Abstract
Background
The degree to which interpersonal problems of depressed patients improve over the course of cognitive therapy (CT) and relate to the quality of the therapeutic alliance and to symptom improvement, remain unclear.
Methods
We analyzed data of adult outpatients (N = 523) with major depressive disorder participating in a clinical trial to determine the factor structure of the Inventory of Interpersonal Problems-Circumplex (IIP-C) and to relate the observed factor scores to the quality of the therapeutic alliance and symptom improvement over the course of CT. Patients received 16–20 sessions protocol (50–60 minutes each) of individual CT according to the treatment manual by Beck et al. (1979).
Results
We found a three-factor structure (interpersonal distress, agency, and communion) of interpersonal problems. Interpersonal distress decreased (d = .90), but interpersonal style did not change substantively during CT (communion d = .03; agency d = .14). High initial agency scores related negatively to the therapeutic alliance (β = −.12), whereas high initial communion scores related positively to the therapeutic alliance (β = .15). Elevated pre-treatment interpersonal distress scores were related to both weaker therapeutic alliances (β = .13) and higher symptom levels throughout treatment (β = .10).
Limitations
All patients in this study had recurrent MDD and it is therefore uncertain whether the results would generalize to patients with other psychiatric disorders.
Conclusions
This study supports the use of the IIP-C as a comprehensive measure of patients' interpersonal style and interpersonal distress. The IIP-C measured before CT showed some predictive validity with respect to therapeutic alliance measured at the midpoint and therapy outcome. The clinical importance of these findings is discussed.
Keywords: Recurrent Depression, Cognitive Therapy, Personality, Interpersonal Style, Therapeutic Alliance
Introduction
Interpersonal problems refer to persistent difficulties that individuals experience in their social relationships (Horowitz et al., 1988; Horowitz et al., 1993). Patients seeking psychotherapy usually report some degree of such problems in addition to their primary symptoms (Horowitz et al., 1988). Moreover, patients with major depressive disorder (MDD) are significantly more distressed by their interpersonal problems than non-depressed individuals (Barrett and Barber, 2007). The broad aim of the present study was to document further the range of interpersonal problems in depressed patients, to determine the extent to which these problems change over a 12–14 week protocol of cognitive therapy (CT; Beck et al., 1979), and to examine relations among interpersonal problems, the therapeutic alliance, and therapy outcome.
Recent efforts to conceptualize interpersonal problems in patients with various clinical problems have relied primarily on the interpersonal circumplex, in which stable interpersonal dispositions are mapped along a two-dimensional space ranging from agency to submission on one axis and from communion to coldness on the other (Horowitz et al., 2006; Wiggins, 1982)2. Agency refers to persons' influence over others and includes traits such as autonomy, independence, and dominance, whereas communion describes involvement with others and includes traits such as cooperation and caring. One of the most frequently used assessment tools in this context is the Inventory of Interpersonal Problems-Circumplex version (IIP-C; Alden et al., 1990; Horowitz et al., 1988).
Previous research has investigated the stability of the IIP-C. Vittengl et al. (2003), for example, assessed interpersonal problems before and after CT in outpatients with recurrent MDD, and found that general distress decreased substantially following 20 sessions of CT, whereas agency and communion scores remained unchanged. From these findings, the authors concluded that the agency and communion dimensions of the IIP-C represent stable interpersonal styles, whereas general distress represents a state-like aspect of interpersonal functioning. In an attempt to replicate these findings, Holtforth et al. (2006) administered the IIP-C to a group of psychiatric outpatients with primarily anxiety and affective disorders, before and after an average of 29 sessions of eclectic psychotherapy. In contrast to the findings by Vittengl et al. (2003), Holtforth and colleagues found that both general distress and interpersonal style (agency and communion) changed during therapy, although distress changed more. Given the inconsistent findings, there is a need to investigate further the (in)stability of general distress and interpersonal style over the course of different types of psychotherapy.
Another relevant question is to what extent interpersonal style and distress relate to the therapeutic alliance and therapy outcome. Interpersonal theories of psychotherapy suggest that patients' friendly-submissive behaviors are complementary to therapists' friendly-dominant behaviors (Kiesler, 1983; Kiesler and Watkins, 1989; Tracey, 1993). Accordingly, patients' having a friendly-submissive interpersonal style should facilitate the therapeutic relationship and positively affect therapy outcome. In contrast, hostile-dominant behaviors likely would conflict with therapy goals, thus contributing to a poor therapeutic alliance and treatment outcome (Tracey, 1993). In terms of IIP-C structure, theory suggests that high communion and low agency are associated with better therapeutic relationships and outcomes. Consistent with this, most research to date indicates that in naturalistic settings, outpatients scoring high on the communion dimension show more symptom improvement over the course of short-term psychodynamic psychotherapy (Filak et al., 1986; Gurtman, 1996; Schauenburg et al., 2000).
Findings regarding the role of agency in predicting therapy outcome and symptom reduction over time are mixed. Some (Borkovec et al., 2002; Gurtman, 1996), but not all (Filak et al., 1986; Schauenburg et al., 2000) studies report an association between high agency scores and poor treatment outcome. Moreover, Ruiz et al. (2004) found that neither communion nor agency was associated with treatment outcome after controlling for general distress. Thus, although most studies support the influence of interpersonal style on therapy outcome, there are also contradictory findings and indications that outcomes are better accounted for by general distress.
Studies relating interpersonal style and distress to the quality of the therapeutic alliance found that interpersonal problems in the hostile-dominant domain (i.e., high agency, low communion) prior to treatment predicted a poor working alliance (Connolly Gibbons et al., 2003; Muran et al., 1994; Puschner et al., 2005). Moreover, IIP-C general distress factor has been associated with poor working alliance (Constantino and Smith-Hansen, 2008), whereas interpersonal problems in the friendly-submissive domain (i.e., low agency, high communion) have been associated with better alliance (Constantino and Smith-Hansen, 2008; Muran et al., 1994; Puschner et al., 2005). In contrast, Paivio & Bahr (1998) found that the IIP-C octant scales social avoidance and non-assertiveness, reflecting low agency and high communion, related negatively to working alliance.
Previous research relating the IIP-C to therapy outcome and the therapeutic alliance either categorized patients' reports into interpersonal problem areas based on the predominant interpersonal problem theme, or used IIP-C parameters to predict outcome or therapeutic alliance. The computation of IIP-C parameters is based on octant scores, which all mark a general distress factor that correlates with anxiety and depression symptoms (Horowitz et al., 2000). Accordingly, a clear distinction between interpersonal style and general distress cannot be made, and some have argued that to identify unique effects of interpersonal style on outcome, the general distress factor should be controlled before examining the octant scales (Vittengl et al., 2003).
One possibility for controlling general distress is to obtain orthogonal factor scores from IIP-C scales that converge highly with the underlying IIP-C structure (Vittengl et al., 2003). This can be done by factor analyzing the IIP-C scales, thereby creating independent factor scores representing both interpersonal style and general distress. Identification of orthogonal factor scores simplifies the interpretation of interpersonal distress distinct from interpersonal style, as captured by the communion and affiliation factors. Vittengl et al. (2003), for example, applied principal components analysis to IIP octant scales and found a three-factor structure resembling the three IIP-C dimensions general distress, agency, and communion. Accordingly, to address the clinically important issues of stability and change of interpersonal style and distress, as well as the relations of these constructs with therapy outcome and the therapeutic alliance, factor scores extracted from the IIP-C scales are preferred over octant scales. Yet, to the best of our knowledge, no published study has addressed the relation of patient's initial interpersonal style and distress with therapy outcome and the therapeutic alliance using orthogonal factor scores as predictors.
Therefore, we sought first to replicate previous findings demonstrating a stable IIP-C circumplex structure (Alden et al., 1990; Horowitz et al., 2000; Vittengl et al., 2003). Although the IIP-C circumplex structure has been demonstrated in depressed patients (Vittengl et al., 2003), the number of outpatients in the present study is about four times larger, thus providing a more reliable estimate of the underlying factor structure. We hypothesized that (1) the IIP-C would demonstrate a three-factor structure, consisting of general distress, agency, and communion factors, both pre- and post-CT. Second, we examined interpersonal problems in depressed patients before and after CT in terms of general distress and angular placement in the circumplex, and hypothesized that (2) the interpersonal style of depressed patients would fall between non-assertiveness and social-avoidance. Third, we sought to determine whether the dimensions of communion and agency represent trait-like interpersonal styles, and hypothesized that (3) the distress factor would decrease from pre- to post-CT, whereas interpersonal style would remain stable.
Following this analysis, we assessed the clinical validity of the IIP-C in predicting therapeutic alliance and therapy outcome and hypothesized that (4) the distress and agency factors would relate negatively to improvement of depressive symptoms, whereas the communion factor would relate positively to symptom improvement. Finally, with respect to therapeutic alliance, we hypothesized that (5) distress and agency would relate negatively, and communion positively, to the quality of the therapeutic alliance.
Methods
Sample
The present report is based on patients participating in the acute phase of the `Continuation Phase Cognitive Therapy Relapse Prevention (C-CT-RP) Trial' (ClinicalTrials.gov Identifiers: NCT00118404, NCT00183664 and NCT00218764). A more detailed description of this multi-stage study is available elsewhere (Jarrett and Thase, 2010). Study protocols were approved annually by the Institutional Review Boards at the two treatment sites (The University of Pittsburgh Medical Center and The University of Texas Southwestern Medical Center) and all 523 out-patients enrolled in the study provided written informed consent. The primary inclusion criteria for participation in the study were: a) a principal diagnosis of recurrent MDD according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed; DSM–IV; American Psychiatric Association, 1994) criteria as assessed by the Structured Clinical Interview for DSM-IV (SCID-I; First et al., 1996) a history of inter-episode recovery with or without antecedent dysthymic disorder, c) a score of at least 14 on the 17-item version of the Hamilton Rating Scale for Depressive Symptoms (HRSD-17; Hamilton, 1960) and d) age between 18 and 70 years.
Patients were excluded if they had a poorly controlled medical disorder that might be correlated with depressed mood either directly or through medication intake; had a DSM-IV diagnosis of any psychotic or organic mental disorder; were pregnant or planned to become pregnant within the next year; or had an active alcohol or drug dependence, bipolar disorder or predominant obsessive compulsive disorder, eating disorder or borderline personality disorder. Moreover, patients were excluded if they were unable to complete questionnaires in English, declined protocol requirements or previously had failed to respond to cognitive therapy or fluoxetine.
The average age of the sample entering the acute phase (N = 523) was 42.4 years (SD = 12.1); 67.5% were female; mean education level was 15.1 years (SD = 2.93); 32.5% were married, 30.2% single, 19.9% divorced, 5.7% separated, 2.3% widowed and 9.4% lived together with their partner. Patients' mean age of MDD onset was 21.2 years (SD = 10.8); median length of current episode was 10 months, mean 25.0 months (SD = 45.1). Mean pretreatment HRSD was 20.4 (range = 13–31; Two patients entered the protocol in error, with HRSD-17 scores of 13 at one of the two diagnostic visits; during cognitive therapy one responded and one dropped out.
Procedure
Acute-phase cognitive therapy
The acute-phase protocol consisted of 16 to 20 sessions, each lasting between 50 and 60 min, across 12 to 14 weeks. Therapy was conducted by experienced, research-certified therapists according to the methods of Beck et al. (1979). The first eight sessions occurred twice weekly. Thereafter, patients who experienced at least a 40% reduction of HRSD scores were seen weekly, whereas those with less improvement received four additional weeks of twice weekly sessions; 410 completed at least 14 of 16 protocol sessions (early responders) or 18 of 20 protocol sessions (late responders).
Assessments
To assess changes in symptom severity, therapists completed the HRSD-17 (Hamilton, 1960) weekly during cognitive therapy, as did an independent evaluator at patient exit or end of treatment. Adequate internal consistency (rs = .46 – .97), interrater reliability (rs = .82 – .98) and retest reliability (rs = .81 – .98) have been reported for the HRSD (Bagby et al., 2004). In the current study we found good interrater reliability (ICC = .91) for the HRSD in a multilevel analysis based on 28 patients rated by 4–14 clinicians each.
Inventory of Interpersonal Problems
The Inventory of Interpersonal Problems (IIP; Horowitz et al., 1988) is a 127-item self-report questionnaire assessing interpersonal difficulties with eight subscales (overly nurturant, intrusive, domineering, vindictive, cold, socially avoidant, nonassertive, exploitable). Each item is phrased as a statement and respondents rate their agreement on a Likert scale ranging from 1 (not at all) to 5 (extremely). In this study, responses to the IIP were scored according to the circumplex system, which is based on 64 items assessing interpersonal problems within two dimensions: agency and communion (IIP-C; Alden et al., 1990). Acceptable internal consistency (median α = .81, range .76–.88, N = 800) and test-retest reliability (median r = .73, range .56–.83, N = 60) of the IIP-C have been reported (Horowitz et al., 2000). In the present study internal consistency (coefficient alpha) for the overall score was .92 pre-treatment and .95 post-treatment. The IIP-C subscales were also shown to demonstrate moderate relations with the Beck Depression Inventory (median r = .38, range = .33–.43, N = 495) and Beck Anxiety Inventory (median r = .36, range = .31–.39, N = 495). The IIP-C was collected at the beginning, middle and end of the acute phase.
Working Alliance Inventory
The Working Alliance Inventory (WAI; Horvath and Greenberg, 1989) is a 36-item self-report measure of the therapeutic alliance, with therapist and client versions. Only the client form (WAI-C) was analyzed here because it has been shown to predict outcome better than the therapist version (Horvath and Symonds, 1991). The WAI has three subscales: task agreement, goal agreement and bond development. Each item is rated on a 7-point Likert-type scale. High internal consistency has been reported for the three subscales (.89–.92) and the overall scale (.87–.93; Horvath and Greenberg, 1989). The WAI-C has been shown to converge moderately with the California Psychotherapy Alliance Scales (r = .74; Gaston, 1991) and the Penn Helping Alliance Scales (r = .85; Alexander et al., 1986; Hatcher and Barends, 1996). The WAI-C was obtained at the middle and at the end of the acute phase. In the present study, internal consistency (coefficient alpha) was .94 for the overall WAI-C score at the middle of the acute phase.
Statistical analyses
Unless stated otherwise, SPSS version 18 for Windows was used for statistical analyses. To investigate hypothesis (1), a principal components analysis was conducted with planned rotations (Vittengl et al., 2003). Principal components analysis was used because the circumplex scales of the IIP were also derived using principal components analysis (Alden et al., 1990). Factors were extracted based on observation of the scree plot and rotated orthogonally using the Procrustes procedure in Stata version 10 for Windows. Orthogonal rotations were used in order to match the underlying circumplex structure closely. Hypothesis (2) was investigated by computing the IIP-C structural summary (Gurtman and Balakrishnan, 1998) based on national gender norms (Horowitz et al., 2000). Angular scores were plotted in the circular space. To investigate hypothesis (3), correlations between pre- and post-treatment factor scores were evaluated. Because factor scores have means of zero, IIP-C parameters obtained from the structural summary were compared using paired-sample t-tests. Multilevel Modeling (MLM) was used to predict change in depressive symptom severity over the course of cognitive therapy as a function of pre-treatment interpersonal style and general distress (hypothesis 4). We applied intention-to-treat analysis, in which all available HRSD total scores were included (523 patients; 1–19 HRSD assessments). Time, interpersonal style, distress and the interactions among these factors were modeled as fixed effects and patients' intercepts as a random effect. Hypothesis (5) was investigated using multiple regression analysis. The WAI-C total score at Session 7 was entered as the dependent variable and the distress, agency and communion factors, as well as interactions among them, were entered as predictors. Non-significant interaction terms were removed from the model and the model was re-run.
Results
Cross-sectional associations
First we determined Pearson correlations among the study variables at the baseline assessment. The distress and agency factors related negatively to the WAI-C total score (r = −.13 and r = −.12, respectively) whereas communion related positively to this variable (r = .14). Moreover, Distress correlated negatively with symptom severity at baseline (r = .23), whereas agency and communion were unrelated to baseline symptom severity (r = .04 and r =−.05, respectively).
IIP-C Circumplex Structure and Stability (Hypothesis 1)
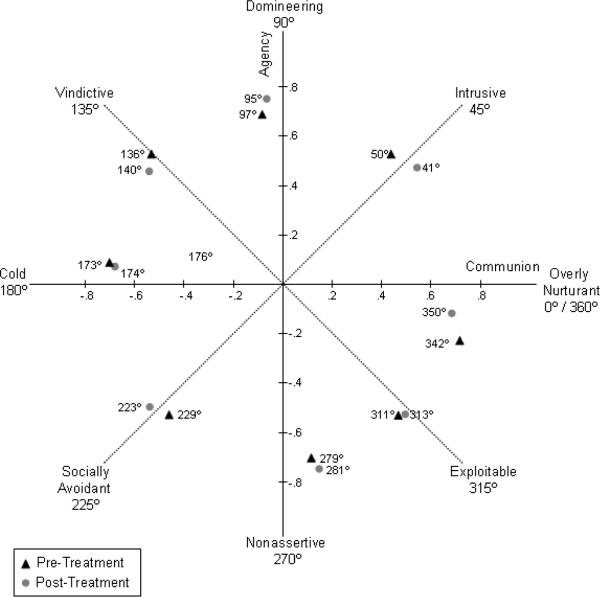
Separate principal components analysis of the pre- and post-treatment scales identified three orthogonal factors at each time point. The rotated factor loadings are summarized in Table 1. To visualize—and guide the interpretation of—the three factors and to demonstrate the circumplex structure of the IIP-C, factor loadings pre- and post-treatment were transformed into circular degree scores and plotted against the hypothetical circumplex structure (see Fig. 1). Although the observed values did not converge perfectly with the expected circumplex structure, visual inspection of Fig. 1 suggests that the circumplex space is adequately covered by the obtained factor loadings. To quantify the convergence between the theoretical circumplex structure and the obtained structure, correlations between the observed and expected angles were computed. The observed factor loadings both pre- and post-treatment correlated highly with the hypothesized circumplex structure (.99), strongly supporting our first hypothesis.
Table 1.
Rotated factor loadings of the Inventory of Interpersonal Problems – Circumplex Version
| Pre-treatment | Post-treatment | |||||
|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | |
| Scale | Distress | Agency | Communion | Distress | Agency | Communion |
| Overly Nurturant | 0.75 | −0.20 | 0.63 | 0.64 | −0.10 | 0.56 |
| Intrusive | 0.71 | 0.57 | 0.47 | 0.76 | 0.52 | 0.59 |
| Domineering | 0.64 | 0.78 | −0.09 | 0.74 | 0.76 | −0.07 |
| Vindictive | 0.75 | 0.47 | −0.48 | 0.68 | 0.44 | −0.52 |
| Cold | 0.73 | 0.08 | −0.66 | 0.66 | 0.07 | −0.65 |
| Socially Avoidant | 0.70 | −0.50 | −0.44 | 0.74 | −0.48 | −0.52 |
| Nonassertive | 0.70 | −0.68 | 0.11 | 0.75 | −0.70 | 0.14 |
| Exploitable | 0.72 | −0.52 | 0.46 | 0.69 | −0.50 | 0.47 |
N = 510 for pre-treatment factor scores and N = 356 for post-treatment factor scores.
Fig. 1.
Angular placement of factor loadings for the Inventory of Interpersonal Problems – Circumplex Version pre- and post-treatment
Note. N = 510; Numbers on the x-axis and y-axis represent factor loadings for factor 1 (distress).
Description of Interpersonal Problems Pre- and Post-Treatment (Hypothesis 2)
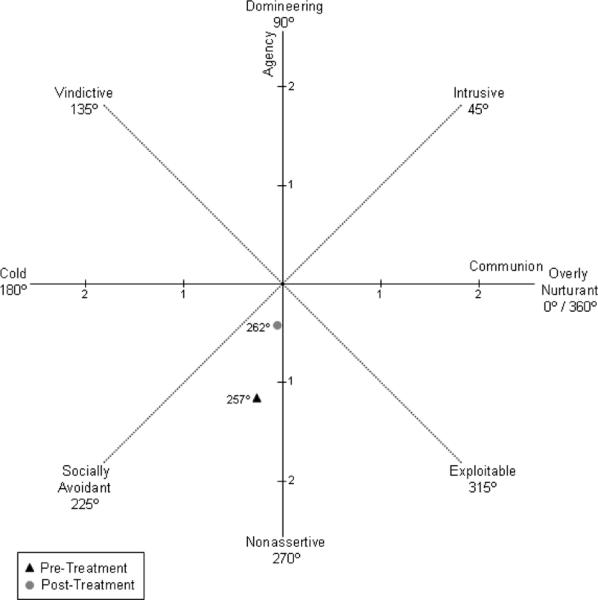
Descriptive and change statistics of the IIP-C octant scales using standardized z-scores are shown in Table 2. Socially avoidant, nonassertive and exploitable problems were somewhat more prominent both pre- and post-treatment, whereas intrusive, domineering and vindictive problems were less prominent both pre- and post-treatment. No octant scale means reached very high levels of distress (T-score > 70) pre- or post-treatment. Patients in our sample improved statistically significantly on all octant scales, with medium effect sizes (Cohen, 1988), such that no octant scale means indicated clinically significant distress (T-score > 60) post-treatment. To describe the sample's mean location in the circumplex space further, we computed the vector direction (angle) that reflected the most prominent form of interpersonal style. The results (see Fig. 2) indicate that the predominant interpersonal style both pre- and post-treatment fell between social avoidance (225°) and non-assertiveness (270°).
Table 2.
Descriptive and change statistics for the Inventory of Interpersonal Problems Circumplex Version pre- and post-treatment
| Pre- treatment | Post- treatment | Paired | ES | ||||
|---|---|---|---|---|---|---|---|
| IIP-C Octant Scale | M (SD) | T score | M (SD) | T score | t-test | DF | (d) |
| Overly Nurturant | 1.20 (1.14) | 64 | 0.42 (1.13) | 56 | 13.2 | 352 | 0.69 |
| Intrusive | 0.67 (1.16) | 57 | 0.11 (1.06) | 51 | 11.1 | 352 | 0.58 |
| Domineering | 0.73 (1.25) | 59 | 0.13 (1.13) | 50 | 10.4 | 352 | 0.50 |
| Vindictive | 0.84 (1.06) | 59 | 0.20 (1.00) | 51 | 12.7 | 352 | 0.62 |
| Cold | 1.14 (1.06) | 61 | 0.42 (1.05) | 54 | 13.7 | 353 | 0.68 |
| Socially Avoidant | 1.62 (1.24) | 67 | 0.77 (1.25) | 58 | 14.1 | 352 | 0.68 |
| Nonassertive | 1.62 (1.20) | 66 | 0.89 (1.17) | 59 | 12.7 | 354 | 0.62 |
| Exploitable | 1.33 (1.12) | 62 | 0.59 (1.16) | 55 | 13.4 | 352 | 0.65 |
N = 353–355 (due to missing values on some subscales). All t-values are statistically significant at p < 0.01 (corrected for multiple testing) and reflect decreased interpersonal problems post-treatment. Effect sizes (ds) were calculated by dividing the mean difference with the pooled standard deviation and may be interpreted as medium (Cohen, 1988).
Fig. 2.
Predominant interpersonal style and mean general distress before and after acute-phase cognitive therapy
Note. N = 356; Numbers on the x-axis and y-axis represent standardized general distress scores, with scores above 1 representing clinical significant distress.
Stability and Change in General Distress and Interpersonal Style (Hypothesis 3)
Table 3 shows Pearson correlations between the pre- and post-treatment factor scores. Correlations between the pre- and post-treatment factors were moderate (r = .54) for distress and somewhat stronger for agency and communion (r = .68 and r = .74, respectively). Moreover, both of the latter were statistically significantly stronger than the former, z = −2.97, p <.01; and z = 4.47, p <.01, respectively. To investigate interpersonal changes further, mean changes of distress, agency and communion from pre-treatment to post-treatment were tested using closely related IIP-C parameters computed earlier. The general distress factor was approximated as the mean z-score of the IIP-C octant scales. The agency and communion factors were approximated by the normative agency and communion scale scores (Horowitz et al., 2000). The general distress, agency and communion factors converged strongly with these approximations both pre-treatment (rs = 1.00, .88, .85, respectively) and post-treatment (rs = 1.00, .82, .82, respectively). Table 4 summarizes the results of the paired samples t-tests between the pre- and post-treatment IIP-C parameters. General distress decreased significantly from pre-treatment (M = 1.15, SD = .75) to post-treatment (M = .45, SD = .81; t(354) = 17.60, p <.01, d = .90), whereas the communion dimension remained stable (t(351) = −0.76 p >.05, d = .03). Scores on the agency dimension also increased significantly from pre-treatment (M = −.47, SD = .79) to post-treatment (M = −.37, SD = .67; t(352) = −3.28, p <.01), but the magnitude of this effect was small (d = .15).
Table 3.
Correlations of the IIP-C factor scores pre- and post-treatment
| Post-treatment | |||
|---|---|---|---|
| Pre-treatment | Distress | Agency | Communion |
| Distress | 54** | −.05 | .00 |
| Agency | .06 | .68** | .11* |
| Communion | .02 | −.09 | 74** |
Correlation is significant at p< 0.05 (two-tailed);
Correlations are significant at p< 0.01 (two-tailed); N = 352.
Table 4.
Mean differences of IIP-C parameters distress, agency and communion as computed from the structural summary pre and post-treatment
| IIP-C Parameter | Pre-treatment Mean (SD) | Post-treatment Mean (SD) | Paired t-test | DF | Cohen's d |
|---|---|---|---|---|---|
| Distress | 1.15 (.75) | 0.45 (.81) | 17.60* | 354 | .90 |
| Agency | −.47 (.79) | −.37 (.67) | −3.28* | 352 | .14 |
| Communion | −.07 (.65) | −.05 (.61) | −.76 | 351 | .03 |
Mean difference is significant at p < 0.01; N = 352–355.
Relations of Interpersonal Style and General Distress with Change in Depressive Symptoms (Hypothesis 4)
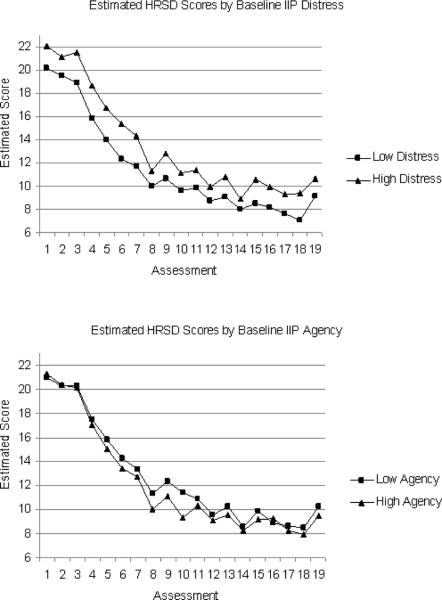
We used MLM to predict change in depressive symptoms over the course of cognitive therapy as a function of time, pre-treatment interpersonal style and general distress (Table 5). There were significant main effects for time, F(18, 6037.76) = 461.12, p <.01 and distress, F(1, 521.12) = 24.82, p <.01. To determine the relative importance of the effect of distress on symptom levels, we calculated standardized beta weights by standardizing all continuous variables before entering them into the model. The relation between general distress and symptom levels was relatively small (β = .10). There was a significant interaction between distress and time, F(18, 6039.16) = 2.06, p <.01 and a marginally significant interaction between agency and time, F(18, 6038.06) = 1.56, p = .06. To interpret these interaction terms, we plotted HRSD total scores over the course of cognitive therapy separately for the low- and high-distress groups and for the low- and high-agency groups (Fig. 3), defined as one SD below and above the respective IIP-C factor-score mean. Patients with higher baseline distress scores had significantly higher mean symptom scores over the course of treatment. Patients with high baseline agency had lower symptom scores in the middle of cognitive therapy and slightly lower symptom scores at the end of cognitive therapy.
Table 5.
General distress, agency and communion as predictors of change in depressive symptom severity (HRSD) over the course of cognitive therapy
| Parameter | Numerator DF | Denominator DF | F | p-value (F) |
|---|---|---|---|---|
| Intercept | 1 | 518.03 | 4003.54 | <.01 |
| Time | 18 | 6037.76 | 461.12 | <.01 |
| Distress | 1 | 521.12 | 24.82 | <.01 |
| Agency | 1 | 519.23 | 2.19 | >.05 |
| Communion | 1 | 513.81 | 0.30 | >.05 |
| Distress*Time | 18 | 6039.16 | 2.06 | <.01 |
| Agency*Time | 18 | 6038.06 | 1.56 | >.05 |
| Communion*Time | 18 | 6036.08 | 0.58 | >.05 |
Fig. 3.
Change in depressive symptom severity over the course of CT predicted by IIP general distress and IIP agency
Note. Upper graph shows significant interaction between time moment and distress for the low and high distress group. Lower graph shows marginally significant interaction between time and agency for the low and high agency groups.
Relations of Interpersonal Style and General Distress with Therapeutic Alliance (Hypothesis 5)
The results of the multiple regression analysis are summarized in Table 6. High general distress and high agency were negatively related to WAI-C total scores (β = −0.13, t(380) = −2.64, p < 0.01 and β = −0.12, t(380) = −2.46, p < 0.05, respectively), whereas high communion was positively related to WAI-C total scores (β = .15, t(380) = 2.91, p < 0.01). This pattern of effects was found for all WAI-C subscales except between the general distress factor and task subscale. Whereas all variables in the model predicted therapeutic alliance in the expected direction, the total variance in WAI-C scores explained by these three factors was small (R2 = .053). To determine whether the relations between interpersonal styles and distress with the therapeutic alliance remain once depressive symptom severity is controlled for, we added the HRSD total score at baseline to the regression model. All predictors remained significant and adding the HRSD baseline score did not improve the overall model (Δ R2 = 0.0). Moreover, HRSD at baseline was unrelated to the WAI-C total score (β = −0.03, t(380) = −0.54, p = .59).
Table 6.
General distress, agency, and communion as predictors of mid-treatment therapeutic alliance
| Factor | Total WAI-C β (SE) | Task β (SE) | Bond β (SE) | Goal β (SE) |
|---|---|---|---|---|
| General Distress | −0.13** (0.03) | −0.09 (0.04) | −0.14** (0.04) | −0.13* (0.04) |
| Agency | −0.12* (0.03) | −0.12* (0.04) | −0.12* (0.04) | −0.10* (0.04) |
| Communion | 0.15** (0.03) | 0.14** (0.04) | 0.14** (0.04) | 0.12* (0.04) |
p < 0.05;
p < 0.01; N= 384.
Discussion
We investigated the structure and stability of the IIP-C (Alden et al., 1990) over the course of a 16-to-20 session protocol of cognitive therapy in a large group of adult outpatients with recurrent MDD. Consistent with earlier studies, applying principal components analysis to IIP-C subscales (Holtforth et al., 2006; Horowitz et al., 1988; Vittengl et al., 2003), we found the hypothesized factor structure, consisting of general distress, agency and communion factors both before and after cognitive therapy. Moreover, when the agency and communion factor loadings were arranged in a circular space, they closely matched the corresponding circumplex octant scales' theoretical angular placements. This finding further supports the robustness of the IIP-C as a measure of interpersonal functioning.
In terms of angular placement in the circumplex, we found that the sample's predominant interpersonal style fell between social avoidance and non-assertiveness both before and after cognitive therapy. This is consistent with previous research investigating interpersonal profiles in patients with depression (Barrett and Barber, 2007). Moreover, although patients experienced significant distress in most areas of interpersonal functioning, on average, none of the eight interpersonal areas reached very high levels of interpersonal distress (i.e., means > 2 SD above the normative sample) either before or after cognitive therapy. However, 73% of individual patients reported very high levels of distress in at least one octant scale. Thus, patients with depression in this sample presented with a wide range of interpersonal problems with high levels of distress.
Following the description of interpersonal profiles, we investigated which aspects of interpersonal problems changed over the course of cognitive therapy. Consistent with previous research reporting improvement on most (Crits-Christoph et al., 2005) or all (Holtforth et al., 2006; Huber et al., 2007; Vittengl et al., 2003) IIP-C subscales, mean scores on all IIP-C subscales were reduced to non-clinical levels following therapy. Moreover, cross-correlations between pre- and post-treatment factor scores and mean-score comparisons of the corresponding IIP-C parameters revealed that this improvement was due largely to reduced distress, whereas interpersonal style remained largely stable, as hypothesized. Contrary to our expectations, agency also decreased at post-treatment, although the effect size was small and not likely to be clinically meaningful. As such, our findings are largely consistent with previous findings (Crits-Christoph et al., 2005; Vittengl et al., 2003), suggesting that the IIP-C captures both state-like (general distress) and trait-like (interpersonal style) constructs.
Our findings differ from those of Holtforth et al. (2006) who reported change on all IIP-C dimensions after psychosocial treatment for depression. There are at least two possible explanations for the divergent findings in our study. First, patients in the Holtforth et al. (2006) study received a eclectic psychotherapy, with therapists free to draw upon process-experiential and interpersonal interventions in addition to cognitive-behavioral strategies. One prior study of 66 patients with MDD found that process-experiential therapy may be more effective in reducing interpersonal problems than cognitive therapy (Watson et al., 2003), but this hypothesis requires further testing.
Perhaps more importantly, patients in the Holtforth et al. study received an average of 29 sessions (range = 5–127) of eclectic psychotherapy, whereas outpatients in this study received a maximum of 20 cognitive therapy sessions. It has been shown previously that the number of therapy sessions is related, in a dose-response fashion, to improvement in interpersonal problems in patients with depression (Barkham et al., 2002).
The present study also addressed the predictive validity of the IIP-C for the therapeutic process and outcome. We tested interpersonal style and distress factor scores as predictors of change in depressive symptom severity over the course of cognitive therapy and hypothesized that the distress and agency factors would be related negatively to improvement of depressive symptoms, whereas the communion factor would be related positively to symptom improvement. In general, our findings that high levels of distress related negatively to symptom improvement whereas high agency levels related positively to symptom improvement are contrary to what we hypothesized based on theoretical grounds (Tracey, 1993) and prior research (Alden and Capreol, 1993; Gurtman, 1996; Muran et al., 1994). One reason for these divergent findings may be that previous studies categorized patients into quadrants of interpersonal problems based on their angular displacement score (Gurtman, 1996). Classification of patients into quadrants may oversimplify the diversity of the interpersonal problems experienced by patients with recurrent depression. Moreover, such a classification does not control for the general distress factor that should be detached from interpersonal style before investigating effects of interpersonal style on outcome. More valid results may be obtained by using dimensional scores, such as factor scores, that differentiate between interpersonal style and general distress.
Finally, we found support for our hypothesis that high scores on the communion factor at baseline would predict high alliance, whereas high scores on the agency and general distress factors would predict poor alliance. This finding is consistent with the idea that a friendly-submissive interpersonal style is complementary to the more active and directive style of cognitive therapists (Kiesler, 1983; Tracey, 1993). Although interpersonal style and distress at baseline consistently predicted therapeutic alliance in the expected direction, these effects were very small. In this context, it should be noted that the mean patients' alliance rating was very high, with very little variability (M = 6.1, SD = 0.67), probably reflecting a ceiling effect. Accordingly, interpersonal style and distress may explain a greater amount of total variance if there were more variation in the therapist-patient alliance.
Limitations
The study results should be interpreted in light of several limitations. First, given the study's inclusion/exclusion criteria, all patients had recurrent MDD. It is therefore uncertain whether or not these findings would generalize to the broader population of patients with other psychiatric disorders. Second, therapists' interpersonal style was not assessed. Because patients with an interpersonal style that is complementary to their therapists' may develop the best alliance, therapists' interpersonal style also should be accounted for rather than assuming that all therapists are friendly-dominant. Finally, the results of all analyses were based on a self-report measure of interpersonal problems. It has been shown that self-reported interpersonal problems on the IIP-C do not necessarily converge with observer-rated interpersonal problems (Leising et al., 2007).
Implications
Despite these limitations, the present study has important implications for clinical care and future research. First, the finding that the IIP-C showed a stable circumplex structure before and after cognitive therapy provides further evidence that the IIP-C can be used as a comprehensive measure of interpersonal constructs before and after treatment. Second, future research that uses the IIP-C should differentiate between interpersonal style and general distress, rather than treat interpersonal problems as a unidimensional construct. In the present study, interpersonal distress, but not interpersonal style, decreased during cognitive therapy. According to the cognitive theory of depression, dysfunctional thoughts are at the core of depression. Dysfunctional thoughts often contain interpersonal themes, such as the belief that one is inferior or will be rejected in interpersonal situations. Cognitive theory assumes that broad behavioral change across domains is possible, including reduction in interpersonal problem levels during cognitive therapy, as shown in the current analyses. At the same time, cognitive theory does not assume that the person's basic personality will change during short-term therapy. Therefore, our finding that interpersonal style remained stable during cognitive therapy for depression (i.e., although patients became less distressed about their interpersonal relations, their basic level of agency and communion did not change) is largely in line with what might be expected based on the cognitive theory of depression. Future research should investigate the stability of interpersonal distress and interpersonal style in other forms of psychotherapy that explicitly target personality or interpersonal functioning. Third, in the present study we determined the predominant interpersonal style of patients with MDD and related interpersonal style and distress to therapy outcome and the quality of the therapeutic alliance. Recent research in patients with anxiety disorders suggests that interpersonal subtypes exist within diagnostic homogeneous groups, and that these subtypes relate differently to treatment outcome (Cain et al., 2010; Salzer et al., 2011). Based on these studies, a next step might be to attempt to identify interpersonal subtypes in MDD. However, recent data in the personality trait domain indicates that subtyping is strongly sample-based and therefore should only be attempted on population representative samples (Eaton et al., 2010). Thus, identifying possible subtypes is an issue for future research. Whereas the present study further supported the use of the IIP-C as a comprehensive circumplex measure of interpersonal functioning, more research is needed investigating the predictive validity of the interpersonal style and distress components of the IIP-C in patients with different types of psychopathology and in different treatment settings.
Acknowledgements
We are grateful to our research teams and our colleagues at Western Psychiatric Institute and Clinic at The University of Pittsburgh (where Dr. Thase was located during patient accrual), and The University of Texas Southwestern Medical Center at Dallas (Dr. Jarrett's current affiliation). We appreciate the assistance of Joanne Sanders, M.S., and Abu Minhajuddin, Ph.D., who helped with data management.
We appreciate the support of the NIMH, particularly that of our Program Officer, Jane Pearson, Ph.D. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health. We also appreciate the careful review by members of the trial's Data Safety and Monitoring Board.
Role of the funding source This report was supported by Grants Number K24 MH001571, R01 MH58397, R01-MH-069619 (to Robin B. Jarrett, Ph.D.) and R01 MH58356 and R01 MH69618 (to Michael E. Thase, M.D.) from the National Institute of Mental Health (NIMH). The funding source had no involvement in study design, in the analysis or interpretation of the data, in the writing of the report, or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributions Drs. Jarrett and Thase are the principal investigators of the study and the senior authors of the manuscript. Dr. Vittengl and Renner, MSc. carried out the data analyses. All of the authors contributed to drafting/revising the manuscript and approved the final manuscript.
Conflict of Interest During the past two years Dr. Thase has consulted with, served on advisory boards for, or received honoraria for talks from: Aldolor, Alkermes, AstraZeneca, Bristol-Myers Squibb Company, Eli Lilly and Company, Forest Laboratories, GlaxoSmithKline, Janssen Pharmaceutica, Lundbeck, MedAvante, Merck, Neuronetics, Inc., Novartis, Otsuka, Pamlab, Pfizer Pharmaceuticals, PharmaNeuroBoost, Rexahn, Shire US Inc., Supernus Pharmaceuticals, Takeda, and Transcept Pharmaceuticals and he has received grant support from Eli Lilly and Company, Forest Laboratories, GlaxoSmithKline, Otsuka, Pamlab, and Rexahn, in addition to funding from the NIMH and the Agency for Healthcare Research and Quality. He has equity holdings for MedAvante, Inc. and has received royalties from American Psychiatric Publishing, Inc. (APPI), Guilford Publications, Herald House, and W.W. Norton & Company, Inc. Two books currently promoted by the APPI specifically pertain to cognitive therapy. Dr. Thase also discloses that his spouse is an employee of Embryon, Inc. (formerly Cardinal Health and Advogent), which does business with several pharmaceutical companies that market medications used to treat depression.
Dr. Jarrett's medical center receives the fees from the cognitive therapy she provides to patients. Dr. Jarrett is a paid consultant to the NIMH.
The other authors declare no conflict of interest.
In the circumplex literature, the x-axis of the circumplex usually was referred to as love, warmth or nurturance and the y-axis as dominance, power, or status. More recently, however, the superordinate terms communion and agency have been used for the x-axis and y-axis, respectively.
References
- Alden LE, Capreol MJ. Avoidant personality disorder: Interpersonal problems as predictors of treatment response. Behavior Therapy. 1993;24:357–376. [Google Scholar]
- Alden LE, Wiggins JS, Pincus AL. Construction of Circumplex Scales for the Inventory of Interpersonal Problems. J. Pers. Assess. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- Alexander LB, Luborsky L, Greenberg LS, Pinsof WM. The psychotherapeutic process: A research handbook. Guilford Press; New York, NY US: 1986. The Penn Helping Alliance Scales; pp. 325–366. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical manual of mental disorders. 4th ed. American Psychiatric Press; Washington, D.C.: 1994. [Google Scholar]
- Bagby RM, Ryder AG, Schuller DR, Marshall MB. The Hamilton Depression Rating Scale: Has the Gold Standard Become a Lead Weight? Am. J. Psychiatry. 2004;161:2163–2177. doi: 10.1176/appi.ajp.161.12.2163. [DOI] [PubMed] [Google Scholar]
- Barkham M, Rees A, Stiles WB, Hardy GE, Shapiro DA. Dose-effect relations for psychotherapy of mild depression: A Quasi-experimental comparison of effects of 2, 8, and 16 sessions. Psychotherapy Research. 2002;12:463–474. [Google Scholar]
- Barrett MS, Barber JP. Interpersonal profiles in major depressive disorder. J. Clin. Psychol. 2007;63:247–266. doi: 10.1002/jclp.20346. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford; New York: 1979. [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J. Consult. Clin. Psychol. 2002;70:288–298. [PubMed] [Google Scholar]
- Cain NM, Pincus AL, Grosse Holtforth M. Interpersonal Subtypes in Social Phobia: Diagnostic and Treatment Implications. J. Pers. Assess. 2010;92:514–527. doi: 10.1080/00223891.2010.513704. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Erlbaum, Hillsdale, NJ; 1988. [Google Scholar]
- Connolly Gibbons MB, Crits-Christoph P, de la Cruz C, Barber JP, Siqueland L, Gladis M. Pretreatment expectations, interpersonal functioning, and symptoms in the prediction of the therapeutic alliance across supportive-expressive psychotherapy and cognitive therapy. Psychotherapy Research. 2003;13:59–76. doi: 10.1093/ptr/kpg007. [DOI] [PubMed] [Google Scholar]
- Constantino M, Smith-Hansen L. Patient interpersonal factors and the therapeutic alliance in two treatments for bulimia nervosa. Psychotherapy Research. 2008;18:683–698. doi: 10.1080/10503300802183702. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Narducci J, Schamberger M, Gallop R. Interpersonal Problems and the Outcome of Interpersonally Oriented Psychodynamic Treatment of GAD. Psychotherapy: Theory, Research, Practice, Training. 2005;42:211–224. [Google Scholar]
- Eaton NR, Krueger RF, South SC, Simms LJ, Clark LA. Contrasting prototypes and dimensions in the classification of personality pathology: evidence that dimensions, but not prototypes, are robust. Psychol. Med. 2010;41:1151–1163. doi: 10.1017/S0033291710001650. [DOI] [PubMed] [Google Scholar]
- Filak J, Abeles N, Norquist S. Clients' pretherapy interpersonal attitudes and psychotherapy outcome. Professional Psychology: Research and Practice. 1986;17:217–222. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute, Biometrics Research Department; New York: 1996. [Google Scholar]
- Gaston L. Reliability and Criterion-Related Validity of the California Psychotherapy Alliance Scales-Patient Version. Psychological Assessment. 1991;3:68–74. [Google Scholar]
- Gurtman MB. Interpersonal problems and the psychotherapy context: The construct validity of the Inventory of Interpersonal Problems. Psychological Assessment. 1996;8:241–255. [Google Scholar]
- Gurtman MB, Balakrishnan JD. Circular measurement redux: The analysis and interpretation of interpersonal circle profiles. Clinical Psychology Science and Practice. 1998;5 [Google Scholar]
- Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, Barends AW. Patients' View of the Alliance in Psychotherapy: Exploratory Factor Analysis of Three Alliance Measures. J. Consult. Clin. Psychol. 1996;64:1326–1336. doi: 10.1037//0022-006x.64.6.1326. [DOI] [PubMed] [Google Scholar]
- Holtforth MG, Lutz W, Grawe K. Structure and change of the IIP-D pre-and postpsychotherapy: A replication using a Swiss clinical sample. European Journal of Psychological Assessment. 2006;22:98–103. [Google Scholar]
- Horowitz LM, Alden LE, Wiggins JS, Pincus AL. Manual for the Inventory of Interpersonal Problems. Harcourt Assessment The Psychological Corporation; Oxford, UK: 2000. [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. J. Consult. Clin. Psychol. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Bartholomew K. Interpersonal problems, attachment styles, and outcome in brief dynamic psychotherapy. J. Consult. Clin. Psychol. 1993;61:549–560. doi: 10.1037//0022-006x.61.4.549. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Wilson KR, Turan B, Zolotsev P, Constantino MJ, Henderson L. How Interpersonal Motives Clarify the Meaning of Interpersonal Behavior: A Revised Circumplex Model. Personality & Social Psychology Review. 2006;10:67–86. doi: 10.1207/s15327957pspr1001_4. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: A meta-analysis. Journal of Counseling Psychology. 1991;38:139–149. [Google Scholar]
- Huber D, Henrich G, Klug G. The Inventory of Interpersonal Problems (IIP): Sensitivity to change. Psychotherapy Research. 2007;17:474–481. [Google Scholar]
- Jarrett RB, Thase ME. Comparative efficacy and durability of continuation phase cognitive therapy for preventing recurrent depression: Design of a double-blinded, fluoxetine- and pill placebo-controlled, randomized trial with 2-year follow-up. Contemporary Clinical Trials. 2010;31:355–377. doi: 10.1016/j.cct.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiesler DJ. The 1982 Interpersonal Circle: A taxonomy for complementarity in human transactions. Psychol. Rev. 1983;90:185–214. [Google Scholar]
- Kiesler DJ, Watkins LM. Interpersonal complementarity and the therapeutic alliance: A study of relationship in psychotherapy. Psychotherapy: Theory, Research, Practice, Training. 1989;26:183–194. [Google Scholar]
- Leising D, Rehbein D, Sporberg D. Validity of the Inventory of Interpersonal Problems (IIP-64) for predicting assertiveness in role-play situations. J. Pers. Assess. 2007;89:116–125. doi: 10.1080/00223890701468428. [DOI] [PubMed] [Google Scholar]
- Muran JC, Segal ZV, Samstag LW, Crawford CE. Patient pretreatment interpersonal problems and therapeutic alliance in short-term cognitive therapy. J. Consult. Clin. Psychol. 1994;62:185–190. doi: 10.1037//0022-006x.62.1.185. [DOI] [PubMed] [Google Scholar]
- Paivio SC, Bahr LM. Interpersonal problems, working alliance, and outcome in short-term experiential therapy. Psychotherapy Research. 1998;8:392–407. [Google Scholar]
- Puschner B, Bauer S, Horowitz LM, Kordy H. The Relationship Between Interpersonal Problems and the Helping Alliance. J. Clin. Psychol. 2005;61:415–429. doi: 10.1002/jclp.20050. [DOI] [PubMed] [Google Scholar]
- Ruiz MA, Pincus AL, Borkovec TD, Echemendia RJ, Castonguay LG, Ragusea SA. Validity of the Inventory of Interpersonal Problems for Predicting Treatment Outcome: An Investigation With The Pennsylvania Practice Research Network. J. Pers. Assess. 2004;83:213–222. doi: 10.1207/s15327752jpa8303_05. [DOI] [PubMed] [Google Scholar]
- Salzer S, Pincus AL, Winkelbach C, Leichsenring F, Leibing E. Interpersonal subtypes and change of interpersonal problems in the treatment of patients with generalized anxiety disorder: A pilot study. Psychotherapy. 2011;48:304–310. doi: 10.1037/a0022013. [DOI] [PubMed] [Google Scholar]
- Schauenburg H, Kuda M, Sammet I, Strack M. The influence of interpersonal problems and symptom severity on the duration and outcome of short-term psychodynamic psychotherapy. Psychotherapy Research. 2000;10:133–146. doi: 10.1080/713663670. [DOI] [PubMed] [Google Scholar]
- Tracey TJ. An interpersonal stage model of the therapeutic process. Journal of Counseling Psychology. 1993;40:396–409. [Google Scholar]
- Vittengl JR, Clark LA, Jarrett RB. Interpersonal problems, personality pathology, and social adjustment after cognitive therapy for depression. Psychological Assessment. 2003;15:29–40. doi: 10.1037/1040-3590.15.1.29. [DOI] [PubMed] [Google Scholar]
- Watson JC, Gordon LB, Stermac L, Kalogerakos F, Steckley P. Comparing the effectiveness of process-experiential with cognitive-behavioral psychotherapy in the treatment of depression. J. Consult. Clin. Psychol. 2003;71:773–781. doi: 10.1037/0022-006x.71.4.773. [DOI] [PubMed] [Google Scholar]
- Wiggins JS. Circumplex models of interpersonal behavior in clinical psychology. In: Kendall PC, Butcher JN, editors. Handbook of research methods in clinical psychology. Wiley; New York: 1982. pp. 183–221. [Google Scholar]