Introduction
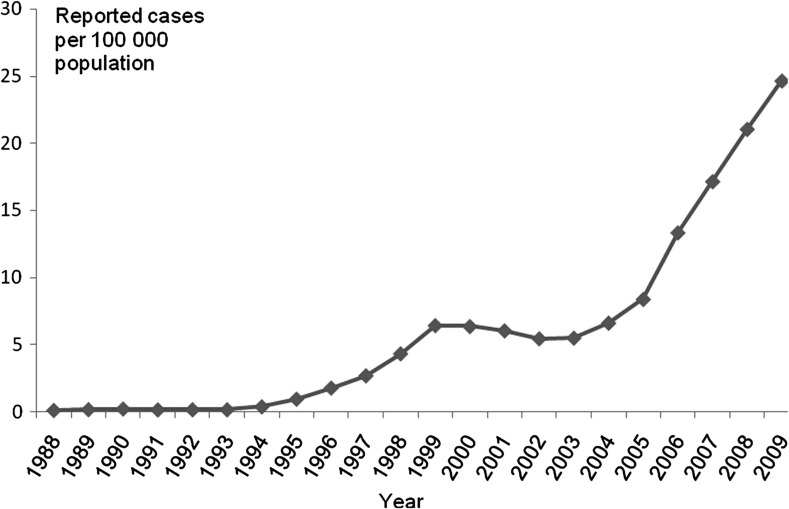
Syphilis has made a dramatic resurgence in China during the past two decades. During the Cultural Revolution (1966–76), sexually transmitted infections (STI) were so uncommon that they were removed from standard Chinese medical training curricula.1 As China's market economy expanded during 1980s economic reforms, reported STI, including syphilis infection, quickly re-appeared. An evolving STI reporting infrastructure largely assembled in the 1990s has noted increasing syphilis cases, particularly during the past 5 years (figure 1).2 3 Now syphilis is among the top five reported communicable diseases in many major province-level municipalities and provinces.4 While China's syphilis case reporting system and potential determinants of spread have been outlined in other reviews,2 there have been many studies on syphilis infection among female sex workers (FSW),5 6 this review analyses syphilis in China from the perspective of two critical high-risk populations: men who have sex with men (MSM) and low-tier FSW. Here we define low-tier FSW as women who usually solicit clients on the street or public outdoor places and sell sex for less than approximately €2–10 per client. Although preventing adverse outcomes associated with syphilis in pregnancy is important,7 this review focuses on adult syphilis infections in China. The purpose of this review is to examine syphilis epidemiology, risk behaviours, control strategies and research priorities in the Chinese context.
Figure 1.
Reported total syphilis cases per 100 000 population in China.2 3
Epidemiology and risk behaviours
Syphilis has emerged as a major public health problem among MSM in China. A meta-analysis of HIV and syphilis prevalence among MSM in China found increasing prevalence of both infections, with a summary syphilis prevalence of 9.1%.8 Several cohort studies have demonstrated a high incidence of HIV, syphilis and HIV/syphilis co-infection among Chinese MSM (table 1).9–13 Whereas MSM are believed to account for 2–4% of the Chinese adult male population,14 they comprised an estimated 32.5% of all new HIV cases in 2009.15 Although disease monitoring has improved in the past 10 years, routine surveillance of MSM remains incomplete, and only 8.6%were covered by health surveillance and outreach efforts by the end of 2008.16
Table 1.
Comparison of syphilis among MSM and low-tier FSW in China
| Variable | MSM | Low-tier FSW* |
| Syphilis prevalence estimates | 9.1% (95% CI 7.6% to 10.8%)8 | 12.5% (IQR 4.1–20.1)19 |
| Syphilis incidence estimates | 8–17 cases per 100 person years9–13 | Unknown† |
| Population size | 3.6–7.1 million30 † | Unknown‡ |
| Partner notification | Not routine | Not routine |
| Civil society organisations31 | 121 | 30 |
Defined as women who usually solicit clients on the street or public outdoor places and sell sex for less than €2–10 per client.
Number of men who have sex with men (MSM) at high risk, which was estimated in 2005.30
Low-tier female sex workers (FSW) are difficult to reach by conventional public health outreach and estimating the population size and retaining them in cohorts is challenging.
Although there are fewer epidemiological studies, low-tier FSW also have an increased risk of syphilis and other STI.17 Extensive sociological and anthropological research from China suggests there are distinct typologies of female sex work, each with well-defined work locations, income and sexual risks.18 Low-tier FSW either independently solicit clients in parks (street-walking FSW) or find clients through managers/pimps at beauty salons or construction sites.18 A systematic review found that low-tier FSW are approximately twice as likely to have syphilis as FSW who charge more per client.19 Some studies have found extremely high syphilis prevalence in this group, ranging from 10% to 38%.20 21 However, low-tier FSW are less well represented in current surveillance and intervention programmes in China. Higher sexual risk among low-tier FSW may be related to greater numbers of clients per day,22 less condom self-efficacy with clients that can pay extra for unsafe sex, or more frequently changing work locations.23 24
Syphilis control strategies
Traditional syphilis control strategies focus on screening of high-risk groups, timely diagnosis and treatment, partner notification and treatment, and education/awareness campaigns.25 Although there have been some small pilot behavioural intervention programmes for MSM26 and low-tier FSW,22 both of these groups are difficult to identify and longitudinally follow in the Chinese context. Several government programmes and the Global Fund initiative have supported local civil society organisations to promote condoms and sexual health, although the programmatic focus has been on HIV prevention to date. China's recently launched 10-year national syphilis control and prevention plan includes explicit targets for decreasing primary syphilis cases, establishing a strong foundation for further targeted syphilis control programmes.27 Beyond case finding, ensuring that individuals and their sex partners receive appropriate treatment is also critical for syphilis control. The availability of rapid point-of-care tests in many public and private clinics in China helps promote routine screening and timely diagnosis.28 In addition, developing syphilis partner notification systems that are acceptable to MSM, low-tier FSW and other high-risk groups are important for developing a comprehensive syphilis control response.
Research priorities
Responding to the syphilis epidemics among MSM and low-tier FSW in China will require further research. Innovative strategies to access hard-to-reach populations and prevent STI/HIV should be developed as only a small part of these two populations are now covered by control programmes in China. Creating responsive clinical services and syphilis testing sites takes time and requires input not only from key public health leaders and clinicians, but also from civil society organisations and community groups that are largely incipient in China. In this context, MSM civil society organisations are more well organised than FSW groups in China, but both types of organisations require further training, more personnel and greater programmatic experience in order to help implement syphilis control programmes. Integration of syphilis testing into provider-initiated HIV testing and counselling may be a good opportunity not only to help detect syphilis infections but also to strengthen HIV case finding.29 An ongoing project supported by the World Health Organization and the China–Australia Health and HIV/AIDS Facility focuses on integrating syphilis control into Chinese provider-initiated HIV testing and counselling practice. The high burden of syphilis among MSM and subsets of FSW creates unique opportunities for syphilis control research.
Conclusions
China has a resurgent syphilis epidemic that is particularly prominent among MSM and low-tier FSW. Several domestic and international programmes focused on these high-risk groups in China establish a strong foundation to implement syphilis-specific control programmes. With explicit benchmarks and process indicators, the national syphilis control plan holds great promise. As China has demonstrated with HIV control efforts, high-level government commitment can translate into a number of scalable, substantive and efficacious programmes.32
Acknowledgments
The authors would like to give special thanks to Helena Chang for providing assistance identifying research focused on low-tier FSW.
Footnotes
Funding: Financial support for this research came from the Mega Project of China National Science Research for the 11th Five-Year Plan (2008ZX10001-005), theNIH Fogarty K01 Award (US NIH 1K01TW008200-01A1), the UNC Social Science Research on HIV/AIDS in China (NIH NICHD R24 HD056670-01), the UNC Center for AIDS Research, the China–Australia Health and HIV/AIDS Facility Project (HIV 04), WHO Country Project (CHN/10/HS/003353) and the WHO Rapid Syphilis Test Project (Unicef/UNDP/World Bank/WHO A70577).
Competing interests: None.
Contributors: JDT, XSC and MSC conceived of the idea, JDT and XSC drafted the manuscript, YPY and BW commented on the draft, and all authors were actively involved in revising the manuscript and approval of the final version.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Cohen MS, Henderson GE, Aiello P, et al. Successful eradication of sexually transmitted diseases in the People's Republic of China: implications for the 21st century. J Infect Dis 1996;174(Suppl 2):S223–9 [DOI] [PubMed] [Google Scholar]
- 2. Chen ZQ, Zhang GC, Gong XD, et al. Syphilis in China: results of a national surveillance programme. Lancet 2007;369:132–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NCSTD Epidemiologic reports of syphilis and gonorroea case reports in China. http://www.ncstdc.org/zxgl-detail/zxgl-xxjl.htm (accessed 11 May 2011).
- 4. Yang LG, Tucker JD, Yang B, et al. Primary syphilis cases in Guangdong Province 1995–2008: opportunities for linking syphilis control and regional development. BMC Public Health 2010;10:793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang H, Wang N, Bi A, et al. Application of cumulative odds logistic model on risk factors analysis for sexually transmitted infections among female sex workers in Kaiyuan city, Yunnan province, China. Sex Transm Infect 2009;85:290–5 [DOI] [PubMed] [Google Scholar]
- 6. Lu F, Jia Y, Sun X, et al. Prevalence of HIV infection and predictors for syphilis infection amone female sex workers in southern China. Southeast Asian J Trop Med Public Health 2009;40:263–72 [PMC free article] [PubMed] [Google Scholar]
- 7. Kamb ML, Newman LM, Riley PL, et al. A road map for the global elimination of congenital syphilis. Obstet Gynecol Int 2010. doi:10.1155/2010/312798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gao L, Zhang L, Jin Q. Meta-analysis: prevalence of HIV infection and syphilis among MSM in China. Sex Transm Infect. 2009;85:354–8 [DOI] [PubMed] [Google Scholar]
- 9. Ruan Y, Jia Y, Zhang X, et al. Incidence of HIV-1, syphilis, hepatitis B, and hepatitis C virus infections and predictors associated with retention in a 12-month follow-up study among men who have sex with men in Beijing, China. J Acquir Immune Defic Syndr 2009;52:604–10 [DOI] [PubMed] [Google Scholar]
- 10. Xu JJ, Zhang M, Brown K, et al. Syphilis and HIV seroconversion among a 12-month prospective cohort of men who have sex with men in Shenyang, China. Sex Transm Dis 2010;37:432–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hao C, Yan H, Yang H, et al. The incidence of syphilis, HIV and HCV and associated factors in a cohort of men who have sex with men in Nanjing, China. Sex Transm Infect 2011;87:199–201 [DOI] [PubMed] [Google Scholar]
- 12. Li D, Jia Y, Ruan Y, et al. Correlates of incident infections for HIV, syphilis, and hepatitis B virus in a cohort of men who have sex with men in Beijing. AIDS Patient Care STDS 2010;24:595–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yang H, Hao C, Huan X, et al. HIV incidence and associated factors in a cohort of men who have sex with men in Nanjing, China. Sex Transm Dis 2010;37:208–13 [DOI] [PubMed] [Google Scholar]
- 14. Wei C, Guadamuz TE, Stall R, et al. STD prevalence, risky sexual behaviors, and sex with women in a national sample of Chinese men who have sex with men. Am J Public Health 2009;99:1978–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. MOH 2009 Estimates for the HIV/AIDS Epidemic in China. Beijing: Ministry of Health/UNAIDS/WHO, 2010 [Google Scholar]
- 16. UNAIDS MSM Update for the International Congress on AIDS in Asia and the Pacific. Bali: UNAIDS, 2010 [Google Scholar]
- 17. Tucker JD. The social context of sexual HIV prevention among female sex workers in China. Int J Epidemiol. Published Online First: 15 February 2011. doi:10.1093/ije/dyr021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang Y, Henderson GE, Pan S, et al. HIV/AIDS risk among brothel-based female sex workers in China: assessing the terms, content, and knowledge of sex work. Sex Transm Dis 2004;31:695–700 [DOI] [PubMed] [Google Scholar]
- 19. Chang H, Zhi X, Chen X-S, et al. Systematic review and meta-analysis of syphilis seroprevalence among female sex workers in China. NIH Fogarty International Clinical Scholar Conference, Bethesda, 24 Sept 2010 [Google Scholar]
- 20. Yang P, Wang QQ, Peng H. A survey of syphilis and HIV infection in medium-low-income female sex workers. China J Lepr Skin Dis 2009;25:174–6 [Google Scholar]
- 21. Chen XS. Preliminary results of the Mega Project of China National Science Research for the 11th Five-Year Plan (2008ZX10001-005). The Fifth National STD Conference of China. Haikou, China, 16–17 May 2010 [Google Scholar]
- 22. Wang Q, Yang P, Gong XD, et al. Syphilis prevalence and high risk behaviors among female sex workers in different settings. Chin J AIDS STDs 2009;15:398–400 [Google Scholar]
- 23. Yang X, Xia G. Gender, work, and HIV risk: determinants of risky sexual behavior among female entertainment workers in China. AIDS Educ Prev 2006;18:333–47 [DOI] [PubMed] [Google Scholar]
- 24. Yang X, Xia G, Li X, et al. Social influence and individual risk factors of HIV unsafe sex among female entertainment workers in China. AIDS Educ Prev 2010;22:69–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Parran T. Shadow on the Land, Syphilis. New York: Reynal & Hitchcock, 1937 [Google Scholar]
- 26. Zeng G, Xiao Y, Xu P, et al. Evaluation of effect of community-based HIV/AIDS interventions among men who have sex with men in eighteen cities, China. Chin J Prev Med 2009;43:977–80 [PubMed] [Google Scholar]
- 27. Anonymous. AIDS-level prevention measures to slow soaring syphilis. Xinhua 22 June 2010. http://www.china.org.cn/china/2010-06/22/content_20314930.htm (accessed 10 Jun 2011). [Google Scholar]
- 28. Tucker JD, Yang LG, Zhu ZJ, et al. Integrated syphilis/HIV screening in China: a qualitative analysis. BMC Health Serv Res 2010;10:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tucker JD, Yang LG, Yang B, et al. A twin response to twin epidemics: integrated HIV/syphilis testing at STI clinics in South China. J Acquir Immune Defic Syndr 2011;57:e106–e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lu F, Wang N, Wu Z, et al. Estimating the number of people at risk for and living with HIV in China in 2005: methods and results. Sex Transm Infect 2006;82(Suppl 3):iii87–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. NCAIDS China HIV/AIDS Information Network 2009/2010 China HIV/AIDS NGO Directory. Beijing: NCAIDS, 2010 [Google Scholar]
- 32. Wu Z, Wang Y, Detels R, et al. China AIDS policy implementation: reversing the HIV/AIDS epidemic by 2015. Int J Epidemiol 2010;39(Suppl 2):ii1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]