Dear Editor,
A 65-year-old male was diagnosed with a left renal tumor. Whole body CT scanning was negative for metastasis. The patient underwent left nephrectomy and pathological examination was consistent with a renal clear cell carcinoma graded 3 on Furhman scale. He was elected to undergo treatment with sunitinib. Chest CT six months later revealed small nodular formations in the left upper lobe 0.5-1 cm in diameter, enlarged mediastinal lymph nodes and bilateral pleural effusion.
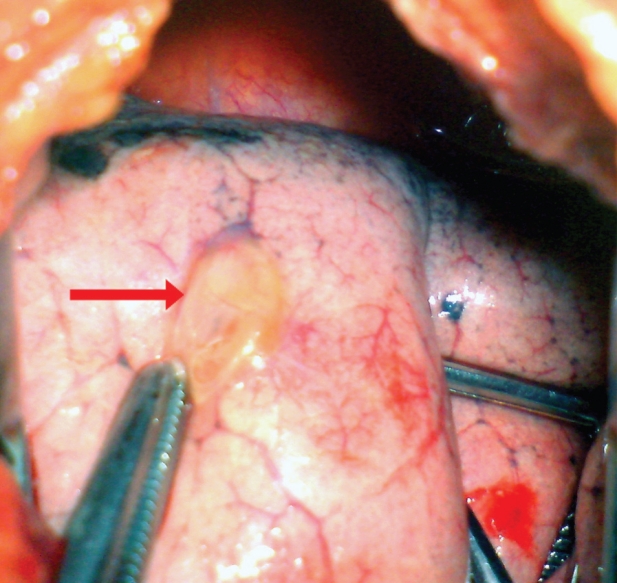
Treatment with sunitinib was continued and two months later, he was admitted with a 5-day history of shortness of breath and pleuritic chest pain. Chest x-ray and CT showed pneumothorax on the left side. Additionally, a cavitation in one of the previously noted lung nodules was revealed and considered as the most probable cause of pneumothorax. A chest tube was placed urgently. Due to persistent air leakage and lung collapse under closed tube, it was decided that the patient was eligible for surgical intervention. He underwent a left mini muscle-sparing thoracotomy. The existence of ruptured bullae on a metastatic lesion was brought to light (Figure 1). Segmentectomy of the left upper lobe was performed. Additional metastasectomies for the other two lesions and a dry gauze abrasion pleurodesis completed the operation. Pathological examination confirmed the presence of metastatic renal carcinoma. One month later, a new chest CT revealed normal findings and sunitinib was restarted.
Figure 1. Intraoperative image of ruptured bullae on a metastatic lesion (red arrow).
The suggested mechanisms for chemotherapy-associated pneumothorax include rapid tumor lysis and necrosis of the large metastatic pulmonary lesions, enlargement of a rapidly necrotizing tumor, chemotherapy-induced impairment of repair processes, and/or persistent local infection1.
References
- 1.Yamada N, Abe N, Usui K, Noda H, Tanaka Y, Tanai C, et al. Clinical analysis of 12 cases of pneumothorax during intensive chemotherapy for malignant neoplasms. Gan To Kagaku Ryoho. 2010;37:1519–1523. [PubMed] [Google Scholar]