Abstract
Background
Tobacco use has been identified as the single biggest cause of inequality in morbidity. The objective of this study is to examine the role of social determinants on current tobacco use in thirteen low-and-middle income countries.
Methodology/Principal Findings
We used nationally representative data from the Global Adult Tobacco Survey (GATS) conducted during 2008–2010 in 13 low-and-middle income countries: Bangladesh, China, Egypt, India, Mexico, Philippines, Poland, Russian Federation, Thailand, Turkey, Ukraine, Uruguay, and Viet Nam. These surveys provided information on 209,027 respondent's aged 15 years and above and the country datasets were analyzed individually for estimating current tobacco use across various socio-demographic factors (gender, age, place of residence, education, wealth index, and knowledge on harmful effects of smoking). Multiple logistic regression analysis was used to predict the impact of these determinants on current tobacco use status. Current tobacco use was defined as current smoking or use of smokeless tobacco, either daily or occasionally. Former smokers were excluded from the analysis. Adjusted odds ratios for current tobacco use after controlling other cofactors, was significantly higher for males across all countries and for urban areas in eight of the 13 countries. For educational level, the trend was significant in Bangladesh, Egypt, India, Philippines and Thailand demonstrating decreasing prevalence of tobacco use with increasing levels of education. For wealth index, the trend of decreasing prevalence of tobacco use with increasing wealth was significant for Bangladesh, India, Philippines, Thailand, Turkey, Ukraine, Uruguay and Viet Nam. The trend of decreasing prevalence with increasing levels of knowledge on harmful effects of smoking was significant in China, India, Philippines, Poland, Russian Federation, Thailand, Ukraine and Viet Nam.
Conclusions/Significance
These findings demonstrate a significant but varied role of social determinants on current tobacco use within and across countries.
Introduction
Socioeconomic inequality and its impact on health is a global public health concern [1]. Smoking has been identified as the single biggest cause of inequality in morbidity and mortality between rich and poor people in many countries [2]. Studies from Western countries have reported an association between social and economic determinants and smoking to the detriment of those in the disadvantaged groups [3]. Several independent studies at international level [4], national level [5] and sub national [6] level from developing countries have shown association of tobacco use with social and economic determinants such as age, education, gender, occupation, ethnicity and place of residence.
National data on prevalence of tobacco use (with some limitations on age groups and gender representation) have been available from Demographic Health Surveys in Bangladesh [7], Egypt [8], India [9], Philippines [10], Turkey [11], Ukraine [12] and Vietnam [13]. These data indicate tobacco use is higher among males, and among disadvantaged sections of society characterized by people living in rural areas and with low education, and lower socioeconomic status. However, the information on tobacco use was only peripheral rather than an objective of these surveys and therefore, the questions on tobacco use were not standardized across countries or even within different surveys in a country.
Global Adult Tobacco Survey (GATS) is a component of the Global Tobacco Surveillance System (GTSS) which includes: the Global Youth Tobacco Survey (GYTS); the Global School Personnel Survey (GSPS); and the Global Health Professions Student Survey (GHPSS). The objectives of GATS in its first phase of implementation was to monitor tobacco use and tobacco control indicators in low and middle income countries bearing the highest burden based on number of adults smokers. The first phase of GATS was implemented in 14 countries during 2008–2010: Bangladesh, Brazil, China, Egypt, India, Mexico, Philippines, Poland, Russian Federation, Thailand, Turkey, Ukraine, Uruguay, and Viet Nam.
GATS is a global standard for systematically monitoring adult tobacco use and tracking key tobacco control indicators. GATS is a nationally representative household survey of adults aged 15 years and older, using a consistent and standard protocol which enables unprecedented cross-country comparisons and change over time for countries that repeat the survey. This paper examines the influence of various socio-demographic variables on current tobacco use within a country and across countries using GATS data.
Materials and Methods
Study Area and Source of Data
GATS data from 13 low-and-middle income countries (Bangladesh, China, Egypt, India, Mexico, Philippines, Poland, Russian Federation, Thailand, Turkey, Ukraine, Uruguay, and Viet Nam) conducted during 2008–2010 were used for analyses. GATS data from Brazil was not included in this paper as the information on important predictor variables collected in Brazil (education, wealth index) was not comparable to other GATS countries. These surveys provided information on 209,027 respondent's aged 15 years and above and the country datasets were analyzed individually for estimating overall current tobacco use as well as by various socio-demographic factors.
GATS used a multi-stage geographically clustered sample design to produce nationally representative data. For each participating country, a standard protocol with respect to questionnaire, sample design, data collection and management procedures was used. Survey information was collected using handheld devices. Additional details of individual country survey methodologies are available in country reports [14 to 26]. The list of GATS collaborating group in the 14 countries and other partner organizations is provided in List S1.
Variables Included in the Analyses
Current tobacco use is the dependent variable used in this analysis and was defined as current smoking or use of any smokeless tobacco product, either daily or occasionally [27] using the following questions: 1) ‘Do you currently smoke tobacco on a daily basis, less than daily, or not at all’ and 2) ‘Do you currently use smokeless tobacco on a daily basis, less than daily, or not at all’. Out of all 13 countries, only Turkey did not ask the questions on smokeless tobacco. Former tobacco users were defined as the number of ever tobacco smokers or smokeless tobacco users who currently do not smoke or use any form of tobacco. Never tobacco users were defined as adults who reported that they neither smoked nor used smokeless tobacco in their life time.
Relevant independent variables included in the analyses were gender (male/female), age, place of residence (urban/rural), knowledge on harmful effects of smoking (three categories), educational level (four categories), and wealth index (five categories). The level of knowledge on harmful effects of smoking was measured using three core questions in each country: ‘based on what you know or believe does smoking tobacco cause the following: stroke (blood clots in the brain that may cause paralysis), heart attack and lung cancer’. Respondents who answered all three questions correctly were classified as having ‘good knowledge’, those who answered any two questions correctly as having ‘some knowledge’ and rest were classified as having ‘little knowledge’. Educational level was grouped into five categories: no formal schooling, less than primary, primary complete, less than secondary, and secondary school complete and above (includes high school, college/university, and post graduate and above education) across all countries. Wealth index, a proxy measure for respondent socioeconomic status, was constructed using principal component analysis with information on household ownership of assets [28]. The asset information included whether households possessed such items as electricity, flush toilet, fixed telephone, cell telephone, television, radio, refrigerator, car, moped/scooter/motorcycle, washing machine, etc. The sample was divided into quintiles from one (lowest) to five (highest) for each country. A single wealth index was developed for the whole respondent sample. Thus, at a national level, for each country, 20 percent of the sample respondents are in each wealth quintile although indexes it is not necessarily true at population level.
Statistical Analysis
The data were appropriately weighted to ensure the true representation of the population of the country; SPSS® version 18.0 for complex samples was used to analyze the data. Statistical analysis included multiple logistic regression accounted for complex survey design for predicting the social determinants of tobacco use. The dependent variable used for this analysis was tobacco use (tobacco user-1; never tobacco user-0). Former tobacco users were removed from the logistic regression analysis due to the fact that current tobacco use may not directly influence from current socioeconomic and demographic status. All the independent variables were categorical. Overall trend for each variable was assessed by assuming the categories of independent variables as continuous variables in the logistic regression, except for age variable where we used age in single years for obtaining the trend.
Results
Table 1 shows the sample characteristics for 13 countries. Since sample design in each country was stratified by gender and place of residence (urban/rural), the distributions for these two variables reflect the population distribution. The age distribution showed a steep pyramidal structure for five countries (Bangladesh, Egypt, India, Mexico and Philippines). The education distribution showed a step gradient for Bangladesh and India. In four countries, over one third of the sample has no formal or less than primary education (Bangladesh, Egypt, India and Thailand). The percent distribution of adult population by wealth quintiles, based on the household assets included in the survey shows more or less an even distribution across many countries except few exemptions (e.g. India, Mexico, Russia, Ukraine, and Uruguay) where a varied socioeconomic status of the population was observed. For example, almost 28% of respondents in India were classified as having lowest wealth index whereas only 11.2% fall under lowest wealth quintile in Mexico. The level of knowledge on harmful effects of smoking varied a great deal across countries. Interestingly, the highest level ‘good knowledge’ was reported most in Egypt (88%) and least in China (less than 23%).
Table 1. Distribution of adults aged 15 years and above by socio-demographic characteristics in 13 low-and-middle income countries, Global Adult Tobacco Survey, 2008–2010.
| Socio-demographic characteristics | Bangladesh | China | Egypt | India | Mexico | Philippines | Poland | Russian Federation | Thailand | Turkey | Ukraine | Uruguay | Viet Nam |
| (n = 9,629) | (n = 13,354) | (n = 20,924) | (n = 69,296) | (n = 13,617) | (n = 9,701) | (n = 7,840) | (n = 11,406) | (n = 20,566) | (n = 9,030) | (n = 8,158) | (n = 5,581) | (n = 9,925) | |
| Gender | |||||||||||||
| Male | 49.7 | 50.9 | 51.0 | 51.7 | 47.7 | 49.9 | 47.7 | 45.3 | 48.6 | 49.1 | 45.4 | 47.4 | 48.6 |
| Female | 50.3 | 49.1 | 49.0 | 48.3 | 52.3 | 50.1 | 52.3 | 54.7 | 51.4 | 50.9 | 54.6 | 52.6 | 51.4 |
| Age | |||||||||||||
| 15–24 | 29.5 | 21.5 | 33.0 | 29.5 | 27.7 | 29.6 | 17.3 | 17.8 | 20.0 | 22.5 | 18.4 | 20.2 | 25.9 |
| 25–34 | 23.5 | 15.4 | 22.4 | 22.7 | 23.3 | 21.4 | 18.9 | 18.0 | 18.2 | 23.5 | 18.0 | 18.6 | 19.7 |
| 35–44 | 19.6 | 24.1 | 17.6 | 19.3 | 19.1 | 20.6 | 15.8 | 16.5 | 23.2 | 19.2 | 16.3 | 16.8 | 22.2 |
| 45–54 | 12.8 | 15.7 | 13.5 | 12.9 | 13.2 | 13.0 | 17.5 | 19.0 | 16.8 | 15.5 | 16.0 | 14.8 | 15.0 |
| 55–64 | 8.0 | 13.5 | 8.0 | 8.8 | 8.6 | 8.9 | 14.6 | 12.8 | 12.1 | 10.1 | 14.0 | 12.4 | 8.4 |
| 65+ | 6.6 | 9.8 | 5.5 | 6.8 | 8.0 | 6.5 | 15.9 | 15.9 | 9.7 | 9.2 | 17.3 | 17.2 | 8.8 |
| Place of residence | |||||||||||||
| Urban | 26.2 | 46.1 | 45.3 | 29.2 | 77.8 | 49.8 | 62.0 | 74.5 | 31.1 | 69.7 | 68.0 | 92.7 | 30.7 |
| Rural | 73.8 | 53.9 | 54.7 | 70.8 | 22.2 | 50.2 | 38.0 | 25.5 | 68.9 | 30.3 | 32.0 | 7.3 | 69.3 |
| Education | |||||||||||||
| No formal education/Less than primary | 51.3 | 15.9 | 41.0 | 43.2 | 18.3 | 21.5 | 1.4 | 0.3 | 33.7 | 17.1 | 0.8 | 10.6 | 21.3 |
| Completed primary/Less than secondary | 33.8 | 18.4 | 6.3 | 28.9 | 23.6 | 17.2 | 14.3 | 3.8 | 21.0 | 48.8 | 10.3 | 36.5 | 24.3 |
| Completed secondary/high school | 11.5 | 53.4 | 41.5 | 19.6 | 49.7 | 39.1 | 69.1 | 65.2 | 37.3 | 25.2 | 66.5 | 45.0 | 48.3 |
| Completed college/university or above | 3.3 | 12.2 | 11.1 | 8.3 | 8.4 | 22.3 | 15.2 | 30.7 | 8.0 | 8.9 | 22.3 | 7.9 | 6.1 |
| Wealth Index | |||||||||||||
| Lowest | 19.2 | 15.7 | 21.9 | 28.0 | 11.2 | 18.1 | 16.3 | 14.8 | 19.2 | 14.5 | 14.2 | 11.9 | 20.6 |
| Low | 21.6 | 18.1 | 19.7 | 18.4 | 15.4 | 18.1 | 19.3 | 16.4 | 21.2 | 20.4 | 15.4 | 16.9 | 24.0 |
| Medium | 23.4 | 20.4 | 17.6 | 24.1 | 19.3 | 20.7 | 18.7 | 21.9 | 20.6 | 21.1 | 20.6 | 19.4 | 21.9 |
| High | 20.8 | 21.4 | 23.0 | 15.5 | 24.1 | 20.4 | 23.5 | 12.3 | 23.1 | 23.8 | 22.9 | 22.0 | 17.6 |
| Highest | 15.0 | 24.5 | 17.8 | 14.0 | 30.0 | 22.7 | 22.2 | 34.5 | 15.9 | 20.3 | 26.9 | 29.7 | 16.0 |
| Knowledge | |||||||||||||
| Little knowledge | 12.9 | 57.5 | 5.1 | 33.1 | 16.5 | 18.4 | 18.7 | 25.9 | 15.5 | 6.0 | 17.7 | 7.0 | 22.9 |
| Some knowledge | 8.4 | 20.4 | 6.9 | 22.5 | 27.3 | 12.1 | 21.4 | 10.4 | 14.1 | 12.7 | 9.1 | 18.0 | 21.5 |
| Good knowledge | 78.7 | 22.1 | 88.0 | 44.5 | 56.2 | 69.6 | 59.8 | 63.7 | 70.4 | 81.2 | 73.2 | 75.0 | 55.5 |
| Tobacco Use | |||||||||||||
| Current tobacco user | 43.3 | 28.1 | 19.7 | 34.6 | 16.0 | 29.5 | 30.5 | 39.3 | 27.2 | 31.2 | 28.9 | 25.0 | 25.0 |
| Never tobacco user | 53.0 | 66.5 | 75.8 | 62.4 | 69.2 | 59.5 | 47.5 | 46.7 | 60.6 | 52.8 | 55.9 | 51.1 | 64.9 |
| Former tobacco user | 3.7 | 5.4 | 4.4 | 3.0 | 14.7 | 11.0 | 22.0 | 13.9 | 12.2 | 15.9 | 15.2 | 24.0 | 10.1 |
Note: n - sample size.
Table 2 shows the prevalence of tobacco use by various socio-demographic factors. The prevalence of current tobacco use varied from 16% in Mexico to 43.3% in Bangladesh. Former users varied much more, from 3% in India to 24% in Uruguay. Among males, the prevalence varied from 25% in Mexico to 60.6% in the Russian Federation. Among females, the variation was much higher from 0.6% in Egypt to 28.7% in Bangladesh. Prevalence varied considerably by gender, the level of education and wealth index and by the level of knowledge on effects of smoking.
Table 2. Prevalence of current tobacco use among adults aged 15 years and above by socio-demographic characteristics in 13 low-and-middle income countries, Global Adult Tobacco Survey, 2008–2010.
| Socio-demographic characteristics | Bangladesh | China | Egypt | India | Mexico | Philippines | Poland | Russian Federation | Thailand | Turkey | Ukraine | Uruguay | Viet Nam |
| Overall | 43.3 | 28.1 | 19.7 | 34.6 | 16.0 | 29.5 | 30.5 | 39.3 | 27.2 | 31.2 | 28.9 | 25.0 | 25.0 |
| Gender | |||||||||||||
| Male | 58.0 | 52.9 | 38.1 | 47.9 | 25.0 | 49.2 | 37.3 | 60.6 | 46.4 | 47.9 | 50.1 | 30.7 | 47.6 |
| Female | 28.7 | 2.4 | 0.6 | 20.3 | 7.9 | 10.0 | 24.4 | 21.7 | 9.1 | 15.2 | 11.3 | 19.8 | 3.6 |
| Age | |||||||||||||
| 15–24 | 16.9 | 17.9 | 11.3 | 18.4 | 17.0 | 21.2 | 24.7 | 43.1 | 19.8 | 25.3 | 30.5 | 24.7 | 13.3 |
| 25–34 | 36.3 | 28.7 | 22.3 | 33.2 | 17.9 | 33.5 | 34.1 | 51.1 | 25.6 | 40.4 | 42.0 | 34.7 | 26.0 |
| 35–44 | 55.0 | 32.4 | 24.5 | 42.2 | 16.1 | 32.3 | 36.6 | 48.2 | 27.8 | 39.4 | 38.0 | 25.7 | 31.7 |
| 45–54 | 67.6 | 36.0 | 26.7 | 45.5 | 17.7 | 33.8 | 43.1 | 41.8 | 26.5 | 32.6 | 32.4 | 32.4 | 31.2 |
| 55–64 | 70.7 | 30.9 | 24.3 | 49.4 | 12.9 | 33.1 | 31.6 | 32.8 | 31.7 | 24.7 | 20.8 | 24.1 | 30.1 |
| 65+ | 70.8 | 22.7 | 20.5 | 47.8 | 8.1 | 32.0 | 11.8 | 14.9 | 39.8 | 10.3 | 8.5 | 8.1 | 24.5 |
| Place of residence | |||||||||||||
| Urban | 38.1 | 26.1 | 19.8 | 25.3 | 17.5 | 25.3 | 32.0 | 40.5 | 22.9 | 33.0 | 30.5 | 25.1 | 23.6 |
| Rural | 45.1 | 29.9 | 19.7 | 38.4 | 11.0 | 33.7 | 28.0 | 36.0 | 29.2 | 27.2 | 25.6 | 23.4 | 25.6 |
| Education | |||||||||||||
| No formal education/Less than primary | 58.1 | 20.9 | 22.7 | 44.6 | 11.5 | 45.1 | 11.6 | 23.9 | 34.3 | 15.0 | 15.7 | 24.4 | 28.4 |
| Completed primary/Less than secondary | 30.3 | 28.5 | 21.6 | 32.7 | 15.4 | 33.6 | 23.9 | 17.6 | 29.5 | 31.4 | 15.5 | 27.1 | 28.2 |
| Completed secondary/high school | 19.3 | 31.5 | 17.5 | 21.7 | 17.6 | 26.6 | 33.6 | 42.0 | 23.0 | 42.0 | 32.5 | 24.1 | 22.4 |
| Completed college/university or above | 29.7 | 22.6 | 16.2 | 18.3 | 18.5 | 16.4 | 24.8 | 36.5 | 11.7 | 31.8 | 24.6 | 20.6 | 20.5 |
| Wealth Index | |||||||||||||
| Lowest | 55.5 | 29.0 | 20.7 | 47.6 | 10.9 | 40.4 | 27.8 | 36.8 | 37.0 | 26.4 | 24.8 | 37.7 | 30.3 |
| Low | 47.4 | 30.6 | 21.8 | 38.4 | 12.1 | 35.6 | 32.2 | 35.3 | 31.8 | 33.6 | 27.3 | 25.7 | 27.7 |
| Middle | 43.5 | 28.3 | 23.1 | 32.4 | 15.4 | 31.7 | 32.8 | 39.8 | 27.7 | 32.8 | 31.4 | 27.1 | 24.1 |
| High | 38.6 | 28.7 | 19.4 | 25.5 | 17.8 | 26.9 | 30.4 | 35.2 | 23.3 | 31.9 | 28.5 | 22.2 | 21.9 |
| Highest | 28.1 | 25.2 | 13.3 | 17.2 | 19.0 | 16.4 | 29.4 | 43.6 | 14.5 | 30.0 | 30.5 | 20.1 | 18.6 |
| Knowledge on effects of smoking | |||||||||||||
| Little knowledge | 50.6 | 30.2 | 22.3 | 41.7 | 13.4 | 42.9 | 46.4 | 56.7 | 32.7 | 29.2 | 42.1 | 32.6 | 34.0 |
| Some knowledge | 38.4 | 25.4 | 21.1 | 31.9 | 18.3 | 30.7 | 31.0 | 44.2 | 26.9 | 31.7 | 34.8 | 22.8 | 23.2 |
| Good knowledge | 42.7 | 25.0 | 19.5 | 30.5 | 15.8 | 25.8 | 25.4 | 31.5 | 26.1 | 31.3 | 25.0 | 24.8 | 21.9 |
| Number of tobacco users (in millions) | 41.3 | 300.8 | 9.8 | 274.9 | 11.0 | 18.1 | 9.9 | 44.2 | 14.3 | 16.0 | 11.6 | 0.6 | 16.1 |
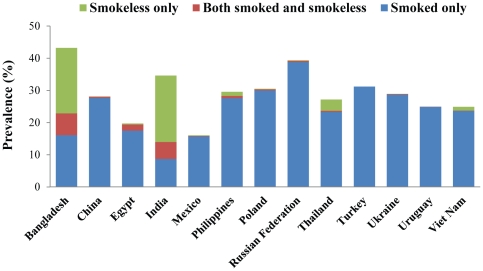
Tobacco use included smoking, smokeless tobacco use and dual use (using both smoked and smokeless). Figure 1 shows the type of tobacco use. It is clear that in Bangladesh and India, smokeless tobacco use constitutes a major part of overall tobacco use. In Thailand, Philippines and Viet Nam smokeless tobacco use also makes some contribution to overall tobacco use. In addition, in the countries where smokeless tobacco use prevalence is high along with smoking, dual use (use of both smoking and smokeless tobacco products) also contributes to a noticeable proportion and somewhat more likely in those countries (e.g. Bangladesh (8.7%) and India (5.3%)).
Figure 1. Type of current tobacco use among adults aged 15 years and above in 13 low-and-middle income countries, Global Adult Tobacco Survey, 2008–2010.
Both Table 3 and Table 4 show the odds ratios for current tobacco use versus no tobacco use using a multiple logistic regression model incorporating all variables in the table. Odds ratios were significantly higher for males in all countries with great variation across countries (from 2.1 in Uruguay to 161.9 in Egypt). As shown in Table 2, the prevalence of current smokers is quite lower among women compared with men in most countries and also sex of the respondent was a very strong determinant of smoking status (Table 3–4). Compared to the lowest age group (15–24 years), odds ratios were significantly higher in almost all age groups in almost all countries with very few exceptions. Except for Mexico and Poland, the trend was significant for all other countries although it was in opposite direction (decreasing with increase in age in Russian Federation, Ukraine and Uruguay). The prevalence after adjusting for other cofactors was significantly higher for rural areas only in India and Thailand. The difference was not significant for Bangladesh, China and Philippines. For educational level, odds ratios were computed taking highest level of education (completed college) as the reference. Most odds ratios were significant with the largest difference being four fold in Bangladesh and Thailand. The trend was significant in Bangladesh, Egypt, India, Philippines and Thailand demonstrating decreasing prevalence of tobacco use with increasing level of education. The trend was in the opposite direction for Turkey and not significant for the rest of the countries.
Table 3. Predictors of current tobacco use among adults age 15 years and above in 13 low-and-middle income countries using logistic regression analysis, Global Adult Tobacco Survey, 2008–2010.
| Socio-demographic characteristics | Bangladesh | China | Egypt | India | Mexico | Philippines | Poland | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||||||||||
| Male | 6.79 | (5.9, 7.8)*** | 82.19 | (63.7, 106.0)*** | 162.2 | (110.9, 237.3)*** | 6.08 | (5.6, 6.6)*** | 4.93 | (4.3, 5.7)*** | 16.93 | (14.4, 19.9)*** | 2.37 | (2.1, 2.7)*** |
| Female (RC) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | |||||||
Note: OR-Odds Ratio; CI-Confidence Interval; RC-Reference Category;
p<0.001,
p<0.01,
p<0.05;
p-values shown for test of linear trend.
Table 4. Predictors of current tobacco use among adults age 15 years and above in 13 low-and-middle income countries using logistic regression analysis, Global Adult Tobacco Survey, 2008–2010.
| Socio-demographic characteristics | Russian Federation | Thailand | Turkey | Ukraine | Uruguay | Viet Nam | ||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||||||||
| Male | 8.3 | (7.1, 9.7)*** | 29.02 | (25.1, 33.5)*** | 7.99 | (6.9, 9.3)*** | 13.18 | (11.1, 15.6)*** | 2.08 | (1.8, 2.5)*** | 87.33 | (68.3, 111.6)*** |
| Female (RC) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | ||||||
Note: OR-Odds Ratio; CI-Confidence Interval; RC-Reference Category;
p<0.001,
p<0.01,
p<0.05;
p-values shown for test of linear trend.
For wealth index, odds ratios were computed taking the highest wealth category as reference. Most of odds ratios were significant with largest effect observed in Thailand. The trend (decreasing odds of tobacco use with increasing wealth) was significant for Bangladesh, India, Philippines, Thailand, Turkey, Ukraine, Uruguay and Viet Nam. The trend was opposite in Mexico and not significant in other countries. Knowledge level was also affected tobacco use, though to a lesser extent. An inverse relationship was observed for level of knowledge and tobacco use; as level of knowledge increased, the odds of tobacco use decreased and was significant for China, India, Philippines, Poland, Russian federation, Thailand, Ukraine and Viet Nam. The trend was not significant in remaining countries.
Discussion
This report provides information about 13 countries where 2.64 billion adults aged 15 years and above live, which constitutes more than half of the world's adult population (5.15 billion) in 2010 [29]. The findings from this report indicate that across these 13 countries over three-quarters of a billion (768.5 millions) are current tobacco users. Moreover, the findings provide evidence that social determinants are associated with tobacco use behavior. Most reports on tobacco use [4] are confined to smoking as it is the only form of tobacco use in most of the countries. Among these 13 countries however, smokeless tobacco use is the dominant form of tobacco use behavior in at least two countries (Bangladesh and India), making it inadvisable to leave out smokeless tobacco use while discussing tobacco use behavior. For the sake of uniformity, we decided to combine both smoking and smokeless tobacco use and termed it as ‘tobacco use’ for all countries. Questions about smokeless tobacco use were asked in all countries except Turkey. The findings show that in addition to Bangladesh and India, smokeless tobacco use was important for Thailand, Philippines and Viet Nam as well.
Our study reveal that the prevalence of current tobacco use, particularly smoking is quite lower among women compared with men in most countries and sex is a very strong determinant of tobacco use status. Stratified analysis of tobacco use by sex (not shown in tables) clearly indicated that the present findings apply to women as well as men. Our study also reveals that the prevalence of tobacco use is generally higher among urban, less educated and low economic groups and people with less knowledge about effects of smoking. Detailed questions about the health effects of smokeless tobacco use were asked only in Bangladesh. The level of knowledge (calculated similar to smoking) based on three specific diseases (stroke, heart attack, and cancer of mouth) that are caused by smokeless tobacco use showed that the smokeless tobacco use is higher among individuals with lower level of knowledge (little knowledge (30%), some knowledge (34.3%) and good knowledge (26.5%)).
An important finding in this study is high prevalence of tobacco use in the middle ages (45 to 64). The health effects of tobacco use start becoming apparent in these age groups in a major way [30]. Therefore, targeting cessation in these age groups would be extremely important as a component of overall policy initiatives for reducing tobacco use prevalence [31]. This will be crucial in reducing morbidity and mortality caused by tobacco use in the immediate future [32]. In general, social determinants associated with inequality such as education and wealth were correlated with increased tobacco use. However, some exceptions were seen. In a few countries increased wealth and education were not associated with decreased tobacco use, with Mexico actually having lower tobacco use in the poor, and with the lowest rates of tobacco use in China present in the poorest and wealthiest. Future research to understand the determinants of these patterns is warranted.
In this paper, we study social determinants as predictors of tobacco use, but in the long term tobacco use itself causes social inequalities [33]. In disadvantaged sections of society, expenditure on tobacco use often replaces expenditure on other essential items and services for the family. In the long term, these families suffer serious morbidity and mortality due to tobacco use which accentuates determinants further [34]. Intra-country differences in tobacco use influence the overall burden of disease and death and substantially contribute to overall between -country differences in other parameters of public health [35]. Monitoring of tobacco epidemic will be necessary to increase the effectiveness of existing public health strategies and for development of tailored interventions [36], particularly targeting young people and women [30] to stop using tobacco use and discourage initiation to reduce tobacco-related disparities.
At least two health parameters included in Millennium Development Goals (MDGs) are strongly related to tobacco use: deaths by tuberculosis and maternal and child health issues [37]. Currently about a billion adults use tobacco every day and about 15,000 die from tobacco-related diseases every day [38]. Smoking causes half of all male deaths among tuberculosis patients in India [39], [40]. Smoking by pregnant women is well established as a causative factor for low birth weight, still birth and other adverse reproductive outcomes. Recent evidence establishes that a non-cigarette form of tobacco use also causes adverse reproductive outcomes [41], especially smokeless tobacco use in India [42], [43]. In addition, there is a strong indication that exposure to secondhand smoke increases the risk of still birth [44]. Tobacco use accounts for one in six of all deaths resulting from Non-Communicable Diseases (NCDs) [45]. Socioeconomic impacts of NCDs are affecting the progress towards UN MDGs [45]. It is therefore clear that a high level of tobacco use especially among disadvantaged groups in these 13 countries is an important hindrance to the attainment of the MDGs.
The findings in this report are subject to a few limitations. The prevalence results are based on self-reports without bioassay validation. Study design allowed for the investigation of only a limited number of socio-demographic variables. It is important to note that former tobacco users were excluded from the logistic regression. The proportion of former users was different in different countries and their distribution by socio-demographic variables used in the analysis might be different. This might affect some comparisons. The information on frequency and length of smoking, though available in GATS data, was not considered in the present study. In some countries the household possession items considered/used in the analysis are based on the items available in the country data and these items may not be a true representation of wealth across all countries.
Despite these limitations, the current study provides evidence of the importance of social determinants on tobacco use. Findings indicate that social determinants and their role should be given high priority when addressing the issue of tobacco use.
Supporting Information
GATS Collaborating Group.
(DOCX)
Acknowledgments
Authors would like to thank Edward Rainey and Sophia Y Song for their assistance with the manuscript. The views expressed in this article are solely those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the GATS partner organizations.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: Funding for the Global Adult Tobacco Survey (GATS) is provided by the Bloomberg Initiative to Reduce Tobacco Use, a program of Bloomberg Philanthropies. Government of India contributed to GATS implementation in India. Bill and Melinda Gates Foundation provided additional funding for GATS implementation in China. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.CSDH. Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. 2008. World Health Organization, Geneva. P. 25–108. Available: http://whqlibdoc.who.int/publications/2008/9789241563703_eng.pdf. Accessed 27 April 2011.
- 2.Jarvis MJ, Wardle J. Social patterning of health behaviours: the case of cigarette smoking. In: Marmot M, Wilkinson RG, editors. Social determinants of health, 2 edition. Oxford: Oxford University Press; 2006. pp. 224–37. [Google Scholar]
- 3.Barbeau EM, Leavy-Sperounis A, Balbach eds: Smoking, social class, and gender: what can public health learn from the tobacco industry about disparities in smoking? Tobacco Control. 2004;13:115–20. doi: 10.1136/tc.2003.006098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tobacco Control. 2003;12:4. doi: 10.1136/tc.12.4.e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hosseinpoor AR, Parker LA, Tursan d'Espaignet E, Chatterji S. Social Determinants of Smoking in Low- and Middle-Income Countries: Results from the World Health Survey. PLoS One. 2011;2011; 6(5):e20331. doi: 10.1371/journal.pone.0020331. doi: 10.1371/journal.pone.0020331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sorensen G, Gupta PC, Pednekar MS. Social disparities in tobacco use in Mumbai, India: the roles of occupation, education, and gender. Am J Public Health. 2005;95(6):1003–8. doi: 10.2105/AJPH.2004.045039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bangladesh Demographic Health Survey (BDHS) National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ORC Macro, Dhaka, Bangladesh and Calverton, Maryland. 2007. Available: http://www.measuredhs.com/pubs/pdf/FR207/FR207April-10-2009.pdf. Accessed on 27 April 2011.
- 8.Ministry of Health, Egypt. Demographic and Health Survey by El-Zanaty and Associates. 2008. Available: http://www.measuredhs.com/pubs/pdf/FR220/FR220.pdf. Accessed on 27 April 2011.
- 9.International Institute for Population Sciences, (IIPS) and Macro International. National Family Health Survey (NFHS-3) 2005–2006: India: Volume I, Mumbai: IIPS. 2007. Available: http://www.measuredhs.com/pubs/pdf/FRIND3/FRIND3-Vol1Oct-17-2008.pdf. Accessed on 27 April 2011.
- 10.National Statistics Office, Manila, Philippines. National Demographic and Health Survey. 2008. Available: http://www.measuredhs.com/pubs/pdf/FR224/FR224.pdf. Accessed on 27 April 2011.
- 11.Hacettepe University Institute of Population Studies Ankara, Turkey. Demographic and Health Survey. 2003. Available: http://www.measuredhs.com/pubs/pdf/FR160/FR160.pdf. Accessed on 27 April 2011.
- 12.Ukrainian Center for Social Reforms Kyiv, Ukraine. State Statistical Committee Kyiv, Ukraine, Ministry of Health, Kyiv, Ukraine, Macro International Inc. Calverton, Maryland, U.S.A., Ukraine Demographic and Health Survey. 2007. Available: http://www.measuredhs.com/pubs/pdf/FR210/FR210.pdf. Accessed on 27 April 2011.
- 13.National Committee for Population, Family and Children Population. Vietnam Demographic and Health Survey. General Statistical Office and ORC Macro Calverton, Maryland USA. 2005. Available: http://www.measuredhs.com/pubs/pdf/AIS3/AIS3.pdf. and http://www.measuredhs.com/pubs/pdf/FR207/FR207April-10-2009.pdf. Accessed on 27 April 2011.
- 14.World Health Organization (WHO) Country Office for Bangladesh. Global Adult Tobacco Survey: Bangladesh Report, Bangladesh. 2009. Available: http://www.who.int/tobacco/surveillance/global_adult_tobacco_survey_bangladesh_report_2009.pdf. Accessed on 27 April 2011.
- 15.GATS China. Global Adult Tobacco Survey: China 2010 Country Report. 2010. Available: http://www.wpro.who.int/internet/files/chn/gats_china_report_en.pdf. Accessed on 27 January 2012.
- 16.The Central Agency for Public Mobilization and Statistics (CAPMAS) The Ministry of Health, Egypt, GATS Egypt country report. 2009. Available: http://www.emro.who.int/tfi/GATS_2009/index.htm. Accessed on 27 April 2011.
- 17.International Institute for Population Sciences, (IIPS), Ministry of Health and Family Welfare, Government of India. Global Adult Tobacco Survey India (GATS India), 2009–10, India. 2009–2010. Available: http://www.whoindia.org/en/Section20/Section25_1861.htm. Accessed on 27 April 2011.
- 18.Ministry of Health, Mexico. GATS Encuesta Global de Tabaquismo en Adultos, México. 2009. Available: http://www.who.int/tobacco/surveillance/gats_rep_mexico.pdf. Accessed on 27 April 2011.
- 19.GATS Philippines'. Philippines' Global Adult Tobacco Survey: Country Report. 2009. Available: http://www.wpro.who.int/internet/resources.ashx/TFI/2009GATSCountryReport_FinalPhilippines.pdf. Accessed on 27 April 2011.
- 20.Ministry of Health, Warsaw. Global Adult Tobacco Survey Poland 2009–2010 Ministry of Health, Poland. 2010. Available: http://www.who.int/tobacco/surveillance/en_tfi_gats_poland_report_2010.pdf. Accessed on 27 April 2011.
- 21.GATS Russian Federation. Global Adult Tobacco Survey: Russian Federation Country Report, Russian Federation. 2009. Available: http://www.who.int/tobacco/surveillance/en_tfi_gats_russian_countryreport.pdf. Accessed on 27 April 2011.
- 22.World Health Organization, Regional office for South East Asia. Global Adult Tobacco Survey: Thailand Country Report, Thailand, World Health Organization. 2009. Available: http://www.who.int/tobacco/surveillance/thailand_gats_report_2009.pdf. Accessed 27 April 2011.
- 23.The Ministry of Health of Turkey. Global Adult Tobacco Survey (GATS) Turkey Country Report, Turkey, Ministry of Health. 2010. Available: http://www.havanikoru.org.tr/Docs_Tutun_Dumaninin_Zararlari/GATS.pdf. Accessed on 27 April 2011.
- 24.GATS Ukraine. Ukraine Global Adult Tobacco Survey: Ukraine Country Report, Ukraine. 2010. Available: http://www.who.int/tobacco/surveillance/en_tfi_gats_ukraine_report_2010.pdf. Accessed on 27 April 2011.
- 25.GATS Uruguay. Global Adult Tobacco Survey Uruguay: Fact Sheet. 2009. Available: http://www.cdc.gov/tobacco/global/gats/countries/amr/fact_sheets/uruguay/2009/pdfs/uruguay_2009.pdf. Accessed on 27 April 2011.
- 26.Ministry of Health Of Viet Nam, Hanoi Medical University, General Statistics Office, Centers for Disease Control and Prevention, World Health Organization. Global Adult Tobacco Survey (GATS) Viet Nam: Country Report, Hanoi. 2010. Available: http://www.who.int/tobacco/surveillance/en_tfi_gats_vietnam_report.pdf. Accessed on 27 April 2011.
- 27.Global Tobacco Surveillance System. Global adult tobacco survey: indicator guidelines: definitions and syntax. Atlanta: CDC; 2009. Available: http://apps.nccd.cdc.gov/gtssdata/Ancillary/Documentation.aspx?SUID=4&DOCT=1. Accessed on 27 January 2012. [Google Scholar]
- 28.Rutstein S. Wealth versus expenditure: Comparison between the DHS wealth index and household expenditures in four departments of Guatemala. Calverton, Maryland: ORC Macro (unpublished); 1999. [Google Scholar]
- 29.Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World Population Prospects: The 2010 Revision. 2010. Available: http://esa.un.org/unpd/wpp/index.htm. Accessed on 4 May 2011.
- 30.Norberg M, Lundqvist G, Nilsson M, Gilljam H, Weinehall L. Changing patterns of tobacco use in a middle-aged population – the role of snus, gender, age, and education. Glob Health Action. 2011;2011; 4 doi: 10.3402/gha.v4i0.5613. 10.3402/gha.v4i0.5613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. WHO report on the global tobacco epidemic: the MPOWER package. Geneva: World Health Organization; 2008. Available: http://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf. Accessed on 27 April 2011. [Google Scholar]
- 32.Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet. 2006;2006; 368:367–70. doi: 10.1016/S0140-6736(06)68975-7. [DOI] [PubMed] [Google Scholar]
- 33.Efroymson D, Ahmed S, Townsend J, Alam SN, Dey AR, et al. Hungry for tobacco: an analysis of the economic impact of tobacco consumption on the poor in Bangladesh. Tobacco Control. 2001;2001; 10:212–217. doi: 10.1136/tc.10.3.212. doi: 10.1136/tc.10.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson NW, Warnakulasuriya S, Gupta PC, Dimba E, Chindia M, et al. Global oral health inequalities in incidence and outcomes for oral cancer: causes and solutions. Adv Dent Res. 2011;2011 May;23(2):237–46. doi: 10.1177/0022034511402082. [DOI] [PubMed] [Google Scholar]
- 35.Zatoński W, Mańczuk M, Sulkowska U HEM project team. Closing the health gap in European Union-European Commission, and Polish Government – Ministry of Science and Higher Education. 2011. Available: https://camtools.cam.ac.uk/access/content/group/5e895f99-398c-46c7-86ab-b1f76a48c718/2_Ppblic_Health_Assessment/03_The_east_west_gap_in_Europe/Closing_the_health_gap_in_EU_chs_1_and_2.pdf. Accessed on 27 April 2011.
- 36.Garrett SE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF. 2011 Cigarette Smoking – United States, 1965–2008 Morbidity and Mortality Weekly Reports (MMWR) Supplements. 2011/60(01);109–113. [PubMed] [Google Scholar]
- 37.World Health Organization. The Millennium Development Goals and Tobacco Control, WHO Geneva. 2004. Available: http://www.who.int/tobacco/publications/mdg_final_for_web.pdf. Accessed on 27 April 2011.
- 38.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, et al. Priority actions for the non-communicable disease crisis. The Lancet. 2011;2011 377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]
- 39.Jha P, Jacob B, Gajalakshmi V, Gupta PC, Dhingra N, et al. A nationally representative case-control study of smoking and death in India. N Engl J Med. 2008;2008 Mar 13;358(11):1137–47. doi: 10.1056/NEJMsa0707719. Epub 2008 Feb 13. [DOI] [PubMed] [Google Scholar]
- 40.Pednekar MS, Gupta PC. Prospective study of smoking and tuberculosis in India. Preventive Medicine. 2007;2007 Jun; 44(6):496–8. doi: 10.1016/j.ypmed.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 41.England LJ, Kim SY, Tomar SL, Ray CS, Gupta PC, et al. Non-cigarette tobacco use among women and adverse pregnancy outcomes. Acta Obstet Gynecol Scand. 2010;2010;89(4):454–64. doi: 10.3109/00016341003605719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta PC, Subramoney S. Smokeless tobacco use and risk of stillbirth: a cohort study in Mumbai, India. Epidemiology. 2006;2006 Jan. 17(1):47–51. doi: 10.1097/01.ede.0000190545.19168.c4. [DOI] [PubMed] [Google Scholar]
- 43.Gupta PC, Sreevidya S. Smokeless tobacco use, birth weight, and gestational age: population based prospective cohort study of 1217 women in Mumbai (Bombay), India. British Medical Journal. 2004;328:1538–40, 2004. doi: 10.1136/bmj.38113.687882.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Subramoney S, d'Espaignet ET, Gupta PC. Higher risk of stillbirth among lower and middle income women who do not use tobacco, but live with smokers. Acta Obstet Gynecol Scand. 2010;2010;89(4):572–7. doi: 10.3109/00016341003801656. [DOI] [PubMed] [Google Scholar]
- 45.Alwan A. Global status report on non-communicable diseases 2010. 2011. World Health Organization, Geneva, 2011.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
GATS Collaborating Group.
(DOCX)