Abstract
Background and Aims
Great efforts have been made to predict disease behavior over time and the response to treatment in Crohn’s disease (CD). Such understanding could personalize therapy. Early introduction of more aggressive therapies to patients at high risk and no introduction of predictable refractory treatments could become possible. We hence tested the influence of the NOD2 carrier status on treatment response.
Patients and Methods
In 185 CD patients (age 45 ± 9.8 years, female n = 108, minimum disease duration 10 years), the three most common polymorphisms (p.Arg702Trp, p.Gly908Arg, p.Leu1007fsX1008) of NOD2 were tested by polymerase chain reaction and sequencing. Detailed clinical and medical history were obtained with a standardized questionnaire and by reviewing the medical charts. Treatments introduced were chosen by physicians blinded to genotype data.
Results
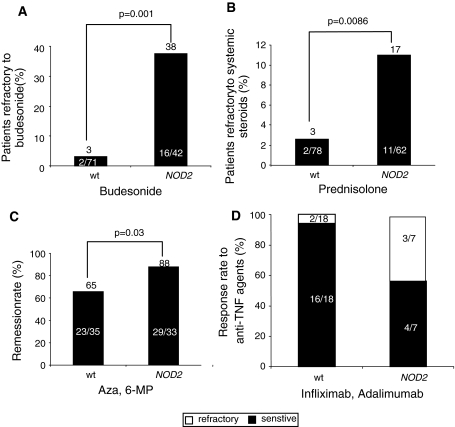
The frequency of the NOD2 variant allele was about one-third (67, 30.2%) of CD patients. NOD2 carriers were more often treated with systemic and locally active steroids and with an immunosuppressant (Azathioprine/6-MP). NOD2 mutation carrier status was more often associated with systemic steroid [8.9% vs. wild-type (WT) 1.2%, P = 0.0086] and local-steroid refractory (14.9% vs. WT 3.5%; P = 0.001). The WT patients were significantly higher refractory to immunosuppressant (12.8% vs. NOD2 carriers, 0.5%, P = 0.03). Most WT patients were treated with TNF-α antagonists and remission rates were significantly higher in this group after 1 year of treatment (84% vs. NOD2 carriers, 33%, P = 0.07).
Conclusions
The study presents first hints for the NOD2 carrier status to be predictive for response to therapy. A higher percentage of CD patients with NOD2 mutation carrier status was steroid refractory but could be treated well with immunosuppressants. The WT status showed a higher response to steroids and remission rates within 1 year of anti-TNF-α therapy. On the way to personalized medicine, this approach should be further investigated in larger studies.
Keywords: NOD2, Crohn’s disease, TNF-α antagonist, Top-down, Step-up
Introduction
Crohn’s disease (CD) is a chronic inflammatory disorder of the gastrointestinal tract. It is a multifactorial, polygenic disease with genetic heterogeneity. In addition to genetic predisposition, various host (e.g., epithelial, immune, and nonimmune) and environmental factors play a major role in the pathogenesis of CD [1, 2]. Guidelines recommend that most patients with active disease should be treated initially with corticosteroids [3, 4]. Although this approach is usually effective for control of symptoms, many patients become refractory to, or dependent on, these drugs [5, 6]. For this reason, a treatment with corticosteroid-sparing drugs, such as azathioprine, mercaptopurine, or methotrexate, should be initiated [7–9]. Recent published data underline the concept of an early combined immunosuppression in CD, the so-called “top-down” strategy [10]. A combined immunosuppressive therapy with antimetabolites/methotrexate and TNF-α antagonists is associated with a higher risk of opportunistic infections and hepatosplenic T cell lymphoma [11]. Therefore, great efforts have been made to predict disease behavior over time and the response to treatment in CD. Early introduction of more aggressive therapies to patients at high risk of disabling disease, and no introduction of predictable refractory treatments to reduce side effects of therapies, could become possible [12]. Attempts have been made to define clinical subgroups on the basis of age at onset, disease location, extent (diffuse or localized), and behavior (primary inflammatory, fistulizing, or fibrostenotic disease). Mucosal TNF-α transcripts in steroid-refractory CD patients receiving immunosuppressive therapy may have predictive values [13].
Crohn’s disease has a strong genetic component, with a lifetime risk of 10–20% to develop CD in the presence of an affected first-degree relative, thus defining subgroups based on genetic mutations might be a helpful marker [14, 15]. To date, genome-wide meta-analysis has identified at least 71 loci that confer susceptibility to CD [16]; the first, and most consistently replicated, critical mutations were found in the CARD15/NOD2 gene on chromosome 16 (IBD1) [17]. The physiological role of the NOD2 protein remains under detailed examination. Variant NOD2 alleles are associated with reduced (alpha)-defensin release from Paneth cells in response to bacteria [18]. Of particular importance is the C-terminus leucine-rich repeat domain, reportedly the major structural motif that functions as a pattern-recognition receptor for the microbial component muramyl dipeptide [19].
Two single-nucleotide polymorphisms of NOD2 (p.Arg702Trp and p.Gly908Arg) and a frame-shift mutation (p.Leu1007fsX1008) were shown by independent groups to be associated with susceptibility to CD [20–22]. The presence of 1 variant allele increases the risk of developing CD from 1.5- to 4.3-fold; the presence of 2 copies increases the risk to 20- to 40-fold [23–25]. CD patients with NOD2 mutations exhibit early onset of the disease, mainly ileal involvement and increased risk of surgical intervention after developing complications such as strictures, fistulas and stenosis [14, 17, 26]. NOD2 mutation carrier status does currently not allow the predicting of disease progression and the need of immunosuppressive therapies such as steroids, azathioprine or biologicals (i.e. TNF-α antagonists).
Based on these observations, we aimed to test a possible influence of the NOD2 carrier status on response to standard medical treatments. Such understanding could personalize therapy.
Patients and Methods
Study Population and Disease Phenotype
Written, informed consent was obtained from all patients prior to the study. The study was approved by the Ethics committee of the Ulm University and adhered to the ethical principles for medical research involving human subjects of the Helsinki Declaration (http://www.wma.net/e/policy/b3.htm). For the diagnosis of CD, established diagnostic guidelines including endoscopic, radiological, and histopathological criteria were used [27]. Patients with CD were assessed according to the Montreal classification based on age at diagnosis (A), location (L), and behavior (B) of the disease. Patients with colonic inflammatory bowel disease unclassified (IBDU) were excluded from the study. Phenotypic characteristics included demographic data and clinical parameters (behavior and anatomic location of IBD, disease-related complications, previous surgery or immunosuppressive therapy) which were recorded by investigation of patient charts and a detailed questionnaire including an interview at the time of enrolment. All phenotypic data were collected blind to the results of the genotypic data.
DNA Extraction and Genotyping of the NOD2 Variants
Blood samples were taken from all study participants, and genomic DNA was isolated from peripheral blood leukocytes using the DNA blood mini kit from Qiagen (Hilden, Germany) according to the manufacturer’s guidelines. DNA was amplified by PCR with primer pairs flanking the p.Arg702Trp, p.Gly908Arg, and p.Leu1007fsX1008 variants as described [28]. After purification, PCR products were analyzed with the ABI PRISM Dye Terminator Cycle Sequencing KIT (Applied Biosystems, Darmstadt, Germany) on an ABI 373A DNA-sequencer using the same primers applied for amplification.
Definitions of Response to Therapy
All patients were treated according to the German clinical practice guidelines on the diagnosis and treatment of CD [27] blinded to the genotype data. Patients received budesonide (9 mg/day), prednisolone (2 mg/kg up to 60 mg), immunomodulators (2.5 mg/kg for AZA and 1–1.5 mg/kg for 6-MP), infliximab (5 mg/kg at weeks 0, 2, 6 and every 8 weeks) or adalimumab (80 mg starting dose followed by 40 mg every second week). When patients were treated with steroids, remission was defined by a decrease of the CDAI score to 150 or less. Patients who responded to prednisolone but relapsed upon steroid withdrawal were defined as steroid-dependent. Patients who did not respond to steroids, defined by decrease of the CDAI score of at least 70 within the first 4 weeks, were defined as steroid-refractory [27]. When immunomodulators (AZA/6-MP) were given, clinical remission was defined by a decrease of the CDAI score to 150 or less after steroid withdrawal for more than 3 months. When TNF-α antagonists (infliximab/adalimumab) were used, remission was defined as a decrease of the CDAI score to 150 or less after 2–3 infusions (infliximab, weeks 3–7) or after 3 injections (adalimumab, week 6).
Statistical Analyses
All data given in the text and figures are expressed as mean values ± SEM. The data were analyzed using non-parametric two-tailed Mann–Whitney U test with P ≤ 0.05 considered as an indicator of significance. In addition, a multivariate assessment of the relationship between the independent variables “group [wild-type (WT) vs. NOD2],” “localization (ileus, colon, etc.),” “stricture (yes vs. no),” “fistula (yes vs. no),” “surgery (yes vs. no)” and the dependent outcome variable “therapy response to steroids (yes vs. no)” was carried out. Due to the binary characteristic of the dependent variable “therapy response,” a multivariate logistic regression model has been chosen as statistical method for analyzing the data.
Results
Demographic Characteristics of the Study Population
One hundred and eighty-five patients were included in our retro-perspective study. NOD2 carrier status was found in 77 patients including 1 homozygous NOD2 carrier. The demographic characteristics and disease location according to the Montreal classification are depicted in Table 1. More patients with NOD2 variants had disease location at the ileal site; significantly more patients with NOD2 carrier status developed stricturing and/or penetrating disease behavior as compared to NOD2 WT patients confirming previous reports (Table 1).
Table 1.
Demographic characteristics of the study population
| NOD2−/− | NOD2+/− | NOD2+/+ | Significance P value | |
|---|---|---|---|---|
| Male n (%) | 41 (53%) | 35 (45%) | 1 (1.3%) | 0.634 |
| Median age at diagnosis (year) | 30.1 (14–59) | 26.4 (15–48) | 18 | 0.712 |
| Disease location (n and %) (Vienna) | ||||
| Ileal disease: L1 | 26/118 (22.1%) | 21/68 (30.9%) | 0.1076 | |
| Colonic disease: L2 | 10 (8.2%) | 3 (4.1%) | 0.09 | |
| Ileocolonic disease: L3 | 59 (50.8%) | 33 (48.8%) | 1 | 0.7966 |
| Upper gastrointestinal involvement | 15 (13.1%) | 2 (3.1%) | <0.05 | |
| Anal involvementa | 24 (21.1%) | 10 (14%) | 1 | 0.134 |
| Disease behavior (n and %) Vienna | ||||
| Inflammatory (B1) | 48 (41%) | 34 (50.5%) | 1 | 0.356 |
| Stricturing (B2) | 16 (14%) | 19 (28.2%) | 1 | 0.08 |
| Penetrating (B3) | 53 (45%) | 20 (29%) | 1 | <0.05 |
| Need for IBD surgery | 52 (44%) | 49 (72%) | 1 | <0.05 |
| History of smoking | 63 (53%) | 31 (45%) | Not significant | |
| Extraintestinal manifestations | 39 (33%) | 24 (35%) | Not significant | |
| p.Arg702Trp | 31 | |||
| p.Gly908Arg | 34 | 1 | ||
| p.Leu1007fsX1008 | 18 | |||
a(L1) + (L3) + (L4 − patients with ileal involvement)
Ninety-four patients were initially treated with budesonide including 42 NOD2 carriers, 140 patients including 62 NOD2 carriers were treated with prednisolone, 68 patients were treated with immunosuppressants(AZA/6-MP), including 33 NOD2 carriers, and 25 patients received TNF-α antagonists (infliximab or adalimumab, respectively) (Table 2).
Table 2.
Medication of the study population including 67 patients with NOD2 variants
| Medication | Study collectivea | WT NOD2 statusb | NOD2 carrierc |
|---|---|---|---|
| Budesonide | 50.8% (94/185) | 44.1% (52/118) | 62% (42/67) |
| Prednisolone | 75.7% (140/185) | 66.1% (78/118) | 92.5% (62/67) |
| Immunomodulators | 36.7% (68/185) | 39.7% (35/118) | 49.2% (33/67) |
| Anti-TNF-α | 13.5% (25/185) | 15.3% (18/118) | 10.4% (7/67) |
aPercentage of patients of the total study collective receiving the indicated medication. The numbers in parentheses indicate the total numbers of patients within the study collective of 185 patients treated by the indicated medication
bPercentage of patients with the WT NOD2 status treated by the indicated medication. The numbers in parentheses indicate the total numbers of 118 patients with WT NOD2 status receiving the indicated medication
cPercentage of patients with NOD2 variants receiving the indicated medication. The numbers in parentheses indicate the total numbers of 67 patients with NOD2 variants treated by the indicated medication
More NOD2 Carriers are Refractory to Treatment with Budesonide
First, we determined the response to budesonide. Seventy-one percent of NOD2 WT patients responded to the treatment with budesonide, 21% were budesonide-dependent and 8% were refractory to budesonide. Budenoside treatment of NOD2 WT patients was more effective in patients with ileal-cecal disease location. When NOD2 carriers were analyzed, 33% of NOD2 carriers responded to budesonide, 19% were steroid-dependent and 48% were refractory to treatment with budesonide. Budesonide-treated patients with NOD2 variants were significantly impaired in response to budesonide (Fig. 1). Together, this data indicated that patients with NOD2 WT status show better response rates to budesonide as compared to patients with NOD2 variants.
Fig. 1.
a The percentage of patients with NOD2 WT status responding to treatment with budesonide is increased as compared to patients with NOD2 variants. The percentage of patients refractory to budesonide treatment is presented. b The percentage of patients with NOD2 carrier status refractory to prednisolone treatment is increased. In the non-parametric two-tailed Mann–Whitney U test, P ≤ 0.05 was considered statistically significant; WT, NOD2 wild-type status; NOD2, patients with NOD2 variants. c The percentage of patients with NOD2 carrier status in remission under treatment with immunomodulators (AZA/6-MP) is increased as compared to patients with NOD2 wild-type status. The percentage of patient in remission under treatment with AZA/6-MP with NOD2 carrier status was compared with WT NOD2 patients. d Patients with NOD2 wild-type status respond to treatment with TNF-α antagonists. Black area indicates the percentage of patients in remission under treatment with TNF-α antagonist, and the white area indicates the percentage of patients responding to treatment with TNF-α anatgonist. Numbers within the area indicate the numbers of patients within the total numbers of patients per indicated group; numbers on top of the bars indicated the percentage of patients in the respective group. A non-parametric two-tailed Mann–Whitney U test was used; P ≤ 0.05 was considered as an indicator of significance; WT, NOD2 wild-type status; NOD2, patients with NOD2 variants
Impaired Response to Prednisolone in CD Patients with NOD2 Carrier Status
Next, we determined the response to prednisolone in our study collective. Fifty-seven percent of patients with NOD2 WT status were sensitive to the treatments with prednisolone, 39% were steroid-dependent, and 2% were refractory to prednisolone treatment. When NOD2 carriers were analyzed, 46% of NOD2 carriers were sensitive to prednisolone, 35% were steroid-dependent, and 17% were refractory to treatment with prednisolone. Again, significantly more patients with NOD2 variants were refractory to prednisolone as compared to patients with NOD2 WT status, but this difference was not as pronounced as with budesonide (Fig. 1). Because more patients with NOD2 variants had disease location at the ileal site and developed more likely stricturing and/or penetrating disease behavior, we tested in a multivariate logistic regression model if the independent variables localization (ileal site), stricturing or internal fistulizing disease behavior and surgery influence the therapy success of the treatment with steroids. The success of treatment with steroids did not depend on disease location, the development of stricturing and/or penetrating disease behavior and not on surgery. The success of treatment with prednisolone depended in our model and patient collective only on the NOD2 carrier status (Table 3).
Table 3.
Effects of the independent variables localization (ileal site), stricturing or internal fistulizing disease behavior and surgery on therapy success with systemic steroids in a multivariate logistic regression model
| P value | |
|---|---|
| Localization (ilelal site L1 + L3) | 0.4682 |
| Stricturing (B2) | 0.1015 |
| Internal fistulizing (B3) | 0.8845 |
| Surgery | 0.8992 |
In the multivariate logistic regression model, a P value <0.05 was considered as statistically significant
Response of NOD2 Carriers to Immunomodulators (AZA/6-MP)
Because the percentage of patient refractory to the treatment with prednisolone was significantly increased among the patients with NOD2 variants as compared to patients with NOD2 WT status, we next analyzed the response of patients with NOD2 variants to immunomodulators (AZA/6-MP). Sixty-five percent of patients with NOD2 WT status went into remission under treatment with AZA/6-MP, whereas 34% of patients with NOD2 WT status were refractory to treatment with AZA/6-MP. Eighty-eight percent of patients with NOD2 variants went into remission under treatment with AZA/6-MP, and 12% of patients with NOD2 variants were refractory to treatment with AZA/6-MP. The percentage of patients with NOD2 variants in remission under treatment with AZA/6-MP was significantly increased as compared to patients with NOD2 WT status (Fig. 1). In contrast, significantly more patients with NOD2 WT status were refractory to treatment with AZA/6-MP as compared to patients with NOD2 variants.
Response of NOD2 Carriers to Treatment with TNF-α Antibodies (Infliximab/Adalimumab)
We next analyzed the response of the patients to the TNF-α antagonists infliximab or adalimumab. Eighty-nine percent of patients with NOD2 WT status went into remission under treatment with TNF-α antagonists. Eleven percent of patients with NOD2 WT status were refractory to treatment with TNF-α antagonists. Fifty-seven percent of patients with NOD2 variants were sensitive to TNF-α antagonists, and 43% of patients with NOD2 variants were refractory to TNF-α antagonists (Fig. 1).
All together, our results demonstrate that CD patients with NOD2 WT status differ in response to standards of medication as compared to NOD2 carriers.
Discussion
Treatment algorithms and the drug history in CD in dependence on the NOD2 mutation carrier status have not yet been investigated. We have shown that patients with CD and NOD2 carrier status were more refractory for steroids but could be treated well with immunosuppressives. The patients with WT NOD2 status, who were steroid-dependent, showed a significantly lower response to treatment with immunomodulators (AZA/6-MP).
In our patients, more CD patients with NOD2 variants were refractory to treatment with budesonide and/or prednisolone. In a multivariate logistic regression model, treatment success with prednisolone was independent of disease localization (ileal site), stricturing or internal fistulizing disease behavior, and the need for surgery. Another study could not find an association of NOD2 carrier status and response to steroids [29]. In contrast to the study of Weiss et al., median age of disease is >18 years in our study cohort. Carrying out the analysis of treatment responses in dependence of NOD2 variants may differ significantly between patient cohorts with pediatric and adult CD patients.
Associations between polymorphism in the TNF-α gene, but not in the multidrug resistance gene 1 (MDR-1), and response to treatment with steroids has been described in an Italian pediatric IBD cohort [30]. High expression of glucocorticoid receptors by mononuclear cells in the peripheral blood of CD patients may predict the response to treatment with steroids [31]. Data of glucocorticoid receptor expression of CD patients with or without NOD2 mutation carrier status are still missing. In patients receiving TNF-α antagonists gene expression profiling and IL-23R variants may predict treatment response to TNF-α antagonists [32, 33]. It might be possible that patients with a reduced glucorticoid receptor expression could have benefited from early combination therapy with immunosuppressants [12].
In our study, CD patients with NOD2 WT status responded to steroids. The percentage of patients with NOD2 WT status refractory to budesonide or prednisolone was decreased as compared to patients with NOD2 carrier status.
More patients with NOD2 carrier status were treated with AZA/6-MP, and the percentage of patients going into remission under treatment with AZA/6-MP was increased as compared to patients with NOD2 WT status. AZA/6-MP metabolites and TPMT activity were not detected on a routine basis in our study [34, 35]. Because most patients received remission under treatment with AZA/6-MP, the discrepancy between patients with NOD2 WT status and patients with NOD2 variants may be associated with genetic and biochemical factors that need to be defined in future studies.
The AZA/6-MP refractory patients with NOD2 WT showed response to TNF-α antagonists. Several studies have investigated the influence of NOD2 polymorphism on response to TNF-α antagonists. NOD2 polymorphism is not predictive for the outcome of treatment with infliximab [36, 37]. We included in our study patients treated with infiximab and adalimumab which may explain differences to previous studies.
NOD2 carriers are characterized by early onset of CD associated with strictures and penetrating disease behavior and increased need for surgery as previously reported [38–40]. In our patients, NOD2 carriers are characterized by early onset of disease, but increased need for surgery could not be confirmed.
Disease phenotype and location are considered to predict disabling disease. Young age, smoking habits, perianal lesions and severe ulcerations are clinical predictors of risk for progressive disease [15, 41]. All treatment regimens in our study were chosen by an algorithmic approach based on national guidelines [27]. Selection of medication depended on the interpretation of the clinical data by the individual physician blinded to the NOD2 genotype status.
Interpretation of the results of our study is limited by the facts that analysis of remission rates depending on treatment regimen was carried out in a retrospective manner, and not in a prospective controlled clinical trial at a single IBD study center only, and not in a multicentre approach. In our study with a limited sample size, a replication cohort is missing. Carrying out genome-wide association studies (GWAS) could be particularly interesting to identify additional variants associated with disease behavior and response to treatment with standard medication.
The task to choose the right medication for an individual IBD patient will likely become more complex in future. Although the prediction of treatment response by phenotype, genotype and serological parameters is still in its infancy, the individual choice of the treatment regimen may help to maximize efficacy, minimize delays to effective treatment, and improve safety and tolerability.
In conclusion, our data show that CD patients without NOD2 mutations suffering from a steroid-dependent or refractory course have significantly less chance to reach steroid-free remission by a treatment with immunosuppressive agents as compared to CD patients with NOD2 mutations, which was independent disease localization (ileal site), stricturing or internal fistulizing disease behavior, and the need for surgery. Otherwise, these NOD2 WT status patients were very sensitive to anti-TNF-α antibodies and all patients reached steroid-free remission. Although this group of patients was small in our study, our results give a first hint that a top-down therapy strategy could be effective especially in these patients. Further studies are needed to prove this concept. This could be an important step toward a personalized therapy in CD patients.
Acknowledgments
We would like to thank Guido Adler for continuous support. The technical support by Julia Geitner, Jana Berthold and Nathalie Birth is greatly acknowledged.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- 6-MP
6-Mercaptopurine
- AZA
Azathioprine
- CARD
Caspase recruitment domain
- CD
Crohn′s disease
- CDAI
Crohn′s disease activity index
- IBD
Inflammatory bowel disease
- NOD
Nucleotide oligomerization domain
- SNP
Single-nucleotide polymorphism
- TNF
Tumor necrosis factor
- WT
Wildtype
Footnotes
Jan Hendrik Niess and Jochen Klaus contributed equally to this work.
References
- 1.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 2.Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009;361:2066–2078. doi: 10.1056/NEJMra0804647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Summers RW, Switz DM, Sessions JT, Jr, Becktel JM, Best WR, Kern F, Jr, Singleton JW. National Cooperative Crohn’s Disease Study: results of drug treatment. Gastroenterology. 1979;77:847–869. [PubMed] [Google Scholar]
- 4.Malchow H, Ewe K, Brandes JW, Goebell H, Ehms H, Sommer H, Jesdinsky H. European Cooperative Crohn’s Disease Study (ECCDS): results of drug treatment. Gastroenterology. 1984;86:249–266. [PubMed] [Google Scholar]
- 5.Faubion WA, Jr, Loftus EV, Jr, Harmsen WS, Zinsmeister AR, Sandborn WJ. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001;121:255–260. doi: 10.1053/gast.2001.26279. [DOI] [PubMed] [Google Scholar]
- 6.Rutgeerts PJ. Review article: the limitations of corticosteroid therapy in Crohn’s disease. Aliment Pharmacol Ther. 2001;15:1515–1525. doi: 10.1046/j.1365-2036.2001.01060.x. [DOI] [PubMed] [Google Scholar]
- 7.Candy S, Wright J, Gerber M, Adams G, Gerig M, Goodman R. A controlled double blind study of azathioprine in the management of Crohn’s disease. Gut. 1995;37:674–678. doi: 10.1136/gut.37.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markowitz J, Grancher K, Kohn N, Lesser M, Daum F. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn’s disease. Gastroenterology. 2000;119:895–902. doi: 10.1053/gast.2000.18144. [DOI] [PubMed] [Google Scholar]
- 9.Feagan BG, Fedorak RN, Irvine EJ, Wild G, Sutherland L, Steinhart AH, Greenberg GR, Koval J, Wong CJ, Hopkins M, et al. A comparison of methotrexate with placebo for the maintenance of remission in Crohn’s disease. North American Crohn’s Study Group Investigators. N Engl J Med. 2000;342:1627–1632. doi: 10.1056/NEJM200006013422202. [DOI] [PubMed] [Google Scholar]
- 10.D’Haens G, Baert F, van Assche G, Caenepeel P, Vergauwe P, Tuynman H, De Vos M, van Deventer S, Stitt L, Donner A, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn’s disease: an open randomised trial. Lancet. 2008;371:660–667. doi: 10.1016/S0140-6736(08)60304-9. [DOI] [PubMed] [Google Scholar]
- 11.Toruner M, Loftus EV, Jr, Harmsen WS, Zinsmeister AR, Orenstein R, Sandborn WJ, Colombel JF, Egan LJ. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008;134:929–936. doi: 10.1053/j.gastro.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 12.Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, Lichtiger S, D’Haens G, Diamond RH, Broussard DL, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362:1383–1395. doi: 10.1056/NEJMoa0904492. [DOI] [PubMed] [Google Scholar]
- 13.Schmidt C, Giese T, Hermann E, Zeuzem S, Meuer SC, Stallmach A. Predictive value of mucosal TNF-alpha transcripts in steroid-refractory Crohn’s disease patients receiving intensive immunosuppressive therapy. Inflamm Bowel Dis. 2007;13:65–70. doi: 10.1002/ibd.20012. [DOI] [PubMed] [Google Scholar]
- 14.Lakatos L, Mester G, Erdelyi Z, Balogh M, Szipocs I, Kamaras G, Lakatos PL. Striking elevation in incidence and prevalence of inflammatory bowel disease in a province of western Hungary between 1977–2001. World J Gastroenterol. 2004;10:404–409. doi: 10.3748/wjg.v10.i3.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650–656. doi: 10.1053/j.gastro.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 16.Franke A, McGovern DP, Barrett JC, Wang K, Radford-Smith GL, Ahmad T, Lees CW, Balschun T, Lee J, Roberts R, et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat Genet. 2010;42:1118–1125. doi: 10.1038/ng.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newman B, Siminovitch KA. Recent advances in the genetics of inflammatory bowel disease. Curr Opin Gastroenterol. 2005;21:401–407. [PubMed] [Google Scholar]
- 18.Kobayashi KS, Chamaillard M, Ogura Y, Henegariu O, Inohara N, Nunez G, Flavell RA. Nod2-dependent regulation of innate and adaptive immunity in the intestinal tract. Science. 2005;307:731–734. doi: 10.1126/science.1104911. [DOI] [PubMed] [Google Scholar]
- 19.Girardin SE, Boneca IG, Viala J, Chamaillard M, Labigne A, Thomas G, Philpott DJ, Sansonetti PJ. Nod2 is a general sensor of peptidoglycan through muramyl dipeptide (MDP) detection. J Biol Chem. 2003;278:8869–8872. doi: 10.1074/jbc.C200651200. [DOI] [PubMed] [Google Scholar]
- 20.Hugot JP, Chamaillard M, Zouali H, Lesage S, Cezard JP, Belaiche J, Almer S, Tysk C, O’Morain CA, Gassull M, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 21.Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, Britton H, Moran T, Karaliuskas R, Duerr RH, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 22.Hampe J, Cuthbert A, Croucher PJ, Mirza MM, Mascheretti S, Fisher S, Frenzel H, King K, Hasselmeyer A, MacPherson AJ, et al. Association between insertion mutation in NOD2 gene and Crohn’s disease in German and British populations. Lancet. 2001;357:1925–1928. doi: 10.1016/S0140-6736(00)05063-7. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad T, Armuzzi A, Bunce M, Mulcahy-Hawes K, Marshall SE, Orchard TR, Crawshaw J, Large O, de Silva A, Cook JT, et al. The molecular classification of the clinical manifestations of Crohn’s disease. Gastroenterology. 2002;122:854–866. doi: 10.1053/gast.2002.32413. [DOI] [PubMed] [Google Scholar]
- 24.Brant SR, Picco MF, Achkar JP, Bayless TM, Kane SV, Brzezinski A, Nouvet FJ, Bonen D, Karban A, Dassopoulos T, et al. Defining complex contributions of NOD2/CARD15 gene mutations, age at onset, and tobacco use on Crohn’s disease phenotypes. Inflamm Bowel Dis. 2003;9:281–289. doi: 10.1097/00054725-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Lesage S, Zouali H, Cezard JP, Colombel JF, Belaiche J, Almer S, Tysk C, O’Morain C, Gassull M, Binder V, et al. CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. Am J Hum Genet. 2002;70:845–857. doi: 10.1086/339432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hisamatsu T, Suzuki M, Reinecker HC, Nadeau WJ, McCormick BA, Podolsky DK. CARD15/NOD2 functions as an antibacterial factor in human intestinal epithelial cells. Gastroenterology. 2003;124:993–1000. doi: 10.1053/gast.2003.50153. [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann JC, Preiss JC, Autschbach F, Buhr HJ, Hauser W, Herrlinger K, Hohne W, Koletzko S, Krieglstein CF, Kruis W, et al. Clinical practice guideline on diagnosis and treatment of Crohn’s disease. Z Gastroenterol. 2008;46:1094–1146. doi: 10.1055/s-2008-1027796. [DOI] [PubMed] [Google Scholar]
- 28.Seiderer J, Dambacher J, Leistner D, Tillack C, Glas J, Niess JH, Pfennig S, Jurgens M, Muller-Myhsok B, Goke B, et al. Genotype-phenotype analysis of the CXCL16 p.Ala181Val polymorphism in inflammatory bowel disease. Clin Immunol. 2008;127:49–55. doi: 10.1016/j.clim.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 29.Weiss B, Lebowitz O, Fidder HH, Maza I, Levine A, Shaoul R, Reif S, Bujanover Y, Karban A. Response to medical treatment in patients with Crohn’s disease: the role of NOD2/CRAD15, disease phenotype, and age of diagnosis. Dig Dis Sci. 2010;55:1674–1680. doi: 10.1007/s10620-009-0936-8. [DOI] [PubMed] [Google Scholar]
- 30.Cucchiara S, Latiano A, Palmieri O, Canani RB, D’Inca R, Guariso G, Vieni G, De Venuto D, Riegler G, De’Angelis GL, et al. Polymorphisms of tumor necrosis factor-alpha but not MDR1 influence response to medical therapy in pediatric-onset inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007;44:171–179. doi: 10.1097/MPG.0b013e31802c41f3. [DOI] [PubMed] [Google Scholar]
- 31.Towers R, Naftali T, Gabay G, Carlebach M, Klein A, Novis B. High levels of glucocorticoid receptors in patients with active Crohn’s disease may predict steroid resistance. Clin Exp Immunol. 2005;141:357–362. doi: 10.1111/j.1365-2249.2005.02846.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Toedter G, Li K, Marano C, Ma K, Sague S, Huang CC, Song XY, Rutgeerts P, Baribaud F. Gene expression profiling and response signatures associated with differential responses to infliximab treatment in ulcerative colitis. Am J Gastroenterol. 2011;106:1272–1280. doi: 10.1038/ajg.2011.83. [DOI] [PubMed] [Google Scholar]
- 33.Jurgens M, Laubender RP, Hartl F, Weidinger M, Seiderer J, Wagner J, Wetzke M, Beigel F, Pfennig S, Stallhofer J, et al. Disease activity, ANCA, and IL23R genotype status determine early response to infliximab in patients with ulcerative colitis. Am J Gastroenterol. 2010;105:1811–1819. doi: 10.1038/ajg.2010.95. [DOI] [PubMed] [Google Scholar]
- 34.Cuffari C, Dassopoulos T, Turnbough L, Thompson RE, Bayless TM. Thiopurine methyltransferase activity influences clinical response to azathioprine in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2004;2:410–417. doi: 10.1016/S1542-3565(04)00127-2. [DOI] [PubMed] [Google Scholar]
- 35.Dubinsky MC, Yang H, Hassard PV, Seidman EG, Kam LY, Abreu MT, Targan SR, Vasiliauskas EA. 6-MP metabolite profiles provide a biochemical explanation for 6-MP resistance in patients with inflammatory bowel disease. Gastroenterology. 2002;122:904–915. doi: 10.1053/gast.2002.32420. [DOI] [PubMed] [Google Scholar]
- 36.Vermeire S, Louis E, Rutgeerts P, De Vos M, Van Gossum A, Belaiche J, Pescatore P, Fiasse R, Pelckmans P, Vlietinck R, et al. NOD2/CARD15 does not influence response to infliximab in Crohn’s disease. Gastroenterology. 2002;123:106–111. doi: 10.1053/gast.2002.34172. [DOI] [PubMed] [Google Scholar]
- 37.Mascheretti S, Hampe J, Croucher PJ, Nikolaus S, Andus T, Schubert S, Olson A, Bao W, Folsch UR, Schreiber S. Response to infliximab treatment in Crohn’s disease is not associated with mutations in the CARD15 (NOD2) gene: an analysis in 534 patients from two multicenter, prospective GCP-level trials. Pharmacogenetics. 2002;12:509–515. doi: 10.1097/00008571-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Seiderer J, Schnitzler F, Brand S, Staudinger T, Pfennig S, Herrmann K, Hofbauer K, Dambacher J, Tillack C, Sackmann M, et al. Homozygosity for the CARD15 frameshift mutation 1007fs is predictive of early onset of Crohn’s disease with ileal stenosis, entero-enteral fistulas, and frequent need for surgical intervention with high risk of re-stenosis. Scand J Gastroenterol. 2006;41:1421–1432. doi: 10.1080/00365520600703900. [DOI] [PubMed] [Google Scholar]
- 39.Seiderer J, Brand S, Herrmann KA, Schnitzler F, Hatz R, Crispin A, Pfennig S, Schoenberg SO, Goke B, Lohse P, et al. Predictive value of the CARD15 variant 1007fs for the diagnosis of intestinal stenoses and the need for surgery in Crohn’s disease in clinical practice: results of a prospective study. Inflamm Bowel Dis. 2006;12:1114–1121. doi: 10.1097/01.mib.0000235836.32176.5e. [DOI] [PubMed] [Google Scholar]
- 40.Henckaerts L, Van Steen K, Verstreken I, Cleynen I, Franke A, Schreiber S, Rutgeerts P, Vermeire S. Genetic risk profiling and prediction of disease course in Crohn’s disease patients. Clin Gastroenterol Hepatol. 2009;7:972.e2–980e2. doi: 10.1016/j.cgh.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 41.Allez M, Lemann M, Bonnet J, Cattan P, Jian R, Modigliani R. Long term outcome of patients with active Crohn’s disease exhibiting extensive and deep ulcerations at colonoscopy. Am J Gastroenterol. 2002;97:947–953. doi: 10.1111/j.1572-0241.2002.05614.x. [DOI] [PubMed] [Google Scholar]