Abstract
Background: Evidence-based best practices for incorporation into an optimal multilevel intervention for suicide prevention should be identifiable in the literature. Aims: To identify effective interventions for the prevention of suicidal behavior. Methods: Review of systematic reviews found in the Pubmed, Cochrane, and DARE databases. Steps include risk-of-bias assessment, data extraction, summarization of best practices, and identification of synergistic potentials of such practices in multilevel approaches. Results: Six relevant systematic reviews were found. Best practices identified as effective were as follows: training general practitioners (GPs) to recognize and treat depression and suicidality, improving accessibility of care for at-risk people, and restricting access to means of suicide. Although no outcomes were reported for multilevel interventions or for synergistic effects of multiple interventions applied together, indirect support was found for possible synergies in particular combinations of interventions within multilevel strategies. Conclusions: A number of evidence-based best practices for the prevention of suicide and suicide attempts were identified. Research is needed on the nature and extent of potential synergistic effects of various preventive activities within multilevel interventions.
Keywords: review, suicide prevention, depressive disorder, restriction of means, multilevel approach
Introduction
Scale of Suicide Problem
In 1984, the member states of the World Health Organization’s (WHO) European region highlighted suicide reduction as one of their prime health policy goals (Lopez, Mathers, & Ezzati, 2006). More than 58,000 people die by suicide in the European Union every year – one of the highest suicide rates in the world (WHO, 2003). Almost 900,000 lives are lost annually through suicide worldwide, constituting 1.5% of the global burden of disease (Lopez et al., 2006). Nonfatal suicidal acts are believed to occur at least 10 times more frequently than fatal suicides (Nock et al., 2008). The economic costs of suicide are also high, with estimates in Ireland and Scotland suggesting average costs of EUR 1.5 million per completed suicide (Kennelly, 2007; McDaid & Kennelly, 2010). These factors make suicide a major public health concern.
Depression as a Key Risk Factor for Suicide
One European study has shown that many suicides occur in the context of psychiatric illness, with a population-attributable risk for lifetime suicide attempts put at 28% in major depressive disorder (MDD) (Bernal et al., 2007). This underlines the importance of effective recognition and treatment. According to a WHO study (Lopez et al., 2006), depression tops the list of disorders contributing to the global burden of disease. Future projections expect it to account for a growing share of the European burden of disease. Despite the availability of effective treatments, only about 21% of primary care patients with MDD receive optimal care (Al Windi, 2005; Fernandez et al., 2007). A number of factors are to blame for the underrecognition and consequent undertreatment of depression. These include deficits in primary care, such as inadequate knowledge about diagnosis and treatment (Tylee & Walters, 2007), competing demands (Rost et al., 1999) and negative public and professional attitudes (Botega & Silveira, 1996; Dowrick, Gask, Perry, Dixon, & Usherwood, 2000; Goldman, Nielsen, & Champion, 1999). Further causes are mental health illiteracy in depressed people (Jorm et al., 2000), reluctance to seek help (in part due to fear of stigmatization) and poor treatment compliance (Goldney, Fisher, Wilson, & Cheok, 2002). Programs to reduce suicide rates have been implemented (Fleischmann et al., 2008; Rutz, von Knorring, & Walinder, 1992; WHO, 2003), some of which appear to be more effective than others.
Synergistic Effects of Individual Activities Within Multilevel Interventions
Several reviews indicate that multilevel interventions should be the strategy of choice for suicide prevention (Althaus & Hegerl, 2003; Mann et al., 2005; Rihmer, Kantor, Rihmer, & Seregi, 2004). Evaluation of multilevel strategies and their components is a sine qua non for understanding their effectiveness, but little research has been done as yet. Multilevel strategies target several populations or several levels within healthcare systems, such as public health or primary care, or they include interventions with more than one focus, such as pharmacotherapy and psychotherapy. Key effective elements in such strategies must be identified, and additional evidence-based interventions need to be found for possible inclusion. As policymakers require up-to-date information that is readily translatable into practice, evaluation research should take place on a periodic basis.
It is also important to be aware of any synergistic potentials in multilevel interventions, as synergistic combinations ought to be part of recommended best practices. Positive synergistic effects occur where the effects of the combined interventions are more than the sum of the two (or more) parts. Synergism could be crucial to creating a critical impact in multilevel interventions. No systematic reviews are available so far that identify such positive synergistic elements.
Our assessment of systematic reviews of best practice therefore serves to identify evidence-based interventions that might be included as key elements in multilevel strategies for suicide prevention, and to identify potentials for synergism between such elements.
Method
Design
The focus of our review required us to obtain systematic reviews exploring different aspects of suicide prevention, levels of interventions and target populations. Our approach was systematic in its methodology, risk-of-bias assessment, data extraction methods, and reporting (Elliot, Crombie, Irvine, Cantrell, & Taylor, 2004).
Procedure
In 2008, a European Union-funded FP7 project entitled Optimizing Suicide Prevention Interventions (OSPI) (Hegerl et al., 2009), building on the work of the European Alliance Against Depression (EAAD) (Hegerl et al., 2008), began preparations for an optimal suicide prevention program in four European countries (Germany, Hungary, Ireland, and Portugal). One of its initial activities was to establish the best-practice interventions needed for inclusion. After consulting with OSPI partners to define aims and objectives, our working group set out to conduct its review of systematic reviews of effective suicide prevention interventions, defining the search terms and selection criteria in accordance with the PRISMA guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009). After analysis and synthesis, we summarized core elements of successful best practices. Levels of evidence were graded using criteria set by the Oxford Centre for Evidence-Based Medicine (CEBM) (Phillips et al., 2009).
Eligibility Criteria, Information Sources, Search
Potentially eligible reviews were identified by searching Pubmed/Medline, the Cochrane Database, and the Database of Abstracts of Reviews of Effectiveness (DARE) at the British National Health Service’s Centre for Reviews and Dissemination; the latter is a database of systematic reviews, including Cochrane reviews. We used medical subject heading (MeSH) terms and free text terms for suicid*, prevent* and review*. As an additional method of review identification, we checked the reference lists of selected articles to detect any missed studies, using the snowballing technique. We also made a hand search of key authors. Working group members checked their personal files for relevant publications and experts were consulted to uncover additional reviews not yet found. The search confined itself to the time frame from January 1964 to January 2011. No language or geographical restrictions were imposed.
Study Selection, Data Collection Process
Our inclusion criteria specified systematic reviews evaluating strategies to prevent suicidal behavior which focused on two or more levels of intervention or two or more target populations. Reviews were considered systematic if, according to their literature review protocol, they conducted a systematic search and reported the findings in line with the QUORUM (Moher et al., 2009) or PRISMA (Moher, Schulz, & Altman, 2001) guidelines. In the first stage of selection, three reviewers (VP, SR, and AT) evaluated whether each study met the inclusion criteria mentioned above on the basis of the title and abstract of the article. The reviewers worked independently and had the same level of seniority. Studies that clearly did not satisfy the criteria were excluded. If a study seemed eligible for inclusion or in case of doubt, the full text was retrieved. In the second stage, the same reviewers independently assessed the full articles. Disagreements regarding inclusion status were resolved by discussion between reviewers. If an agreement could not be reached the study was to be excluded. No study had to be excluded because of lack of consensus. In a third stage, the working group and other OSPI members were consulted to identify any missing reviews.
Risk-of-Bias Assessment
Risk of bias was determined by checking whether the systematic reviews included qualitative assessments of the primary studies they analyzed, according to generally accepted guidelines such as the Cochrane (Cochrane CC:DAN working group, 1998) or CEBM (Phillips et al., 2009) quality criteria. If a review did not fulfill these criteria, it was to be excluded. The risk-of-bias determinations were made by a fourth assessor (CFC), who consulted the OSPI partners. No study had to be excluded.
Summary Measures
Interventions had to be described in sufficient detail to enable us to classify them as suicide-prevention programs. They were to focus on more than one group of participants or mental disorders, or have been performed on at least two levels. The focus could be on preventing either suicides or suicide attempts. Outcome measures were to include the impact of interventions on the number of completed or attempted suicides.
Synthesis of Results
After consultation with OSPI partners, it was agreed to analyze the reviews systematically, including identification of:
The patient or participant groups and the mental disorders targeted by each intervention;
The interventions and their effect sizes;
Whether attempts were made to assess synergistic effects;
Whether reviews came to similar conclusions about recommendable prevention strategies.
We (DV, CFC) then formulated recommendations for best practices based on the outcomes of these analyses, after securing input from OSPI partners. Results were summarized in a data extraction table (Table 3).
Table 3. Key elements of best practice interventions for suicide prevention.
| LEVEL 1. Cooperation with general practitioners (GPs) to improve their knowledge and abilities in detecting and managing suicide risks | |
| Training content | Use of screening tools for detecting depression and suicide risks, e.g., PHQ-9 |
| Information about treating depression and suicidal patients according to existing national guidelines | |
| Information about different forms of pharmacological treatment and their relation to decreased suicide risk | |
| Knowledge of populations vulnerable to suicide risk | |
| Training format | Embedded in continuing medical education or professional supervision sessions |
| Provided on a periodic basis | |
| 3 to 4 sessions of up to 3 h | |
| Embedded in the GPs’ primary care organizations (vital both to facilitate implementation and ensure sustainability) | |
| GPs engaged in planning the training | |
| Possibly with a basic component for a large group and secondary sessions in smaller groups with role plays | |
| Tools to facilitate GPs | Telephone helpline providing psychiatric consultation for GPs |
| Information materials for different vulnerable populations | |
| Guidelines containing options for referring patients at risk of self-harm to relevant local mental health services | |
| LEVEL 2. Public awareness campaigns and cooperation with local media to improve public attitudes on depression and facilitate help seeking (suicidality not the main focus due to possible contrary effects) | |
| Tools to facilitate public campaign | Posters, placards, leaflets and brochures with information about help available locally, self-tests, warning signals and treatment options |
| Special leaflets for vulnerable groups | |
| Keyring torch showing youth telephone helplines, distributed by youth services | |
| Websites with information about depression, suicide and treatment options, contact information for local mental health services and announcements of regional educational activities like open days, lectures and seminars | |
| Cinema information trailer | |
| Public events, such as Jogging Against Depression | |
| Opening ceremony in public campaign | |
| Media guidelines | Responsible professional media coverage: avoiding sensationalism and glorification, martyrification and mystification of suicide; avoiding detailed descriptions of suicide methods used; focusing on treatability of mental disorders and preventability of suicide |
| Training of journalists and editors in application of guidelines | |
| Media blackouts on suicides | |
| LEVEL 3. Training sessions for gatekeepers, multipliers and community facilitators on the detection of depression and suicide risks. Community facilitators can play key roles in early detection within different target populations and act as multipliers in disseminating knowledge about depression and suicide risks. They include teachers, priests, geriatric care providers, journalists, pharmacists and police, as well as telephone hotlines, businesses, social services, entrepreneurs and youth workers. | |
| Training content | Theoretical aspects of depression and suicide (e.g., symptoms, treatment) |
| Practical elements (e.g., how to talk about suicidality, detect suicidality, handle an acute suicidal crisis) | |
| What to do if treatment needs are encountered | |
| Populations vulnerable to suicide | |
| Presentation and distribution of information materials for various vulnerable populations | |
| LEVEL 4. Services and self-help activities for high-risk groups to facilitate access to professional help | |
| Targeted information materials (e.g., leaflets for people in bereavement or survivors of suicide victims) providing concrete advice and help | |
| Medical emergency card for high-risk individuals, showing a contact telephone number and recommending steps to take in an acute crisis, including telephone numbers of important local services | |
| Support for self-help activities | |
| Psychoeducation sessions for relatives of patients at risk of suicidal behavior to raise awareness of suicide risk factors | |
| LEVEL 5. Restriction of access to potential lethal means for suicide: nationwide documentation of available means and communication to policymakers | |
| Firearm control legislation, restrictions on pesticides, detoxification of domestic gas | |
| Restrictions on prescription and sale of barbiturates, packaging analgesics in blister packets only and reducing number of tablets per package | |
| Mandatory use of catalytic converters in motor vehicles, construction of barriers at jumping sites | |
| Use of new, lower-toxicity antidepressants | |
| LEVEL 6. Improvement of access to care | |
| Improvement of acute, continuation and maintenance treatment, including psychiatric hospitalization, for people at risk | |
| Aftercare and easy entry to care for suicide attempters | |
| Improvement of care to individuals with recurrent or chronic psychiatric disorders | |
| Telephone support and other forms of contact and emotional support for persons known to have engaged in suicidal behaviors or suicidal ideation | |
Results
Study Selection
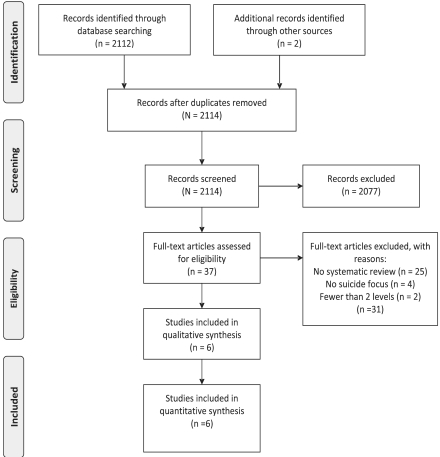
The search strategy yielded 2114 citations, 6 of which (Dumesnil, & Verger, 2009; Isaac et al., 2009; Leitner, Barr, & Hobby, 2008; Mann et al., 2005; Pignone et al., 2002; Tarrier, Taylor, & Gooding, 2008) were reviews satisfying our PRISMA-based (Moher et al., 2009) inclusion criteria. This process is represented in Figure 1. The reviewers were consistent in their decision to include all the systematic reviews in the qualitative synthesis. Five systematic reviews were identified by the team of reviewers, and one systematic review (Leitner et al., 2008) was added after consultation with the working group and members of the OSPI Consortium. Also, for this additional review, all reviewers were consistent in the evaluation that the study met the eligibility criteria for inclusion.
Figure 1. PRISMA 2010 flow diagram.
Characteristics of the Analyzed Studies
Study designs and risk of bias are indicated in Table 1. All six selected reviews met our quality criteria; none of the selected reviews had to be excluded.
Table 1. Risk of bias.
| Article | Specific research question | Appropriate search | Specified search terms | Inclusion/exclusion criteria | Clarity of individual study findings | Analysis of study findings | Valid conclusions |
|---|---|---|---|---|---|---|---|
| Note. *No clear information available on this point. | |||||||
| Mann et al. (2005) | To examine evidence for the effectiveness of specific suicide-prevention interventions and make recommendations for future prevention programs and research | Yes | Yes | Yes | Yes | Yes | Yes |
| Leitner et al. (2008) | To provide a comprehensive overview of the known effectiveness of interventions to prevent suicide, suicidal behavior, and suicidal ideation, both in key risk groups and in the general population | Yes | Yes | Yes | Yes | Yes | Yes |
| Isaac et al. (2009) | To review the state of evidence on gatekeeper training for suicide prevention and propose directions for further research | Yes | Yes | * | No | * | * |
| Dumesnil et al. (2009) | To summarize data on the impact and effectiveness of campaigns for depression and suicide awareness | Yes | Yes | Yes | Yes | Yes | Yes |
| Williams et al. (2009) | To assess the health effects of routine primary care screening for MDD in children and adolescents aged 7–18 | Yes | Yes | Yes | Yes | Yes | Yes |
| Tarrier et al. (2008) | To assess whether cognitive-behavioral therapy reduces suicidal behavior | Yes | Yes | Yes | Yes | Yes | Yes |
All strategies involved public health and/or clinical approaches aiming at suicide prevention either in general populations or in specific subgroups (including children and adolescents, previous suicide attempters and psychiatric patients). As the reviews focused on differing modes of intervention, there was no substantial overlap between the primary studies analyzed. The reviews covered universal and indicated approaches, ranging from public-health interventions targeting whole communities to individually focused psychopharmacological or psychotherapeutic interventions.
Synthesis of Results
The working group first examined the interventions described in the reviews to identify which intervention levels and target populations were included. The results are described below and summarized in Table 2. If potential synergies were detected within particular strategies, that was indicated. Levels of evidence were determined. The data extraction table indicates the effectiveness of the identified interventions, including any potential synergistic effects we detected. The reviews themselves made no explicit evaluations of synergistic effects within multilevel interventions.
Table 2. Suicide prevention strategies identified in systematic reviews and their effects on outcomes in terms of attempted or completed suicides.
| Author of systematic review/Number of studies | Level of intervention | Target populations | Effect size | Highest level of evidence | Synergism |
|---|---|---|---|---|---|
| Notes. Based on the Oxford Centre for Evidence-Based Medicine (CEBM) levels of evidence: 1A = systematic review of RCTs; 1B = individual RCT; 2A = systematic review of cohort studies; 2B = individual cohort study, low-quality RCT; 2C = ecological studies; 3A = systematic review of case-control studies; 3B = individual case-control study; 4 = case-series, poor-quality cohort and case-control studies. *No information. | |||||
| Mann et al. (2005) | Awareness and education | General public | No detectable effect | 2B | Mentioned, but no assessment |
| SRs n = 10, RCTs n = 18, Cohorts n = 24, Ecological n = 41 | |||||
| GPs | Modest | 2B | * | ||
| Gatekeepers | Modest | 2B | * | ||
| Media | Modest | 2B | * | ||
| Screening | Adults in primary care | No outcomes on attempted/completed suicide | 2A | * | |
| Pharmacotherapy | Adolescents | Inconclusive | 1A | * | |
| Adults | Modest effect in adults | 1A | * | ||
| Psychotherapy | Not specified | Inconclusive | 1A | * | |
| Follow-up care after suicide attempts | Suicide attempters | Modest effect | 2B | * | |
| Restriction of means | Not specified | Modest effect | 2C | * | |
| Tarrier et al. (2008) | Individual cognitive-behavioral therapy | Adults | Highly significant effect in reducing suicidal behavior when compared to minimal treatment or treatment as usual (but not when compared to other active treatment) | 1A | * |
| RCTs n = 28 | |||||
| Adolescents | No effect | ||||
| Isaac et al. (2009) | Gatekeeper training for suicide prevention | GPs | Rate decrease from 19.7 to 7.1 per 100,000 | 2B | * |
| Cohorts n = 6 | |||||
| 24% decrease in attempted and completed suicides | 2B | * | |||
| Lower rate (ns) | 2B | * | |||
| Air force personnel | 33% relative risk reduction in suicide rate | 2B | * | ||
| Adolescents | 73% decrease in mean number of attempts | 2B | * | ||
| Dumesnil et al. (2009) | Awareness campaigns | Media | No effect | 2B | Mentioned, but no assessment |
| Cohorts n = 2, RCTs n = 11 | |||||
| Gatekeepers | No outcomes for suicide reduction | 2B | Mentioned, but no assessment | ||
| General public | Reduced suicide rates in 1 of 9 programs | 2B | Mentioned, but no assessment | ||
| Williams et al. (2009) | Primary-care screening with follow-up treatment for MDD (SSRI and/or psychotherapy) | Children and adolescents aged 7–18 | No data describing health outcomes in screened and unscreened populations | 1A | * |
| RCTs of screening and treatment vs no screening n = 0, Diagnostic accuracy studies n = 9, RCTs of treatment with SSRIs or psychotherapy n = 20, RCTs reporting adverse events of SSRIs n = 9 | |||||
| Leitner et al. (2009) | |||||
| 200 primary empirical studies, 37 systematic reviews | |||||
| Ethnic minority children | Effect | 3A | * | ||
| Community-wide health program | Community | Effect | 3A | * | |
| Media | Effect | 3A | * | ||
| Inpatient and outpatient treatment | Depressed patients | Effect | 3A | * | |
| SSRI, SNRI, dual-action antidepressants, high-potency anxiolytics, mood stabilizers, lithium | Bipolar and unipolar depressed patients | Effect | 3A | * | |
| SSRIs | Depressed elderly | Effect | 3A | * | |
| Atypical antipsychotics | Psychotic patients | Effect | 3A | * | |
| Intermediate care service | People in contact with criminal justice system | Effect | 3A | * | |
| Restriction of means | Effect | 3A | * | ||
A list of identified best practices is provided in Table 3. Multilevel strategies target several populations or several levels within healthcare systems, such as public health or primary care, or they include interventions with more than one focus, such as pharmacotherapy and psychotherapy.
Intervention Levels
Primary Care
At the primary-care level, an improvement in depression recognition and suicide risk evaluation by GPs was found to be an important component of suicide prevention (see Table 3) (Leitner et al., 2008; Mann et al., 2005). The recent systematic review by Isaac et al. (2009) has confirmed that increased antidepressant prescribing rates and significantly reduced suicide rates are reflected in studies examining depression recognition and treatment in relation to suicidal behavior after GP education programs. The mechanism here is generally assumed to involve improved recognition and treatment of underlying mental disorders (Mann et al., 2005). Psychiatric disorders are present in at least 90% of suicides, and up to 80% of such cases have gone untreated at the time of death (Lopez et al., 2006). Studies also indicate that pharmacological treatment can contribute significantly to decreased suicidal risk in individuals with various mental disorders (Mann et al., 2005). The new generation of psychotropics (selective serotonin reuptake inhibitors, SSRIs; serotonin-norepinephrine reuptake inhibitors, SNRIs; dual-action antidepressants; high-potency anxiolytics; atypical antipsychotics) has the potential for safe and effective treatment either in the short or the long term. Many different forms of psychotherapy were evaluated in reviewed studies, yet with one exception (cognitive-behavioral therapy) none were to be found successful in reducing suicide risks (Mann et al., 2005). The review by Tarrier et al. (2008) reported a highly significant overall effect of cognitive-behavioral therapy in curbing suicidal behavior. Subgroup analysis revealed a significant treatment effect for adults (but not for adolescents) in comparison to treatment as usual or minimal treatment, but not in comparison to other active treatment; the authors caution against overoptimistic interpretation and warn of possible publication bias.
Population Level: General Public and Gatekeepers
In examining public awareness as a level of preventive intervention, Mann et al. (2005) note that public education campaigns aim mostly at improving suicide risk recognition and help-seeking behavior by fostering a clearer understanding of causes and risk factors for suicidal behavior, particularly mental illness. Public awareness approaches also seek to reduce the stigmatization of mental illness and suicide. Although awareness raising is a widely employed strategy, systematic reviews yield conflicting results in terms of attempted and completed suicides. Mann et al. (2005) reported no detectable effects of public awareness on the primary outcome measure of reduced rates of suicidal acts – and also not on intermediate measures like increased treatment seeking or antidepressant use. This was possibly because educating journalists and establishing of media guidelines for reporting suicide have had mixed results (Goldney, 2005; Mann et al., 2005). Dumesnil and Verger (2009) reported mixed overall results and suggested that the sustainability of outcomes should be evaluated. They also believe that more robust outcomes might be achieved by combining the public awareness intervention with other interventions at regional levels. Isaac et al. (2009) reported clear and significant reductions in attempted and completed suicides in several studies evaluating the training of gatekeepers, but they emphasize that such interventions were generally part of more complex strategies, making it difficult to ascertain their specific impacts.
High-Risk Groups
In public health terms, an approach to suicide prevention outlined by Mann et al. (2005) could be used to screen for people at risk of suicidal behavior and depression. Thus far, no published studies have evaluated the effectiveness of screening for suicide risk in adults or children and adolescents in primary care (Pignone et al., 2002; Williams, O’Connor, Eder, & Whitlock, 2009). Although a review of depression screening studies did not find evidence that isolated routine screening in primary care improves depression care in the absence of adequate follow-up care (Gilbody, Sheldon, & House, 2008), there is enough evidence of improved depression outcomes if such resources are available, or when treatment is offered only to those individuals with scores above certain thresholds (Gilbody, House, & Sheldon, 2005). Given these findings, it may be premature to include screening in primary-care settings as a best-practice component of suicide prevention. Yet research to improve case finding of at-risk individuals is certainly indicated; viable instruments like the Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer, & Williams, 2001) are available, as are effective treatments (Bower, Gilbody, Richards, Fletcher, & Sutton, 2006).
Restricting Access to Means of Suicide
Means restriction was identified by Mann et al. (2005) as a further important element in suicide prevention. Suicide deaths as a consequence of methods with high lethality have been shown to decrease after access to them is restricted (Goldney, 2005; Mann et al., 2005; Rihmer et al., 2004).
Targeted Populations
Psychiatric Patients
Psychiatric patients are most definitely one of the high-risk groups for suicidal behavior. Consequently, as pointed out by Mann et al. (2005), the improvement of acute, continuation, and maintenance treatment, including psychiatric hospitalization, for people with recurrent or chronic psychiatric disorders (and particularly those who have already attempted suicide) has preventive potential. According to the review by Leitner et al. (2008), telephone support and other forms of contact and emotional support provided to people known to have engaged in suicidal behavior or suicidal ideation significantly mitigates their risk of suicidal behavior.
Children and Adolescents
Suicide prevention programs for children and adolescents have had mixed results in terms of effectiveness and impact. For children in particular, there is some limited evidence that certain interventions – including pharmaceutical, psychotherapeutic, behavioral and staff- or parent-training initiatives – may be effective in reducing suicidal behavior and ideation. Studies show that while knowledge about suicide improves, there are both beneficial and harmful effects in relation to help-seeking, attitudes, and peer support. School curriculum-based programs enhance knowledge and improve attitudes about mental illness and suicide, but there is insufficient evidence that they actually prevent suicidal behavior. Indeed, they may even disturb high-risk adolescents and make them more prone to harmful behaviors, especially if they do not afford direct access to care. It is suggested that awareness raising combined with easier access to care may have synergistic effects, but this has yet to be confirmed in children and adolescents. Improving problem-solving and stress-coping abilities and resilience appear to enhance hypothesized protective factors, but the effects on suicidal behavior remain unevaluated (Mann et al., 2005).
Older People
As noted by Leitner et al. (2008), treatment studies of SSRIs in older adult populations report reductions in attempted suicides following psychopharmacological interventions. The authors also point to reductions in suicide after the provision of palliative care to older people with cancer. Community-based support programs for older people in rural areas have also reportedly decreased suicide incidence. A recent US Food and Drug Administration analysis of suicidality and antidepressants in adults is worth noting too, as it found some signs of protective effects of SSRIs in people older than about 25, but not in younger people (Khan, Khan, Kolts, & Brown, 2003).
Ethnic Minorities
Successful interventions for ethnic minorities identified in the systematic review by Leitner et al. (2008) include ethnically tailored, community-wide public health programs; video-focused educational interventions to modify family expectations regarding self-harm; and school-based initiatives to train school staff and pupils to respond to suicidal crises.
Discussion
Findings
This review of six systematic reviews on suicide prevention yielded evidence for the actual or potential effectiveness of several types of preventive interventions: (1) the training of GPs in the recognition and treatment of mental disorders, especially unipolar and bipolar depression; (2) awareness campaigns, provided that a clear fast track to treatment is available; (3) the training of gatekeepers and community facilitators in recognizing suicidality and helping at-risk people to access appropriate services; (4) improvement of healthcare services targeting people at risk, including organizational measures such as making adequate inpatient and outpatient aftercare available to people who have attempted suicide; (5) the training of journalists in responsible reporting about suicide or the imposing of media blackouts; (6) restricting public access to lethal means of suicide.
The last of these measures could be highly effective and should probably be part of any multilevel intervention; wide variations in outcomes might be expected, however, as the measures taken may differ among countries (Värnik et al., 2008, 2009). If national multilevel approaches are adopted, it is crucial to ensure that adequate suicide surveillance data are brought to the attention of policymakers on a regular basis, enabling them to devise responsive measures. There might be scope here both for national or pannational measures, such as limiting package sizes for medications, and for more locally specific actions, such as revising laws on the accessibility of firearms in certain jurisdictions.
None of the studies we reviewed here included outcome measures to evaluate synergistic effects of the separate types of interventions analyzed. As seen in Table 2, some synergistic mechanisms were alluded to, but they were not evaluated as such. Some potentially beneficial suggestions were made, such as Dumesnil’s (Dumesnil et al., 2009) proposal to combine interventions in specific regions to obtain better outcomes and Mann’s (Mann et al., 2005) reference to complex interventions. The systematic reviews thus provide no firm evidence that multilevel interventions are a more effective approach, and more research on them is urgently needed.
The literature and findings so far suggest that an integrated strategy that includes community facilitator training, GP training and ready access to mental healthcare offer the greatest potential for synergism. These might also be combined with more sociological strategies, such as policies targeting the media or restricting access to means for self-harm. One local intervention program for which there is some evidence of effectiveness was the Nuremberg Alliance Against Depression (NAD). This multilevel approach showed a clear effect in terms of reducing suicides and suicide attempts, and it also improved the care of depressed patients, in a prepost design (Hegerl, Althaus, Schmidtke, & Niklewski, 2006). Comprehensive, integrated approaches like these, however, have not yet been evaluated in a controlled design, although attempts to do so are currently underway (Marušic, 2008). On the basis of these positive outcomes, the NAD approach was rolled out across Europe in the European Alliance Against Depression (EAAD), which resulted in the implementation of a four-level, community-based intervention in 17 countries (Hegerl & Wittenberg, 2009; Hegerl et al., 2006). This includes (1) cooperation with general practitioners and pediatricians, (2) public awareness campaigns and cooperation with local media, (3) cooperation with local actors such as healthcare professionals, geriatric care providers, counselors, and religious leaders, who play important roles as multipliers in disseminating knowledge about depression, particularly to children and adolescents, (4) targeted interventions for high-risk groups such as young people in adolescent crisis and people who have attempted suicide. All four types of interventions are being implemented concurrently in a multilevel approach. Independent thereof, several countries also developed and implemented systematic multilevel strategies involving national-level depression treatment programs (De Jong et al., 2009; Ijff et al., 2007; Katon & Seelig, 2008; Meredith et al., 2006; Van der Feltz-Cornelis, 2009) or national action plans for suicide prevention (Austria, 2008; Belgium, 2009; Northern Ireland, 2006; Scotland, 2002; Switzerland, 2005; The Netherlands, 2007; UK, 2002; Wales, 2008). These are based on regional or national networks and are multidisciplinary in nature.
Strengths and Limitations of This Review
Among the limitations is that we were unable to generate effect sizes because of the lack of meta-analyses in the original systematic reviews. We could therefore only describe the evidence. Yet all evidence points in the same direction: Suicide prevention interventions can be effective at several levels. Although researchers have pointed out the methodological difficulties of demonstrating effects of an intervention on suicidal behavior in a controlled design, the reviews examined here highlighted several types of interventions that appear to reduce suicide rates.
Another key limitation of our review is its pragmatic reliance on studies identified in previous systematic reviews. Some new primary studies may have thereby been missed. Limitations in the scope of the databases examined may have also caused us to overlook reviews focusing on infrastructure change, such as improvements in bridge and railway safety. We hope to have minimized such limitations by using DARE and Cochrane, high-quality databases on systematic reviews. A further limitation is that the studies examined here were mostly conducted in Europe, thus potentially limiting the relevance for other regions.
Although several of the systematic reviews discussed here advocated multilevel approaches, they made no systematic attempt to identify possible synergies between interventions. Their evidence does suggest that preventive interventions at several levels can be effective against suicidal behavior. Some reviews suggested combinations of interventions with potential synergistic effects. The relative impact of interventions within multilevel approaches still needs exploring.
On the basis of the evidence of effectiveness established so far, the strongest impact can probably be expected from GP training, facilitating access to care for at-risk people and restricting access to means of suicide. Obviously this is a topic for future research. Another topic would be to explore approaches that would work in countries where GPs do not have gatekeeping functions, that is, where primary care plays a less prominent role and individuals can directly access specialist care; a specific question is who needs to be trained in countries without primary care-led systems.
It is also worth noting that the systematic reviews discussed here do not take account of the recent debate about associations between SSRI use and rising or falling suicide rates, a discussion that has only really emerged in recent years; Mann et al. (2005) point out the need for further research on this issue.
Research Implications
It follows from our analysis that groups at risk of suicide would be more likely to receive adequate mental healthcare if a regional or supraregional approach were adopted that combines awareness campaigns in schools and in the general public with the training of community facilitators in closest contact with at-risk groups. Organizational interventions such as collaborative care arrangements (Adli, Bauer, & Rush, 2006; Bower et al., 2006) would facilitate entry into care (De Jong et al., 2009), and GP training would improve both the recognition of risk and the quality of care. Restricting access to potentially lethal means for committing suicide might have an added beneficial effect. Concurrent awareness campaigns might encourage individuals who are contemplating suicide to seek help. A combined approach should thus be more effective than the sum of its parts. In view of the lack of research so far into synergistic effects, further evaluation is needed on strategies that combine these interventions. One way to produce synergistic effects would be to begin with a strong public awareness element, which might later facilitate cooperation with GPs and other multipliers. Yet awareness raising may only be useful if support is provided in finding help. An example will show how synergistic effects might be generated. A public awareness campaign motivates a depressed individual to discuss depressive symptoms with a GP, which in turn motivates the GP to obtain more training on the issue. Such training would be available under the multilevel approach. Yet training alone may not be sufficient. Judging from a recent debate, GPs are still unable to reliably identify and treat depressed patients despite decades of training on the issue. They may therefore need additional support above and beyond such training. In a multilevel approach, the public awareness campaign, supplemented by materials such as a waiting-room poster on depression, may make it easier for a GP to suggest a possible diagnosis of depression to patients who have come for other reasons, and to discuss and start treatment. Another multilevel strategy would be to combine such a public campaign with secondary prevention measures such as screening for and helping high-risk individuals and providing aftercare for individuals bereaved by suicide, as is now being evaluated in Japan (Ono et al., 2008).
Screening for disorders like depression might indeed be useful. Detection and treatment of moderately severe cases of major depressive disorder in primary care settings has proved effective in reducing depressive symptoms, provided appropriate resources are available to improve the quality of routine care (Gilbody et al., 2005). Screening for other conditions such as psychotic disorders has not yet been shown to be effective. Thus, the specific effectiveness of screening in reducing suicide rates in the public health domain has yet to be established and requires further research.
Careful, well-conducted research is needed, as emphasized in the WHO study on the mental health treatment gap. It explicitly highlights suicide prevention strategies that combine interventions from inside and outside the health sector and calls for an innovative, comprehensive multisectoral approach, including health sectors as well as nonhealth sectors such as education, labor, police, justice, religion, law, politics, and media.
Beyond measuring the impact of such strategies on suicide rates, future studies of multilevel interventions must also assess the cost-effectiveness of proposed measures and their effects on intermediate outcomes, such as rates of GP-diagnosed major depression and antidepressant prescription rates. The ongoing OSPI study provides an opportunity to address these questions (Hegerl et al., 2009).
Contributions of Authors
CFC wrote the article, updated the literature search and study selection, performed the risk-of-bias assessment, and completed the data extraction and the list of best practices. VP, AT, and SR performed the initial search and selection of reviews, and discussed approaches to analyzing the systematic review articles, provided comments, and approved the final version. VC and DM helped with the search, checked the selection of reviews, gave comments, and approved the final version. VP performed data extraction and wrote parts of the article, gave comments, and approved the final version. DV assembled the list of best practices resulting from the data extraction, gave comments, and approved the final version. AI and MM recommended relevant reviews and action plans, commented on previous versions, and approved of the final version. MS, RO, CVA, GS, RG, and UH gave comments and approved the final version.
Disclosures in the Past 12 months: CFC
Her employer, the Trimbos Institute, was reimbursed by Eli Lilly and Company for investigator-initiated research. The funders had no influence on the content of lectures, on data assemblage, and analysis nor on the writing of protocols, reports, or other publications deriving from the present research project. CFC was involved in development of a Dutch multidisciplinary guideline, funded by the Netherlands Ministry of Health and the Dutch Psychiatric Association. UH has worked as an adviser for Lilly, Sanifi-Aventis, and Lundbeck. The other authors report no conflicts of interest.
Acknowledgments
This research received funding from OSPI-Europe as part of the European Community’s Seventh Framework Program (FP7/2007–2013) under grant agreement 223138. The authors wish to thank Ella Arensman, James Coyne, and Maria Kopp, for their advice and recommendations in preparing the article.
About the authors
Christina van der Feltz-Cornelis, MD PhD, psychiatrist and epidemiologist, is Professor of Social Psychiatry in the Department of Developmental and Clinical Psychology at Tilburg University, The Netherlands. She heads the Research Program Diagnosis and Treatment and the Depression Initiative at the Trimbos Institute, is the Dutch national representative in EAAD, and participates in OSPI, an EU-funded initiative for suicide prevention.
Marco Sarchiapone, MD PhD, is Associate Professor of Psychiatry at the University of Molise, Italy, as well as a psychiatrist and psychoanalyst. He is Secretary General of the Section on Suicidology of the World Psychiatric Association and co-chair of the Section on Suicidology and Suicide Prevention of the Association of European Psychiatrists.
Vita Postuvan, MSc, is a psychologist preparing her PhD thesis on the topic of suicide survivors. She has been involved in suicide research and mental health promotion, treatment, and intervention for several years. She has worked internationally in the field of suicide prevention.
Daniëlle Volker, MSc, is Junior Researcher in the Research Program Diagnosis and Treatment at the Trimbos Institute, The Netherlands. She works as a research associate in EAAD and OSPI. She obtained her masters degree in clinical psychology at Leiden University in 2007.
Saska Roskar, PhD in psychology, is employed at the Institute of Public Health of Slovenia. She is engaged in a number of mental health projects, with a special interest in depression and suicide. She is national representative for Slovenia in the International Association for Suicide Prevention (IASP).
Alenka Tančič, BA in psychology, works at the Institute of Public Health of Slovenia. She is engaged in several projects in the field of mental health, with a special interest in depression and suicide. She is also employed part-time as a research assistant at the University of Primorska.
Vladimir Carli, MD PhD, is a psychiatrist and psychotherapist who has always worked in the field of suicidology. He is on the board of the Sections on Suicidology of the World Psychiatric Association and the European Psychiatric Association. He is currently a postdoctoral fellow in the Department of Public Health Sciences, Karolinska Institute, Sweden.
David McDaid, MSc, is Senior Research Fellow in Health Policy and Health Economics at the London School of Economics and Political Science, UK. He has published more than 60 peer-reviewed papers, particularly in mental health, public health, and health policy. In addition to his health economics specialization, he is a qualified information scientist.
Rory O’Connor, PhD, is Professor of Psychology at the University of Stirling in Scotland, where he leads the Suicidal Behavior Research Group.
Margaret Maxwell, PhD, is Professor and Deputy Director of the Nursing Midwifery and Allied Health Professions Research Unit at the University of Stirling in Scotland.
Angela Ibelshäuser, MSc in education, is public relations coordinator at the Society for Mental Health – pro mente tirol in Austria and coordinator in the current project Austrian and Tyrolean Alliance Against Depression. She has experience in educational settings and in several European projects (e.g., BASES, EAAD, OSPI).
Chantal Van Audenhove, PhD, is a clinical psychologist and professor in the Department of Medicine at the University of Leuven in Belgium and Director of the LUCAS Centre for Care Research and Consultancy. Her chief research topics are in mental healthcare and care for persons with dementia.
Gert Scheerder, PhD in medical sciences, is Senior Researcher in mental health at the LUCAS Centre for Care Research and Consultancy at the University of Leuven in Belgium. He has been involved in several research projects on depression and suicide, including the EAAD and OSPI projects.
Merike Sisask, PhD, is Executive Director and Senior Researcher at the Estonian-Swedish Mental Health and Suicidology Institute (ERSI). She holds a bachelors degree in law (1991), a psychological counselor’s qualification (2003), a masters degree in public health (2005), and PhD degree in sociology (2011).
Ricardo Gusmão, MD PhD, is a psychiatrist, professor of psychiatry, and Coordinator of Research on Affective Disorders and Suicide Prevention at the Chronic Diseases Research Centre (CEDOC), Medical Sciences Faculty, New University of Lisbon, Portugal.
Ulrich Hegerl, MD PhD, was Professor of Psychiatry at Ludwig Maximilian University, Munich. Since 2006 he has been Chair and Medical Director of the Department of Psychiatry, University of Leipzig. He has headed the German Research Network on Depression and Suicidality and the European Alliance Against Depression and is the principal investigator in OSPI, an EU-funded program for suicide prevention.
References
- Adli M., Bauer M., & Rush A. J. (2006). Algorithms and collaborative-care systems for depression: Are they effective and why? A systematic review. Biological Psychiatry, 59, 1029–1038. [DOI] [PubMed] [Google Scholar]
- Althaus D., & Hegerl U. (2003). The evaluation of suicide prevention activities: State of the art. The World Journal of Biological Psychiatry, 4, 156–165. [DOI] [PubMed] [Google Scholar]
- Al Windi A. (2005). Depression in general practice. Nordic Journal of Psychiatry, 59, 272–277. [DOI] [PubMed] [Google Scholar]
- Bernal M., Haro J. M., Bernert S., Brugha T., de Graaf R., Bruffaerts R., ... the ESEMED/MHEDEA investigators. (2007). Risk factors for suicidality in Europe: Results from the ESEMED study. Journal of Affective Disorders, 101(1-3), 27–34. [DOI] [PubMed] [Google Scholar]
- Bool M., Blekman J., de Jong S., Ruiter M., & Voordouw I. (2007). Reduction of suicidality. Utrecht, Netherlands: Trimbos-Instituut. [Google Scholar]
- Botega N. J., & Silveira G. M. (1996). General practitioners attitudes toward depression: A study in primary care setting in Brazil. International Journal of Social Psychiatry, 42, 230–237. [DOI] [PubMed] [Google Scholar]
- Bower P., Gilbody S., Richards D., Fletcher J., & Sutton A. (2006). Collaborative care for depression in primary care: Making sense of a complex intervention: Systematic review and meta-regression. British Journal of Psychiatry, 189, 484–493. [DOI] [PubMed] [Google Scholar]
- De Jong F. J., van Steenbergen-Weijenburg K. M., Huijbregts K. M., Vlasveld M., Van Marwijk H. W. J., Beekman A. T. F., & Van der Feltz-Cornelis C. M. (2009). The Depression Initiative. Description of a collaborative care model for depression and of the factors influencing its implementation in the primary care setting in the Netherlands. Projects and Developments. International Journal of Integrated Care, 9, 81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health, Social Services and Public Safety (DHSSPS). (2006). Protect life – A shared vision. The Northern Ireland Suicide Prevention Strategy and Action Plan, 2006–2011. Belfast, Ireland: Author. [Google Scholar]
- Dowrick C., Gask L., Perry R., Dixon C., & Usherwood T. (2000). Do general practitioners’ attitudes toward depression predict their clinical behavior? Psychological Medicine, 30, 413–419. [DOI] [PubMed] [Google Scholar]
- Dumesnil H., & Verger P. (2009). Public awareness campaigns about depression and suicide: A review. Psychiatric Services, 60, 1203–1213. [DOI] [PubMed] [Google Scholar]
- Elliot L., Crombie I., Irvine L., Cantrell J., & Taylor J. (2004). The effectiveness of public health nursing: The problems and solutions in carrying out a review of systematic reviews. Journal of Advanced Nursing, 45, 117–125. [DOI] [PubMed] [Google Scholar]
- Fernandez A., Haro J. M., Martinez-Alonso M., Demyttenaere K., Brugha T. S., Autonell J., ... Alonso J. (2007). Treatment adequacy for anxiety and depressive disorders in six European countries. British Journal of Psychiatry, 190, 172–173. [DOI] [PubMed] [Google Scholar]
- Fleischmann A., Bertolote J. M., Wasserman D., De Leo D., Bolhari J., Botega N. J., ... Thanh H. (2008). Effectiveness of brief intervention and contact for suicide attempters: A randomized controlled trial in five countries. Bulletin of the World Health Organisation, 86, 703–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S., House A. O., & Sheldon T. A. (2005). Screening and case finding instruments for depression. Cochrane Database Systemic Reviews, (4), :CD002792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbody S., Sheldon T., & House A. (2008). Screening and case-finding instruments for depression: A meta-analysis. Canadian Medical Association Journal, 178, 997–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman L. S., Nielsen N. H., & Champion H. C. (1999). Awareness, diagnosis, and treatment of depression. Journal of General Internal Medicine, 14, 569–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldney R. D. (2005). A pragmatic review of recent studies. Crisis, 26, 128–140. [DOI] [PubMed] [Google Scholar]
- Goldney R. D., Fisher L. J., Wilson D. H., & Cheok F. (2002). Mental health literacy of those with major depression and suicidal ideation: An impediment to help seeking. Suicide and Life-Threatening Behavior, 32, 394–403. [DOI] [PubMed] [Google Scholar]
- Hegerl U., & Wittenburg L. (2009). Focus on mental health care reforms in Europe: The European alliance against depression: A multilevel approach to the prevention of suicidal behavior. Psychiatric Services, 60, 596–599. [DOI] [PubMed] [Google Scholar]
- Hegerl U., Althaus D., Schmidtke A., & Niklewski G. (2006). The Alliance Against Depression: Two-year evaluation of a community based intervention to reduce suicidality. Psychological Medicine, 36, 1225–1234. [DOI] [PubMed] [Google Scholar]
- Hegerl U., Mergl R., Havers I., Schmidtke A., Lehfeld H., Niklewski G., & Althaus D. (2010). Sustainable effects on suicidality were found for the Nuremberg alliance against depression. European Archives of Psychiatry and Clinical Neuroscience, 260, 401–406. [DOI] [PubMed] [Google Scholar]
- Hegerl U., Wittman M., Arensman E., van Audenhove C., Bouleau J. H., Van der Feltz-Cornelis C. M., ... Pfeiffer-Gerschel T. (2008). The European Alliance Against Depression (EAAD): A multifaceted, community-based action program against depression and suicidality. The World Journal of Biological Psychiatry, 9(1), 51–59. [DOI] [PubMed] [Google Scholar]
- Hegerl U., Wittenburg L., Arensman E., Van Audenhove C., Coyne J. C., McDaid D., ... Bramesfeld A. (2009). Optimizing suicide prevention programs and their implementation in Europe (OSPI Europe): An evidence-based multilevel approach. BMC Public Health, 9, 428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IJff M. A., Huijbregts K. M., van Marwijk H. W., Beekman A. T., Hakkaart-van Roijen L., Rutten F. F., ... van der Feltz-Cornelis C. M. (2007). Cost-effectiveness of collaborative care including PST and an antidepressant treatment algorithm for the treatment of major depressive disorder in primary care: A randomized clinical trial. BMC Health Services Research, 7, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaac M., Elias B., Katz L. Y., Belik S. L., Deane F. P., Enns M. W., ... Sareen J. (2009). Gatekeeper training as a preventive intervention for suicide: A systematic review. Canadian Journal of Psychiatry, 54, 260–268. [DOI] [PubMed] [Google Scholar]
- Jorm A. F., Medway J., Christensen H., Korten A. E., Jacomb P. A., & Rodgers B. (2000). Public beliefs about the helpfulness of interventions for depression: Effects on actions taken when experiencing anxiety and depression symptoms. Australian and New Zealand Journal of Psychiatry, 34, 619–626. [DOI] [PubMed] [Google Scholar]
- Katon W. J., & Seelig M. (2008). Population-based care of depression: Team care approaches to improving outcomes. Journal of Occupational Environmental Medicine, 50, 459–467. [DOI] [PubMed] [Google Scholar]
- Kennelly D. (2007). The economic costs of suicide in Ireland. Crisis, 28, 89–94. [DOI] [PubMed] [Google Scholar]
- Khan A., Khan S., Kolts R., & Brown W. A. (2003). Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: Analysis of FDA reports. American Journal of Psychiatry, 160, 790–792. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R. L., & Williams J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitner M., Barr W., & Hobby L. (2008). Effectiveness of interventions to prevent suicide and suicidal behavior: A systematic review. Edinburgh, UK: Scottish Government Social Research. [Google Scholar]
- Lopez A. D., Mathers C. D., Ezzati M., Jamison D. T., & Murray C. J. (2006). Global and regional burden of disease and risk factors: Systematic analysis of population health data. Lancet, 367, 1747–1757. [DOI] [PubMed] [Google Scholar]
- Mann J. J., Apter A., Bertolote J., Beautrais A., Currier D., Haas A., ... Hendin H. (2005). Suicide prevention strategies: A systematic review. Journal of the American Medical Association, 294, 2064–2074. [DOI] [PubMed] [Google Scholar]
- Marušic A. (2008). Seven steps to integrating suicidology. Crisis, 29, 115–117. [DOI] [PubMed] [Google Scholar]
- McDaid D., & Kennelly B. (2010). Suicide across the five continents: An economic perspective. In Wassermann D. & Wassermann C. (Eds.), Suicide across the five continents (pp. 359–368). Oxford: Oxford University Press. [Google Scholar]
- McGuire H., Moncrieff J., & Churchill R. (1998). Quality assessment of trials found within the scope of Cochrane Collaboration Depression, Anxiety and Neurosis (CCDAN). Baltimore, MD: International Cochrane Colloqium. [Google Scholar]
- Meredith L. S., Mendel P., Pearson M., Wu S. Y., Joyce G., Straus J. B., ... Unützer J. (2006). Implementation and maintenance of quality improvement for treating depression in primary care. Psychiatric Services, 57(1), 48–55. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., & Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Journal of Clinical Epidemiology, 62, 1006–1012. [DOI] [PubMed] [Google Scholar]
- Moher D., Schulz K. F., & Altman D. G. (2001). The CONSORT statement: Revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology, 1, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock M. K., Borges G., Bromet E. J., Alonso J., Angermeyer M., Beautrais A., ... Williams D. (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry, 192, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ono Y., Awata S., Iida H., Ishida Y., Ishizuka N., Iwasa H., ... Watanabe N. (2008). Community intervention trial of multimodal suicide prevention program in Japan: A novel multimodal community intervention program to prevent suicide and suicide attempt in Japan, NOCOMIT-J. BMC Public Health, 8, 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips B., Ball C., Sackett D., Badenoch D., Straus S., Haynes B., & Dawes M. (1998, updated 2009). Levels of evidence. Retrieved from http://www.cebm.net/?o=1025. [Google Scholar]
- Pignone M. P., Gaynes B. N., Rushton J. L., Burchell C. M., Orleans C. T., Mulrow C. D., & Lohr K. N. (2002). Screening for depression in adults: A summary of the evidence for the U. S. Preventive Services Task Force. Annals of Internal Medicine, 136, 765–776. [DOI] [PubMed] [Google Scholar]
- Rihmer Z., Kantor Z., Rihmer A., & Seregi K. (2004). Suicide prevention strategies – A brief review. Neuropsychopharmacologia Hungarica, 6, 195–199. [PubMed] [Google Scholar]
- Rost K., Nutting P., Smith J., Coyne J. C., Cooper-Patrick L., & Rubenstein L. V. (1999). The role of competing demands in the treatment provided primary care patients with major depression. Archives of Family Medicine, 9, 150–154. [DOI] [PubMed] [Google Scholar]
- Rutz W., von Knorring L., & Walinder J. (1992). Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatrica Scandinavica, 85(1), 83–88. [DOI] [PubMed] [Google Scholar]
- Scottish Executive. (2002). Choose life: A national strategy and action plan to prevent suicide in Scotland. Edinburgh, UK: Stationary Office. [Google Scholar]
- Sonneck G., & Niederkrotenthaler T. (2008). Zum österreichischen Suizidpräventionsplan [The Austrian Suicide Prevention Plan]. Spectrum Psychiatrie, 2, 20–23. [Google Scholar]
- Tarrier N., Taylor K., & Gooding P. (2008). Cognitive-behavioral interventions to reduce suicide behavior: A systematic review and meta-analysis. Behavior Modification, 32(1), 77–108. [DOI] [PubMed] [Google Scholar]
- Tylee A., & Walters P. (2007). Underrecognition of anxiety and mood disorders in primary care: Why does the problem exist and what can be done? Journal of Clinical Psychiatry, 68(Suppl. 2), 27–30. [PubMed] [Google Scholar]
- Department of Health. (2002). National suicide prevention strategy for England. London: Author. [Google Scholar]
- Van der Feltz-Cornelis C. M. (2009). Toward integrated primary health care for depressive disorder in the Netherlands. The Depression Initiative. International Journal of Integrated Care, 9, 83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Värnik A., Kolves K., Allik J., Arensman E., Aromaa E., van Audenhove C., ... Hegerl U. (2009). Gender issues in suicide rates, trends and methods among youths aged 15–24 in 15 European countries. Journal of Affective Disorders, 113, 226. [DOI] [PubMed] [Google Scholar]
- Värnik A, Kolves K., Van der Feltz-Cornelis C. M., Marusic A., Oskarsson H., Palmer A., ... Hegerl U. (2008). Suicide methods in Europe: A gender-specific analyses of countries participating in the “European Alliance Against Depression.” Journal of Epidemiology and Community Health, 62, 545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlaams Agentschap Zorg en Gezondheid. (2009). Belgian Action Plan Suicide Prevention. Brussels, Belgium: Author. [Google Scholar]
- von Greyerz S., & Keller-Guglielmetti E. (2005). Suizid und Suizidprävention in der Schweiz: Bericht in Erfüllung des Postulates Widmer [Suicide and suicide prevention in Switzerland: Report in fulfillment of the Postulates Widmer]. Bern, Switzerland: Federal Office of Public Health. [Google Scholar]
- Welsh Assembly Government. (2008). “Talk to me”: The national action plan to reduce suicide and self harm in Wales, 2008–2013. Cardiff, UK: Author. [Google Scholar]
- WHO. (2003). Suicide prevention in Europe. The WHO European monitoring survey on national suicide prevention programs and strategies. Copenhagen: WHO Regional Office for Europe. [Google Scholar]
- Williams S. B., O’Connor E. A., Eder M., & Whitlock E. P. (2009). Screening for child and adolescent depression in primary care settings: A systematic evidence review for the US Preventive Services Task Force. Pediatrics, 123, e716–e735. [DOI] [PubMed] [Google Scholar]