Abstract
Background/Aim
Second generation antipsychotics (SGAs) are used to treat schizophrenia but can cause serious metabolic side-effects, such as obesity and diabetes. This study examined the effects of low to high doses of olanzapine on appetite/metabolic regulatory signals in the hypothalamus and brainstem to elucidate the mechanisms underlying olanzapine-induced obesity.
Methodology/Results
Levels of pro-opiomelanocortin (POMC), neuropeptide Y (NPY) and glutamic acid decarboxylase (GAD65, enzyme for GABA synthesis) mRNA expression, and cannabinoid CB1 receptor (CB1R) binding density (using [3H]SR-141716A) were examined in the arcuate nucleus (Arc) and dorsal vagal complex (DVC) of female Sprague Dawley rats following 0.25, 0.5, 1.0 or 2.0 mg/kg olanzapine or vehicle (3×/day, 14-days). Consistent with its weight gain liability, olanzapine significantly decreased anorexigenic POMC and increased orexigenic NPY mRNA expression in a dose-sensitive manner in the Arc. GAD65 mRNA expression increased and CB1R binding density decreased in the Arc and DVC. Alterations to neurotransmission signals in the brain significantly correlated with body weight and adiposity. The minimum dosage threshold required to induce weight gain in the rat was 0.5 mg/kg olanzapine.
Conclusions
Olanzapine-induced weight gain is associated with reduced appetite-inhibiting POMC and increased NPY. This study also supports a role for the CB1R and GABA in the mechanisms underlying weight gain side-effects, possibly by altering POMC transmission. Metabolic dysfunction can be modelled in the female rat using low, clinically-comparable olanzapine doses when administered in-line with the half-life of the drug.
Introduction
The second generation antipsychotic (SGA) olanzapine is prescribed to treat schizophrenia and a growing number of other disorders in adults and children [1]–[8], but can cause adverse metabolic side-effects including increased body weight [9], caloric intake [10], [11] and abdominal adiposity [12], [13], and reduced physical activity [14]–[16]. Metabolic side-effects are a growing concern due to co-morbidities such as diabetes and obesity [17], and are a risk factor for medication non-compliance [18]. A number of potential mechanisms for SGA-induced metabolic dysfunction have emerged over the past few years [19]–[21]. In particular, the histaminergic, serotonergic and dopaminergic neurotransmitter systems are thought to be highly implicated in SGA-induced body weight gain [21]–[26]. However, SGAs have a broad receptor binding profile that allows direct and indirect effects on multiple neural and peripheral signalling pathways [26], and further research into other candidate systems is required.
The hypothalamic arcuate nucleus (Arc) and the dorsal vagal complex (DVC) of the brainstem are well-documented for their role in appetite and energy homeostasis [27]–[29]; responding to the acute nutritional status and long-term regulation of energy stores in the body. Neurons of the Arc and DVC express Gi/o-coupled cannabinoid CB1 receptors (CB1R) [30], [31], which facilitate the effects of cannabinoids on appetite and energy metabolism [32]. Weight gain during olanzapine and clozapine treatment is associated with a CB1R gene polymorphism in individuals with chronic schizophrenia [33], and chronic high-dose risperidone treatment increases cannabinoid receptor agonist, [3H]CP-55940, binding density in the Arc of male rats [34]. We previously demonstrated a decrease in [3H]CP-55940 binding density in the DVC of rats treated with olanzapine, but not aripiprazole or haloperidol [35]. However, whether changes in receptor density were attributed to the CB1R is unclear due to the low specificity of the ligand used [36] and localisation of cannabinoid CB2 receptors in the brain [37]. Moreover, the effects of olanzapine on CB1R density in the Arc remain unknown.
The appetite enhancing effects of the major neuronal inhibitor, γ-aminobutyric acid (GABA) in the hypothalamus were reported more than 30 years ago [38]. GABAergic neurons in the Arc are sensitive to leptin [39], and GABA receptor agonists and antagonists stimulate and suppress feeding behaviour, respectively [40]. Down-regulated expression of glutamic acid decarboxylase (GAD, the GABA synthesising enzyme) has been observed in individuals with schizophrenia, bipolar and mood disorder, whereas antipsychotic drug treatment increases cortical GAD expression in rats and primates [41]. GAD exists as two isoforms, 65 and 67; the latter is found throughout the neuronal cytoplasm, whereas GAD65 is located primarily in the axon terminal [42]–[44] and is the predominant transcript in the hypothalamus of the adult rat brain [45]. However, to our knowledge the effects of olanzapine on GAD65 mRNA expression in the hypothalamic Arc or the DVC have not been investigated.
The Arc and DVC both express mRNA for orexigenic neuropeptide Y (NPY) and anorexigenic pro-opiomelanocortin (POMC) [46]–[48]. The POMC gene encodes for neuropeptides such as adrenocorticotropic hormone, β-endorphin and α-melanocortin stimulating hormone; the latter of which exerts its anorexigenic effects largely through melanocortin-3 and melanocortin-4 receptor (MC4-R) subtypes [49]. Conversely, the central application of NPY induces food intake in a number of species [50], hypolocomotor activity in rats [51], [52], and can lead to obesity following chronic over-exposure [53], [54]. Therefore, it is possible that interference in the balance of POMC and NPY by olanzapine may contribute to the drug's obesogenic liability. Several reports demonstrated increased NPY immunoreactivity in the Arc of clozapine-treated rats [55], [56], whereas chronic risperidone treatment in male rats had no effect on POMC or NPY expression, or body weight [34], which may be due to the lower sensitivity of male rats to SGA-induced metabolic side-effects compared to females [57]–[60]. Other studies have examined antipsychotic effects on NPY mRNA expression in the brain with region-dependent outcomes [61]–[65]. The effects of antipsychotics on POMC or NPY in the brainstem have not been examined and studies on hypothalamic appetite-regulating peptides during olanzapine treatment are confounding; one group reported an increase in orexigenic NPY and AgRP and a concurrent reduction in appetite-inhibiting POMC and cocaine- and amphetamine-related transcript (CART) [66], whilst another reported no change in several hypothalamic peptides, including NPY and POMC [67]. A key factor that may contribute to the difference in findings is drug dosage (i.e.: 1 mg/kg olanzapine [66] vs. a supratherapeutic dose of 3 mg/kg olanzapine [67] (b.i.d.). Indeed, metabolic outcomes can differ with antipsychotic dosage [68]–[71] and increased dose induces greater metabolic dysfunction in the rat [66], [72], [73], however, high antipsychotic dosages in the rat may not represent the clinic [74]. In addition, both studies had a large dosage interval, i.e.: 6–7 then 17–18 hourly treatments, b.i.d. [66], [67]. As the half-life of olanzapine is 5.1 hours in the rat brain with high levels remaining after 8-hours [75], compared to approximately 75.2 hours in the human brain [76], multiple dosages are required in the rat in order to minimise drug fluctuations below sub-therapeutic D2 receptor occupancy levels [74], [77]. Therefore, it may be possible to model olanzapine-induced metabolic dysfunction in the rat using low olanzapine dosages when administered in accordance with the half-life of the drug, i.e.: 8 hourly (t.i.d.) within in 24-hours.
Using an established rat model of olanzapine-induced metabolic dysfunction [35], [70], [78]–[80], this study aimed to investigate the mechanisms underlying weight gain associated with olanzapine treatment by examining its effects on POMC, NPY and GAD65 mRNA expression, and CB1R binding density (using the CB1R-specific ligand [3H]-SR141716A) in the Arc and DVC. Statistical correlations between these parameters in the brain and body weight, food intake and visceral adiposity were investigated. To identify the minimum dosage threshold required to induce metabolic change, rats were treated with different clinically-relevant olanzapine dosages, calculated based on comparable therapeutic in-vivo dopamine D2 receptor occupancy levels [74] and differences in body surface area between species [81]. Collectively, the present study demonstrates that olanzapine changes the balance of anorexigenic POMC and orexigenic NPY mRNA expression in the Arc, does not alter POMC or NPY in the DVC, and increases GAD65 mRNA expression but reduces CB1R density in both the hypothalamus and brainstem. These largely dose-sensitive changes may underlie a shift in energy balance that favours weight gain during olanzapine treatment. Metabolic dysfunction can be modelled in the female rat using low olanzapine doses when administered in-line with the half-life of the drug.
Methods
Ethics Statement
All experimental procedures were approved by the Animal Ethics Committee (Approval #: AE06/32), University of Wollongong, and complied with the Australian Code of Practice for the Care and Use of Animals for Scientific Purposes (2004). All efforts were made to minimise animal distress and prevent suffering.
Animals and Treatment
Seven week-old female Sprague Dawley rats (Animal Resources Centre, Perth, WA, Australia), housed in 12-h light–dark cycle (lights on 07:00, 22°C) were habituated for 1-week, then randomly assigned to 0.25, 0.5, 1.0 or 2.0 mg olanzapine/kg (Zyprexa, Eli Lilly, Indianapolis, IN, USA) or vehicle (control) (n = 12), administered three-times daily in a sweet cookie dough pellet, as described previously [70]. Briefly, olanzapine tablets were de-coated and pulverized then the assigned dosage was added to measured dry ingredients. Water droplets were added immediately prior to administration to achieve a dry-dough consistency. After a 1-week teaching period, rats learnt to voluntarily self-administer a 0.3 g cookie-dough pellet either containing the assigned dosage of olanzapine, or plain cookie-dough without the drug (control group), offered by a metal spoon at 8-hourly intervals (3 pellets/day) for 14-days. Consumption of each pellet was observed to ensure complete dosing. Body weight and food intake measurements were recorded (n = 12). Animals were allowed ad libitum access to water and standard laboratory chow diet throughout the study. Animals were fasted for 4–6 hours then euthanized using sodium pentobarbitone 10–12 hours after the last treatment. Brain tissue was immediately frozen in liquid nitrogen and stored at −80°C. Visceral (perirenal and periovary) white fat pads were dissected and weighed (n = 12). Six brains were randomly selected from each treatment group for use in the mRNA expression and receptor binding experiments. Tissue was sectioned (14 µm, −18°C) along the coronal plane then stored at −20°C.
NPY, POMC and GAD65 mRNA In-Situ Hybridisation
POMC mRNA expression was observed using in-situ hybridisation techniques previously described by our laboratory [82], using the following specific antisense hybridisation probe: 5′-CGTTCTTGATGATGGCGTTCTTGAAGAGCGTCACCAGGGGCGTCT-3′ (J00612, 547–591). NPY mRNA expression was observed using in-situ hybridisation techniques previously described by our laboratory [65], [82], using the following specific antisense hybridisation probe: 5′-GAGTGTATCTGGCCATGTCCTCTGCTGGCGCGTCCTCGCCCGG-3′ (M15792, 1650–1693). GAD65 mRNA expression was observed using the following specific antisense hybridisation probe: 5′-GGCGTCCACACTGCAAGGCCTTGTCTCCCGTGTCATAGGACAGGTCAT-3′ (NM_012563.1, 1419-1372), as previously described by Ling et al., [83]. Oligonucleotide probes were terminally labelled using [35S]dATP (1000 Ci/mmol, Perkin Elmer, Waltham, MA, USA) in 10-fold molar excess and terminal transferase (Promega, Madison, WI, USA), then purified using a MicroSpin G-50 column (GE Healthcare Ltd, Buckinghamshire, UK). Hybridisation was performed by incubating slides in hybridisation buffer (4× SSC, 1× Denhardt's solution, 50% de-ionised formamide, 200 µg/ml sperm DNA, 100 µg/1 ml polyA, 120 µg/ml heparin, 20 mM sodium phosphate and labelled probe, pH 7.0) for 18-hours at 37°C. Slides were then washed in 1× SSC buffer at 55°C (3×30-minutes each) and incubated for 1-hour in SSC buffer at room temperature. Sections were dipped in Milli-Q water followed sequentially by 70% then 95% ethanol, and dried under a gentle stream of air. Autoradiographic images were captured on film (Kodak BioMax MR film, Rochester, NY, USA) exposed for 3-weeks. Films were quantified using a GS-800 Densitometer (Bio-Rad Laboratories, Inc), and analysis software (Quantity One, v4.6.7, Bio-Rad Laboratories, Inc, CA, USA). Values were derived from a standard curve generated from a [14C]-labelled autoradiographic standard (GE Healthcare Ltd, Buckinghamshire, UK) (mean binding nCi/g tissue equivalent vs. density). Slides were dipped in Emulsion solution (GE Healthcare Ltd, Buckinghamshire, UK) and exposed for 6-weeks, then stained with cresyl violet (Nissl stain) (Sigma-Aldrich, NSW, Australia), to allow further examination of positive signals at the cellular level.
CB1R Binding Density
CB1R binding density was detected using methods previously published by our laboratory [84]. Briefly, air-dried slides were pre-incubated for 15 min in incubation buffer containing 50 mM Tris–HCl buffer (pH 7.4) and 0.1% bovine serum albumin, at room temperature. Sections were then incubated with 10 nM [3H] SR141716A (52 Ci/mMol, Amersham, UK), a CB1R-specific inverse agonist, in buffer (pH 7.4) at room temperature for 60 minutes to determine total binding. Non-specific binding was determined by incubating subsequent sections in 10 nM [3H] SR141716A in the presence of 100 µM CP-55940, in buffer (pH 7.4) for 60 minutes at room temperature. Slides were washed in ice cold buffer (pH 7.4), (2×30 minutes), then dipped in distilled water and dried under a gentle stream of cool air. CB1R autoradiographic images were captured using a Beta Image camera (BioSpace, Paris, France), which counts the amount of β-particles emitted from the tissue (3.5 hours exposure) to determine the level of radioactivity bound to the brain sections. Radioactive levels were obtained in counts per minute per square millimetre of tissue (cpm/mm2), converted to nCi/mg tissue equivalent using standard tissue sections calibrated with commercial standards (Amersham, Buckinghamshire, United Kingdom), then transformed into fmol/mg tissue equivalent by taking into account the specific activity of the radioligand (52 Ci/mMol). Quantification was conducted using β-Image Plus software (version 4, BioSpace, Paris, France).
Quantification and Statistical Analysis
Quantification of autoradiographic images was performed on the hypothalamic Arc and the DVC of the brainstem, which were confirmed using a corresponding set of cresyl violet-stained slides and a standard rat brain atlas [85]. Data were analysed using SPSS (version 17.0, SPSS, Chicago, IL, USA). All data points were within ±2 standard deviations. One-Sample Kolmogorov-Smirnov tests revealed normal data distribution. One-way ANOVAs were employed to determine the effect of treatment on percentage body weight change, food intake, visceral adiposity, as well as NPY, POMC and GAD65 mRNA expression, and CB1R binding density in the hypothalamus and brainstem. ANOVAs were followed by multiple comparisons using post-hoc Dunnett-T tests where relevant (p<0.05). Correlations were identified using Pearson's correlation tests.
Results
Body Weight, Food Intake and Visceral Adiposity
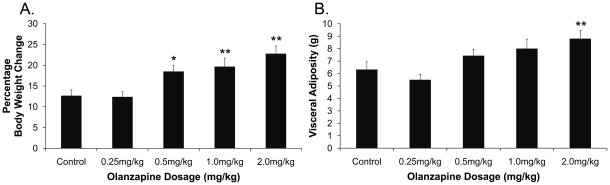
There was a significant effect of treatment on the percentage of body weight change from treatment day 0 (F 4,55 = 7.68, p<0.01). Compared to controls, olanzapine significantly increased percentage of body weight change in the 0.5 mg/kg (p<0.05), 1.0 mg/kg and 2.0 mg/kg (p<0.01) treatment groups, but not in the low dosage group of 0.25 mg/kg (p>0.05) (Figure 1A). Mean cumulative food intake significantly increased in the 2.0 mg/kg olanzapine dosage group compared to the control group (318.6±11.2 g vs. 269.4±11.1 g, p<0.05). An increase (7–8%) in food intake was also observed in the 0.5 mg/kg and 1.0 mg/kg olanzapine treatment groups, but did not reach significance compared to the controls (0.5 mg/kg: 289.1±13.9 g vs. 269.4±11.1 g, 1.0 mg/kg: 291.6±12.1 g vs. 269.4±11.1 g, p>0.05), and the low dosage group (0.25 mg/kg) did not differ to the control group (265.4±11.7 g vs. 269.4±11.1 g). Olanzapine treatment had a significant effect on visceral adiposity (F 4,55 = 4.60, p<0.01), with a significant increase observed in the 2.0 mg/kg olanzapine treatment group (p<0.05) and a trend for an increase in the 1.0 mg/kg dosage group (p = 0.09), but not in the lower dosage groups (p>0.05) (Figure 1B).
Figure 1. Weight Gain and Visceral Adiposity.
(A): Percentage body weight change and (B): visceral adiposity in female Sprague Dawley rats (n = 12/treatment group) treated with 0.25, 0.5, 1.0 or 2.0 mg/kg olanzapine or vehicle (control), (14-days, t.i.d). Data expressed as mean±SEM. *p<0.05, **p<0.01 vs. control.
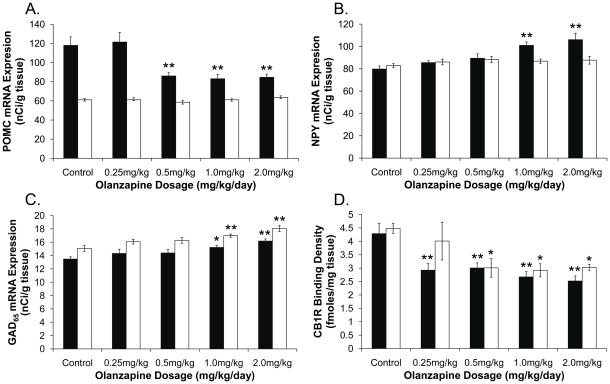
POMC and NPY mRNA Expression
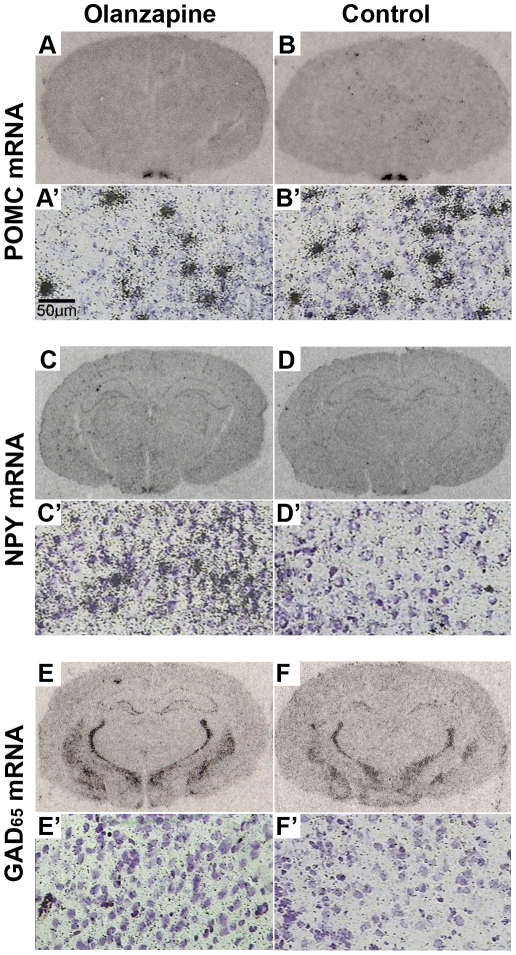
Examples of POMC and NPY mRNA expression in the hypothalamus are shown in Figure 2A–D. Olanzapine had a significant effect on POMC mRNA expression in the Arc (F 4,25 = 8.32, p<0.01), not in the DVC (F 4,25 = 1.44, p = 0.25) (Figure 3A). Post-hoc analysis identified a significant decrease in POMC mRNA expression in the Arc following dosages of 0.5 mg/kg, 1.0 mg/kg and 2.0 mg/kg (p<0.01) olanzapine, but not 0.25 mg/kg olanzapine (p = 0.90), compared to controls (Figure 3A). There was also a significant effect of treatment on NPY mRNA expression in the Arc (F 4,25 = 8.55, p<0.01), with a significant increase in the Arc following 1.0 mg/kg and 2.0 mg/kg olanzapine (Figure 3B), but not in the lower dosage groups (p = 0.34 and p = 0.11 for 0.25 mg/kg and 0.5 mg/kg olanzapine, respectively) (Figure 3B). NPY mRNA expression in the DVC was unaltered by olanzapine (F 4,25 = 0.73, p = 0.58) (Figure 3B).
Figure 2. Examples of POMC, NPY and GAD65 mRNA Expression Following Olanzapine Treatment.
Examples of pro-opiomelanocortin (POMC), neuropeptide Y (NPY) and glutamic acid decarboxylase 65 (GAD65) mRNA expression in the female Sprague Dawley rat brain following 2.0 mg/kg olanzapine treatment (A-A′, C-C′, E-E′) or vehicle (control) (B-B′, D-D′, F-F′) for 14-days (t.i.d.). (A–F): Low magnification film autoradiographs depicting mRNA expression in the rat brain, (A′–F′): High magnification emulsion/cresyl violet–stained slides showing mRNA expression specifically in the arcuate nucleus. Autoradiographs are examples of raw data used for the graphs depicted in Figure 3A–C and are average representations of 6 rats per treatment group.
Figure 3. Dosage Effects of Olanzapine Treatment on POMC, NPY and GAD65 mRNA Expression, and CB1R Binding Density.
(A): Pro-opiomelanocortin mRNA expression (nCi/g tissue), (B): neuropeptide Y mRNA expression (nCi/g tissue), (C): glutamic acid decarboxylase (GAD65) mRNA expression (nCi/g tissue), (D): cannabinoid CB1 receptor binding density (fmoles/mg tissue), in rats treated with 0.25. 0.5, 1.0 or 2.0 mg/kg olanzapine or vehicle (control) (14-days, t.i.d.) (n = 6/treatment group). Key: ▪ arcuate nucleus □ dorsal vagal complex. Data is expressed as mean ± SEM. *p<0.05, **p<0.01 vs. control.
GAD65 mRNA Expression
Examples of GAD65 mRNA expression are shown in Figure 2E–F. A significant effect of treatment on GAD65 mRNA expression was observed in the Arc (F 4,25 = 5.21, p<0.01) and DVC (F 4,25 = 7.73, p<0.01), with an increase following olanzapine dosages of 1.0 mg/kg (Arc p<0.05, DVC p<0.01) and 2.0 mg/kg (both regions p<0.01), but not in the 0.5 mg/kg or 0.25 mg/kg groups (p>0.05), compared to controls (Figure 3C).
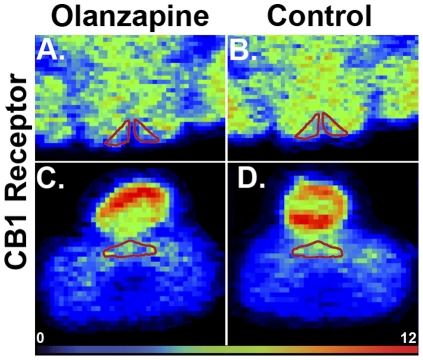
CB1R Binding Density
An example of CB1R binding density in the hypothalamus and DVC is shown in Figure 4. There was a significant effect of treatment on CB1R binding density in the Arc (F 4,25 = 7.48, p<0.01), with a reduction in all olanzapine treatment groups compared to controls (p<0.01) (Figure 3D). Olanzapine decreased CB1R binding density in the DVC (F 4,25 = 3.48, p<0.05) of animals treated with 0.5 mg/kg, 1.0 mg/kg or 2.0 mg/kg olanzapine (p<0.05), but not 0.25 mg/kg olanzapine (p = 0.43) (Figure 3D).
Figure 4. Example of CB1R Binding Density Following Olanzapine Treatment.
Example of cannabinoid CB1 receptor binding density (using [3H]SR-141716A) in the A, C: hypothalamic arcuate nucleus and B, D: dorsal vagal complex of the caudal brainstem of female Sprague Dawley rats following A, B: 2.0 mg/kg olanzapine treatment, C, D: vehicle (control) for 14-days (t.i.d.). Autoradiographs are examples of raw data used for the graphs depicted in Figure 3D and are average representations of 6 rats per treatment group.
Correlations
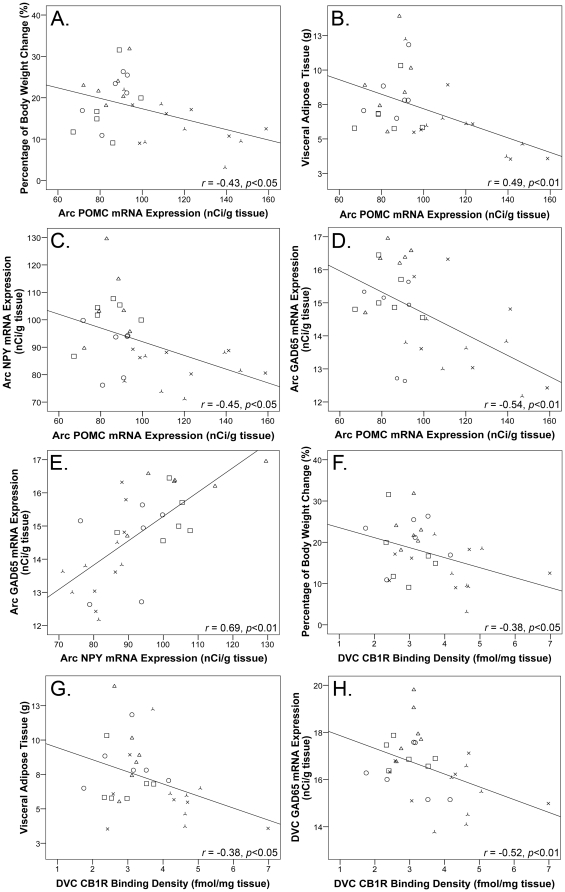
POMC mRNA expression in the Arc significantly correlated to percentage body weight change (r = −0.43, p<0.05), visceral adiposity (r = −0.49, p<0.01), NPY mRNA expression (r = −0.45, p<0.05), and GAD65 mRNA expression in the Arc (r = −0.54, p<0.01) (Figure 5A–D). There was a significant positive correlation between NPY and GAD65 mRNA expression in the Arc (r = 0.69, p<0.01) (Figure 5E), however the two factors did not correlate to percentage body weight change (p>0.05). CB1R binding density in the DVC correlated to percentage body weight change (r = −0.38, p<0.05), visceral adiposity (r = −0.38, p<0.05) and GAD65 mRNA expression in the DVC (r = −0.52, p<0.01) (Figure 5F–H), and a weak correlation was observed between CB1R binding density in the Arc and percentage body weight change (r = −0.33, p = 0.08).
Figure 5. Correlations.
Correlations between pro-opiomelanocortin (POMC) mRNA expression in the arcuate (Arc) nucleus and (A): percentage of body weight change, (B): visceral adipose tissue, (C): neuropeptide Y (NPY) mRNA expression in the Arc, (D): glutamic acid decarboxylase (GAD65) mRNA expression in the Arc, (E): Arc NPY and GAD65 mRNA expression, (F): cannabinoid CB1 receptor (CB1R) binding density in the dorsal vagal complex (DVC) and percentage of body weight changed, (G): DVC CB1R binding density and visceral adipose tissue, and (H): DVC CB1R binding density and GAD65 mRNA expression, following 14-days olanzapine treatment or vehicle (control). Correlation analyses were made from raw data underlying the graphs presented in Figures 1 and 3. Key: <$>\raster="rg1"<$> control, ×0.5 mg/kg, ○ 0.5 mg/kg, □ 1.0 mg/kg, ▵ 2.0 mg/kg olanzapine.
Discussion
We found that olanzapine alters signals in the hypothalamus and brainstem that are implicated in appetite and energy homeostasis in a largely dose-sensitive manner. These changes may underlie a shift in energy balance that favours weight gain. The data support a role for POMC in the mechanisms underlying olanzapine-induced obesity. Reduced POMC satiety signalling leads to obesity in the clinic and in animal models of obesity, for example, POMC mRNA expression is attenuated in genetically obese Zucker rats [86], tubby mice (tub gene mutation) [87] and diet-induced obese mice [88]. In addition, genetic POMC deficiency leads to obesity in humans [89] and mice [90], and MC4-R deficiency leads to morbid obesity associated with enhanced adiposity and chronic hyperphagia [91]. The result of unaltered POMC mRNA expression in the DVC was not entirely surprising as the role of POMC neurons in the DVC is not well-characterised, and functional and chemical distinctions to the Arc have been identified [92], [93].
NPY mRNA expression was upregulated in the Arc following 1.0 mg/kg and 2.0 mg/kg olanzapine treatment, however no significant correlation with weight gain was observed. This is consistent with some NPY transgenic and deficiency models i.e.: mice and rats that over-express NPY do not have a hyperphagic/obese phenotype [94], and genetic modelling of NPY-deficiency does not result in reduced body weight, adiposity, or food intake [95]–[97]. However, it is possible that NPY had an indirect effect on weight gain in olanzapine-treated animals, for example by inhibiting POMC. Indeed, NPY neurons synapse on POMC cell bodies and can inhibit their spontaneous activity [98]–[100], however, unlike POMC, NPY mRNA expression did not change in the 0.5 mg/kg olanzapine treatment group suggesting a role for other systems in POMC regulation. The dosage response of NPY mRNA expression was in-line with the increase in GAD65 mRNA expression in the 1.0 mg/kg and 2.0 mg/kg olanzapine treatment groups, although GAD65 mRNA expression increased in both the Arc and DVC. Upregulated GABAergic signalling during weight gain is consistent with previous reports that whilst NPY and/or AgRP gene deficiency is insufficient to reduce food intake [101], ablation of NPY/AgRP/GABA neurons results in acute hypophagia [102] and deletion of vesicular GABA transporter in AgRP neurons (which co-express NPY) results in a lean, obesity-resistant phenotype in mice [103]. GABA is co-localised in approximately 30% of POMC [104] and NPY/AgRP neurons in the Arc [105], and GABA derived from NPY/GABA axons can suppress spontaneous firing of POMC neurons [98]. In addition, a dense population of leptin-responsive, largely non-AgRP GABAergic neurons that increase inhibitory post-synaptic currents in POMC neurons were recently identified in the Arc [39]. Therefore, the increase in Arc GAD mRNA expression observed in the present study may have arisen from a number of GABAergic sources.
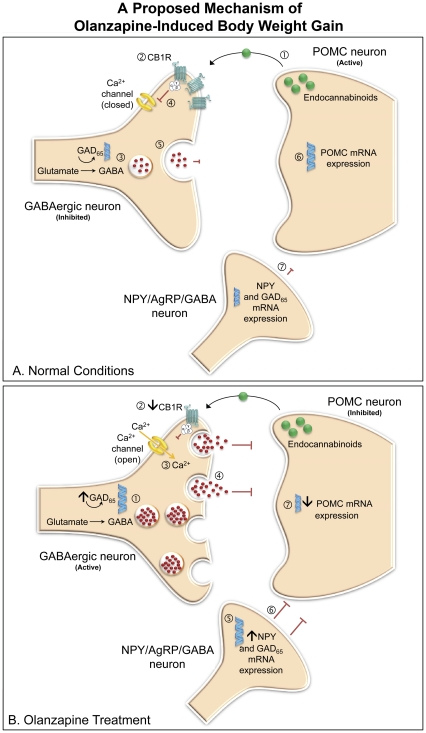
Olanzapine treatment elicited a robust reduction in CB1R density in the Arc and DVC. Using the CB1R-specific ligand, [3H]-SR141716A, we confirm that our original findings of a reduction in [3H]CP-55940 binding density in the DVC during olanzapine treatment [35] were attributed to the CB1R sub-type and extend these findings into the hypothalamus. CB1R number and cell signal transduction pathways decrease following over-exposure to agonists [106] and animal models of obesity, for example obese db/db and ob/ob mice, and fatty Zucker rats, exhibit elevated hypothalamic endocannabinoid levels [107]. Therefore, reduced CB1R binding density following olanzapine treatment may be a result of increased endogenous cannabinoids. Endogenous cannabinoids play an important regulatory role in synaptic transmission by modulating neuronal excitatory and inhibitory input [108], [109]. Interestingly, POMC neurons secrete endocannabinoids under basal conditions that retrogradely activate CB1Rs expressed on GABAergic neurons [110], [111]. G-protein sub-units coupled to the CB1R inhibit the opening of calcium channels, which reduces vesicular release of GABA [109]. CB1R activation can relieve inhibitory input to the post-synaptic POMC neuron [110]–[112]. We suggest that reduced CB1R density during olanzapine treatment may diminish cannabinoid-regulated inhibition of GABA, and therefore enhance GABAergic input to POMC neurons, suppressing POMC and encouraging body weight gain (Figure 6). In addition, anandamide and CP-55940 increase NPY release in the hypothalamus [113], therefore, increased endocannabinoid levels may contribute to an increase in NPY during olanzapine treatment that further suppresses POMC (Figure 6). CB1Rs can also modulate GABA and glutamate release in the DVC [30], however the functional implications of changes in CB1R density and GAD65 mRNA expression during olanzapine treatment require further investigation. Additionally, the influence of olanzapine on other neurotransmitter systems may play a role in the mechanisms underlying SGA-induced weight gain [25], [114]. For example, olanzapine is a potent histamine H1 receptor antagonist [115] and antipsychotic affinity for the H1 receptor can predict its weight gain liability [114], however the underlying mechanisms for the effect of the H1 receptor on antipsychotic-induced body weight may be independent of melanocortinergic neurotransmission [116]. On the other hand, dopamine D1 and D2 receptor antagonism influences hypothalamic NPY mRNA expression [117]–[119] and serotonin 5-HT2C receptor agonists can activate POMC neurons [120], [121], therefore, the antagonistic affinity of olanzapine to D2 and 5-HT2C receptors [122], [123] may contribute to its weight gain side-effects [24]. These receptors may form broader components of the mechanism proposed in the present study, however further research is necessary.
Figure 6. A Proposed Mechanism for Olanzapine-Induced Weight Gain through Interactions Between POMC, NPY, CB1 and GABA systems.
(A) Normal Conditions. Schematic illustrating proposed inhibitory synaptic transmission to the POMC neuron modulated by NPY, cannabinoid and GABAergic systems under normal conditions. (1) Endogenous cannabinoids are released from the post-synaptic POMC neuron and retrogradely activate CB1 receptors located on the non-AgRP GABAergic neuron (2). GABA is synthesised from glutamate via the rate limiting enzyme GAD (3), however G-protein sub-units coupled to the CB1R inhibit the opening of calcium channels (4), which reduces vesicular release of GABA from the presynaptic terminal to the POMC neuron (5), disinhibiting POMC (6). A number of NPY neurons co-express GABA and can also inhibit POMC. These NPY/AgRP/GABA neurons synapse on POMC neurons and can regulate POMC cell activity (7). (B) Olanzapine Treatment: Our data demonstrates that olanzapine decreases POMC mRNA expression and CB1R binding density, whilst simultaneously increasing NPY and GAD mRNA expression. Based on these findings we suggest a potential mechanism contributing to weight gain during olanzapine treatment. (1) Increased GAD mRNA expression enhances the potential for GABA production, whilst (2) decreased CB1R density following olanzapine treatment may remove inhibition of calcium channels (3) and allow vesicular release of GABA (4). The combined effect may be to increase GABA production and release. (5) Olanzapine increases NPY mRNA expression, which can inhibit POMC activation (6). Therefore, reduced CB1R density, and enhanced GAD and NPY may contribute to the suppression of POMC (7). As POMC is an important anorexigenic peptide, its prolonged inhibition during olanzapine treatment may lead to increased body weight and adiposity side-effects.
Our finding of a decrease in POMC and increase in NPY mRNA expression during olanzapine treatment coincide with Ferno et al [66], but contrast to the lack of change reported by Davoodi et al [67]. As discussed earlier, these studies differ in olanzapine dosage and treatment interval [66], [67]. Additionally, in Davoodi's study animals were not fasted and PCR methods were used to detect expressional changes in the whole hypothalamus [67], whereas rats were fasted prior to euthanasia and in-situ hybridisation techniques were utilised to target expression specifically in the Arc in the present study and [66]. Furthermore, patterns of daily changes in hypothalamic NPY and POMC gene expression have been reported [124], therefore timing of euthanasia may also confound results. A previous study from our laboratory reported a drug withdrawal response of NPY mRNA expression to olanzapine treatment cessation, i.e.: no change in Arc NPY mRNA expression after 2-hour drug washout and a decrease after 48-hour withdrawal after 5-weeks olanzapine treatment [65]. As body weight associated with olanzapine treatment follows a ‘peak-and-plateau’ trend over time [71], [79], [125], the lack of change in NPY mRNA expression [65] may be related to compensatory mechanisms that coincide with a plateau in body weight. Further investigation into the time-dependent pattern of NPY mRNA expression during chronic olanzapine treatment would be useful.
Secher et al. [34] reported increased [3H]CP-55940 binding density in the Arc following 28-days risperidone treatment, and observed a significant correlation between plasma drug levels and visceral adiposity. These results are similar to our study as olanzapine influenced CB1R density in the Arc and changes in CB1R density correlated with adiposity. Differences in the direction of CB1R density change may be attributed to several differences in experimental design in Secher et al.'s study [34], including drug dosage above the upper clinical limit [34], administration method i.e.: continuous drug application via mini-pump with no drug washout period, and treatment duration as time-dependent changes in CB1R density and transduction pathways have been reported [106]. Neither drugs have an affinity for the CB1R (>10,000 Ki (nM) [126], [127]), indicating that effects on the CB1R are secondary changes and exactly how these SGAs influence CB1Rs should be investigated in future studies. An olanzapine-induced decrease in CB1R binding density seems contrary to the orexigenic influence of CB1R activation, and appetite suppression of CB1R blockade [128]. However, there is vast potential for the endogenous cannabinoid system to modulate metabolism, including central and peripheral effects on food intake and reward aspects of feeding, glucose and lipid metabolism, and energy expenditure [129]–[136]; aspects of which may contribute to the weight loss efficacy of rimonabant [135]. Olanzapine-induced weight gain is associated with increased GABA and decreased CB1R density, whereas anorexigenic rimonabant, decreases GABA release from NPY/AgRP/GABA neurons, possibly via modulation of cannabinoid-sensitive opioid peptides [112]. This suggests that although olanzapine and rimonabant influence the CB1R, they exert their effects through different modes of action.
The doses used in the present study were selected based on the recommended clinical olanzapine dosage range of 5–20 mg/day [70], [74], [81] excluding the 0.25 mg/kg treatment group, which was included as a minimum response threshold. Olanzapine was administered every 8-hours, based on the half-life of olanzapine in the rat brain [75], to minimise inappropriate peaks and troughs in drug levels between treatments [74]. The present study demonstrates that olanzapine-induced metabolic dysfunction can be modelled in the female rat using low olanzapine dosages when treatment is administered in accordance with the half-life of the drug. In addition, treatment was voluntarily self-administered orally in a cookie-dough pellet, which aimed to minimise potential handling stress [137] and maintain a consistently high drug dosage in the brain [74], [75]. Oral drug administration in rats requires a teaching period to ensure voluntary pellet consumption, however this method resembles clinical administration and may circumvent limitations reported using other administration techniques, such as mini-pump, injection and gavage [74], [138]–[140]. Consistent with the clinic [141], olanzapine has a sedative effect in the rat at high doses [72] and we previously reported a general trend of reduced locomotor activity in response to increasing olanzapine dosage [70]. It is possible that sedation plays a role in weight gain during olanzapine treatment, however, as hyperphagia was only apparent in the high dosage group (2 mg/kg olanzapine) in the present study, it is unlikely that sedation influenced the animal's ability to consume food.
In conclusion, our data demonstrates that olanzapine, an antipsychotic drug with a high metabolic liability, alters key metabolic signals in the hypothalamus and brainstem in a manner that favours positive energy balance and may contribute to its weight gain/obesity side-effects. Olanzapine decreases anorexigenic POMC, increases orexigenic NPY, and alters CB1R and GABAergic signalling in a largely dose-sensitive manner. Low dosages of 0.5 mg/kg and 1.0 mg/kg olanzapine (t.i.d.) were sufficient to induce metabolic changes. Drug dosage may contribute, in-part, to inconsistencies observed between reports in the literature. Enhanced body weight and visceral adiposity during olanzapine treatment are associated with reduced anorexigenic POMC mRNA expression. We propose that increased NPY and enhanced inhibitory GABAergic input, possibly through reduced CB1R density, may contribute to POMC inhibition (Figure 6). However, the present study has several limitations, firstly, statistical correlations do not provide direct evidence of a causal link, and secondly, changes to mRNA and receptor binding density may not reflect a functional protein change, therefore further studies are required to confirm the mechanism proposed in the present study. Examination of olanzapine's effects on the GAD67 isoform and other hypothalamic neuropeptides, such as AgRP and CART, would be useful, as well as investigation into the time-response of all parameters at different intervals during treatment. Finally, as CB1R density decreased in all olanzapine dosage groups, experiments using lower dosages are required to identify the minimum dosage threshold. Taken together, this study supports a role for the melanocortinergic, GABAergic and cannabinoid systems in the underlying mechanisms contributing to olanzapine-induced weight gain side-effects and provides direction on dosage consideration for future animal modelling studies.
Acknowledgments
We sincerely thank Dr Kai Kang, Dr Mei Han, Ms Kelly Liu and Ms Jiamei Lian for their expert technical assistance.
Footnotes
Competing Interests: The authors have read the journal's policy and have the following conflicts: CD received an honorarium from Eli Lilly, Australia, for presenting at the Cutting Edge Debate, Melbourne (2010). This does not alter the authors' adherence to all PLoS ONE policies on sharing data and materials.
Funding: This study was supported by a University of Wollongong (www.uow.edu.au) University Research Centre (URC) grant to CD, an Australian National Health and Medical Research Council (NHMRC, www.nhmrc.gov.au) grant to XH and CD (ID 635231), and by the Schizophrenia Research Institute (SRI, www.schizophreniaresearch.org.au), utilising infrastructure funding from New South Wales Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ballard C, Waite J, Birks J. Atypical antipsychotics for aggression and psychosis in Alzheimer's disease. Cochrane Database of Systematic Reviews. 2006;2006:Art. No.: CD003476. doi: 10.1002/14651858.CD003476.pub2. DOI: 003410.001002/14651858.CD14003476.pub14651852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brambilla F, Monteleone P, Maj M. Olanzapine-induced weight gain in anorexia nervosa: Involvement of leptin and ghrelin secretion? Psychoneuroendocrinology. 2007;32:402–406. doi: 10.1016/j.psyneuen.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Bridle C, Palmer S, Bagnall AM, Darba J, Duffy S, et al. A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder. Health Technol Assess. 2004;8:iii–iv. doi: 10.3310/hta8190. [DOI] [PubMed] [Google Scholar]
- 4.Budman C, Gayer A, Lesser M, Shi Q, Bruun R. An open-label study of the treatment efficacy of olanzapine for Tourette's disorder. J Clin Psychiatry. 2001;62:290–294. doi: 10.4088/jcp.v62n0412. [DOI] [PubMed] [Google Scholar]
- 5.Centorrino F, Eakin M, Bahk W-M, Kelleher JP, Goren J, et al. Inpatient Antipsychotic Drug Use in 1998, 1993, and 1989. Am J Psychiatry. 2002;159:1932–1935. doi: 10.1176/appi.ajp.159.11.1932. [DOI] [PubMed] [Google Scholar]
- 6.De Hert M, Dobbelaere M, Sheridan EM, Cohen D, Correll CU. Metabolic and endocrine adverse effects of second-generation antipsychotics in children and adolescents: A systematic review of randomized, placebo controlled trials and guidelines for clinical practice. Eur Psychiat. 2011;26:144–158. doi: 10.1016/j.eurpsy.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Frenchman IB. Atypical antipsychotics for nursing home patients: a retrospective chart review. Drugs & Aging. 2005;22:257–264. doi: 10.2165/00002512-200522030-00006. [DOI] [PubMed] [Google Scholar]
- 8.Pickar D, Vinik J, Bartko JJ. Pharmacotherapy of Schizophrenic Patients: Preponderance of Off-Label Drug Use. PLoS ONE. 2008;3:e3150. doi: 10.1371/journal.pone.0003150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newcomer J. Second-Generation Atypical Antipsychotics and Metabolic Effects. A Comprehensive Literature Review. CNS Drugs. 2005;19:1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- 10.Eder U, Mangweth B, Ebenbichler C, Weiss E, Hofer A, et al. Association of olanzapine-induced weight gain with an increase in body fat. Am J Psych. 2001;158:1719. doi: 10.1176/appi.ajp.158.10.1719. [DOI] [PubMed] [Google Scholar]
- 11.Gothelf D, Falk B, Singer P, Kairi M, Phillip M, et al. Weight Gain Associated With Increased Food Intake and Low Habitual Activity Levels in Male Adolescent Schizophrenic Inpatients Treated With Olanzapine. Am J Psychiatry. 2002;159:1055–1057. doi: 10.1176/appi.ajp.159.6.1055. [DOI] [PubMed] [Google Scholar]
- 12.Ryan MCM, Flanagan S, Kinsella U, Keeling F, Thakore JH. The effects of atypical antipsychotics on visceral fat distribution in first episode, drug-naive patients with schizophrenia. Life Sci. 2004;74:1999–2008. doi: 10.1016/j.lfs.2003.08.044. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Z-J, Yao Z-J, Liu WEN, Fang QUN, Reynolds GP. Effects of antipsychotics on fat deposition and changes in leptin and insulin levels: Magnetic resonance imaging study of previously untreated people with schizophrenia. Br J Psychiatry. 2004;184:58–62. doi: 10.1192/bjp.184.1.58. [DOI] [PubMed] [Google Scholar]
- 14.Allison DB, Newcomer JW, Dunn AL, Blumenthal JA, Fabricatore AN, et al. Obesity Among Those with Mental Disorders: A National Institute of Mental Health Meeting Report. Am J Prev Med. 2009;36:341–350. doi: 10.1016/j.amepre.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 15.Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med. 1999;29:697–701. doi: 10.1017/s0033291798008186. [DOI] [PubMed] [Google Scholar]
- 16.Archie S, Wilson J, Osborne S, Hobbs H, McNiven J. Pilot study: access to fitness facility and exercise levels in olanzapine-treated patients. Can J Psychiatry. 2003;48:628–632. doi: 10.1177/070674370304800910. [DOI] [PubMed] [Google Scholar]
- 17.Rader DJ. Effect of Insulin Resistance, Dyslipidemia, and Intra-abdominal Adiposity on the Development of Cardiovascular Disease and Diabetes Mellitus. Am J Med. 2007;120:S12–S18. doi: 10.1016/j.amjmed.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Weiden PJ, Mackell JA, McDonnell DD. Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res. 2004;66:51–57. doi: 10.1016/s0920-9964(02)00498-x. [DOI] [PubMed] [Google Scholar]
- 19.Coccurello R, Moles A. Potential mechanisms of atypical antipsychotic-induced metabolic derangement: Clues for understanding obesity and novel drug design. Pharmacol Ther. 2010;127:210–251. doi: 10.1016/j.pharmthera.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Starrenburg FCJ, Bogers JPAM. How can antipsychotics cause diabetes mellitus? Insights based on receptor-binding profiles, humoral factors and transporter proteins. Eur Psychiat. 2009;24:164–170. doi: 10.1016/j.eurpsy.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Reynolds GP, Kirk SL. Metabolic side effects of antipsychotic drug treatment - pharmacological mechanisms. Pharmacol Ther. 2010;125:169–179. doi: 10.1016/j.pharmthera.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 22.Deng C, Weston-Green K, Huang X-F. The role of histaminergic H1 and H3 receptors in food intake: A mechanism for atypical antipsychotic-induced weight gain? Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:1–4. doi: 10.1016/j.pnpbp.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 23.Kim SF, Huang AS, Snowman AM, Teuscher C, Snyder SH. Antipsychotic drug-induced weight gain mediated by histamine H1 receptor-linked activation of hypothalamic AMP-kinase. Proceedings of the National Academy of Sciences. 2007;104:3456–3459. doi: 10.1073/pnas.0611417104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirk S, Glazebrook J, Grayson B, Neill J, Reynolds G. Olanzapine-induced weight gain in the rat: role of 5-HT2C and histamine H1 receptors. Psychopharmacology. 2009;207:119–125. doi: 10.1007/s00213-009-1639-8. [DOI] [PubMed] [Google Scholar]
- 25.Matsui-Sakata A, Ohtani H, Sawada Y. Receptor occupancy-based analysis of the contributions of various receptors to antipsychotics-induced weight gain and diabetes mellitus. Drug Metabolism and Pharmacokinetics. 2005;20:368–378. doi: 10.2133/dmpk.20.368. [DOI] [PubMed] [Google Scholar]
- 26.Nasrallah H. Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles. Mol Psychiat. 2008;13:27–35. doi: 10.1038/sj.mp.4002066. [DOI] [PubMed] [Google Scholar]
- 27.Berthoud H-R. Multiple neural systems controlling food intake and body weight. Neurosci Biobehav Rev. 2002;26:393–428. doi: 10.1016/s0149-7634(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 28.Broberger C, Hökfelt T. Hypothalamic and vagal neuropeptide circuitries regulating food intake. Physiol Behav. 2001;74:669–682. doi: 10.1016/s0031-9384(01)00611-4. [DOI] [PubMed] [Google Scholar]
- 29.Faulconbridge LF, Grill HJ, Kaplan JM, Daniels D. Caudal brainstem delivery of ghrelin induces fos expression in the nucleus of the solitary tract, but not in the arcuate or paraventricular nuclei of the hypothalamus. Brain Res. 2008;1218:151–157. doi: 10.1016/j.brainres.2008.04.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derbenev AV, Stuart TC, Smith BN. Cannabinoids suppress synaptic input to neurones of the rat dorsal motor nucleus of the vagus nerve. J Physiol (Lond) 2004;559:923–938. doi: 10.1113/jphysiol.2004.067470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berrendero F, Romero J, García-Gil L, Suarez I, De la Cruz P, et al. Changes in cannabinoid receptor binding and mRNA levels in several brain regions of aged rats. Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1998;1407:205–214. doi: 10.1016/s0925-4439(98)00042-8. [DOI] [PubMed] [Google Scholar]
- 32.Bermudez-Silva FJ, Viveros MP, McPartland JM, Rodriguez de Fonseca F. The endocannabinoid system, eating behavior and energy homeostasis: The end or a new beginning? Pharmacol Biochem Behav. 2010;95:375–382. doi: 10.1016/j.pbb.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 33.Tiwari AK, Zai CC, Likhodi O, Lisker A, Singh D, et al. A Common Polymorphism in the Cannabinoid Receptor 1 (CNR1) Gene is Associated with Antipsychotic-Induced Weight Gain in Schizophrenia. Neuropsychopharmacology. 2010;35:1315–1324. doi: 10.1038/npp.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Secher A, Husum H, Holst B, Egerod KL, Mellerup E. Risperidone Treatment Increases CB1 Receptor Binding in Rat Brain. Neuroendocrinology. 2010;91:155. doi: 10.1159/000245220. [DOI] [PubMed] [Google Scholar]
- 35.Weston-Green K, Huang X-F, Han M, Deng C. The effects of antipsychotics on the density of cannabinoid receptors in the dorsal vagal complex of rats: implications for olanzapine-induced weight gain. Int J Neuropsychopharmacol. 2008;11:827–835. doi: 10.1017/S1461145708008560. [DOI] [PubMed] [Google Scholar]
- 36.Pertwee RG. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther. 1997;74:129–180. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- 37.Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, et al. Identification and Functional Characterization of Brainstem Cannabinoid CB2 Receptors. Science. 2005;310:329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 38.Meeker RB, Myers RD. GABA and glutamate: Possible metabolic intermediaries involved in the hypothalamic regulation of food intake. Brain Res Bull. 1980;5:253–259. [Google Scholar]
- 39.Vong L, Ye C, Yang Z, Choi B, Chua S, et al. Leptin Action on GABAergic Neurons Prevents Obesity and Reduces Inhibitory Tone to POMC Neurons. Neuron. 2011;71:142–154. doi: 10.1016/j.neuron.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meister B. Neurotransmitters in key neurons of the hypothalamus that regulate feeding behavior and body weight. Physiol Behav. 2007;92:263–271. doi: 10.1016/j.physbeh.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 41.Akbarian S, Huang H-S. Molecular and cellular mechanisms of altered GAD1/GAD67 expression in schizophrenia and related disorders. Brain Research Reviews. 2006;52:293–304. doi: 10.1016/j.brainresrev.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 42.Kaufman DL, Houser CR, Tobin AJ. Two Forms of the γ-Aminobutyric Acid Synthetic Enzyme Glutamate Decarboxylase Have Distinct Intraneuronal Distributions and Cofactor Interactions. J Neurochem. 1991;56:720–723. doi: 10.1111/j.1471-4159.1991.tb08211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Esclapez M, Tillakaratne NJ, Kaufman DL, Tobin AJ, Houser CR. Comparative localization of two forms of glutamic acid decarboxylase and their mRNAs in rat brain supports the concept of functional differences between the forms. J Neurosci. 1994;14:1834–1855. doi: 10.1523/JNEUROSCI.14-03-01834.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Martin DL, Rimvall K. Regulation of γ-Aminobutyric Acid Synthesis in the Brain. J Neurochem. 1993;60:395–407. doi: 10.1111/j.1471-4159.1993.tb03165.x. [DOI] [PubMed] [Google Scholar]
- 45.Feldblum S, Erlander MG, Tobin AJ. Different distributions of GAD65 and GAD67 mRNAS suggest that the two glutamate decarboxylases play distinctive functional roles. J Neurosci Res. 1993;34:689–706. doi: 10.1002/jnr.490340612. [DOI] [PubMed] [Google Scholar]
- 46.Schwartz MW, Woods SC, Porte D, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 47.Bronstein DM, Schafer MKH, Watson SJ, Akil H. Evidence that [beta]-endorphin is synthesized in cells in the nucleus tractus solitarius: detection of POMC mRNA. Brain Res. 1992;587:269–275. doi: 10.1016/0006-8993(92)91007-2. [DOI] [PubMed] [Google Scholar]
- 48.Wai S, Kindler P, Lam E, Zhang A, Yew D. Distribution of neuropeptide Y-immunoreactive neurons in the human brainstem, cerebellum, and cortex during development. Cell Mol Neurobiol. 2004;24:667–684. doi: 10.1023/B:CEMN.0000036404.39432.0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu Q, Palmiter RD. GABAergic signaling by AgRP neurons prevents anorexia via a melanocortin-independent mechanism. Eur J Pharmacol. 2011;660:21–27. doi: 10.1016/j.ejphar.2010.10.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beck B. Neuropeptide Y in normal eating and in genetic and dietary-induced obesity. Philosophical Transactions of the Royal Society B: Biological Sciences. 2006;361:1159–1185. doi: 10.1098/rstb.2006.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Heilig M, Murison R. Intracerebroventricular neuropeptide Y suppresses open field and home cage activity in the rat. Regul Pept. 1987;19:221–231. doi: 10.1016/0167-0115(87)90278-3. [DOI] [PubMed] [Google Scholar]
- 52.Heilig M, Wahlestedt C, Widerlöv E. Neuropeptide Y (NPY)-induced suppression of activity in the rat: evidence for NPY receptor heterogeneity and for interaction with [alpha]-adrenoceptors. Eur J Pharmacol. 1988;157:205–213. doi: 10.1016/0014-2999(88)90384-6. [DOI] [PubMed] [Google Scholar]
- 53.Beck B, Strickerkrongrad A, Nicolas JP, Burlet C. Chronic and continuous intracerebroventricular infusion of Neuropeptide-Y in Long-Evans rats mimics the feeding-behavior of obese Zucker rats. Int J Obes. 1992;16:295–302. [PubMed] [Google Scholar]
- 54.Stanley BG, Kyrkouli SE, Lampert S, Leibowitz SF. Neuropeptide Y chronically injected into the hypothalamus: A powerful neurochemical inducer of hyperphagia and obesity. Peptides. 1986;7:1189–1192. doi: 10.1016/0196-9781(86)90149-x. [DOI] [PubMed] [Google Scholar]
- 55.Obuchowicz E. Long-term treatment with chlorpromazine and haloperidol but not with sulpiride and clozapine markedly elevates neuropeptide Y-like immunoreactivity in the rat hypothalamus. Neuropeptides. 1996;30:471–478. doi: 10.1016/s0143-4179(96)90012-8. [DOI] [PubMed] [Google Scholar]
- 56.Kirk SL, Cahir M, Reynolds GP. Clozapine, but not haloperidol, increases neuropeptide Y neuronal expression in the rat hypothalamus. J Psychopharmacol (Oxf) 2006;20:577–579. doi: 10.1177/0269881106061199. [DOI] [PubMed] [Google Scholar]
- 57.Baptista T, Araujo de Baptista E, Ying Kin NMKN, Beaulieu S, Walker D, et al. Comparative effects of the antipsychotics sulpiride or risperidone in rats: I: Bodyweight, food intake, body composition, hormones and glucose tolerance. Brain Res. 2002;957:144–151. doi: 10.1016/s0006-8993(02)03616-8. [DOI] [PubMed] [Google Scholar]
- 58.Pouzet B, Mow T, Kreilgård M, Velschow S. Chronic treatment with antipsychotics in rats as a model for antipsychotic-induced weight gain in human. Pharmacol Biochem Behav. 2003;75:133–140. doi: 10.1016/s0091-3057(03)00042-x. [DOI] [PubMed] [Google Scholar]
- 59.Minet-Ringuet J, Even PC, Goubern M, Tomé D, de Beaurepaire R. Long term treatment with olanzapine mixed with the food in male rats induces body fat deposition with no increase in body weight and no thermogenic alteration. Appetite. 2006;46:254–262. doi: 10.1016/j.appet.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 60.Minet-Ringuet J, Even PC, Guesdon B, Tomé D, de Beaurepaire R. Effects of chronic neuroleptic treatments on nutrient selection, body weight, and body composition in the male rat under dietary self-selection. Behav Brain Res. 2005;163:204–211. doi: 10.1016/j.bbr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 61.Obuchowicz E, Krysiak R, Wieronska JM, Smialowska M, Herman ZS. Alterations in striatal neuropeptide Y system activity of rats with haloperidol-induced behavioral supersensitivity. Neuropeptides. 2005;39:515–523. doi: 10.1016/j.npep.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 62.Obuchowicz E, Turchan J. Influence of typical and atypical antipsychotics on neuropeptide Y-like immunoreactivity and NPY mRNA expression in rat striatum. Neuropeptides. 1998;32:473–480. doi: 10.1016/s0143-4179(98)90074-9. [DOI] [PubMed] [Google Scholar]
- 63.Obuchowicz E, Turchan J. Clozapine decreases neuropeptide Y-like immunoreactivity and neuropeptide Y mRNA levels in rat nucleus accumbens. Eur Neuropsychopharmacol. 1999;9:329–335. doi: 10.1016/s0924-977x(99)00003-6. [DOI] [PubMed] [Google Scholar]
- 64.Obuchowicz E, Krysiak R, Herman ZS. Does neuropeptide Y (NPY) mediate the effects of psychotropic drugs? Neurosci Biobehav Rev. 2004;28:595–610. doi: 10.1016/j.neubiorev.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 65.Huang XF, Deng C, Zavitsanou K. Neuropeptide Y mRNA expression levels following chronic olanzapine, clozapine and haloperidol administration in rats. Neuropeptides. 2006;40:213–219. doi: 10.1016/j.npep.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 66.Ferno J, Varela L, Skrede S, Vazquez MJ, Nogueiras R, et al. Olanzapine-Induced Hyperphagia and Weight Gain Associate with Orexigenic Hypothalamic Neuropeptide Signaling without Concomitant AMPK Phosphorylation. PLoS ONE. 2011;6:e20571. doi: 10.1371/journal.pone.0020571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Davoodi N, Kalinichev M, Korneev S, Clifton P. Hyperphagia and increased meal size are responsible for weight gain in rats treated sub-chronically with olanzapine. Psychopharmacology. 2009;203:693–702. doi: 10.1007/s00213-008-1415-1. [DOI] [PubMed] [Google Scholar]
- 68.Ota M, Mori K, Nakashima A, Kaneko Y, Fujiwara K, et al. Peripheral injection of risperidone, an atypical antipsychotic, alters the bodyweight gain of rats. Clin Exp Pharmacol Physiol. 2002;29:980–989. doi: 10.1046/j.1440-1681.2002.t01-1-03755.x. [DOI] [PubMed] [Google Scholar]
- 69.Hartfield A, Moore N, Clifton P. Effects of clozapine, olanzapine and haloperidol on the microstructure of ingestive behaviour in the rat. Psychopharmacology. 2003;167:115. doi: 10.1007/s00213-002-1368-8. [DOI] [PubMed] [Google Scholar]
- 70.Weston-Green K, Huang X-F, Deng C. Olanzapine treatment and metabolic dysfunction: a dose response study in female Sprague Dawley rats. Behav Brain Res. 2011;217:337–346. doi: 10.1016/j.bbr.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 71.Nemeroff C. Dosing the antipsychotic medication olanzapine. J Clin Psychiatry. 1997;58:45–49. [PubMed] [Google Scholar]
- 72.Albaugh V, Henry C, Bello N, Hajnal A, Lynch S, et al. Hormonal and metabolic effects of olanzapine and clozapine related to body weight in rodents. Obesity. 2006;14:36–50. doi: 10.1038/oby.2006.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cope MB, Nagy TR, Fernandez JR, Geary N, Casey DE, et al. Antipsychotic drug-induced weight gain: development of an animal model. Int J Obes Relat Metab Disord. 2005;29:607–614. doi: 10.1038/sj.ijo.0802928. [DOI] [PubMed] [Google Scholar]
- 74.Kapur S, VanderSpek SC, Brownlee BA, Nobrega J. Antipsychotic Dosing in Preclinical Models Is Often Unrepresentative of the Clinical Condition: A Suggested Solution Based on in Vivo Occupancy. J Pharmacol Exp Ther. 2003;305:625–631. doi: 10.1124/jpet.102.046987. [DOI] [PubMed] [Google Scholar]
- 75.Aravagiri M, Teper Y, Marder SR. Pharmacokinetics and tissue distribution of olanzapine in rats. Biopharm Drug Dispos. 1999;20:369–377. doi: 10.1002/1099-081x(199911)20:8<369::aid-bdd200>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 76.Tauscher J, Jones C, Remington G, Zipursky R, Kapur S. Significant dissociation of brain and plasma kinetics with antipsychotics. Mol Psychiat. 2002;7:317–321. doi: 10.1038/sj.mp.4001009. [DOI] [PubMed] [Google Scholar]
- 77.Kapur S, Wadenberg ML, Remington G. Are animal studies of antipsychotics appropriately dosed? Lessons from the bedside to the bench. Canadian Journal Of Psychiatry Revue Canadienne De Psychiatrie. 2000;45:241–246. doi: 10.1177/070674370004500302. [DOI] [PubMed] [Google Scholar]
- 78.Deng C, Weston-Green KL, Han M, Huang X-F. Olanzapine treatment decreases the density of muscarinic M2 receptors in the dorsal vagal complex of rats. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:915–920. doi: 10.1016/j.pnpbp.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 79.Han M, Deng C, Burne THJ, Newell KA, Huang X-F. Short- and long-term effects of antipsychotic drug treatment on weight gain and H1 receptor expression. Psychoneuroendocrinology. 2008;33:569–580. doi: 10.1016/j.psyneuen.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 80.Huang X-F, Han M, Huang X, Zavitsanou K, Deng C. Olanzapine differentially affects 5-HT2A and 2C receptor mRNA expression in the rat brain. Behav Brain Res. 2006;171:355–362. doi: 10.1016/j.bbr.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 81.Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. The FASEB Journal. 2007;22:659–661. doi: 10.1096/fj.07-9574LSF. [DOI] [PubMed] [Google Scholar]
- 82.Lin S, Storlien LH, Huang X-F. Leptin receptor, NPY, POMC mRNA expression in the diet-induced obese mouse brain. Brain Res. 2000;875:89–95. doi: 10.1016/s0006-8993(00)02580-4. [DOI] [PubMed] [Google Scholar]
- 83.Ling LL, Hughes LF, Caspary DM. Age-related loss of the GABA synthetic enzyme glutamic acid decarboxylase in rat primary auditory cortex. Neuroscience. 2005;132:1103–1113. doi: 10.1016/j.neuroscience.2004.12.043. [DOI] [PubMed] [Google Scholar]
- 84.Deng C, Han M, Huang X. No changes in densities of cannabinoid receptors in the superior temporal gyrus in schizophrenia. Neurosci Bull. 2007;23:341–347. doi: 10.1007/s12264-007-0051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. CA, USA: Elselvier Academic Press Inc; 2007. [Google Scholar]
- 86.Kim E-M, O'Hare E, Grace MK, Welch CC, Billington CJ, et al. ARC POMC mRNA and PVN [alpha]-MSH are lower in obese relative to lean Zucker rats. Brain Res. 2000;862:11–16. doi: 10.1016/s0006-8993(00)02060-6. [DOI] [PubMed] [Google Scholar]
- 87.Guan X-M, Yu H, Van der Ploeg LHT. Evidence of altered hypothalamic pro-opiomelanocortin/neuropeptide Y mRNA expression in tubby mice. Mol Brain Res. 1998;59:273–279. doi: 10.1016/s0169-328x(98)00150-8. [DOI] [PubMed] [Google Scholar]
- 88.Huang X-F, Han M, South T, Storlien L. Altered levels of POMC, AgRP and MC4-R mRNA expression in the hypothalamus and other parts of the limbic system of mice prone or resistant to chronic high-energy diet-induced obesity. Brain Res. 2003;992:9–19. doi: 10.1016/j.brainres.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 89.Krude H, Biebermann H, Luck W, Horn R, Brabant G, et al. Severe early-onset obesity, adrenal insufficiency and red hair pigmentation caused by POMC mutations in humans. Nat Genet. 1998;19:155–157. doi: 10.1038/509. [DOI] [PubMed] [Google Scholar]
- 90.Martin NM, Small CJ, Sajedi A, Liao XH, Weiss RE, et al. Abnormalities of the hypothalamo-pituitary-thyroid axis in the pro-opiomelanocortin deficient mouse. Regul Pept. 2004;122:169–172. doi: 10.1016/j.regpep.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 91.Cone R. Anatomy and regulation of the central melanocortin system. Nat Neurosci. 2005;8:571–578. doi: 10.1038/nn1455. [DOI] [PubMed] [Google Scholar]
- 92.Meister B, Gömüç B, Suarez E, Ishii Y, Dürr K, et al. Hypothalamic proopiomelanocortin (POMC) neurons have a cholinergic phenotype. Eur J Neurosci. 2006;24:2731–2740. doi: 10.1111/j.1460-9568.2006.05157.x. [DOI] [PubMed] [Google Scholar]
- 93.Zhang Y, Rodrigues E, Gao YX, King M, Cheng KY, et al. Pro-opiomelanocortin gene transfer to the nucleus of the solitary track but not arcuate nucleus ameliorates chronic diet-induced obesity. Neuroscience. 2010;169:1662–1671. doi: 10.1016/j.neuroscience.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ste Marie L, Luquet S, Cole T, Palmiter R. Modulation of neuropeptide Y expression in adult mice does not affect feeding. Proc Natl Acad Sci U S A 102: 18632–18637. Epub 12005 Dec. 2005;18638 doi: 10.1073/pnas.0509240102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Erickson JC, Clegg KE, Palmiter RD. Sensitivity to leptin and susceptibility to seizures of mice lacking neuropeptide Y. Nature. 1996;381:415–418. doi: 10.1038/381415a0. [DOI] [PubMed] [Google Scholar]
- 96.Hollopeter G, Erickson JC, Seeley RJ, Marsh DJ, Palmiter RD. Response of neuropeptide Y-deficient mice to feeding effectors. Regul Pept. 1998;75–76:383–389. doi: 10.1016/s0167-0115(98)00092-5. [DOI] [PubMed] [Google Scholar]
- 97.Lin S, Boey D, Herzog H. NPY and Y receptors: lessons from transgenic and knockout models. Neuropeptides. 2004;38:189–200. doi: 10.1016/j.npep.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 98.Cowley MA, Smart JL, Rubinstein M, Cerdan MG, Diano S, et al. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature. 2001;411:480. doi: 10.1038/35078085. [DOI] [PubMed] [Google Scholar]
- 99.Csiffa'ry A, Görcs TJ, Palkovits M. Neuropeptide Y innervation of ACTH-immunoreactive neurons in the arcuate nucleus of rats: a correlated light and electron microscopic double immunolabeling study. Brain Res. 1990;506:215–222. doi: 10.1016/0006-8993(90)91253-d. [DOI] [PubMed] [Google Scholar]
- 100.Roseberry AG, Liu H, Jackson AC, Cai X, Friedman JM. Neuropeptide Y-Mediated Inhibition of Proopiomelanocortin Neurons in the Arcuate Nucleus Shows Enhanced Desensitization in ob/ob Mice. Neuron. 2004;41:711–722. doi: 10.1016/s0896-6273(04)00074-1. [DOI] [PubMed] [Google Scholar]
- 101.Qian S, Chen H, Weingarth D, Trumbauer ME, Novi DE, et al. Neither Agouti-Related Protein nor Neuropeptide Y Is Critically Required for the Regulation of Energy Homeostasis in Mice. Molecular Cell Biology. 2002;22:5027–5035. doi: 10.1128/MCB.22.14.5027-5035.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gropp E, Shanabrough M, Borok E, Xu AW, Janoschek R, et al. Agouti-related peptide-expressing neurons are mandatory for feeding. Nat Neurosci. 2005;8:1289–1291. doi: 10.1038/nn1548. [DOI] [PubMed] [Google Scholar]
- 103.Tong Q, Ye C-P, Jones JE, Elmquist JK, Lowell BB. Synaptic release of GABA by AgRP neurons is required for normal regulation of energy balance. Nat Neurosci. 2008;11:998–1000. doi: 10.1038/nn.2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hentges ST, Nishiyama M, Overstreet LS, Stenzel-Poore M, Williams JT, et al. GABA Release from Proopiomelanocortin Neurons. J Neurosci. 2004;24:1578–1583. doi: 10.1523/JNEUROSCI.3952-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Horvath TL, Bechmann I, Naftolin F, Kalra SP, Leranth C. Heterogeneity in the neuropeptide Y-containing neurons of the rat arcuate nucleus: GABAergic and non-GABAergic subpopulations. Brain Res. 1997;756:283–286. doi: 10.1016/s0006-8993(97)00184-4. [DOI] [PubMed] [Google Scholar]
- 106.Howlett AC, Breivogel CS, Childers SR, Deadwyler SA, Hampson RE, et al. Cannabinoid physiology and pharmacology: 30 years of progress. Neuropharmacology. 2004;47:345–358. doi: 10.1016/j.neuropharm.2004.07.030. [DOI] [PubMed] [Google Scholar]
- 107.Di Marzo V, Goparaju SK, Wang L, Liu J, Batkai S, et al. Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature. 2001;410:822–825. doi: 10.1038/35071088. [DOI] [PubMed] [Google Scholar]
- 108.Alger BE. Retrograde signaling in the regulation of synaptic transmission: focus on endocannabinoids. Progress in Neurobiology. 2002;68:247–286. doi: 10.1016/s0301-0082(02)00080-1. [DOI] [PubMed] [Google Scholar]
- 109.Wilson RI, Nicoll RA. Endocannabinoid signaling in the brain. (Review: Neuroscience). Science. 2002;296:678(675). doi: 10.1126/science.1063545. [DOI] [PubMed] [Google Scholar]
- 110.Hentges ST, Low MJ, Williams JT. Differential Regulation of Synaptic Inputs by Constitutively Released Endocannabinoids and Exogenous Cannabinoids. J Neurosci. 2005;25:9746–9751. doi: 10.1523/JNEUROSCI.2769-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Nguyen Q, Wagner E. Estrogen differentially modulates the cannabinoid- induced presynaptic inhibition of amino acid neurotransmission in proopiomelanocortin neurons of the arcuate nucleus. Neuroendocrinology. 2007;84:123. doi: 10.1159/000096996. [DOI] [PubMed] [Google Scholar]
- 112.Menzies JRW, Ludwig M, Leng G. Direct and Indirect Effects of Cannabinoids on in vitro GABA Release in the Rat Arcuate Nucleus. J Neuroendocrinol. 2010;22:585–592. doi: 10.1111/j.1365-2826.2010.01990.x. [DOI] [PubMed] [Google Scholar]
- 113.Gamber KM, Macarthur H, Westfall TC. Cannabinoids augment the release of neuropeptide Y in the rat hypothalamus. Neuropharmacology. 2005;49:646–652. doi: 10.1016/j.neuropharm.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 114.Kroeze WK, Hufeisen SJ, Popadak BA, Renock SM, Steinberg S, et al. H1-Histamine receptor affinity predicts short-term weight gain for typical and atypical antipsychotic drugs. Neuropsychopharmacology. 2003;28:519–526. doi: 10.1038/sj.npp.1300027. [DOI] [PubMed] [Google Scholar]
- 115.Richelson E, Souder T. Binding of antipsychotic drugs to human brain receptors: Focus on newer generation compounds. Life Sci. 2000;68:29–39. doi: 10.1016/s0024-3205(00)00911-5. [DOI] [PubMed] [Google Scholar]
- 116.Yoshimatsu H. The neuronal histamine H1 and pro-opiomelanocortin-melanocortin 4 receptors: Independent regulation of food intake and energy expenditure. Peptides. 2006;27:326–332. doi: 10.1016/j.peptides.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 117.Kuo D-Y. Co-administration of dopamine D1 and D2 agonists additively decreases daily food intake, body weight and hypothalamic neuropeptide Y level in rats. J Biomed Sci. 2002;9:126–132. doi: 10.1007/BF02256023. [DOI] [PubMed] [Google Scholar]
- 118.Kuo D-Y. Hypothalamic neuropeptide Y (NPY) and the attenuation of hyperphagia in streptozotocin diabetic rats treated with dopamine D1/D2 agonists. British Journal of Pharmacology. 2006;148:640–647. doi: 10.1038/sj.bjp.0706754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pelletier G, Simard J. Dopaminergic regulation of pre-proNPY mRNA levels in the rat arcuate nucleus. Neurosci Lett. 1991;127:96–98. doi: 10.1016/0304-3940(91)90903-7. [DOI] [PubMed] [Google Scholar]
- 120.Heisler LK, Cowley MA, Tecott LH, Fan W, Low MJ, et al. Activation of Central Melanocortin Pathways by Fenfluramine. Science. 2002;297:609–611. doi: 10.1126/science.1072327. [DOI] [PubMed] [Google Scholar]
- 121.Qiu J, Xue C, Bosch MA, Murphy JG, Fan W, et al. Serotonin 5-Hydroxytryptamine2C Receptor Signaling in Hypothalamic Proopiomelanocortin Neurons: Role in Energy Homeostasis in Females. Mol Pharmacol. 2007;72:885–896. doi: 10.1124/mol.107.038083. [DOI] [PubMed] [Google Scholar]
- 122.Bymaster F, Calligaro D, Falcone J, Marsh R, Moore N, et al. Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology. 1996;14:87–96. doi: 10.1016/0893-133X(94)00129-N. [DOI] [PubMed] [Google Scholar]
- 123.Bymaster F, Hemrick-Luecke S, Perry K, Fuller R. Neurochemical evidence for antagonism by olanzapine of dopamine, serotonin, alpha1-adrenergic and muscarinic receptors in vivo in rats. Psychopharmacology. 1996;124:87–94. doi: 10.1007/BF02245608. [DOI] [PubMed] [Google Scholar]
- 124.Xu B, Kalra PS, Farmerie WG, Kalra SP. Daily Changes in Hypothalamic Gene Expression of Neuropeptide Y, Galanin, Proopiomelanocortin, and Adipocyte Leptin Gene Expression and Secretion: Effects of Food Restriction. Endocrinology. 1999;140:2868–2875. doi: 10.1210/endo.140.6.6789. [DOI] [PubMed] [Google Scholar]
- 125.Nasrallah H. A review of the effect of atypical antipsychotics on weight. Psychoneuroendocrinology. 2003;28:83–96. doi: 10.1016/s0306-4530(02)00114-2. [DOI] [PubMed] [Google Scholar]
- 126.NIMH Psychoactive Drug Screening Program website. Available: http://pdsp.med.unc.edu/kidb.php. Accessed 2011 Oct 20.
- 127.Roth B, Kroeze W, Patel S, Lopez E. The Multiplicity of Serotonin Receptors: Uselessly diverse molecules or an embarrassment of riches? The Neuroscientist. 2000;6:252–262. [Google Scholar]
- 128.Li C, Jones PM, Persaud SJ. Role of the endocannabinoid system in food intake, energy homeostasis and regulation of the endocrine pancreas. Pharmacol Ther. 2011;129:307–320. doi: 10.1016/j.pharmthera.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 129.Cavuoto P, Wittert GA. The role of the endocannabinoid system in the regulation of energy expenditure. Best Pract Res Cl En. 2009;23:79–86. doi: 10.1016/j.beem.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 130.Nogueiras R, Diaz-Arteaga A, Lockie SH, Velásquez DA, Tschop J, et al. The endocannabinoid system: Role in glucose and energy metabolism. Pharmacol Res. 2009;60:93–98. doi: 10.1016/j.phrs.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 131.Harrold J, Williams G. The cannabinoid system: a role in both the homeostatic and hedonic control of eating? Br J Nutr. 2003;90:729–734. doi: 10.1079/bjn2003942. [DOI] [PubMed] [Google Scholar]
- 132.Kirkham TC. Cannabinoids and appetite: Food craving and food pleasure. Int Rev Psychiatr. 2009;21:163–171. doi: 10.1080/09540260902782810. [DOI] [PubMed] [Google Scholar]
- 133.Gomez R, Navarro M, Ferrer B, Trigo JM, Bilbao A, et al. A Peripheral Mechanism for CB1 Cannabinoid Receptor-Dependent Modulation of Feeding. J Neurosci. 2002;22:9612–9617. doi: 10.1523/JNEUROSCI.22-21-09612.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Cota D, Marsicano G, Tschop M, Glubler Y, Flachskamm C, et al. The endogenous cannabinoid system affects energy balance via central orexigenic drive and peripheral lipogenesis. J Clin Invest. 2003;112:423–431. doi: 10.1172/JCI17725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sharkey KA, Pittman QJ. Central and Peripheral Signaling Mechanisms Involved in Endocannabinoid Regulation of Feeding: A Perspective on the Munchies. Sci STKE. 2005:pe15. doi: 10.1126/stke.2772005pe15. [DOI] [PubMed] [Google Scholar]
- 136.Kirkham T. Endocannabinoids and the neurochemistry of gluttony. J Neuroendocrinol. 2008;20:1099–1100. doi: 10.1111/j.1365-2826.2008.01762.x. [DOI] [PubMed] [Google Scholar]
- 137.Balcombe J, Barnard N, Sandusky C. Laboratory routines cause animal stress. Contemp Top Lab Anim. 2004;43:42–51. [PubMed] [Google Scholar]
- 138.Remington G, Mann S, McCormick P, Nobrega JN, Hahn M, et al. Modeling chronic olanzapine exposure using osmotic minipumps: Pharmacological limitations. Pharmacology Biochemistry and Behavior. 2011;100:86–89. doi: 10.1016/j.pbb.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 139.van der Zwaal EM, Luijendijk MCM, Adan RAH, la Fleur SE. Olanzapine-induced weight gain: Chronic infusion using osmotic minipumps does not result in stable plasma levels due to degradation of olanzapine in solution. Eur J Pharmacol. 2008;585:130–136. doi: 10.1016/j.ejphar.2007.11.078. [DOI] [PubMed] [Google Scholar]
- 140.de Meijer VE, Le HD, Meisel JA, Puder M. Repetitive orogastric gavage affects the phenotype of diet-induced obese mice. Physiol Behav. 2010;100:387–393. doi: 10.1016/j.physbeh.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Beasley JCM, Tollefson G, Tran P, Satterlee W, Sanger T, et al. Olanzapine versus placebo and haloperidol: Acute phase results of the North American double-blind olanzapine trial. Neuropsychopharmacology. 1996;14:111–123. doi: 10.1016/0893-133X(95)00069-P. [DOI] [PubMed] [Google Scholar]