Abstract
With the growth of mobile health in recent years, learning through the use of mobile devices (mobile learning [mLearning]) has gained recognition as a potential method for increasing healthcare providers' access to medical information and resources in resource-limited settings. In partnership with the University of Botswana School of Medicine (SOM), we have been exploring the role of smartphone-based mLearning with resident (physicians in specialty training) education. The SOM, which admitted its first class of medical students and residents in 2009, is committed to providing high-level on-site educational resources for resident physicians, even when practicing in remote locations. Seven residents were trained to use an Android-based myTouch 3G smartphone equipped with data-enabled subscriber identity module (SIM) cards and built-in camera. Phones contained locally loaded point-of-care and drug information applications, a telemedicine application that allows for the submission of cases to local mentors, and e-mail/Web access. Surveys were administered at 4 weeks and 8 weeks following distribution of phones. We found that smartphones loaded with point-of-care tools are effectively utilized by resident physicians in resource-limited settings, both for accessing point-of-care medical information at the bedside and engaging in self-directed learning at home.
Introduction
In parallel with the growth of mobile health (mHealth), mobile learning (mLearning) has emerged as a tool that leverages mobile technology to increase healthcare providers' access to medical information and resources, especially in resource-limited settings.1–5 Across Africa, information needs of healthcare providers are not being met, and this has been associated with suboptimal delivery of healthcare to a substantial portion of the world's population.6 Mobile devices and wireless networks allow resource-limited countries to implement information and communication technology systems by circumventing low bandwidth and substandard computer resources.3,7–9
Botswana has a national public health system made up of health posts, clinics, primary hospitals, district hospitals, and referral hospitals. There are approximately 40 physicians per 100,000 people in the country,10 and access to physicians, especially specialists, remains a challenge outside the major city centers. The health system is burdened by the second highest prevalence of human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) in the world, estimated at 24.6% of adults aged 15–49.11 mHealth and mLearning efforts in Botswana benefit from a significant mobile device ownership12 and an existing network of multiple competing telecommunication companies.
In response to the HIV/AIDS epidemic, the Government of Botswana, the University of Botswana, and the University of Pennsylvania (UPenn) formed the Botswana-UPenn Partnership to build capacity in Botswana. Since 2001, UPenn has been helping to train healthcare providers in the prevention and treatment of HIV/AIDS, to develop postgraduate training programs at the University of Botswana, to build joint research programs, and to offer global health experiences to UPenn trainees.
In 2009, the University of Botswana School of Medicine (SOM) admitted its first class of students and residents, physicians in specialty training. Residents rotate throughout the health system, and access to information technology resources at all training sites is crucial. In the capital city of Gaborone, however, access at the referral hospital is limited by poor Internet connection and availability of functioning computers. In remote areas, gaining access is even more challenging, and specialist mentors are not readily available.
Incentivizing physicians to continue practicing in Botswana and in remote clinics is the major goal of the SOM. A smartphone-based mLearning tool was implemented to help residents train and care for patients by providing access to medical resources and remote mentoring. We will discuss our experiences to date with this ongoing program.
Methods
Seven residents in Medicine and Pediatrics residency programs, based at a public referral hospital in Gaborone, were provided with myTouch 3G smartphones, equipped with Android-based medical information applications, built-in camera, and data-enabled subscriber identity module (SIM) card (Fig. 1). The phones contained locally loaded point-of-care applications, including UCentral, Skyscape, and ePocrates Rx. UCentral and Skyscape are medical software that each contain multiple applications, including drug references (e.g., A-Z Drug Facts, RxDrugs) and clinical decision-making resources (e.g., 5-Minute Clinical Consult, DynaMed). ePocrates Rx is a stand-alone drug reference application. The phones also had e-mail/Web access and a telemedicine application that allows for the submission of cases to local mentors. Calling and texting capabilities were not activated.
Fig. 1.
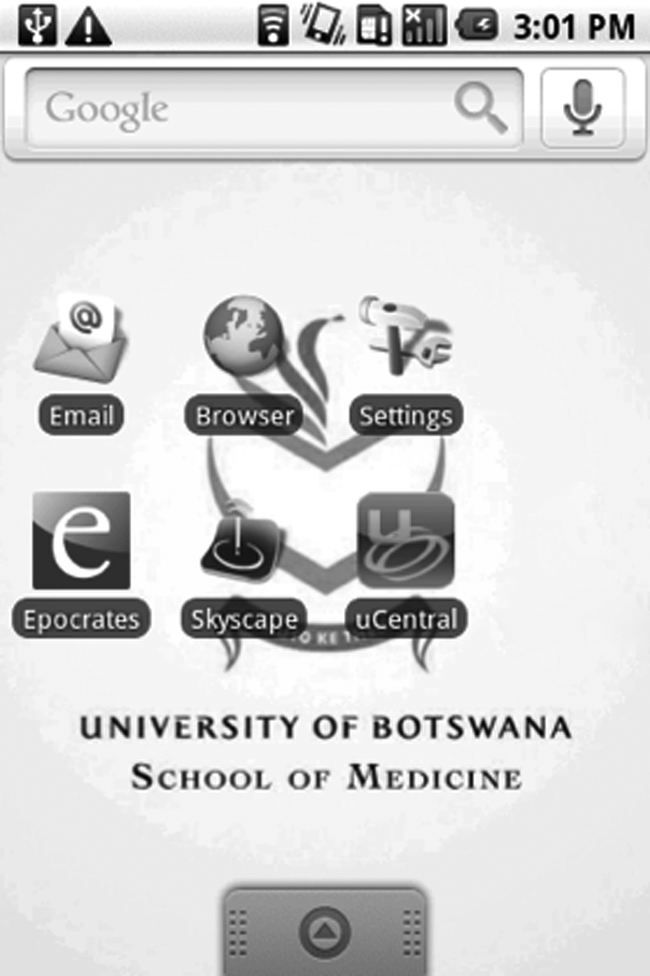
Screenshot of the phone's home page.
Study coordinators conducted an initial training session, which covered use of the smartphone and its applications. Prior to phone distribution, residents completed an initial written survey with multiple-choice questions, which assessed familiarity with smartphone technology. At 4 and 8 weeks following phone distribution, residents completed a follow-up written survey with multiple-choice and free response questions, which assessed comfort level, frequency of use, and applications used. One resident did not complete follow-up surveys due to scheduling conflicts.
Results
Between follow-up at 4 and 8 weeks, residents increased their usage of the phone, which they primarily attributed to increased opportunity for use and growing familiarity. Residents reported gaining familiarity through the initial training session, help from other residents, and spending time alone with the phone. While six out of seven residents initially surveyed were unfamiliar with smartphones, these six felt comfortable with the phone after 8 weeks of use.
Residents listed use of the following medical information applications: five out of six used UCentral, of which four used 5-Minute Clinical Consult and one used A-Z Drug Facts; two out of six used Skyscape; three out of six used ePocrates Rx. Five out of six residents used the phone not only for access to point-of-care applications in the medical setting, but also for supplementary reading outside of the hospital. When asked to provide suggestions for other types of information, four out of six residents requested increased access to journals.
Discussion
We have found that smartphones loaded with point-of-care tools are effectively utilized by resident physicians in resource-limited settings, both for accessing point-of-care medical information at the bedside and for self-directed learning at home. As reported elsewhere, we found that users required only a short period of time to learn how to use the smartphone and search for information.2
Ongoing plans include scaling up the use of the phone to remote clinic sites and residents in other specialties, such as Family Medicine and Emergency Medicine. We are currently implementing the telemedicine case consultation program. As data collection efforts increase, mentors will be able to identify medical topics that residents find challenging by evaluating the types of cases being submitted for consultation.
In 2000, citizens of developing countries owned one-fourth of the world's 700 million mobile devices. By the beginning of 2009, their share had grown to three-quarters of the four billion total mobile devices in the world, and this exponential growth is expected to continue in the coming years.13 Competition among different mobile phone companies has driven improvement in the number and quality of smartphone applications available, as well as enhancement of phone features. By 2015, an estimated 500 million people will access mHealth applications on smartphones.14
Use of mobile devices to access information leverages an existing, robust network of mobile connectivity. As smartphones become more affordable worldwide, mLearning will likely play an integral role in providing education to people in remote and resource-limited areas of the world.1,15 Within medicine, mLearning is poised to be an invaluable resource for addressing the medical information needs of healthcare providers in resource-limited settings.
Acknowledgments
This work has been made possible by the Orange Foundation in Botswana, National Library of Medicine in the United States, EBSCO Publishing, and Unbound Medicine, Inc., as well as support from the University of Botswana School of Medicine.
Disclosure Statement
No competing financial interests exist.
References
- 1.Chang LW. Mwanika A. Kaye D, et al. Information and communication technology and community-based health sciences training in Uganda: Perceptions and experiences of educators and students. Inform Health Soc Care. 2011 doi: 10.3109/17538157.2010.542530. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Zolfo M. Iglesias D. Kiyan C, et al. Mobile learning for HIV/AIDS healthcare worker training in resource-limited settings. AIDS Res Ther. 2010;7:35. doi: 10.1186/1742-6405-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwankam SY. What e-Health can offer. Bull World Health Organ. 2004;82:800–802. [PMC free article] [PubMed] [Google Scholar]
- 4.Lester R. Karanja S. Mobile phones: Exceptional tools for HIV/AIDS, health, and crisis management. Lancet Infect Dis. 2008;8:738–739. doi: 10.1016/S1473-3099(08)70265-2. [DOI] [PubMed] [Google Scholar]
- 5.Prgomet M. Georgiou A. Westbrook JI. The impact of mobile handheld technology on hospital physicians' work practices and patient care: A systematic review. J Am Med Inform Assoc. 2009;16:792–801. doi: 10.1197/jamia.M3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pakenham-Walsh N. Bukachi F. Information needs of health care workers in developing countries: A literature review with a focus on Africa. Hum Resour Health. 2009;7:30. doi: 10.1186/1478-4491-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beveridge M. Howard A. Burton K. Holder W. The Ptolemy project: A scalable model for delivering health information in Africa. BMJ. 2003;327:790–793. doi: 10.1136/bmj.327.7418.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hadley GP. Mars M. Postgraduate medical education in paediatric surgery: Videoconferencing—a possible solution for Africa? Pediatr Surg Int. 2008;24:223–226. doi: 10.1007/s00383-007-2085-5. [DOI] [PubMed] [Google Scholar]
- 9.Alexander L. Igumbor EU. Sanders D. Building capacity without disrupting health services: Public health education for Africa through distance learning. Hum Resour Health. 2009;7:28. doi: 10.1186/1478-4491-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Botswana Country Profile. www.afro.who.int/en/countries.html. [Mar 1;2011 ]. www.afro.who.int/en/countries.html
- 11.Joint United Nations Programme on HIV/AIDS. UNAIDS Report on the global AIDS epidemic. 2010. www.unaids.org/globalreport/Global_report.htm. [Feb 3;2011 ]. www.unaids.org/globalreport/Global_report.htm
- 12.Central Intelligence Agency. The World Factbook 2010. Botswana Communications Profile. www.cia.gov/library/publications/the-world-factbook/geos/bc.html. [Mar 1;2011 ]. www.cia.gov/library/publications/the-world-factbook/geos/bc.html
- 13.United Nations. Human Development Report 2010. 2010. http://hdr.undp.org/en/reports/ [Nov 14;2010 ]. http://hdr.undp.org/en/reports/
- 14.research2guidance. Global Mobile Health Market Report 2010–2015. www.research2guidance.com. [Nov;2010 ]. www.research2guidance.com
- 15.Motlik S. Mobile learning in developing nations. Int Rev Res Open Dist Learn. 2008;9:1–7. [Google Scholar]


