Abstract
The use of telehealth technologies to overcome the geographic distances in the delivery of hospice care has been termed telehospice. Although telehospice research has been conducted over the last 10 years, little is known about the comprehensive findings within the field. The purpose of this systematic article was to focus on available research and answer the question, What is the state of the evidence related to telehospice services? The article was limited to studies that had been published in the English language and indexed between January 1, 2000 and March 23, 2010. Indexed databases included PubMed and PsycINFO and contained specified key words. Only research published in peer review journals and reporting empirical data, rather than opinion or editorials, were included. A two-part scoring framework was modified and applied to assess the methodological rigor and pertinence of each study. Scoring criteria allowed the evaluation of both quantitative and qualitative methodologies. Twenty-six studies were identified with the search strategy. Although limited in number and in strength, studies have evaluated the use of a variety of technologies, attitudes toward use by providers and consumers, clinical outcomes, barriers, readiness, and cost. A small evidence base for telehospice has emerged over the last 10 years. Although the evidence is of medium strength, its pertinence is strong. The evidence base could be strengthened with randomized trials and additional clinical-outcome-focused research in larger randomized samples and in qualitative studies with better-described samples.
Key words: telehealth, technology, telemedicine, home health monitoring
Introduction
Hospice care is delivered to more than one million terminally ill patients and families each year in the United States. The National Hospice and Palliative Care Organization estimates that >38% of all deaths in the United States now receive hospice services.1 Although 49% of hospices in the United States remain as not-for-profit providers, another 47% are now declared for-profit.1 Despite the tax status, management of a per diem fixed federal reimbursement payment requires all providers to carefully manage costs while delivering care to a geographically disperse, often isolated, and always clinically fragile population.
Hospice care in the United States is primarily delivered in the home setting. This home environment creates many similarities to home healthcare, including large geographic distribution of the patient population. The cost considerations and geographic challenges make telehealth technology an interesting solution for both home health and hospice populations. Although both the technology and research for telehealth technology has grown dramatically over the last decade in home healthcare, there has been less focus on the use of such technology in hospice care. The use of telehealth technologies to overcome the geographic distances in the delivery of hospice care has been termed telehospice. Although telehospice research has been conducted over the last 10 years, little is known about the comprehensive findings within the field. The purpose of this study was to systematically review the literature to discern available research and answer the question, what is the state of the evidence related to telehospice services?
Methods
A systematic review of the published literature was initiated to assess the evidence. PubMed and PsycINFO databases were searched for studies published between January 1, 2000 and March 23, 2010. Key words in the search included “telehospice,” “telemedicine and hospice,” “telehealth and hospice,” “technology and hospice,” and “informatics and hospice.” Studies were included if they were published in English in peer-reviewed journals and reported empirical data. Studies were excluded if they were non-English, in trade or nonpeer reviewed journals, and did not report data but were opinion or editorials. Data were extracted from each article using a standardized form. The extraction process identified the authors, sample size, setting, objectives, study design, and findings. Information collected on the standardized form was entered into a spreadsheet for analysis. The individual study findings were then coded to allow for comparison and identify common themes. Initial coding was developed by one author and reviewed for discussion among all authors. Finally, the articles were each reviewed and scored using the scoring form shown in Table 1 and described next.
Table 1.
Methodological Rigor Scoring
| Articles are scored with a methodology score from EITHER Part I A or Part I B AND a pertinence score using Part II | |
| PART I | |
| A. Quantitative article2 | |
| 1. Aims/outcome (observational and experimental) | |
| a. Defined at outset | 2 |
| b. Implied in paper | 1 |
| c. Unclear | 0 |
| 2. Sample formation (observational and experimental) | |
| a. Random | 2 |
| b. Quasi-random; sequential series in given setting or total available | 1 |
| c. Selected, historical, other, insufficient information | 0 |
| 3. Inclusion/exclusion criteria (observational and experimental) | |
| a. Explicitly described | 2 |
| b. Implied by patient characteristics, setting | 1 |
| c. Unclear | 0 |
| 4. Subjects described (observational and experimental) | |
| a. Full information | 2 |
| b. Partial information | 1 |
| c. No information | 0 |
| 5. Power of study calculated (observational and experimental) | |
| a. Yes | 2 |
| b. No | 0 |
| 6. Outcome measures (observational and experimental) | |
| a. Objective | 2 |
| b. Subjective | 1 |
| c. Not explicit | 0 |
| 7. Follow-upa (observational and experimental) | |
| a. >80% of subjects available for follow-up | 2 |
| b. 70-80% of subjects available for follow-up | 1 |
| c. <70% of subjects available for follow-up | 0 |
| 8. Analysis (observational and experimental) | |
| a. Intention to treat/including all available data | 2 |
| b. Excluding drop-outs but evidence of bias adjusted or no bias evident | 1 |
| c. Excluding drop-outs and no attention to bias or imputing results | 0 |
| 9. Baseline differences between groups (experimental only) | |
| a. None or adjusted | 2 |
| b. Differences unadjusted | 1 |
| c. No information | 0 |
| d. Cohort/descriptive study only/not applicable | 0 |
| 10. Unit of allocation to intervention (experimental only) | |
| a. Appropriate | 2 |
| b. Nearly | 1 |
| c. Inappropriate or no control group | 0 |
| d. Cohort/descriptive study only/not applicable | 0 |
| 11. Randomization/method of allocation of subjects (experimental only) | |
| a. Random | 2 |
| b. Method not explicit | 1 |
| c. Before exclusion of drop-outs or nonrandomized | 0 |
| d. Cohort/descriptive study only/not applicable | 0 |
| Total score (possible 22) | |
| PART I | |
| B. Qualitative scoring3 | |
| 1. Is there a clear connection to an existing body of knowledge/Theoretical framework? | |
| a. Yes | 1 |
| b. No | 0 |
| 2. Are research methods appropriate to the question being asked? | |
| a. Yes | 1 |
| b. No | 0 |
| 3. Is the description of the context for the study clear and sufficiently detailed? | |
| a. Yes | 1 |
| b. No | 0 |
| 4. Is the description of the method clear and sufficiently detailed to be replicated? | |
| a. Yes | 1 |
| b. No | 0 |
| 5. Is there an adequate description of the sampling strategy? | |
| a. Yes | 1 |
| b. No | 0 |
| 6. Is the method of data analysis appropriate and justified? | |
| a. Yes | 1 |
| b. No | 0 |
| 7. Are procedures for data analysis clearly described and in sufficient detail? | |
| a. Yes | 1 |
| b. No | 0 |
| 8. Is there evidence that the data analysis involved more than one researcher? | |
| a. Yes | 1 |
| b. No | 0 |
| 9. Are the participants adequately described? | |
| a. Yes | 1 |
| b. No | 0 |
| 10. Are the findings presented in an accessible and easy-to-follow manner? | |
| a. Yes | 1 |
| b. No | 0 |
| 11. Is sufficient original evidence provided to support the relationship between interpretation and evidence? | |
| a. Yes | 1 |
| b. No | 0 |
| Total score (possible 11) | |
| PART II | |
| Pertinence of studies to telehospice research. Scoring criteria adapted from Higginson5 | |
| 1. Study relevance to telehospice (The significance and bearing on the body of evidence in telehospice) | |
| 5 | Only or earliest published study in the review in its category |
| 4 | One of two studies of its type with in a review category |
| 3 | One of only a few studies of its type but with a unique aspect or findings |
| 2 | Replication of a previous telehospice study but with a unique aspect (sample, instrument, etc) or findings |
| 1 | of a previous telehospice study with different yet similar aspects or findings |
| 0 | Little relevance to telehospice-replication of a previous study with no unique aspects or findings |
| 2. Study applicability to telehospice (Degree and difficulty to which a study was translated into the hospice setting) | |
| 5 | hospice staff implemented without training or resources |
| 4 | hospice staff implemented with limited training or resources |
| 3 | hospice staff implemented with substantial training and resources |
| 2 | staff implemented without training or resources |
| 1 | staff implemented with training or resources |
| 0 | not determine whether new or existing staff implemented and what training or resources were necessary |
| 3. Study value to telehospice (the significance of the evidence to the overall establishment of evidence for the field.) | |
| 5 | Findings show improvement or challenge to specified outcomes or practice for telehospice |
| 4 | Findings show potential for improvement or challenge to specified outcomes or practice for telehospice |
| 3 | Findings identify new direction for practice or research in telehospice |
| 2 | Findings provide background for development of future telehospice projects or research |
| 1 | Findings support current telehospice practice or research |
| 0 | Findings do not apply to telehospice practice or research |
| Total score (possible 15) | |
#7 Follow-up modified from original to reflect time frames identified in the study and percentages changed to reflect high attrition found in hospice studies. #9,10,11 scoring of item d changed from 8 to 0 to allow comparison of scores.
Given the limited evidence available in both telehealth and hospice, a decision was made to evaluate the evidence by assessing both the methodological rigor and the significance of each study to the field of telehospice. As suggested by Gysles and Higginson,2 each study received a methodological score to reflect its scientific rigor as well as a pertinence score to recognize its significance to the overall evidence base found in the field. A study could, therefore, be of poorer methodological rigor yet have findings that are important to the evidence base. This was viewed as an especially critical issue in an emerging domain with limited but increasing evidence.
In recognition of and appreciation for the differences between quantitative and qualitative designs, different scoring schema were used to assess the methodological rigor based on the study design for individual articles. A standardized scoring form was developed to promote reliability in scoring across studies (See Table 1). The methodological rigor for quantitative articles used a modified scoring format from Gysles and Higginson2 that recognizes differences between observational and experimental research studies. The scoring format is outlined in Table 1, Part 1A. In this model, higher scores represent higher scientific rigor in the data collection, analysis, and reporting process. Scores range from 0 to 22 depending on the presence of certain elements influencing the methodological rigor. For example, a specified randomization procedure is given two points, a nonspecified randomization would be given one point, and a nonrandomized sample would receive no points for that element; thus, lower scores indicate less methodological rigor.
Likewise, the methodological rigor for qualitative articles was assessed using a standardized scoring form modified from the work of Greenwood.3 There is debate regarding the feasibility of quality assessment in qualitative research, and there is currently no gold standard scoring criteria for qualitative research. Greenwood's model was selected for this project because of its inclusion of relevant elements from several qualitative assessment frameworks and the ease of assessment and scoring generated from this approach. The quality assessment elements are outlined in Table 1, Part 1B. Similar to the quantitative scoring, a higher score reflects a higher degree of methodological rigor in the qualitative data collection, analysis, and reporting process. Articles were scored on a 0–11 scale with higher scores assigned to increased methodological rigor. In general, the more transparent the data collection and analysis, or the better detailed the procedures, the higher the score, as rigor in qualitative methodology is often based on the trustworthiness of the data.4
The second part of the assessment of the evidence involved evaluation of the pertinence of each of the studies, as illustrated in Table 1, Part 2. This criteria was adopted from a similar scheme for grading studies in palliative care.5 Pertinence refers to the degree to which the evidence is significant to telehospice.6 In a Higginson5 review, the pertinence of the evidence was a sum of three components: (1) the relevance to the building of evidence, (2) the applicability of the study, and the (3) overall value of the study. Relevance refers to having significant and demonstrable bearing on the facts or evidence of telehospice. Applicability is the ease to which the study translates into the implementation in hospice. Finally, value is determined by the significance of the evidence to the base of proof for the field. As in the scoring of methodological rigor, determining the pertinence of a study relies heavily on the clarity and transparency of the information reported in the article. For example, if an author does not report details on how the staff were involved in implementation, the study receives a lower score on this criteria in the same way it would if there were no sampling protocol reported.
Relevance was assessed in the context of the 26 articles reviewed. Articles that contributed something different than the others or a study conducted before others in a category or with a larger more diverse sample were seen as more relevant. Applicability was assessed through the evaluation of the translation of the study to the staff, how the study applied to hospice practice by the staff as well as the demands for staff, training, and resources. For example, if implementing a telehospice project requires substantial staff training, then it is not as translational or applicable as a project that uses current staff without additional training. Finally, a study's value was assessed based on the importance of the study findings for the future of the implementation of telehospice projects or future research in the field. Since pertinence is open to individual interpretation, it was not held as a single quality indicator for any article, rather it was combined with the methodological rigor scores in assessing the overall state of the evidence in telehospice. Although other studies have used this joint approach, no analysis of telehospice has involved this dual assessment.
To minimize bias in the scoring of each article, initial data extraction and scoring was done independently by the two authors not involved on any of the studies in this sample (T.D., H.N.). Coders were familiar with the health arena, but did not have telemedicine experience. Inter-rater reliability was achieved by discussion between the independent graders, and consensus was reached on the final scoring. An analysis table was built outlining the individual scores from each study, and the table was reviewed and discussed by all authors. Bias within studies was assessed in the scoring model through consideration of rigor; bias between studies in the sample was assessed by reviewing the sample of authors, journals, and themes.
Results
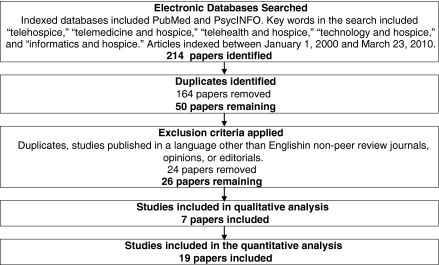
The initial search strategy identified 214 published articles. After a review of the abstracts and elimination of duplicates from the combined databases, a list of 50 articles was generated. Finally, the full articles were reviewed, and the inclusion criteria were applied, resulting in a final list of 26 unduplicated, peer-reviewed, empirically based telehospice studies published between January 1, 2000 and March 23, 2010. Figure 1 is a flow diagram of the sampling process.
Fig. 1.
Flow diagram of the search strategy.
The 26 studies were published in 13 unique journals, indicating no journal bias. Of note, the sample involved 10 teams of authors, with 47 different authors publishing evidence related to telehospice. Eight teams published one study, whereas two teams published 18 (61.5%) of the papers, indicating a limited number of researchers in the field and potential researcher bias in the evidence. Funding was acknowledged in 16 of the studies by nine sources and included university funding, private foundation support, and U.S. federal funding from the National Library of Medicine, National Cancer Institute, National Institute of Nursing Research, and U.S. Department of Commerce. The mean sample size in all studies was slightly >407, although there was a large variance with a range of 2 to 3,569. Table 2 identifies and summarizes the articles in the sample.
Table 2.
Summary of Studies in Telehospice
| PRIMARY AUTHOR (DATE) | FUNDING | SAMPLE SIZE | SETTING POPULATION | OBJECTIVE | STUDY DESIGN | FINDINGS | THEME |
|---|---|---|---|---|---|---|---|
| Carr et al. (2008)15 | Not specified | 155 | Staff from 2 hospice programs in Northeast | To evaluate use of telephone in a Palliative Care Advice Line | Interviews,Focus groups, surveys | Telephone advice line resolved specific clinical needs and provided support. | Use |
| Cook et al. (2001)16 | Not specified | 16 | Staff from 2 hospices in Kansas and Michigan | Analyze the success and challenges of doing telehospice care. | Interviews | Factors influencing success: administrative support, organizational culture, providers. | Use |
| Day et al. (2007)11 | National Library of Medicine | 17 | Staff from 2 Midwest hospice agencies | Understand staff perceptions and attitudes regarding the use of videophones in hospice. | Interviews | Providers had high degree of perceived use but lower perceptions of ease of use which may have impacted utilization. | Providers Attitude Barriers |
| Demiris et al. (2007)19 | Foundation | 12 | Senior caregivers in two hospice programs | To evaluate videophones as intervention tool to decrease caregiver anxiety and improve caregiver quality of life. | Outcome measures- STAI, CQLI-R | Caregivers were satisfied. Anxiety and quality of life are possible clinical outcomes. | Clinical Outcomes |
| Demiris et al. (2004)20 | University | 10 | Staff members from 5 Midwestern hospices | To assess receptiveness of hospice providers to telehospice, identify ways providers anticipate telehospice innovation to be useful, and identify concerns providers have about videophone technology. | Focus group | Providers had positive attitudes toward. | Providers Attitude |
| Demiris et al. (2008)21 | Nat. Cancer Inst. | 81 | Patient care discussions in two hospice programs | To explore the information flow of hospice meetings focusing on information access, exchange, and documentation. | Content analysis of videotapes | Technology may assist communication issues in team meetings. | Use |
| Doolittle (2000)22 | U.S. Department of Commerce | 3569 | Staff from one hospice in Ks/Mo | Examine the expenses of providing telehospice and to compare with traditional hospice. | Cost data analysis | Telemedicine visits are less expensive than home visits. | Cost |
| Doolittle et al. (2005)23 | U.S. Department of Commerce | 597 | 2 hospices in Kansas and Michigan | Conduct an initial needs assessment for telehospice. | Record review | Hospice services could be provided using technology to replace visits. | Use |
| Gregory et al. (2007)24 | Not specified | 88 | Palliative care units in the UK | Establish the current after hours prescribing practices in the UK. | Surveys | More guidance needed for remote prescribing. | Use |
| Hong et al. (2009)25 | Not specified | 3174 | Hospice nurses in Korea | Evaluate the adaption of a PDA information system. | Observation | PDA technology reduced nursing documentation time. | Use |
| Long et al. (2000)26 | Not specified | 122 | Staff across US | Determine use of computers and Internet in hospice and explore educational needs of staff. | Web-based survey | Staff had various computer experience and skill, education barriers exist. | Readiness |
| Parker Oliver and Demiris (2004)27 | Not specified | 124 | 62 hospice programs in Missouri | Identify current use of technology by hospice staff, assess readiness for telemedicine. | Mailed survey | Staff had various technology readiness but a willingness to use. | Readiness |
| Oliver and Haggarty (2003)28 | Not specified | 27 | One UK hospice | Evaluate the usefulness of displaying pro-forma information in case presentations. | Survey | Provider found technology useful and perceived as effective. | Use |
| Parker Oliver et al. (2009)29 | National Cancer Institute | 42 | Two hospices in Midwest | Evaluate experience of providers and caregivers to a telehospice intervention. | Interviews with staff and caregivers | Caregivers and providers found value in video. | Providers Attitudes Caregivers |
| Parker Oliver et al. (2006)9 | Foundation | 2 | 2 Hospice caregivers | Evaluate a telehospice intervention effect on anxiety and quality of life. | Interviews | Clinical outcomes assessed included Anxiety and Quality of Life. | Clinical Outcomes |
| Parker Oliver et al. (2005)30 | University | 74 | Seniors and hospice staff | Assess attitudes of seniors and hospice staff. | Observation | Seniors and Providers had positive attitudes toward the videophones. | Providers attitudes Patient attitudes |
| Parker Oliver et al. (2010)10 | National Cancer Institute | 143 | Caregivers and staff in two hospice agencies | Evaluate the use of a telehospice intervention on caregiver perception of pain. | Clinical assessment and interviews, observation | Caregivers Perception of Pain Medication was identified as the most sensitive measure, other measures not significant but used included patient and caregiver quality of life. | Clinical Outcomes |
| Quan et al. (2003)31 | Foundation | 980 | 2 hospices and 2 hospitals in Edmonton and Calgary | Determine whether TELFORM can be used to collect data. | Summary and note review, descriptive statistics and resource utilization. | A data collection tool was developed. | Use |
| Saysell and Routley (2003)32 | Not specified | 41 | Hospice in UK | Evaluate provider experience with a telehospice project. | Surveys, comments focus groups | Teleconference sessions improved teamwork, reduced costs, and kept patients in home longer. Providers had positive attitudes. | Providers attitudes |
| Washington et al. (2009)33 | University of Missouri | 160 | Hospice in 6 states | Explore staff perceived use and perceived usefulness of videophone technology in hospice. | Survey | Workers had positive perceived use and ease of use. | Providers attitudes |
| Whitten (2006)7 | U.S. Department of Commerce | 265 | 2 hospices in Kansas and Michigan | To explore providers and caregiver perception and utilization of telehospice. | Survey, interviews, nurses notes | Providers reported the technology easy to use. | Providers attitudes Patient attitudes |
| Whitten et al. (2004)34 | U.S. Department of Commerce | 189 | 1 hospice in Michigan | Describe how telehospice is used, why patients decline, and what patients like and do not like. | Survey, interviews, nurses notes | Patients had positive experience with the technology. | Patient attitudes |
| Whitten et al. (2005)35 | U.S. Department of Commerce | 55 | 1 hospice in Michigan | Understand provider perceptions of telehospice and how they change with use and the impact of provider perceptions on utilization. | Survey | Providers are gatekeepers for access. | Barriers |
| Whitten (2009)13 | Not specified | 25 | 1 hospice in Michigan | Identify elements of unified theory of acceptance that can explain nonadoption and understand what elements of organizational readiness for change can explain nonadoption | Survey and focus groups | Organizational factors influence acceptance. | Barriers |
| Whitten et al. (2005)36 | Not specified | 593 | 2 hospices in Michigan | To identify factors influencing provider acceptance | Survey and focus groups | Programs dependent on providers who are gatekeepers | Barriers |
| Wilkie et al. (2009)37 | NINR | 131 | Chicago hospices | Assess acceptability of pentablet program and the influence of various variables on acceptability | Observe and record review | Pen tablet was easy to use and patients willing to use | Patients attitudes |
PDA, personal digital assistant.
The findings of the individual studies were categorized into six themes: use, provider attitudes, patient/family attitudes, clinical outcomes, readiness, and cost. The most common findings related to assessments of the use of different telehospice technologies and assessments of provider attitudes. These two categories accounted for 61.5% of all articles. Studies assessing the use of telehospice included the evaluation of telephone advice lines, videophones, personal digital assistants, pen tablets, and computers. The various forms of technology were all found useful in the hospice setting and various considerations for success were identified. Overall, providers were supportive of all forms of the telehospice technologies. The provider attitudes were positive for both perceived usefulness and ease of use in different studies by different groups of researchers. Similarly, patient/family attitudes were assessed in 15% of the studies. Without exception, all articles reported that the majority of patients and families found the technology useful and helpful and demonstrating positive attitudes. In some cases, patients/families reported feeling that their providers could have used the technology more.7
Clinical outcomes were measured in only three of the studies.8–10 The outcomes measured included patient anxiety, caregiver quality of life, communication anxiety, and caregiver perceptions of pain medication. No study was large enough to find significance in these clinical measures, but all found the clinical tools appropriate for use in the setting.
Three studies reported various issues related to barriers to the implementation of telehospice projects. Specifically, despite the positive attitudes toward telehospice technologies, providers were found to be gatekeepers in the referral of consumers for telehospice interventions, thus limiting utilization. These results were discussed among two separate teams of videophone researchers.11,12 Additionally, organizational considerations were identified that facilitated and impeded the implementation of telehospice projects.13
The categories of study findings involved the assessment of readiness by providers in two studies and the assessment of cost in one study. Readiness to use and experience with technology varied among providers and points to the need for comprehensive training with implementation of any telehospice project. There was one study that focused on cost of telehospice visits and determined that they were a cost-effective alternative for providers.14
Methodological rigor was evaluated for each study and is summarized in Table 3. Nearly three quarters (73%) of the studies used quantitative methodologies. Studies were predominately cohort or descriptive. There was one experimental study; however, the differences between the groups were not adjusted, and assignment was not randomized, thus lowering its rigor. The criteria for follow-up (element 7 in the model) were difficult to score, because most studies did not report this information. The mean score for quantitative studies was 9.2 (range of 5–14) representing low-medium strength evidence. The lack of randomization and the lack of a power calculation weakened most of the evidence.
Table 3.
Scoring Summary of Studies in Telehospice
| |
QUALITY OF METHODOLOGY |
PERTINENCE |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PRIMARY AUTHOR (DATE) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | MEAN TOTAL | 1 | 2 | 3 | TOTAL |
| Qualitative Studies | ||||||||||||||||
| Carr et al. (2008)15 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 9 | 5 | 3 | 3 | 11 |
| Cook et al. (2001)16 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 5 | 5 | 3 | 5 | 13 |
| Day et al. (2007)11 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 | 3 | 3 | 5 | 11 |
| Demiris et al. (2004)20 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | 5 | 3 | 12 | |
| Demiris et al. (2008)21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 | 5 | 5 | 4 | 14 |
| Parker Oliver et al. (2009)29 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 | 5 | 4 | 4 | 13 |
| Parker Oliver et al. (2006)9 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 6 | 5 | 3 | 2 | 10 |
| Mean Qualitative Score | 9.0 | Mean Total | 12 | |||||||||||||
| Possible score 0–11 | Possible 15 | |||||||||||||||
| Quantitative Studies | ||||||||||||||||
| Demiris et al. (2007)19 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 14 | 4 | 4 | 2 | 10 |
| Doolittle (2000)22 | 2 | 0 | 2 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 10 | 5 | 5 | 1 | 11 |
| Doolittle et al. (2005)23 | 2 | 1 | 2 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 11 | 5 | 4 | 1 | 10 |
| Gregory et al. (2007)24 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 13 | 5 | 5 | 2 | 12 |
| Hong et al. (2009)25 | 2 | 0 | 1 | 0 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 7 | 5 | 3 | 4 | 11 |
| Long et al. (2000)26 | 2 | 0 | 0 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 8 | 4 | 5 | 3 | 12 |
| Parker Oliver and Demiris (2004)27 | 2 | 0 | 2 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 10 | 4 | 5 | 4 | 13 |
| Oliver and Haggarty (2003)28 | 2 | 0 | 1 | 1 | 0 | 1 | NA | 2 | 0 | 0 | 0 | 7 | 5 | 5 | 4 | 14 |
| Parker Oliver et al. (2005)30 | 2 | 2 | 1 | 2 | 0 | 1 | NA | 1 | 0 | 0 | 0 | 9 | 5 | 3 | 4 | 12 |
| Parker Oliver et al. (2010)10 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 1 | 0 | 13 | 5 | 5 | 4 | 14 |
| Quan et al. (2003)31 | 2 | 1 | 1 | 1 | 0 | 2 | NA | 1 | 0 | 0 | 0 | 8 | 5 | 4 | 4 | 13 |
| Saysell and Routley (2003)32 | 1 | 0 | 1 | 1 | 0 | 1 | NA | 2 | 0 | 0 | 0 | 6 | 5 | 5 | 4 | 14 |
| Washington et al. (2009)33 | 1 | 1 | 2 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 10 | 3 | 4 | 4 | 11 |
| Whitten et al. (2006)7 | 2 | 0 | 1 | 1 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 8 | 5 | 5 | 4 | 14 |
| Whitten et al. (2004)34 | 2 | 0 | 1 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 9 | 4 | 5 | 4 | 13 |
| Whitten et al. (2005)35 | 2 | 0 | 1 | 0 | 0 | 1 | 2 | 2 | 0 | 0 | 0 | 8 | 3 | 4 | 4 | 11 |
| Whitten et al. (2009)13 | 2 | 0 | 1 | 1 | 0 | 2 | 0 | 1 | 0 | 0 | 0 | 7 | 4 | 4 | 3 | 11 |
| Whitten et al. (2005)36 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 5 | 2 | 4 | 4 | 10 |
| Wilkie et al. (2009)37 | 2 | 0 | 2 | 2 | 0 | 2 | NA | 2 | 0 | 0 | 0 | 10 | 5 | 3 | 4 | 12 |
| Mean Quantitative Score | 9.1 | Mean Total | 12 | |||||||||||||
| Possible score 0–22 | Possible 15 | |||||||||||||||
Seven studies used qualitative methodology. The mean score of the qualitative evidence was 9 out of 11 (range of 5–11), representing medium-high strength of evidence. In reviewing the individual components of the quality scoring, the weakest component involved the adequate description of the subjects in three studies.9,15,16
In assessing the pertinence of the evidence, three component scores created a total score for each study. The total pertinence score averaged 12 (range of 10–14) out of a possible 15 for both quantitative and qualitative articles. This score demonstrates fairly high pertinence of the evidence. Several studies were small, thus reflecting the pilot nature of telehospice research.
Discussion
The assessment of research quality, although controversial, is important for building evidence-based medicine. The goal of a systematic review is to separate unsound or redundant work from innovative and carefully designed studies in an effort to identify gaps and provide guidance to research agendas.2 A systematic review is, in fact, a systematic collation and analysis of research findings that reduces information into a meaningful integrated package of evidence.17,18 One of the assumptions of a systematic review is that the evaluation of the evidence reflects what is published, and, thus, the comprehensiveness and accuracy of the evaluation is limited to what is documented in any given article.
The standard orientation of reviews has been toward using the randomized controlled trial (RCT) as the gold standard: however, in many instances, including emerging fields, the assessment of evidence needs to address different types of research, as decisions are made related to policy and implementation on a wider variety of evidence, inclusive of experimental, nonexperimental, and qualitative research. The methodology of these nonrandomized studies lays an important foundation of evidence for understanding meaning and issues that are critical to the future building of more clinically based traditional RCTs. Although there is no universally accepted way to assess qualitative and nonexperimental studies, there are models that have been used to assess the validity of these works.2
Despite the limitations presented by a small research base in terms of the traditional gold standard RCT, the standardized assessment of evidence can be valuable and used to inform future research agendas. Given the subjective nature of any scoring scheme inclusive of non-RCT studies, we have attempted to do so with the purpose of identifying gaps in the evidence and strengthening the future research in the field. To minimize the limitations, we have used a systematic process for identification of evidence and a defined standardized assessment schema, based on previous reviews in related fields (palliative care), as well as using a two-pronged approach to assess both rigor and pertinence. Finally, as authors of some of the studies in the review, we recognize the potential for bias in the assessment of evidence and, thus, have collaborated with two authors responsible for independent study assessment and consensus.
The identification of twenty six empirical studies shows that an evidence base for telehospice has emerged over the last 10 years. These studies, although of limited number, have established a foundation for the field. The evidence generated indicates that telehospice technologies hold promise to be useful and important tools for the future delivery of hospice care. The studies demonstrate that several technologies may be of use, that stakeholders (staff, patients, and family members) are interested and accepting the use, and that there are potential clinical outcomes and cost benefits. Implementation of telehospice technology has faced barriers in these early efforts including the various levels of readiness among staff, the differing perceptions of use and ease of use, and differing reports of technical quality challenges. Finally, implementation of more than one project has faced gate-keeping challenges by hospice staff, limiting the sample sizes, utilization, and success of the initial projects.
The evidence base, although growing and promising, is of mixed scientific rigor with lower-medium strength evidence in quantitative studies and medium-higher strength evidence in qualitative studies. Due to the limited number of researchers involved in telehospice research, there is also an element of researcher bias in the evidence. In spite of the limited amount of evidence available, the pertinence of all studies is fairly strong. Publication bias is limited, as these studies appeared in several journals across many disciplines including telemedicine, palliative medicine, and computer science. The interest by numerous journals in different disciplines indicates that telehospice is important and has wide-reaching practice, thus further validating the significance of building an evidence base.
If hospices are to invest in telehospice technology, then the evidence needs strengthening. Given the limited resources of hospice programs, patient outcome evidence is critical not only from a clinical perspective but also an administrative one. If telehospice is to live up to the promises found in these initial studies, then increased focus needs to be made in the building of evidence to identify the clinical benefits of telehospice programs and its associated cost savings. Finally, funding is needed to conduct large randomized trials and overcome the methodological limitations that are currently preventing the generalization of research findings. This, however, is not unlike the building of any evidence in palliative care, also a new and emerging field within medicine.
Disclosure Statement
No competing financial interests exist.
References
- 1.National Hospice and Palliative Care Organization. NHPCO Facts and Figures. Hospice Care in America 2008; 2009. [Google Scholar]
- 2.Gysels M. Higginson IJ. Systematic reviews. In: Addington-Hall J, et al., editors. Research methods in palliative care. Oxford: Oxford University Press; 2007. pp. 115–1134. [Google Scholar]
- 3.Greenwood N. Mackenzie A. Cloud GC. Wilson N. Greenwood N. Mackenzie A. Cloud GC. Wilson N. Informal primary carers of stroke survivors living at home-challenges, satisfactions and coping: a systematic review of qualitative studies. Disabil Rehabil. 2009;31:337–351. doi: 10.1080/09638280802051721. [DOI] [PubMed] [Google Scholar]
- 4.Tashakkori A. Teddlie C. Handbook of mixed methods in social and behavioral research. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- 5.Higginson IJ. Finlay I. Goodwin D. Jood K. Edwards A. Cook A. Douglas H. CE N. Is there evidence that palliative care teams alter end of life experiences of patients and their caregivers? J Pain Symptom Manage. 2003;25:150–168. doi: 10.1016/s0885-3924(02)00599-7. [DOI] [PubMed] [Google Scholar]
- 6.American heritage dictionary of the English language. Fourth. Houghton Miffin Company; 2009. [Aug;2010 ]. [Google Scholar]
- 7.Whitten P. Doolittle G. Hellmich S. Telehospice: Using telecommunication technology for terminally ill patients. J Comput Med Commun. 2006;6 doi: 10.1111/j.1083-6101.2001.tb00128.x. [DOI] [Google Scholar]
- 8.Demiris G. Parker Oliver D. Courtney K. Day M. Use of telehospice tools for senior caregivers: A pilot study. Clin Gerontol. 2007;31:43–58. [Google Scholar]
- 9.Parker Oliver D. Demiris G. Day H. Courtney KL. Porock D. Telehospice support for elder caregivers of hospice patients: two case studies. J Palliat Med. 2006;9:264–267. doi: 10.1089/jpm.2006.9.264. [DOI] [PubMed] [Google Scholar]
- 10.Parker Oliver D. Demiris G. Wittenberg-Lyles E. Porock D. Collier J. Arthur T. Caregiver participation in hospice interdisciplinary team meetings via videophone technology: A pilot study to improve pain management. Am J Hosp Palliat Care. 2010;27:465–473. doi: 10.1177/1049909110362402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Day M. Demiris G. Parker Oliver D. Exploring underutilization of videophones in hospice settings. Telemed J E Health. 2007;13:25–31. doi: 10.1089/tmj.2006.0023. [DOI] [PubMed] [Google Scholar]
- 12.Whitten P. Doolittle G. Mackert M. Whitten P. Doolittle G. Mackert M. Providers' acceptance of telehospice. J Palliat Med. 2005;8:730–735. doi: 10.1089/jpm.2005.8.730. [DOI] [PubMed] [Google Scholar]
- 13.Whitten P. Holtz B. Meyer E. Nazione S. Whitten P. Holtz B. Meyer E. Nazione S. Telehospice: reasons for slow adoption in home hospice care. J Telemed Telecare. 2009;15:187–190. doi: 10.1258/jtt.2009.080911. [DOI] [PubMed] [Google Scholar]
- 14.Doolittle GC. A cost measurement study for a home-based telehospice service. J Telemed Telecare. 2000;6(Suppl 1):S193–S195. doi: 10.1258/1357633001934645. [DOI] [PubMed] [Google Scholar]
- 15.Carr S. Lhussier M. Wilcockson J. Trasferring palliative care knowledge: Evaluating the use of a telephone advice line. Int J Palliat Nurs. 2008;4:303–308. doi: 10.12968/ijpn.2008.14.6.30026. [DOI] [PubMed] [Google Scholar]
- 16.Cook DJ. Doolittle GC. Whitten PS. Administrator and provider perceptions of the factors relating to programme effectiveness in implementing telemedicine to provide end-of-life care. J Telemed Telecare. 2001;7(Suppl 2):17–19. doi: 10.1258/1357633011937335. [DOI] [PubMed] [Google Scholar]
- 17.Mulrow C. Rationale for systematic reviews. BMJ. 1994;309:597–599. doi: 10.1136/bmj.309.6954.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pettigrew M. Systematic reviews from astronomy to zoology:myths and misconceptions. BMJ. 2001;322:98–101. doi: 10.1136/bmj.322.7278.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demiris G. Oliver DP. Courtney KL. Day M. Telehospice tools for caregivers: A pilot study. Clin Gerontol. 2007;31:43–57. [Google Scholar]
- 20.Demiris G. Parker Oliver D. Fleming D. Edison K. Hospice staff attitudes towards telehospice. Am J Hosp Palliat Care. 2004;21:343–347. doi: 10.1177/104990910402100507. [DOI] [PubMed] [Google Scholar]
- 21.Demiris G. Washington K. Parker Oliver D. Wittenberg-Lyles E. A study of information flow in hospice interdisciplinary team meetings. J Interprof Care. 2008;22:621–629. doi: 10.1080/13561820802380027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doolittle G. A cost measurement study for a home-based telehospice service. J Telemed Telecare. 2000;6:S193–S195. doi: 10.1258/1357633001934645. [DOI] [PubMed] [Google Scholar]
- 23.Doolittle G. Whitten PS. McCartney M. Cook D. Nazir N. An empirical chart analysis of the suitability of telemedicine for hospice visits. Telemed E Health. 2005;11:90–97. doi: 10.1089/tmj.2005.11.90. [DOI] [PubMed] [Google Scholar]
- 24.Gregory A. Todd J. Wanklyn S. Out-of-hours prescribing: a survey of current practice in the UK. Palliat Med. 2007;21:575–580. doi: 10.1177/0269216307081949. [DOI] [PubMed] [Google Scholar]
- 25.Hong H. Kim I. Lee S. Kim H. Adoption of a PDA-based home hospice care system for cancer patients. Comput Inform Nurs. 2009;27:365–371. doi: 10.1097/NCN.0b013e3181bcab43. [DOI] [PubMed] [Google Scholar]
- 26.Long C. Greenberg E. Ismeurt R. Smith G. Computer and Internet use by home care and hospice agencies. Home Healthcare Nurse. 2000;18:666–671. doi: 10.1097/00004045-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Parker Oliver D. Demiris G. An assessment of the readiness of hospice organizations to accept technological innovation. J Telemed Telecare. 2004;10:170–174. doi: 10.1258/135763304323070832. [DOI] [PubMed] [Google Scholar]
- 28.Oliver D. Haggarty P. Use of a pro forma and overhead projector to improve multidisciplinary team communication. Int J Palliat Nurs. 2003;9:358–359. doi: 10.12968/ijpn.2003.9.8.11525. [DOI] [PubMed] [Google Scholar]
- 29.Parker Oliver D. Washington K. Wittenberg-Lyles E. Demiris G. Porock D. “They're part of the team”: Participant evaluation of the ACTive intervention. Palliat Med. 2009;23:549–555. doi: 10.1177/0269216309105725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parker Oliver D. Demiris G. Porock D. The usability of videophones for seniors and hospice providers: A brief report on two studies. Comput Biol Med. 2005;35:782–790. doi: 10.1016/j.compbiomed.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 31.Quan K. Vigano A. Fainsinger R. Evaluation of a data collction tool (TELEform) for palliative care research. J Palliat Med. 2003;6:401–408. doi: 10.1089/109662103322144718. [DOI] [PubMed] [Google Scholar]
- 32.Saysell E. Routley C. Telemedicine in community-based palliative care: Evaluation of a videolink teleconference project. Int J Palliat Nurs. 2003;9:489–495. doi: 10.12968/ijpn.2003.9.11.11874. [DOI] [PubMed] [Google Scholar]
- 33.Washington K. Demiris G. Parker Oliver D. Day M. Telehospice acceptance among providers: A multidisciplinary comparison. Am J Hosp Palliat Med. 2009;25:452–457. doi: 10.1177/1049909108322289. [DOI] [PubMed] [Google Scholar]
- 34.Whitten P. Doolittle G. Mackert M. Whitten P. Doolittle G. Mackert M. Telehospice in Michigan: Use and patient acceptance. Am J Hosp Palliat Med. 2004;21:191–195. doi: 10.1177/104990910402100307. [DOI] [PubMed] [Google Scholar]
- 35.Whitten PS. Dolittle G. Mackert M. Providers' acceptance of telehospice. J Palliat Med. 2005;8:730–735. doi: 10.1089/jpm.2005.8.730. [DOI] [PubMed] [Google Scholar]
- 36.Whitten PS. Mackert MS. Whitten PS. Mackert MS. Addressing telehealth's foremost barrier: Provider as initial gatekeeper. Int J Technol Assess Health Care. 2005;21:517–521. doi: 10.1017/S0266462305050725. [DOI] [PubMed] [Google Scholar]
- 37.Wilkie D. Kim Y. Suarez M. Dauw C. Stapleton S. Gorman G. Storjell J. Zhao Z. Extending computer technology to hospice research: interactive pentablet measurement of symptoms by hospice cancer patients in their home. J Palliat Med. 2009;12:599–602. doi: 10.1089/jpm.2009.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]