practice is conducted through the detection of drug-related problems for the prevention of negative medication outcomes. This service requires a commitment that should be provided on a continual basis and in a systematic and well-documented way. Pharmacotherapy should be carried out in collaboration with the patient and other professional health care staff members with the aim of achieving results that improve the patient’s quality of life and understanding of drug-related problems in which the use or misuse of medicines causes or appears to cause a negative outcome. Negative medication outcomes are not consistent with the objectives of pharmacotherapy and are associated with errors in the use of medicines.
The CPE pharmacotherapy course, which was sponsored by the pharmaceutical industry and designed for community pharmacists, provided theoretical training applied to real patient cases and were conducted by means of synchronous satellite videoconferences held in 56 classrooms throughout Spain. Four sessions were held for the 2001 and 2002 courses, 3 sessions for the 2003 course, and 2 sessions for the 2004 course. The content of each course was accredited by the National Committee for the Continuous Training of Health Professionals, with credits awarded based on the number of tests passed. Pharmacists obtain 1 of 2 types of accreditation depending on whether they completed only the examination or the examination and a complementary test based on a clinical case study.
The objective of providing the pharmaceutical care courses was to encourage the use of the Dader pharmacotherapy follow-up service. The hypothesis was that if pharmacists completed the pharmacotherapy CPE course they would be more inclined to participate in the Dader program.
METHODS
A database was created of all pharmacists enrolled over the 2002-2004 period in the distance pharmaceutical care course of the Research Group into Pharmaceutical Care of the University of Granada, sponsored by the Stada pharmaceutical company (Barcelona, Spain). This explorative quantitative study used data provided by Stada laboratories on community pharmacists enrolled in CPE courses and data provided by the Dader program on the number of pharmaceutical interventions sent to them by those pharmacists in attempts to resolve suspicions of negative medication outcomes in patients included in the pharmacotherapy follow-up service. The following items were analyzed: the name of the pharmacist enrolled in the CPE course; the attendance code for pharmaceutical care courses; the number of sessions attended each year; gender; the total number of interventions sent to the Dader program from January 1, 2000, to December 30, 2005; the percentage of attendance at sessions in which they were enrolled; the number and percentage of examinations; and number of complementary tests completed. The influence of pharmaceutical care courses on the enrolled pharmacists was analyzed. Additionally, we examined the influence of the CPE courses on pharmacists who had not sent interventions to the Dader program before completing the courses. Comparing the number of interventions sent by pharmacists already enrolled in the Dader program with the number sent by pharmacists previously not enrolled in the program was used as an indicator of the effectiveness of the CPE courses.
Statistical analysis of the data was performed using SPSS, v.14.0 (SPSS, Chicago, IL) and AnswerTree v.3.0 (SPSS, Data Mining, Statistical Analysis Software). Univariate, bivariate, and multivariate analyses were conducted. The bivariate analysis was performed to evaluate the possible relationship between pairs of variables (sending of interventions to the Dader program, the dependent variable, and the other variables), using correspondence20,21 and non-parametric contrast analyses depending on the type of variable, Friedman contrast, chi-square21 contrast, Wilcoxon contrast, and Mann-Whitney contrast. In turn, this bivariate analysis depended on whether various related samples, pairs of numerical variables, pairs of related samples, or pairs of non-related21 samples were processed. Multivariate statistical techniques allowed for the establishment and identification of the most influential variable in the sending of interventions to the Dader program. Interdependence and dependence analyses were conducted for this purpose. The interdependence analyses included factorial analysis that allowed the number of variables studied to be reduced depending on the behavior of the participants as well as cluster analysis to establish 2 attendance and participation profiles. Hierarchical segmentation analysis was included in the dependence analyses (chi square automatic interaction detection analysis), which determines which predictive variable has the most influence on the dependent variable (sending of interventions to the Dader program) in addition to logistic regression analysis,20,21 which quantifies that influence. The significance level used was 5%.
RESULTS
The number of pharmacists enrolled 1 or more times in the pharmaceutical care CPE courses over the 2001-2004 period was 10,981. Eighty-six percent attended at least 1 or more sessions in each of the study years. Attendance at 1 or more sessions increased over the 4 years, from 3,769 pharmacists in 2001 to 4,429 in 2002, 4,849 in 2003, and 4,909 in 2004, with a mean attendance in 1 or more sessions per year of 73.7%, 86.8%, 95.1%, and 96.3% of the 10,981 pharmacists, respectively (p < 0.001). Attendance by gender showed significant differences in 2001, 2003, and 2004, with a greater percentage of men participating in 2001 (p < 0.001) and a greater percentage of women participating in 2003 and 2004 (p < 0.001).
Two homogenous groups, 2001/2002 and 2003/2004, were identified with regard to attendance at sessions, allowing us to combine the data for these groups and reduce the number of variables included in the analysis from 4 to 2. With the output of the factor analysis, cluster analysis allowed us to group the pharmacists enrolled into 2 profiles of attendance: 1 with a high level of attendance (corresponding to 29% of those enrolled) and another with a low level of attendance (corresponding to 71% of those enrolled). The high-attendance group included pharmacists who attended more than 50% of the sessions per year, while the low-attendance group included pharmacists who attended fewer than 50% of sessions per year.
In the high-attendance group, 50% of those enrolled attended all of the sessions held for 2001, 2002, 2003, and 2004. In the low-attendance group, 25% of those enrolled attended 1 or more of the 2003 sessions and all of the 2004 sessions. There was not a significant difference in attendance rates between men and women (p = 0.640) in either of the 2 groups.
Participation in the pharmaceutical care CPE courses was determined based on the enrolled pharmacists’ completion of examinations (theoretical knowledge tests) and participation in clinical cases. The mean number of clinical cases sent per province in relation to the number of pharmacists enrolled increased significantly during the study period (p = 0.001). An increase in the number of theoretical knowledge tests sent (p = 0.001) occurred each year. The number of theoretical knowledge tests completed was twice the number of clinical cases.
As with attendance, 2 profiles of pharmacist participation were observed: one high-participation group, consisting of 52.4% of the pharmacists, and one low-participation group, consisting of 47.7% of the pharmacists. The pharmacists in the high-participation group submitted an average of 93.2% of the examinations and 47% of the complementary practical tests for the courses, whereas the pharmacists in the low-participation group submitted an average of 8.4% and 1.2% of examinations and complementary tests, respectively. There were more women (55.3%) than men (45.1%) in the high-participation group (p < 0.001).
Overall, 96% of the pharmacists enrolled in the CPE courses did not send any pharmaceutical interventions to the Dader Program of Pharmacotherapy Follow-Up. Of the 3.9% who participated in the Dader program, approximately 50% had participated in the Dader program before enrolling in the pharmaceutical care CPE courses. The mean number of interventions sent to the Dader program by pharmacists already affiliated with it was 50, compared with a mean of 22 interventions sent by pharmacists who began sending interventions as a result of taking the CPE courses (p < 0.001). An important dispersion of these data was observed in both groups, with a variation coefficient >1. Participation in the Dader program was similar for men and women (p = 0.141).
Participants’ level of attendance and participation (the predictive variables considered) had a significant impact on whether they sent interventions to the Dader program (p < 0.001), with participation being the most influential variable. When we analyzed only pharmacists who had not participated in the Dader program before enrolling in the pharmaceutical care courses, the level of attendance and participation in the CPE courses had a significant influence on the interventions sent to the Dader program (p < 0.001), with attendance being the most relevant variable.
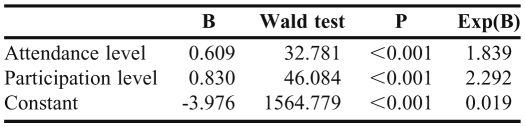
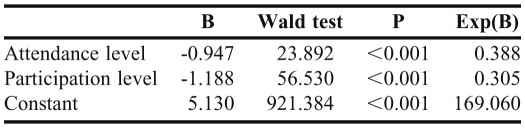
The importance of attendance and participation in the CPE courses on the interventions was evaluated using logistic analysis, analyzing all pharmacists enrolled (model 1) and only pharmacists who had not participated in the Dader program prior to enrolling in the pharmaceutical care courses (model 2). The estimation of the first logistic model (Table 1) allowed us to calculate the probability of the interventions in the Dader program for pharmacists in the high-participation and high-attendance profile: 7.3% (CI: 4.8%-11.0%). The second model (Table 2) allowed us to calculate the probability of interventions and patient referrals to the Dader program from pharmacists in the high-participation and high-attendance profile: 4.7% (CI: 2.0%-9.0%).
Table 1.
Logistics Model 1: Pharmacists’. Attendance and Participation Level in Continuing Pharmaceutical Education Courses as Predictors of Participation in the Dader Program of Pharmacotherapy Follow-Up
Table 2.
Logistics Model 2: Pharmacists’ Attendance and Participation Level in Continuing Pharmaceutical Education Courses as Predictors of Participation in the Dader Program of Pharmacotherapy Follow-Up
DISCUSSION
The analysis of attendance and participation in CPE courses over the 4 years indicated that these variables had little quantitative influence on participating in the pharmacotherapy follow-up service. Despite the decrease in the number of sessions provided per CPE course in 2003 and 2004, a significant reduction in attendance was observed in the last session of a course compared with the first session of the same course. The course design included facilitators who encouraged attendance at the sessions by application of theoretical knowledge to the clinical cases of real patients, and all information for the course was not provided in the printed teaching material. Despite this, a majority of the pharmacists (70.9%) had low attendance profiles, which suggests that, for both genders, the perceived benefits of attending the sessions did not justify the effort necessary to attend the classes.
Participation was closely linked to the higher accreditation awarded to pharmacists who participated and passed the practical tests. However, each year, the number of clinical cases was considerably lower, comparatively, than the number of theoretical knowledge tests completed. This difference can be explained by the greater profitability of the credits obtained from passing the theory examination. Participation increased over the study period, with the difference between the percentage of theoretical and practical tests diminishing due to an increase in the pharmacists’ participation in clinical cases and the acquisition of training. Of the pharmacists enrolled in 2004, 68% had attended a previous course.
The high participation profile of 52.4% of the pharmacists compared to the high attendance profile of 29.1% of those enrolled indicates a greater interest among the pharmacists in obtaining credits than in attending classes (attendance at sessions did not earn credit). This difference was greater among women than men, suggesting that women were more concerned with their academic curriculum.
Pharmacist participation of less than 4% in the Dader program and the mean number of interventions sent shows the low impact of the pharmaceutical care courses on participation in the program. There were no significant differences in terms of gender, as Aguas22 notes. Despite the use of data on the total number of interventions sent to the Dader program from January 1, 2000, to December 30, 2005, which includes 1 year of accumulated data for those pharmacists who began sending interventions before the pharmaceutical care courses. The mean number of interventions sent to the Dader program dropped to nearly half in the group of pharmacists who had not participated in the Dader program prior to enrolling in the pharmaceutical care courses. This fact demonstrates the influence of factors other than the continuing training received, such as different individual attitudes as a result of less professional experience resulting in a lower confidence level regarding interventions when faced with the suspicion of a negative medication outcomes.23
The results show no impact of attendance and participation in the pharmaceutical care courses on the sending of interventions to the Dader program. There is no direct relationship, as has been reported by other authors22 who have noted the influence of attendance at training activities on pharmacotherapy follow-up and the sending of interventions without implying a direct link between attendance and interventions sent.
To investigate the significance of participation in courses a logistic model was used that allowed us to quantify this significance and to determine that, even though we selected pupils with the best attendance and participation profiles, a participation percentage of only 7.3% was achieved in the Dader program. The remaining 92.7% of pharmacists who received theoretical training and passed the theoretical knowledge test and/or clinical cases did not join the Dader program. Therefore, most pharmacists who achieved the highest accreditation awarded by those courses were not sufficiently capable of opting for the accreditation awarded by the Dader program to conduct pharmacotherapy follow-up on real patients.
If we consider only the pharmacists who had not participated in the Dader program before enrolling in the pharmaceutical care courses, the impact of the courses can be observed on the sending of interventions, but with a lesser probability than in the total group of those enrolled. This decrease in probability is not considered significant because it is within the same confidence interval.
In the total group of those enrolled, participation is the variable of greatest influence, whereas in the group of pharmacists who had not participated in the Dader program before the course, attendance is the most relevant variable, possibly because of their lower theoretical knowledge and need to attend a greater number of sessions to receive basic training in the pharmaceutical care courses.
It may be said that the pharmaceutical care courses had an impact, but it was not significant. Different degrees of significance in participation and attendance were observed depending on whether the pupils had previous participation in the Dader program.
Because of the resources available, there are limitations to the research methods employed. The sending of interventions from the pharmacists enrolled in the Dader Pharmacotherapy Follow-up Program was used as an indicator of the effectiveness of the pharmaceutical care courses without considering other courses or sources of information that may have influenced the number of interventions the pharmacists made. The possibility must also be considered that a small number of interventions to resolve negative results from medication are not stated in the records of the Dader program because they were not communicated. This number is considered negligible because the obtained accreditation for participating in the program depends on the number of interventions received. There was also a lack of knowledge about the number of patients who were attended one time and whether they were included in the pharmacotherapy follow-up service.
CONCLUSIONS
Approximately half of the pharmacists who submitted interventions to the Dader Program of Pharmacotherapy Follow-Up had previous enrollment in the CPE courses. The average number of interventions submitted was lower for pharmacists who had not participated in the Dader program prior to enrolling in the CPE courses. There was a relationship between course attendance and participation and the submission of interventions, but this relationship was not quantitatively relevant, even among the pharmacists with high-participation profiles. Therefore, it can be concluded that training is not the sole facilitator for achieving significant participation among pharmacists in the Dader Program of Pharmacotherapy Follow-Up.
REFERENCES
- 1.Martin-Calero MJ, Machuca M, Murillo MD, Cansino J, Gastelurrutia MA, Faus MJ. Structural process and implementation programs of pharmaceutical care in different countries. Curr Pharm Design. 2004;10:3969–3985. doi: 10.2174/1381612043382549. [DOI] [PubMed] [Google Scholar]
- 2.Amariles P, Machuca M, Faus MJ, Baena MI, Martinez-Martinez F, Jiménez-Martin J. Application of the SCORE and Wilson-Grundy methods for the assessment of cardiovascular risk in community pharmacies. J Clin Pharm Ther. 2008;33:475–481. doi: 10.1111/j.1365-2710.2008.00953.x. [DOI] [PubMed] [Google Scholar]
- 3.Gastelurrutia MA, Fajardo PC, Baena MI, et al. Identification and prioritisation of facilitators for the implementation of cognitive services in Spanish community pharmacies. Pharm World Sci. 2007;29:469–470. [Google Scholar]
- 4.Baena MI, Faus MJ, Fajardo P, et al. Medicine-related problem resulting in emergency department visits. Eur J Clin Pharmacol. 2006;62:387–393. doi: 10.1007/s00228-006-0116-0. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez-Llimos F, Faus MJ, Gastelurrutia MA, Baena I, Martínez-Martínez F. Evolution of the concept of drug-related problems: outcomes as focus of the new paradigm. Seguim Farmacoter. 2005;3:167–188. [Google Scholar]
- 6.Grupo de Investigación en Atención Farmacéutica de la Universidad de Granada. Dader method to provide pharmacotherapy follow up. Ars Pharm. 2005;46:309–337. [Google Scholar]
- 7.Gastelurrutia MA, Fernandez-Llimos F, Benrimoj SI, Castillo CC, Faus MJ. Barreras para la implantación de servicios cognitivos en la farmacia comunitaria española. Aten Primaria. 2007;39:465–472. doi: 10.1157/13109494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Driesen A, Verbeke K, Simoens S, Laekeman G. International trends in lifelong learning for pharmacists. Am J Pharm Educ. 2007;71(3):Article 52. doi: 10.5688/aj710352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hanson AL, Bruskiewitz RH, DeMuth JE. Pharmacists’ perceptions of facilitators and barriers to lifelong learning. Am J Pharm Educ. 2007;71(4):Article 67. doi: 10.5688/aj710467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Driesen A, Leemans L, Baert H, Laekeman G. Flemish community pharmacists´motivation and related to continuing education. Pharm World Sci. 2005;27(6):447–452. doi: 10.1007/s11096-005-0950-7. [DOI] [PubMed] [Google Scholar]
- 11.Ried LD, McKenzie M. A preliminary report on the academic performance of pharmacy students in a distance education program. Am J Pharm Educ. 2004;68(3):Article 65. [Google Scholar]
- 12.Lenz TL, Monaghan MS, Wilson AF, Tilleman JA, Jones RM, Hayes MM. Using performance-based assessments to evaluate parity between a campus and distance education pathway. Am J Pharm Educ. 2006;70(4):Article 90. doi: 10.5688/aj700490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ried LD, Motycka C, Mobley C, Meldrum M. Comparing self-reported burnout of pharmacy students on the founding campus with those at distance campuses. Am J Pharm Educ. 2006;70(5):Article 114. doi: 10.5688/aj7005114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacLaughlin EJ, Supernaw RB, Howard KA. Impact of distance learning using videoconferencing technology on student performance. Am J Pharm Educ. 2004;68(3):Article 58. [Google Scholar]
- 15.De Muth JE, Bruskiewitz R. A. Comparison of the acceptability and effectiveness of two methods of distance education: CD-ROM and audio teleconferencing. Am J Pharm Educ. 2006;70(1):Article 11. doi: 10.5688/aj700111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross LA, Crabtree BL, Theilman GD, Ross BS, Cleary JD, Byrd HJ. Implementation and refinement of a problem-based learning model: a ten-year experience. Am J Pharm Educ. 2007;71(1):Article 17. doi: 10.5688/aj710117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moridani M, Chem DC. Asynchronous video streaming vs. synchronous videoconferencing for teaching a pharmacogenetic pharmacotherapy course. Am J Pharm Educ. 2007;71(1):Article 16. doi: 10.5688/aj710116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sibbald D. A student assessment of the virtual interactive case tool for asynchronous learning (VITAL) and other self-directed learning formats. Am J Pharm Educ. 2004;68(1):Article 11. [Google Scholar]
- 19.Moreno-Sanz C, Pascual-Pedreño A, Corral-Sánchez MA, Seoane-González J. Experiencia inicial con un portal de Internet dedicado a la formación continuada en cirugía mínimamente invasiva. Cirugía Española. 2003;73(5):276–281. Accreditation Council for Pharmacy Education. Accreditation Standards for Continuing Pharmacy Education. Adoption: June 20, 2007. Released: October 5, 2007. Effective: January 1, 2009. http://www.acpe-accredit.org/pdf/CPE Standards Final.pdf Accessed Jan 20, 2010. [Google Scholar]
- 20.Pérez C. Técnicas Estadísticas con SPSS. Madrid: Prentice-Hall. 2001. Fjortoft N. Students’ motivations for class attendance. Am J Pharm Educ. 2005;69(1):Article 15. [Google Scholar]
- 21.Stada. Formación continuada realizada. http://www.stada.es/es/farmacia_realizada_aula_satelite_02.php Accessed July 29, 2010.
- 22.Aguas Y. Análisis de la efectividad de las acciones de un centro de información de medicamentos en la implantación del seguimiento farmacoterapéutico en farmacias comunitarias. [dissertation] Granada, Spain: Universidad de Granada; 2005. [Google Scholar]
- 23.Gastelurrutia MA, Benrimoj SI, Castrillon CC, Casado de Amezua MJ, Fernadez-Llimós F, Faus MJ. Facilitators for practice change in Spanish community pharmacy. Pharm World Sci. 2009;31(1):32–39. doi: 10.1007/s11096-008-9261-0. [DOI] [PubMed] [Google Scholar]