Abstract
Objectives
Community Health Workers (CHWs) have been recommended to reduce diabetes disparities, but few robust trials of this approach have been conducted. Limitations of prior studies include: unspecified a priori outcomes; lack of blinded outcome assessments; high participant attrition rates; and lack of attention to intervention fidelity. These limitations reflect challenges in balancing methodologic rigor with the needs of vulnerable populations. The Mexican-American Trial of Community Health workers (MATCH) was a blinded randomized controlled trial testing CHW efficacy in improving physiologic outcomes and self-management behaviors among Mexican-Americans with type 2 diabetes. This paper describes methods used to overcome limitations of prior studies.
Research Design and Methods
The primary aim was to determine if a CHW intervention would result in significant reductions in Hemoglobin A1c and rates of uncontrolled blood pressure. 144 Mexican-Americans with diabetes were randomized. The intervention consisted of self-management training delivered by CHWs over a 24-month period; the comparison population received identical information via bilingual newsletter. Blinded research assistants completed assessments at baseline, 12 months, and 24 months post-randomization.
Results
The MATCH cohort was characterized by low acculturation and socioeconomic status. Study participants had low rates of medication adherence and glucose monitoring. 70% had poor glycemic control with A1c levels over 7.0, and 57.3% had blood pressures worse than ADA target levels (<130/80).
Conclusions
MATCH preserved community sensitivity and methodologic rigor. The study’s attention to intervention fidelity, behavioral attention control, blinded outcomes assessment, and strategies to enhance participant retention can be replicated by researchers testing culturally-tailored CHW interventions.
Keywords: behavioral clinical trial, community-based research, diabetes self-management, community health workers
Introduction
The past decade has seen a significant rise in the prevalence of diagnosed diabetes mellitus among adults in the US, with adverse impact particularly felt by ethnic minorities and low income populations. Compared to a 6.6% rate among non-Hispanic whites today, the age-adjusted prevalence of diabetes is 11.8% among non-Hispanic blacks, 11.9% among Mexican Americans, and 12.6% among Puerto Ricans (1). Persistent health disparities in diabetes incidence and complications have led to calls for the development of effective interventions for underserved at-risk groups(2, 3). Glazier’s review of interventions to improve diabetes care in socially disadvantaged populations concluded that the most effective interventions were characterized by cultural tailoring, use of lay community educators, individualized treatments, the incorporation of treatment algorithms, a focus on behavior-related tasks, provision of feedback, and a high number of contacts over more than 6 months(4).
The Community Health Worker (CHW) model has garnered great interest in recent years as one such culturally tailored approach towards improving diabetes outcomes. For several decades, CHW programs in the US have hired and trained lay people who live in target communities to provide outreach and health education (5, 6). Although trained and supervised by health professionals, the value of CHWs is believed to lie in the shared experience, language, and/or culture with the communities they serve(7).
Despite their potential to reduce diabetes disparities, CHW interventions have to date had only modest adoption by public and private payers. One barrier to adoption is the paucity of well-designed clinical trials, leading to calls for greater methodologic rigor in the field (6, 8–10). Methodologic limitations may reflect practical challenges in working with vulnerable and underserved communities, in which research processes and external observers may be viewed with suspicion.
This paper describes the design and implementation of the Mexican American Trial of Community Health workers (MATCH), a blinded, behavioral randomized controlled trial to test the efficacy of a CHW intervention in improving diabetes self care and outcomes in a vulnerable minority population. Study design reflected the MATCH investigators’ belief that, despite challenges associated with implementing research in underserved communities, a rigorous study design could be used and cultural sensitivity preserved.
MATCH was developed to test the hypothesis that indigenous CHWs, trained to teach culturally appropriate diabetes self-management skills, could reduce mean levels of Hemoglobin A1c levels, and increase the percent of study participants who achieved target blood pressure at the end of one year, and sustain these improvements at the end of two years. Improvements in three specific self-management behaviors were also assessed: daily self-monitoring of blood glucose, daily medication-taking, and adherence to diet and physical activity recommendations.
Research Design and Methods
Recruitment
MATCH was designed as a single site behavioral randomized efficacy trial based at Rush University Medical Center, with recruitment from several contiguous Mexican-American neighborhoods in Chicago and adjoining suburbs. Recruitment strategies have been previously described(11). 144 persons with type 2 diabetes mellitus were randomized to intervention and attention control conditions. Eligible participants had to be Mexican-American, defined as either having been born in Mexico, or having at least one parent or two grandparents born in Mexico. Because adherence to medications was a major study outcome, assessed using an electronic pill cap device, participants were required to be using at least one oral medication to control their diabetes. To ensure that lack of access to health care services did not pose an insurmountable barrier to diabetes self-management, participants were required to have health insurance or to be enrolled as a patient at a free clinic or public facility at the time of randomization. Exclusions for participation included: active treatment for schizophrenia; inability to provide informed consent; any prior major end-organ complications of diabetes such as end-stage renal disease or stroke; another household member already participating in MATCH; or plans to spend more than four months in Mexico in the next year.
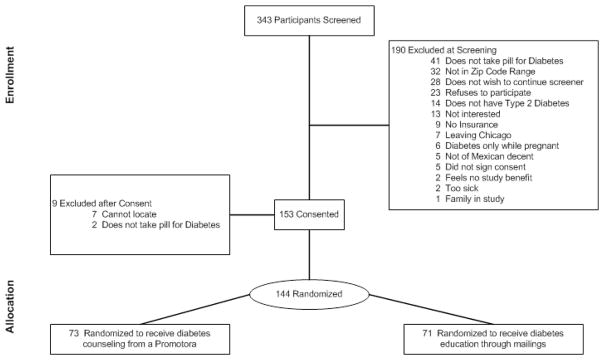
Enrollment for the study was completed over a 35 month period. Patient flow from screening to enrollment is shown in Figure 1. The study had a screening to enrollment ratio of 42%, comparable to other published trials involving Hispanics. In order to test the CHW intervention under real world conditions, no financial or other incentives were offered in exchange for study participation. Recruitment materials, consent documents, and the study protocol were reviewed and approved by the Rush University Institutional Review Board.
FIGURE 1.
Study Design
After giving informed consent, participants underwent baseline evaluations in two separate home visits; twelve participants elected to have these visits conducted in either a community setting or at the Medical Center. During the first visit, the following assessments were completed: demographics, co-morbidities, acculturation (12), health care utilization, the Personal Resource Questionnaire of social support(13), Perceived Discrimination (14), Perceived Stress(15), Spielberger Trait Anxiety(16), Diabetes Empowerment Scale(17), the Summary of Diabetes Self-care Activities(18), the four-item Morisky Medication Adherence Scale(19), the PHQ2 depression screen(20), and the Beck Depression Inventory. Interviews were conducted in the participant’s preferred language, using validated Spanish translations of instruments. Clinical assessments included: height, weight, blood pressure, waist circumference and a blood specimen collected for Hemoglobin A1c.
At the conclusion of the evaluation, a medication bottle with a MEMS electronic monitoring pill cap was given to the participants to use with one of their oral diabetes medications to document daily medication adherence (MEMS 6 Track Cap, AARDEX, Ltd, Switzerland). Thirty days later, a brief second visit was conducted to collect the pill cap; at that visit, the participant’s glucose meter was also examined to determine the number of days in the preceding month on which glucose had been checked at least once.
Upon return of the electronic pill caps to the Data Management Center (DMC), participants were randomized and informed of their group assignment. Participants could not be blinded to which treatment they were receiving, either educational visits by a community health worker or diabetes education via a bilingual newsletter mailed to their home. In order to maintain blinding to the study hypothesis however, participants were told during the consent process that the study was comparing two methods of diabetes self-management education, either a bilingual newsletter with diabetes education for two years, or regular home visits by a CHW over the same period. All recruitment and consent documents preserved equipoise, and indicated that investigators did not know which approach was more effective. At randomization, participants in both arms were reminded that their assigned intervention would provide them with information to help them better manage their diabetes. Participants were informed that a blinded Research Assistant would check in with them by phone every four months, and that home visits would be scheduled at 12 and 24 months post randomization.
Community Health Worker Intervention
The MATCH intervention employed CHWs as culturally-competent peer interventionists to enhance diabetes self-efficacy and increase rates of diabetes self-management behaviors. MATCH CHWs were Mexican-Americans, for whom Spanish was their first language, recruited from the same neighborhoods as study participants. CHW training and evaluation protocols have been described previously(21). The CHWs themselves did not have diagnosed diabetes.
The MATCH curriculum taught seven core diabetes self-management behaviors, developed from the curriculum content recommended by the American Academy of Diabetes Educators, the “AADE-7”(22). In order to help participants overcome barriers and begin to successfully implement these behaviors, the CHWs also coached participants in five general skills: brainstorming and problem-solving; using a journal or written record; modifying the home environment to support behavior change; seeking social support from family or friends; and stress management. Training was based on principles of social cognitive theory positing that individuals will make behavior changes only if they believe that they are capable of organizing and executing the specific behaviors(23). By facilitating problem-solving, providing performance feedback, and coaching participants through repeated efforts at implementing diabetes self-management behaviors, the CHWs were to help participants gain self-efficacy and make sustained changes.
The curriculum was delivered in 36 individual visits, usually in the home of the participants, over a two year period. Individual home visits were selected rather than a group intervention in order to promote behavior changes in the milieu in which those behaviors most often take place. Visits were scheduled twice monthly during the first year (24 visits), and once a month in the second year (12 visits). This number of visits was selected because skill mastery occurs gradually over numerous attempts, and in stages going from acquisition to generalization and ultimately maintenance. Initial visits focused on building a relationship with the participant, with particular emphasis on identifying the participant’s concerns and mastery of basic diabetes knowledge. These visits also introduced self-management techniques and an overview of the curriculum. By the fourth visit, CHWs began to work with one or two specific diabetes self-management issues at a time. Although core content was specified by study protocol, the specific training sequence was not; sequence of content was individualized by the CHW in response to challenges that the participant voiced at the time of the visit. The CHW then coached the participant in using self-management skills to help them successfully implement diabetes self-care behaviors. As the first year progressed, it was anticipated that participants would be better able to apply general skills to improving diabetes self-care. Repeated visits covering the same diabetes self-management behaviors were scheduled during the second year to provide participants with an opportunity to further increase self-efficacy and foster long-term maintenance of the targeted diabetes behaviors.
Intervention fidelity is of critical importance in a behavioral clinical trial. In MATCH, this was ensured by requiring the CHWs to complete a documentation worksheet for each intervention visit. CHWs documented the diabetes behavior that was the primary focus of the visit, and the self-management strategies that were taught. All visits were audiotaped with the consent of the participants, and tapes reviewed by the project psychologist (CL) to ensure that the documentation worksheets were accurate and to provide on-going feedback to CHWs regarding intervention delivery and consistent application of behavioral self-management training techniques. Monthly control reports ensured that each participant received all of the components of the MATCH intervention.
Control Condition
Participants randomized to the control condition received a bilingual newsletter called “DiabetesAction”. Thirty-six newsletters were mailed to control participants on the same schedule as the CHW intervention. Newsletters covered the seven diabetes self-management behaviors, and provided tips to promote problem-solving, social support, environmental restructuring, self-monitoring, and stress management.
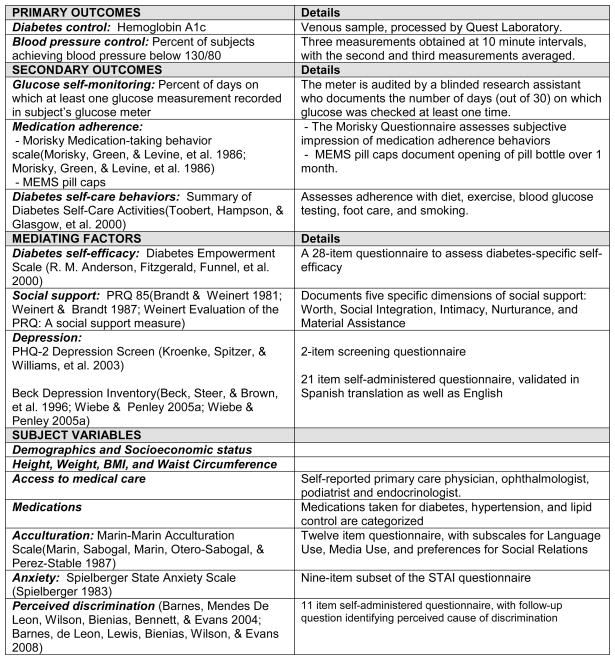
Outcome Assessment
All outcome measures listed in Figure 2 were collected at baseline, and were repeated at 12 and 24 months post-randomization. Research assistants were blinded to participants’ treatment arm, and at each contact they began by emphasizing that the participants were not to make specific reference to any treatment that they were receiving as part of the study. Research assistants had no contact with the CHW interventionists and were not involved in sending out mailings. Although the PI (SKR) and other investigators (MAM, SMS, LHP) interacted with the CHW interventionists in staffings, specific information about individual participants was limited to a single psychologist supervisor (CTL) who was not involved in any assessments of outcomes.
FIGURE 2.
Variables Measured At Time Of Randomization And 1-Year And 2-Year Follow-Up
Retention Plan
MATCH faced several challenges to participant retention that were addressed in study design. The two year duration of the study with in-person exams at 12-month intervals posed particular risk of loss to follow-up. In addition, this low income, immigrant population was at risk of frequent moves due to job loss, eviction, repossession of homes, or return to Mexico for family or economic reasons. To reduce the risk of loss to follow-up, at least three alternative contacts were sought for each participant at the time of enrollment. Research assistants called all study participants at three month intervals to check in, verify contact information, and review any anticipated changes in residence or telephone. If a participant could not be contacted at a quarterly telephone call after several attempts, an aggressive loss to follow-up protocol was initiated to resume contact and ascertain their likely location at the time of the annual evaluation. For participants who left the area, outcome assessments included interview by telephone, use of lab testing from a national reference lab, and physical measures provided by physicians in their new community.
The MATCH protocol also guarded against differential ascertainment. Because of their frequent contact with participants, CHWs would frequently know when and where participants had moved, if they were likely to return to the area, and how to reach them. Because this information would not be equally available for recipients of the control newsletter, it was not conveyed to the research assistants and not used for purposes of retention. Although tempting to use this contact information, to do so would have been to introduce bias through excess ascertainment of outcomes in the CHW group relative to the control group.
Statistical Analysis Plan
In order to fully utilize data to detect differences in change of Hemoglobin A1c over time between the treatment and control groups, a repeated measures analysis of variance with one repeated factor will be used with time, treatment group and time by treatment group interaction as the variables of interest. If the data are skewed, then data transformations and non-parametric tests may be utilized. Continuous secondary outcomes will be examined using a similar approach. Categorical variables will be analyzed using a logistic mixed model. Analyses of treatment efficacy are planned for pre-specified subgroups, identified at baseline, which include age, gender, and acculturation. For these analyses, interaction terms (subgroup × treatment) will be evaluated in multivariate modeling that includes the interaction and its main effects.
If the MATCH intervention demonstrates improvements in A1c and blood pressure relative to the control, cost-effectiveness will be assessed. Costs associated with the intervention including CHW time and all training and supervisory time were documented and provide a basis for determining program costs. Opportunity costs for participants will be estimated by multiplying intervention time by published mean rates adjusted for age and gender. Health care utilization documented during the study includes self-reported physician utilization, hospitalizations, and medication usage. Program, opportunity, and utilization costs will be similarly determined for the control group, and subtracted from the estimated intervention costs.
Findings/Baseline Characteristics
As shown in Tables 1 and 2, randomization was largely successful in that the intervention and control groups did not differ significantly in demographic or clinical variables. For outcome measures, the intervention group had somewhat higher baseline Hemoglobin A1c and blood pressure than the control group, but only the differences in diastolic blood pressure (72.5 mm Hg vs 69.2mmg Hg) was statistically significant (p=0.02).
TABLE 1.
DEMOGRAPHIC CHARACTERISTICS OF PARTICIPANTS
| Measures | Overall N = 144 |
Intervention N =73 |
Control N =71 |
p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years), mean(std)§ | 53.7 (12.2) | 53.7 (11.7) | 53.6 (12.7) | 0.97 |
| Female, N(%)* | 97 (67.4) | 47 (64.4) | 50 (70.4) | 0.60 |
| Education, N(%)* | 0.88 | |||
| Less than Elementary School (≤5 yrs) | 48 (33.3) | 24 (32.9) | 24 (33.8) | |
| Elementary School (6 yrs) | 33 (22.9) | 158 (24.7) | 15 (21.1) | |
| Some High School (7–11 yrs) | 22 (15.3) | 11 (15.1) | 11 (15.5) | |
| High school or equivalent (12 yrs) | 30 (20.8) | 16 (21.9) | 14 (19.7) | |
| Some college (≥ 13 yrs) | 11 (7.6) | 4 (5.5) | 7 (9.9) | |
| Marital Status, N(%)* | 0.54 | |||
| Married/Common Law Marriage | 94 (65.3) | 44 (60.3) | 50 (70.4) | |
| Separated/Divorced | 19 (13.2) | 12 (16.4) | 7 (9.9) | |
| Widowed | 12 (8.3) | 6 (8.2) | 6 (8.5) | |
| Never married | 19 (13.2) | 11 (15.1) | 8 (11.3) | |
|
| ||||
| Economic | ||||
| Difficulty paying for basics, N(%)* | 0.23 | |||
| Very hard | 31 (24.0) | 12 (18.8) | 19 (29.2) | |
| Somewhat hard | 61 (47.3) | 30 (46.9) | 31 (47.7) | |
| Not hard at all | 37 (28.7) | 22 (34.4) | 15 (40.5) | |
| Insurance Status, N(%)* | 0.89 | |||
| Private | 41 (29.9) | 22 (31.4) | 19 (28.4) | |
| Medicare | 18 (13.1) | 8 (11.4) | 10 (14.9) | |
| Medicaid | 16 (11.7) | 9 (12.9) | 7 (10.5) | |
| None | 62 (45.3) | 31 (44.3) | 31 (46.3) | |
|
| ||||
| Acculturation | ||||
| Acculturation Score, mean(std)*^ | 1.6 (0.8) | 1.6 (0.8) | 1.6 (0.8) | 0.98 |
| Preferred Language: Spanish, N(%)* | 130 (90.3) | 67 (91.7) | 63 (88.7) | 0.52 |
| Born In Mexico, N(%)+ | 134 (93.1) | 65 (89.0) | 69 (97.2) | 0.10 |
p-value from unequal variance t-test
p-value from chi-square test
p-value from fisher’s exact test
Ranges from 1 (low acculturation)-5 (high acculturation)
TABLE 2.
CLINICAL CHARACTERISTICS OF PARTICIPANTS
| Measure | Overall N = 144 |
Intervention N =73 |
Control N =71 |
p-value |
|---|---|---|---|---|
| Body Mass Index (BMI) | ||||
| Continuous, mean (std)§ | 33.4 (8.5) | 32.7 (7.4) | 34.2 (9.5) | 0.60 |
| Categorized, N (%)* | 0.65 | |||
| Normal weight (18.5 – 25.0) | 20 (14.1) | 10 (13.7) | 10 (14.5) | |
| Overweight (25.0 – 29.9) | 35 (24.7) | 20 (27.4) | 15 (21.7) | |
| Class I Obesity (30.0 – 34.9) | 40 (28.2) | 19 (26) | 21 (30.4) | |
| Class II Obesity (35.0 – 39.9) | 21 (14.8) | 13 (17.8) | 8 (11.6) | |
| Class III Obesity (≥ 40.0) | 26 (18.3) | 11 (15.1) | 15 (21.7) | |
|
| ||||
| Hemoglobin A1c | ||||
| Continuous, mean(std)§ | 8.3 (2.0) | 8.5 (2.2) | 8.1 (1.6) | 0.25 |
| Categorized, N(%)* | 0.30 | |||
| <7.0 | 42 (30.0) | 24 (33.8) | 18 (26.1) | |
| 7.0 – 9.0 | 52 (37.1) | 22 (31.0) | 30 (43.5) | |
| >9.0 | 46 (32.9) | 25 (35.2) | 21 (30.4) | |
|
| ||||
| Blood Pressure (BP) | ||||
| Self Reported Hypertension, N(%)* | 87 (60.4) | 49 (67.1) | 38 (53.5) | 0.10 |
| Systolic BP mm HG, mean(std)§ | 131.7 (14.9) | 133.6 (16.5) | 129.7 (12.9) | 0.25 |
| Diastolic BP mm HG, mean(std)§ | 70.8 (10.2) | 72.5 (8.5) | 69.2 (11.5) | 0.02 |
| Uncontrolled Hypertension (≥ 130/80), N(%)* | 82 (56.9) | 44 (60.3) | 38 (53.5) | 0.41 |
|
| ||||
| Medical Management | ||||
| On Oral Diabetic Agent, N(%)* | 144 (100.0) | 73 (100.0) | 71 (100.0) | >0.99 |
| On Insulin, N (%)* | 23 (16.0) | 14 (19.2) | 9 (12.7) | 0.29 |
| On ACE-inhibitor or ARB, N(%)* | 67 (46.5) | 29 (39.7) | 38 (53.5) | 0.14 |
| Total # of medications, mean(std)§ | 4.8 (2.9) | 4.5 (2.7) | 5.1 (3.0) | 0.21 |
|
| ||||
| Self- Management Behaviors | ||||
| Used glucose meter in past 30 days, N(%)* | 85 (86.7) | 44 (89.8) | 41 (83.7) | 0.37 |
| Checked Glucose ≥ 5 out of 10 days, N(%)* | 58 (45.0) | 30 (46.9) | 28 (43.1) | 0.67 |
| Self Reported days in the last week: | ||||
| Blood glucose checked, mean(std)§ | 2.8 (3.0) | 2.5 (3.1) | 3.2 (3.0) | 0.13 |
| Adhered to diabetic diet, mean(std)§ | 3.6 (2.7) | 3.4 (2.7) | 3.8 (2.8) | 0.43 |
| Some physical activity, mean(std)§ | 1.8 (1.9) | 1.6 (1.7) | 1.9 (2.1) | 0.38 |
| Morisky Med Adherence Measure, mean(std)*^ | 1.2 (1.1) | 1.2 (1.0) | 1.3 (1.1) | 0.56 |
| Taking diabetes medications >80% of time as measured by pillcap openings, N(%)* | 63 (44.1) | 32 (44.4) | 31 (43.7) | 0.92 |
p-value from unequal variance t-test
p-value from chi-square test
Ranges from 0 (high adherence)-4 (low adherence)
Demographic characteristics of participants shown in Table 1 are presented as mean and SD, or as a percentage. At the start of the trial, the mean age for participants was 53.7 years. 67.4% of the population was female, and 65.3% were married. The MATCH cohort was of very low level of acculturation; 93% were born in Mexico, and for over 90%, Spanish remained their preferred language. The population was of lower socioeconomic and educational status, and experienced barriers to specialty health care services. 74% of the sample had not completed high school (or equivalent), and over 70% reported that it is “somewhat” or “very hard” to pay for basic needs. Although all participants had a source of primary care, only 25% reported having ever seen an ophthalmologist, and only 9% had ever seen a podiatrist. None reported having ever been treated by an endocrinologist.
Clinical characteristics are shown in Table 2. The cohort was characterized by a high rate of overweight and obesity, with a mean BMI of 33.4, and over 18% having a BMI classified as Obese Class III or Morbid Obesity (≥40). The American Diabetes Association has set a standard for diabetes care of reducing Hemoglobin A1c levels to less than 7.0. At baseline, mean A1c was 8.29, and 70% of the cohort had Hemoglobin A1c levels exceeding 7.0 as compared with 58% in NHANES (24). 32.9% of the cohort had A1c levels larger than 9.0 as compared to 21% of NHANES respondents. Only 42.7% of participants had blood pressures at target levels set by national guidelines, below 130/80, modestly better than the rate of 35.8% reported for the general population of persons with diabetes(24). Medication review indicated that 46% were taking either an ACE-Inhibitor or ARB in accordance with practice guidelines; this number was slightly higher in the control group. Participants were taking a mean of 4.8 medications, including over-the-counter and prescribed, for all conditions.
With regard to self-reported diabetes self-management behaviors, study participants reported monitoring their blood glucose levels on average only 2.8 days per week, and this was verified by review of glucose monitors in which only. As documented by pill cap openings, only 44% of participants took their medication on 80% of days. The Summary of Diabetes Self-Care Activities(18), a survey assessing daily adherence with various behaviors (with each behavior reported on range from 0 to 7 days in the past week) documented low adherence with diet and exercise; participants reported dietary adherence only half the time (an average of 3.6 days per week), and infrequent physical activity (1.8 days per week). Consistent with other studies of low acculturation Mexican Americans, smoking was infrequent in the MATCH cohort; only 6.9% reported having smoked a cigarette in the past week.
Discussion
Despite decades of CHW programs in the US and the enthusiasm of those who have worked with CHWs, few controlled trials have been conducted to determine their effectiveness. Thus, widespread adoption of the CHW model has been hindered by lack of strong evidence. The purpose of the MATCH trial was to provide a rigorous test of the effectiveness of a CHW intervention in increasing diabetes self-management behaviors and improving physiologic outcome measures (Hemoglobin A1c and Blood Pressure) in a vulnerable minority population.
The demographics and clinical characteristics of the MATCH cohort document a well-defined health disparity population with challenges similar to those of many low-income minority communities. Mexican-Americans experience disparities in both diabetes self-care and health outcomes, and this was reflected in our study sample. They also faced language, cultural, and socioeconomic barriers to health care, which CHWs are well-suited to address. The MATCH cohort, characterized by low acculturation, high rates of overweight and obesity, low rates of glycemic control, and limited access to evidence-based diabetes care, was representative of a highly vulnerable, health disparity community.
More research is needed in vulnerable populations that suffer some of the highest rates of chronic illness. Implementation of this research has been impeded by challenges of recruitment and methodological rigor in these vulnerable populations who are typically unfamiliar with the research process and often disenfranchised from the mainstream medical system. Additionally, the application of standard rigorous trial methods presents unique challenges when the intervention being tested is behavioral, compared to pharmaceutical or procedural. The MATCH study succeeds in achieving methodological rigor that is fully compatible with sensitivity to a vulnerable community experiencing major health and social disparities. Specifically, the design of this trial provides solutions to the previously described methodological limitations from prior CHW studies (6, 8–10):
Clear conceptual intervention model
The MATCH intervention meets many of the criteria established by Glazier for effective diabetes interventions with minority populations(Glazier, Bajcar, Kennie, et al. 2006). It provided a culturally tailored intervention, delivered by lay community health workers, through individualized sessions focusing on behavior change. Treatment was grounded in established literature on self-management(23). The intervention was of high intensity over a prolonged period in an effort to achieve significant, sustained change.
Clearly stated hypotheses with outcomes defined a priori
The primary study hypothesis was that when compared to an attention control group, the MATCH CHW intervention group would achieve significant reductions in Hemoglobin A1c and in the percentage of persons with uncontrolled hypertension. These outcomes were chosen because of their contribution to the risk of diabetes complications. For example, a 1.0% reduction in Hemoglobin A1c levels would correspond with an anticipated 30% reduction in rate of microvascular complications.
Defined study population drawn from community
The study population in MATCH was recruited from an urban community sample, not dependent on a single clinic or health system. Baseline data documented a vulnerable population with low socioeconomic status and lower levels of acculturation. These characteristics support the external validity of the trial, and make findings generalizable to a broad range of urban dwelling Mexican-Americans.
Attention to intervention fidelity
The CHW literature has been limited by lack of standardization in intervention and delivery. In contrast, MATCH has carefully documented CHW recruitment and training(21), and delivered protocol-defined diabetes self-management content, consistent with the standards of the American Association of Diabetes Educators. Teaching content and self-management tools were documented at every visit by the CHWs, and subsequently verified by review of audiotapes by one of the investigators (CTL). Audiotaping allowed investigators to verify both accuracy of diabetes content and appropriateness of the behavioral intervention. Monthly control reports further enhanced treatment fidelity.
Although the MATCH intervention was highly prescriptive regarding content and goal setting, the intervention also allowed customization to meet the needs of each individual participant. CHWs were thus able to sequence content to address the concerns of a participant at a given time. In addition, the intervention recognized that participants face a wide variety of psychosocial challenges, and CHWs were encouraged to provide support around issues other than diabetes.
Use of a behavioral attention control
The MATCH newsletter control condition delivered the same informational content, with the same frequency and duration as the CHW intervention. This approach masked the study hypothesis from participants, and helped preserve blinding. It also fulfilled an ethical need to not withhold basic health information from a vulnerable population that might otherwise lack access to that education. This control increased the likelihood that any improvements that may be found in the intervention group will be the direct result of the CHW themselves and not solely attributable to information content.
Blinded outcome assessment
In many published CHW studies, the CHWs themselves collect outcome measures on participants. MATCH used blinded Research Assistants who completed all measurements and surveys. Although participants in this behavioral clinical trial could not be blinded to which intervention they received, they were blinded to the study hypothesis, and during randomization and subsequent evaluation visits they were advised not to indicate the type of intervention to which they had been assigned. In addition, Hemoglobin A1c levels were reported by an outside reference lab, and were thus unaffected by inadvertent knowledge of group assignment.
Strategies to enhance participant retention
Working with an immigrant population, the MATCH trial faced several challenges regarding participant retention. Investigators excluded participation by individuals who indicated a likelihood to leave the US for long periods, in order to improve retention over a two year period. Multiple contacts were identified for each participant, as well as contact information for their health care providers. Quarterly phone calls to all participants, along with birthday and holiday cards, helped reduce drop-out and loss to follow-up in both intervention and control arms, and reduced risk of differential ascertainment between the two groups.
Limitations
When outcomes data are analyzed, the MATCH study will determine the efficacy of CHWs in delivering a diabetes self-management intervention to a generalizable, urban, Mexican-American population. This trial can not provide a definitive answer to the question of whether the MATCH intervention will have similar outcomes in other ethnic and racial communities, nor will it be able to establish the ability of CHWs to deliver other clinical interventions. Replication will be needed, as well as additional trials to determine retention of behavior changes post-intervention.
If the MATCH CHW intervention is effective in reducing Hemoglobin A1c and blood pressure levels and in increasing self-management in this population, the findings will have importance for reducing diabetes morbidity and mortality in vulnerable populations. Regardless of the outcomes of the trial, the MATCH study design provides a framework for rigorously testing culturally-tailored CHW interventions that could address the challenge of growing diabetes health disparities.
Acknowledgments
The design, development, and implementation of the MATCH study, and the work described in this paper, would not have been possible without the efforts of promotoras Pilar Gonzalez, Susana Leon, Maria Sanchez, and the staff of Centro San Bonifacio. Estamos agradecidos.
Footnotes
Author Contributions
Authors SKR, MSM, SMS, and LHP (all from Rush University Medical Center), and CTL (private practice): design and implementation of the trial, writing and editorial assistance on the manuscript. Authors EFA and IJ (Rush University Medical Center): implementation, statistical analysis, editorial assistance.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Steven K. Rothschild, Departments of Preventive Medicine and Family Medicine, Rush University Medical Center, 1700 W. Van Buren, Suite 470, Chicago, IL 60612.
Molly A. Martin, Department of Preventive Medicine, Rush University Medical Center, Chicago, IL 60612.
Susan M. Swider, College of Nursing, Rush University Medical Center, Chicago, IL 60612.
Carmen T. Lynas, Carmen Lynas Psychotherapy, Oak Brook, IL 60523.
Elizabeth F. Avery, Department of Preventive Medicine, Rush University Medical Center, Chicago, IL 60612.
Imke Janssen, Department of Preventive Medicine, Rush University Medical Center, Chicago, IL 60612.
Lynda H. Powell, Department of Preventive Medicine, Rush University Medical Center, Chicago, IL 60612.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: General information and national estimates on diabetes in the united states, 2007. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 2.Caballero AE. Type 2 diabetes in the hispanic or latino population: Challenges and opportunities. Current Opinion in Endocrinology, Diabetes & Obesity. 2007 Apr;14(2):151–7. doi: 10.1097/MED.0b013e32809f9531. [DOI] [PubMed] [Google Scholar]
- 3.Coronado GD, Thompson B, Tejeda S, Godina R. Attitudes and beliefs among mexican americans about type 2 diabetes. Journal of Health Care for the Poor & Underserved. 2004 Nov;15(4):576–88. doi: 10.1353/hpu.2004.0057. [DOI] [PubMed] [Google Scholar]
- 4.Glazier RH, Bajcar J, Kennie NR, Willson K. A systematic review of interventions to improve diabetes care in socially disadvantaged populations YR 2006 FD july JF JO SP 1675 OP 1688 DO 10.2337/dc05-1942 VO 29 IS 7 UL. AB Diabetes Care. 2006 July;29:1675–88. doi: 10.2337/dc05-1942. http://care.diabetesjournals.org/content/29/7/1675.abstract. [DOI] [PubMed]
- 5.Rosenthal EL. A summary of the national community health advisor study. Baltimore: Annie E. Casey Foundation; 1998. [Google Scholar]
- 6.Swider SM. Outcome effectiveness of community health workers: An integrative literature review. Public Health Nursing. 2002 January/February;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 7.Love M, Gardner K, VL Community health workers: Who they are and what they do. Health Education and Behavior. 1997;24(4):510–22. doi: 10.1177/109019819702400409. [DOI] [PubMed] [Google Scholar]
- 8.Viswanathan M, Kraschnewski J, Nishikawa B, Morgan LC, Thieda P, Honeycutt A, et al. Outcomes of community health worker interventions. evidence report/technology assessment no. 181. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [PMC free article] [PubMed] [Google Scholar]
- 9.Norris SL, Chowdhury FM, VanLet K, Brownstein JN, Zhang X, Jack L, Jr, et al. Effectiveness of community health workers in the care of persons with diabetes. Diabetic Medicine. 2006;23:544–56. doi: 10.1111/j.1464-5491.2006.01845.x. [DOI] [PubMed] [Google Scholar]
- 10.Lewin S, Dick J, Pond P, Zwarenstein M, Aja GN, van Wyk BE, et al. Lay health workers in primary and community health care. Cochrane Database of Systematic Reviews. 2005;(1) doi: 10.1002/14651858.CD004015.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Martin MA, Swider SM, Olinger T, Avery E, Tumialan Lynas CM, Carlson K, et al. Recruitment of mexican-american adults for an intensive diabetes intervention trial. Ethn Dis. 2011;21 In Press. [PMC free article] [PubMed] [Google Scholar]
- 12.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for hispanics. Hispanic Journal of Behavioral Sciences. 1987 June 1;9(2):183–205. [Google Scholar]
- 13.Weinert C. Measuring social support: Revision and further development of the personal resource questionnaire. In: Waltz C, Strickland O, editors. Measurement of Nursing Outcomes. New York: Springer; 1988. pp. 309–27. [Google Scholar]
- 14.Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the united states. J Health Soc Behav. 1999 September;40(3):208–30. [PubMed] [Google Scholar]
- 15.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983 December;24(4):385–96. [PubMed] [Google Scholar]
- 16.Spielberger CD. Manual for the state-trait anxiety inventory. Palo Alto (CA): Consulting Psychologists Press; 1983. [Google Scholar]
- 17.Anderson RM, Fitzgerald JT, Funnel MM, Marrero DG. The diabetes empowerment scale: A measure of psychosocial self-efficacy. Diabetes Care. 2000;23(6):739–43. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- 18.Toobert D, Hampson S, Glasgow R. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care. 2000 July;23(7):943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 19.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care. 2003;41:1284–94. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 21.Swider SM, Martin M, Lynas C, Rothschild SK. Project MATCH: Training for a promotora intervention. The Diabetes Educator. 2009 Nov 12; doi: 10.1177/0145721709352381. (on-line) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Association of Diabetes Educators. Standards for outcomes measurements of diabetes self-management education. The Diabetes Educator. 2003 September/October;29(5):807–16. doi: 10.1177/014572170302900510. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. The social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 24.Saydeh SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular diseae among adults with previously diagnosed diabetes. JAMA. 2004 January 21;291(3):335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]