Abstract
Purpose
To evaluate electroretinogram (ERG) changes after silicone oil removal.
Methods
Scotopic and photopic ERGs, and best-corrected visual acuity (BCVA) were checked before and shortly after silicone oil removal in eyes that had previously undergone vitrectomy and silicone oil injection for complex retinal detachment. Pre- and postoperative ERG a- and b-wave amplitudes were compared.
Results
Twenty-eight eyes of 28 patients including 20 male and 8 female subjects with mean age of 39.3 ± 0.06 (range, 12 to 85) years were studied. Mean interval from primary vitreoretinal surgery to silicone oil removal was 21.04 ± 0.52 (range, 7 to 39) months. Mean duration from silicone oil removal to second ERG was 13.04 ± 1.75 (range, 10 to 16) days. Before silicone oil removal, mean a-wave amplitudes in maximal combined response, rod response and cone response ERGs were 27.4 ± 19.9, 7.2 ± 4.5 and 5.5 ± 3.4 μv, respectively. These values increased to 48.8 ± 31.9, 15.1 ± 14.4 and 17.4 ± 22.2 μv, respectively after silicone oil removal (P < 0.001). Mean b-wave amplitudes in the same order, were 69.41 ± 51, 41.2 ± 30.4 and 25.1 ± 33.9 μv before silicone oil removal, increasing to 165.6 ± 102.5, 81.7 ± 53.7 and 44.7 ± 34.1 μv respectively, after silicone oil removal (P < 0.001). Mean BCVA significantly improved from 1.10 ± 0.34 at baseline to 1.02 ± 0.33 logMAR after silicone oil removal (P < 0.001).
Conclusion
The amplitudes of ERG a- and b-waves under scotopic and photopic conditions increased significantly shortly after silicone oil removal. An increase in BCVA was also observed. These changes may be explained by the insulating effect of silicone oil on the retina.
Keywords: Vitrectomy, Silicone Oil, Electroretinogram
INTRODUCTION
Silicone oil was introduced by Cibis and associates for intraocuar tamponade in the surgical management of complicated retinal detachments.1,2 It has been used successfully for long term tamponade and maintenance of reattachment in complex retinal detachments (RDs), severe proliferative vitreoretinopathy (PVR), and RDs following severe trauma. The use of silicone oil in conjunction with vitrectomy is considered as the last resort for treatment of severe proliferative diabetic retinopathy (PDR).3,4 With the improved understanding of vitreoretinal abnormalities and advanced surgical techniques, silicone oil is being used extensively for many retinal disorders.4–8 The use of silicone oil for temporary internal tamponade in our patients provided us a chance to study the insulating effect of silicone oil on the retina by electroretinography (ERG) and to compare its changes after removal of the oil.
METHODS
Twenty-eight eyes of 28 patients, including 20 male and 8 female subjects with mean age of 39.3±0.06 (range, 12 to 85) years with complex RD who had undergone vitrectomy and temporary tamponade with purified silicone (5000 centistokes) were studied. Minimum follow-up after surgery was 3 months. Patients with vascular eye disease such as diabetic retinopathy or retinal vascular accidents, pre- or postoperative glaucoma, media opacity (corneal or dense cataract), and complicated silicone removal were excluded from the study. Uneventful silicone oil removal was considered essential for comparison of pre- and postoperative electrophysiological results. The retina was attached before silicone oil removal in all cases.
Photopic (cone response), scotopic (rod response) and maximal combined response ERGs were obtained according to the methods described by the International Society for Clinical Electrophysiology of Vision (ISCEV) using the Mono Elec 2 system (Metrovision Inc., France) in all cases before and shortly after silicone oil removal. The amplitude of a- and b-waves before and after silicone oil removal in conditions of rod response, maximal combined response and cone response were detected and compared using Wilcoxon test with significance set at P<0.05.
RESULTS
Table 1 summarizes demographic and clinical data of the patients. Underlying conditions leading to vitrectomy and internal tamponade with silicone oil were traumatic RD in 9 (32.1%), pseudophakic RD in 8 (28.6%), myopic RD in 7 (25.9%), and aphakic RD, macular hole RD, giant retinal tear and stickler syndrome, each in one (3.57%) case. The retina remained attached after silicone oil removal in all 28 patients. Mean duration of silicone oil retention was 21.04±0.06 (range, 7 to 39) months. Mean duration from silicone oil removal to the second ERG recording was 13.04±1.75 (range, 10 to 16) days.
Table 1.
Demographic and clinical data of the patients before and after silicone oil removal
| No | Age (years) | Sex | Eye | Underlying disease | Duration of retained silicone oil (months) | Duration from oil removal to ERG (days) | BCVA | a-wave amplitude (μv) | b-wave amplitude (μv) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maximal combined response | Rod response | Cone response | Maximal combined response | Rod response | Cone response | |||||||||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||||||
| 1 | 69 | F | OD | Myopic RRD | 23 | 14 | 20/200 | 20/160 | 28.1 | 99.2 | 3.1 | 14.1 | 7 | 6 | 93.7 | 244 | 59.3 | 144 | 24.3 | 84.7 |
| 2 | 54 | F | OS | Myopic RRD | 16 | 16 | CF3m | CF3m | 17.2 | 26.6 | 10.8 | 7.7 | 6.4 | 8.7 | 24.9 | 63.2 | 11.7 | 17.2 | 13.5 | 14.6 |
| 3 | 28 | M | OS | Traumatic RRD | 7 | 13 | CF2.5m | CF3m | 47.7 | 78 | 10.2 | 15 | 10.2 | 12.3 | 84.3 | 205 | 50.7 | 98.3 | 28 | 54.1 |
| 4 | 26 | M | OS | Traumatic RRD | 8 | 14 | 20/160 | 20/160 | 43 | 50 | 10.2 | 8.7 | 6 | 18.9 | 93.7 | 312 | 55.4 | 90 | 26.4 | 53.7 |
| 5 | 21 | F | OS | Pseudophakic RRD | 25 | 13 | 20/200 | 20/120 | 1.6 | 3.8 | 6.3 | 7 | 1 | 5.4 | 10.9 | 10.8 | 7.7 | 7 | 18.5 | 14.9 |
| 6 | 12 | M | OS | Myopic RRD | 19 | 12 | CF4m | CF4m | 14.1 | 37.5 | 11.7 | 3.1 | 5.2 | 7.4 | 31.2 | 37.5 | 14 | 14 | 5.6 | 7.5 |
| 7 | 31 | F | OD | Myopic RRD | 30 | 13 | 20/160 | 20/120 | 7 | 16.4 | 0.8 | 1.2 | 4.3 | 4.5 | 17.9 | 38.2 | 8.5 | 11.6 | 7.6 | 19 |
| 8 | 30 | M | OD | Traumatic RRD | 28 | 14 | 20/50 | 20/50 | 46.1 | 67.2 | 7.8 | 10.2 | 16.2 | 14.2 | 198 | 266 | 108 | 104 | 44.9 | 56.2 |
| 9 | 37 | M | OS | Aphakic RRD | 32 | 15 | CF3m | CF4m | 9.4 | 66.2 | 1.5 | 68.8 | 2.2 | 8.1 | 21.8 | 66.2 | 5.5 | 92.9 | 4.3 | 9.8 |
| 10 | 52 | M | OS | Traumatic RRD | 36 | 15 | CF2m | CF2.5m | 23.3 | 6.3 | 6.9 | 5.6 | 2.6 | 1.2 | 84.4 | 64.6 | 42.2 | 39.7 | 9 | 5.7 |
| 11 | 33 | F | OD | Retinal angiomatosis | 27 | 14 | CF1.5m | CF2m | 37.5 | 39.1 | 5.5 | 5.5 | 7.9 | 6.3 | 94.4 | 148 | 53 | 93.7 | 24.1 | 21.2 |
| 12 | 60 | M | OD | Pseudophakic RRD | 39 | 12 | CF3m | CF3m | 20.3 | 23.4 | 3.1 | 6.3 | 6.3 | 120 | 35.8 | 294 | 16.3 | 20.5 | 15.2 | 152 |
| 13 | 54 | M | OS | Pseudophakic RRD | 21 | 13 | 20/200 | 20/120 | 22.7 | 68 | 0 | 1.5 | 2.6 | 23.2 | 31.9 | 121 | 28 | 105 | 17.4 | 13.5 |
| 14 | 16 | M | OS | Myopic RRD | 15 | 11 | 20/160 | 20/160 | 15.6 | 58.6 | 12.5 | 7.8 | 6.3 | 10.5 | 37.4 | 121 | 18.7 | 46 | 13.9 | 41.5 |
| 15 | 32 | M | OS | Myopic RRD | 18 | 10 | CF1m | CF1.5m | 14 | 39.1 | 11.7 | 43.8 | 2.1 | 9.1 | 15.6 | 213 | 68.7 | 138 | 22.9 | 49.2 |
| 16 | 47 | M | OS | Pseudophakic RRD | 31 | 13 | 20/160 | 20/160 | 3.9 | 16.2 | 6.3 | 16 | 8.7 | 40.8 | 34.3 | 112 | 21 | 69.4 | 24.9 | 61.2 |
| 17 | 85 | M | OS | Traumatic RRD | 17 | 16 | CF1m | CF2m | 76 | 91.4 | 0.8 | 13.3 | 5.2 | 19.1 | 112 | 249 | 66.3 | 130 | 30 | 90.9 |
| 18 | 38 | F | OS | Stickler syndrome | 20 | 13 | 20/200 | 20/160 | 45.8 | 43 | 0 | 28.1 | 7.2 | 14.7 | 166 | 173 | 105 | 118 | 27 | 32.8 |
| 19 | 19 | M | OS | Traumatic RRD | 8 | 13 | 20/200 | 20/120 | 42.2 | 56.3 | 12 | 12.5 | 4.3 | 28.9 | 106 | 202 | 74 | 113 | 190 | 58.4 |
| 20 | 50 | M | OD | Pseudophakic RRD | 28 | 14 | 20/200 | 20/200 | 32.8 | 58.6 | 14.1 | 20.3 | 5.6 | 8.3 | 60.8 | 176 | 54.6 | 108 | 7.8 | 32.2 |
| 21 | 36 | M | OS | Macular hole RD | 25 | 11 | CF5m | 20/160 | 10.4 | 14.8 | 0.7 | 2.3 | 1.7 | 3.9 | 13.6 | 98.4 | 6.3 | 23 | 1.4 | 17 |
| 22 | 38 | F | OS | Traumatic RRD | 15 | 15 | 20/160 | 20/160 | 75 | 149 | 14.1 | 21.1 | 8.3 | 23.2 | 112 | 318 | 59.3 | 173 | 27.7 | 81.7 |
| 23 | 39 | M | OS | Pseudophakic RRD | 12 | 12 | 20/160 | 20/120 | 45.3 | 73.4 | 7 | 35.2 | 9.4 | 34.1 | 162 | 326 | 79.6 | 208 | 32.4 | 99.6 |
| 24 | 43 | F | OD | Myopic RRD | 29 | 12 | CF5m | CF5m | 34.4 | 43.8 | 7.7 | 15.6 | 0.6 | 8.1 | 28.1 | 49.9 | 5.5 | 24.2 | 17.2 | 23.3 |
| 25 | 39 | M | OD | Pseudophakic RRD | 17 | 14 | CF2m | CF2.5m | 7.7 | 24.9 | 8.1 | 11 | 2.2 | 7.9 | 12.5 | 35.9 | 3 | 10.9 | 2.1 | 17 |
| 26 | 55 | M | OS | RRD | 19 | 10 | 20/80 | 20/80 | 26.6 | 39.1 | 6 | 8.6 | 2.6 | 11.8 | 65.5 | 98.3 | 26.5 | 72.6 | 18.8 | 26.1 |
| 27 | 27 | M | OS | Traumatic RRD | 11 | 13 | 20/160 | 20/160 | 4.3 | 59.1 | 10.3 | 12.5 | 6 | 18.8 | 93.2 | 315 | 55.4 | 98 | 26.2 | 54.5 |
| 28 | 30 | M | OD | Traumatic RRD | 13 | 10 | 20/60 | 20/60 | 15 | 17.9 | 12.5 | 18.7 | 6.8 | 12.7 | 91 | 278 | 49 | 117 | 23 | 58 |
F, female; M, male; OD, right eye; OS, left eye; RRD, rhegmatogenous retinal detachment; BCVA, best-corrected visual acuity; CF, counting fingers; Pre, before silicone oil removal; Post, after silicone oil removal.
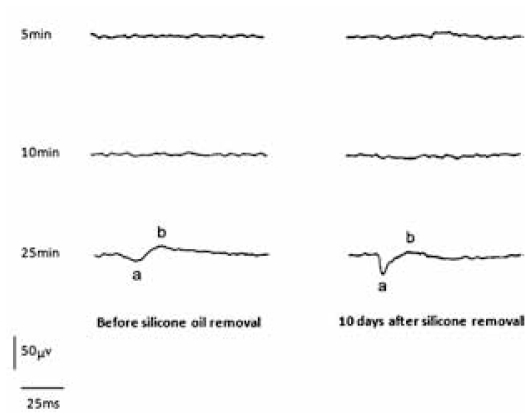
The amplitudes of ERG a- and b-waves were greatly reduced or even unrecordable before silicone oil removal. The amplitudes of both waves increased significantly after silicone oil removal (Fig. 1), although the anatomic condition and retinal attachment status remained unchanged.
Figure 1.
A representative case (No:6) demonstrates minimal response ERG; despite increasing dark adaptation from 5 minutes to 10 and 25 minutes and use of a high intensity stimulus, no significant electroretinographic amplitude could be recorded before silicone oil removal. ERG in the same patient 10 days after silicone oil removal demonstrates a significant increase in both a- and b-wave amplitudes with the use of a high-intensity stimulus and progressive dark adaptation.
Mean BCVA before silicone oil removal was 1.10±0.34 (range, 0.04 to 1.70) logMAR which significantly improved 1.02±0.33 (range, 0.04 to 1.70) logMAR afterwards, indicating a mean difference of −0.08±0.09 logMAR (95% confidence interval, −0.11 to −0.03; P<0.001).
Tables 2 and 3 compare a- and b-wave amplitudes before and after silicone oil removal under conditions of maximal combined, rod and cone response respectively; all changes were statistically significant (P<0.001) in all conditions.
Table 2.
a-wave amplitude (microvolts) before and after silicone oil removal
| Response | Mean ± Standard Deviation (range) | 95% CI of difference | P value | ||
|---|---|---|---|---|---|
| Pre | Post | Difference | |||
| Maximal combined | 27.4 ± 19.9 27 (1.6 to 76) |
48.8 ± 31.9 43.4 (3.8 to 149) |
21.4 ± 22.4 14.8 (−17 to 74) |
12.7 to 30.1 | <0.001 |
| Rod | 7.2 ± 4.5 7.4 (0 to 14.1) |
15.1 ± 14.4 11.8 (1.2 to 68.8) |
7.8 ± 15.1 2.8 (−8.6 to 67.3) |
−2 to 13.7 | 0.001 |
| Cone | 5.5 ± 3.4 5.8 (0.6 to 16.2) |
17.4 ± 22.2 11.2 (1.2 to 120) |
11.9 ± 21.8 5.9 (−2 to 113.7) |
3.5 to 20.3 | <0.001 |
Pre, before silicone oil removal; Post, after silicone oil removal; CI, confidence interval
Table 3.
b-wave amplitude (microvolts) before and after silicone oil removal
| Response | Mean ± Standard deviation (range) | 95% CI of difference | P value | ||
|---|---|---|---|---|---|
| Pre | Post | Difference | |||
| Maximal combined | 69.0 ± 51.0 63.2 (10.9 to 198) |
165.6 ± 102.5 160.5 (10.8 to 326) |
96.5 ± 78.5 84.2 (−19.8 to 258.2) |
66.1 to 127 | <0.001 |
| Rod | 41.2 ± 30.4 45.6 (3.0 to 10.8.0) |
81.7 ± 53.7 93.3 (7.0 to 208.0) |
40.5 ± 36.1 39.9 (−4 to 128.4) |
26.5 to 54.4 | <0.001 |
| Cone | 25.1 ± 33.9 20.9 (1.4 to 190) |
44.7 ± 34.1 37.2 (5.7 to 152) |
19.5 ± 42.1 15.2 (−131.6 to 136.8) |
3.2 to 35.8 | <0.001 |
Pre, before silicone oil removal; Post, after silicone oil removal; CI, confidence interval
DISCUSSION
Histologic and electrophysiologic findings following vitreoretinal surgery utilizing silicone oil tamponade seem contradictory and different conclusions have been made on the toxicity of liquid silicone.9–10 In enucleated eyes after silicone surgery, vacuole formation has been observed in the retina and optic nerve, and even beyond the lamina oribrosa.11 In animal experiments, vacuole formation and destruction of ganglion cells have been described following silicone injection.9–12 Although cataract formation, keratopathy and secondary glaucoma are well known complications of silicone oil filling,8,13 the question of retinal toxicity still remains unanswered.
Most investigators have reported no histological evidence of retinal damage due to silicone oil. All agree that in silicone oil filled eyes, ERG and EOG (electrooculogram) waves are diminished or even unrecordable, but they have different interpretations for these finding. Some authors9,12,14 consider them as a sign of retinal toxicity, while others3,15,16 have assumed an insulator effect by silicone oil. The insulating effect of silicone oil on the retina was confirmed in our study such that the amplitude of ERG a- and b-waves under both photopic and scotopic conditions was either low or unrecordable before silicone oil removal but increased significantly in all patients; a finding which is in line with other published reports.17,18
Regarding the minimum duration of four weeks for photoreceptor recovery after retinal reattachment,19,20 silicone oil was removed 7 to 39 months after vitreoretinal surgery in our series. We assumed that by this time, the photoreceptors should have made ultimate recovery and ERG amplitudes could be considered as a reliable baseline for comparison after silicone oil removal.19,20
The baseline level of the corneoretinal potential was low in all eyes before silicone oil removal but increased afterwards. The reduced baseline level of the corneoretinal potential in silicone oil filled eyes is due to an insulating effect and equivalent to reduction of ERG amplitudes. A similar insulating effect has been reported in gas-filled eyes as long as the gas is retained within the eye.17
We may conclude that silicone oil removal increases ERG wave amplitudes and improves visual acuity after an adequate period of retention necessary for establishment of retinal reattachment and photoreceptor recovery. These changes in ERG a- and b-wave amplitudes may be attributed to the insulating effect of silicone oil on the retina rather than actual toxicity. Silicone oil should therefore be removed from all eyes after accomplishment of its effect.
Footnotes
Conflicts of Interest
None.
REFERENCES
- 1.Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol. 1962;68:590–599. doi: 10.1001/archopht.1962.00960030594005. [DOI] [PubMed] [Google Scholar]
- 2.Lucke KH, Foerster MH, Laqua H. Long-term results of vitrectomy and silicone oil in 500 cases of complicated retinal detachments. Am J Ophthalmol. 1987;104:624–633. doi: 10.1016/0002-9394(87)90176-0. [DOI] [PubMed] [Google Scholar]
- 3.Gabel VP, Kampik A, Burkhardt J. Analysis of intraocularly applied silicone oils of various origins. Graefes Arch Clin Exp Ophthalmol. 1987;225:160–162. doi: 10.1007/BF02175441. [DOI] [PubMed] [Google Scholar]
- 4.Grey RH, Leaver PK. Silicone oil in the treatment of massive preretinal retraction. I. Results in 105 eyes. Br J Ophthalmol. 1979;63:355–360. doi: 10.1136/bjo.63.5.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Momirov D, van Lith GH, Zivojnović R. Electroretinogram and electrooculogram of eyes with intravitreously injected silicone oil. Ophthalmologica. 1983;186:183–188. doi: 10.1159/000309284. [DOI] [PubMed] [Google Scholar]
- 6.Zivojnović R, Mertens DA, Baarsma GS. Fluid silicon in detachment for surgery. Klin Monbl Augenheilkd. 1981;179:17–22. [PubMed] [Google Scholar]
- 7.Zivojnović R, Mertens DA, Peperkamp E. Liquid silicone in amotio surgery (II). Report on 280 cases - further development of the technic. Klin Monbl Augenheilkd. 1982;181:444–452. [PubMed] [Google Scholar]
- 8.Leaver PK, Grey RH, Garner A. Silicone oil injection in the treatment of massive preretinal retraction. II. Late complications in 93 eyes. Br J Ophthalmol. 1979;63:361–367. doi: 10.1136/bjo.63.5.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee PF, Donovan RH, Mukai N, Schepens CL, Freeman HM. Intravitreal injection of silicone: an experimental study. Ann Ophthalmol. 1969;1:15–25. [PubMed] [Google Scholar]
- 10.Meredith TA, Lindsey DT, Edelhauser HF, Goldman AI. Electroretinographic studies following vitrectomy and intraocular silicone oil injection. Br J Ophthalmol. 1985;69:254–260. doi: 10.1136/bjo.69.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ni C, Wang WJ, Albert DM, Schepens CL. Intravitreous silicone injection. Histopathologic findings in a human eye after 12 years. Arch Ophthalmol. 1983;101:1399–1401. doi: 10.1001/archopht.1983.01040020401013. [DOI] [PubMed] [Google Scholar]
- 12.Mukai N, Lee PF, Oguri M, Schepens CL. A long-term evaluation of silicone retinopathy in monkeys. Can J Ophthalmol. 1975;10:391–402. [PubMed] [Google Scholar]
- 13.Haut J, Ullern M, Chermet M, Van Effenterre G. Complications of intraocular injections of silicone combined with vitrectomy. Ophthalmologica. 1980;180:29–35. doi: 10.1159/000308952. [DOI] [PubMed] [Google Scholar]
- 14.Alexandridis E, Daniel H. Results of silicone oil injection into the vitreous. Dev Ophthalmol. 1981;2:24–27. doi: 10.1159/000395298. [DOI] [PubMed] [Google Scholar]
- 15.Foerster MH, Esser J, Laqua H. Silicone oil and its influence on electrophysiologic findings. Am J Ophthalmol. 1985;99:201–206. doi: 10.1016/0002-9394(85)90233-8. [DOI] [PubMed] [Google Scholar]
- 16.Armaly MF. Ocular tolerance to silicones. I. Replacement of aqueous and vitreous by silicone fluids. Arch Ophthalmol. 1962;68:390–395. doi: 10.1001/archopht.1962.00960030394013. [DOI] [PubMed] [Google Scholar]
- 17.Doslak MJ. Quantitative analysis of the insulating effect of silicone oil on the electroretinogram. Med Biol Eng Comput. 1989;27:254–259. doi: 10.1007/BF02441482. [DOI] [PubMed] [Google Scholar]
- 18.Thaler A, Lessel MR, Gnad H, Heilig P. The influence of intravitreously injected silicone oil on electrophysiological potentials of the eye. Doc Ophthalmol. 1986;62:41–46. doi: 10.1007/BF00140545. [DOI] [PubMed] [Google Scholar]
- 19.Sakai T, Calderone JB, Lewis GP, Linberg KA, Fisher SK, Jacobs GH. Cone photoreceptor recovery after experimental detachment and reattachment: an immunocytochemical, morphological, and electrophysiological study. Invest Ophthalmol Vis Sci. 2003;44:416–425. doi: 10.1167/iovs.02-0633. [DOI] [PubMed] [Google Scholar]
- 20.Guérin CJ, Anderson DH, Fariss RN, Fisher SK. Retinal reattachment of the primate macula. Photoreceptor recovery after short-term detachment. Invest Ophthalmol Vis Sci. 1989;30:1708–1725. [PubMed] [Google Scholar]