Abstract
Introduction
Medical school surveys of pre-doctoral curriculum hours in the somnology, the study of sleep, and its application in sleep medicine/sleep disorders (SM) show slow progress. Limited information is available regarding dentist training. This study assessed current pre-doctoral dental education in the field of somnology with the hypothesis that increased curriculum hours are being devoted to SM but that competencies are still lacking.
Materials and methods
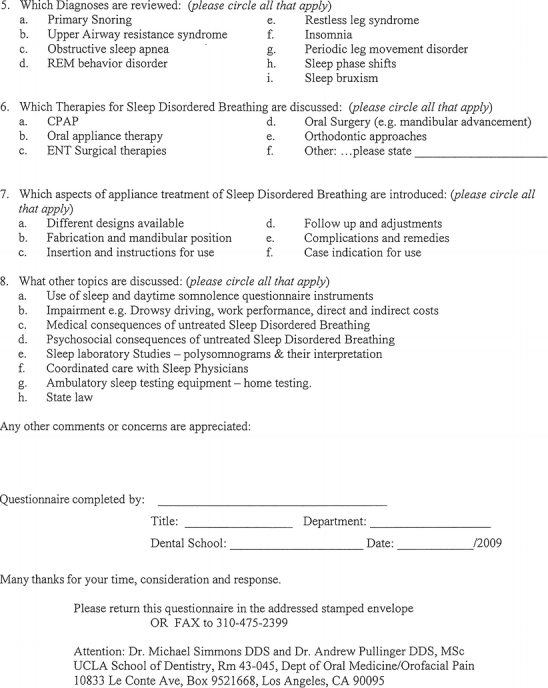
The 58 US dental schools were surveyed for curriculum offered in SM in the 2008/2009 academic year using an eight-topic, 52-item questionnaire mailed to the deans. Two new dental schools with interim accreditation had not graduated a class and were not included. Responses were received from 49 of 56 (87.5%) of the remaining schools.
Results and Conclusions
Results showed 75.5% of responding US dental schools reported some teaching time in SM in their pre-doctoral dental program with curriculum hours ranging from 0 to 15 h: 12 schools spent 0 h (24.5%), 26 schools 1–3 h, 5 schools 4–6 h, 3 schools 7–10 h, and 3 schools >10 h. The average number of educational hours was 3.92 h for the schools with curriculum time in SM, (2.96 across all 49 responding schools). The most frequently covered topics included sleep-related breathing disorders (32 schools) and sleep bruxism (31 schools). Although 3.92 h is an improvement from the mean 2.5 h last reported, the absolute number of curriculum hours given the epidemic scope of sleep problems still appears insufficient in most schools to achieve any competency in screening for SRBD, or sufficient foundation for future involvement in treatment.
Keywords: Dental school somnology education, Teaching sleep medicine, Competency, Sleep bruxism, Sleep-related breathing disorder, Oral appliance therapy
Introduction
Dental sleep medicine is a contemporary topic of considerable interest to dentists, for which the education has been mostly post-graduation continuing education and academy meetings. The purpose of this study was to determine how many US dental schools were now engaged in foundational teaching of somnology in their pre-doctoral programs, and whether this was an increase in the number of schools and/or an increase in the average number of hours taught per school. This paper also projects what would be necessary to achieve a competency standard in screening, collaborative (co-)diagnosis, and co-treatment of sleep-related breathing disorders (SRBD) along with the traditional dental interest in sleep bruxism (SB) which is a sleep-related movement disorder (SRMD). Because the model supported is dental sleep medicine as a component part of the sleep medicine team, the recent history and any progress in education in both dentistry and medicine are reviewed and any progress was noted.
In terms of morbidity and mortality, the most serious sleep disorder is considered to be SRBD [1] and it is in this diagnostic category that dentists and dentistry can make a significant health contribution in screening, co-diagnosis, and co-treatment. Dental practices have become significantly more involved with treating SRBDs, providing oral appliance therapies and mandibular telegnathic surgeries, and considering growth and developmental orthodontic intervention and treatment approaches. The prevalence of SRBD and comorbidities, along with the proximity of the upper collapsible airway to the oral tissues, would suggest that screening of sleep disorders could and should be a routine part of dental screening intake by dentists. According to American Dental Association statistics, there are just over 181,700 professionally active dentists in the US [2], and approximately 300,000 US dental patient visits per year [3], seeing patients on a routine rather than a medical crisis basis. This is an ideal environment to apply SRBD wellness screening to large numbers of the population, possibly catching many before serious medical consequences are manifested.
Historically, Ivanhoe et al. [4] reported in 2003 that 18 of 43 US dental schools (42%) acknowledged the teaching and treatment of upper airway disorders. This averaged 2.5 teaching hours for those 18 schools out of a total of 64 schools surveyed. This therefore averaged to 1.0 educational hours for all 43 responding schools. Of note 25 of the 43 responding dental schools (58%) reported no curriculum time in sleep disorders. However, only 6 of the 18 schools endorsed teaching this material at the pre-doctoral DDS level, 5 of 18 at the postdoctoral level, and the remaining 7 dental schools combined hours between pre- and postdoctoral teaching. The average 2.5 h therefore significantly overstates pre-doctoral education time.
The history of sleep medicine (SM) teaching in MD training programs is also weak but inroads have been made to recognize and improve the situation. The 1988 Task Force on Medical School Curriculum consensus document [5] concluded that “No complete and truly global understanding of human health and disease is possible without an understanding of sleep and its recognition as a system on a par with circulation, digestion, and reproduction.” In 1992, the US congressionally appointed National Commission on Sleep Disorders Research, chaired by William C. Dement, reported how much sleep and sleep disorders affected the lives of Americans [6]. The striking findings were that there was “pervasive sleep deprivation with all its consequences for errors, accidents, disability, damage, and death,” “an epidemic of more than 40 million undiagnosed and untreated, or misdiagnosed and mistreated, chronically ill sleep disorder victims,” and that “knowledge about sleep was completely absent from the educational system.” In his 1998 update report [7] to US congress, commission chairman Dr. Dement reported that “The absence of awareness is so pervasive and complete, it can be changed only by a strong Federal initiative” and added “the diagnosis and treatment of sleep disorders in primary care medicine today is essentially zero.” The more recent 2006 guest editorial by Dement [8] still reported that “teaching somnology and sleep medicine remains outside the mainstream educational system. As a result, vast numbers of health professionals are inadequately informed.”
Methods
This research study surveyed all the 58 US dental schools to gather information on the pre-doctoral curriculum time offered in sleep disorders in the 2008–2009 academic year. The survey instrument was a two-page cover letter with embedded 52 questions questionnaire (Appendix 1) formatted into eight main question categories. Surveys were mailed to the deans of each institution in March 2009, with request to answer or to forward to the appropriate faculty member(s). Repeated follow-up resulted in the high response rate. Two new dental schools with interim accreditation had not graduated a class and were not included. The main eight categories included: the number of hours taught in each of the 4 years; whether the time spent was didactic, clinical laboratory, observational, rotations, or clinical care; which department(s) taught the material; which topic areas were presented; which diagnoses were reviewed; which therapies for SRBD were discussed; which aspects of oral appliance therapy (OAT) were introduced; and what additional topics if any were discussed. Results were tabulated and rechecked on an MS Excel spreadsheet prior to final analysis.
Results
Engagement of dental schools in sleep disorders
Forty nine out of the 56 dental schools (87.5%) included in the study responded to the survey. Of the responding dental schools, 75.5% (37 of 49) reported some educational time in SM. By corollary, 24.5% reported no curriculum time.
Figure 1 shows the current range of pre-doctoral teaching time in sleep disorders in the responding US dental schools. The average total pre-doctoral teaching time in sleep disorders was 3.92 h, (SD 3.39) in the 37 schools reporting sleep curriculum time (2.96 h if averaged across all 49 responding schools), ranging from 0 to 15 h. The mode value was 2 h by 14 schools. This reveals that dental schools are engaged and a few are beginning to extend the curriculum experience.
Fig. 1.
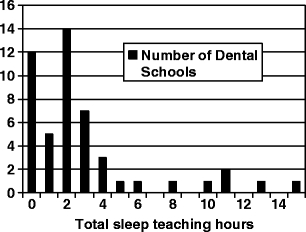
Total pre-doctoral teaching hours in sleep medicine/dental sleep medicine in a 2008–2009 study of 49 US dental schools responding to the survey
Figure 2 shows the percentage distribution by year of the total hours devoted to teaching somnology. The greatest focus of hours was in the DDS third year with a corresponding mean of 1.81 h, followed by the DDS fourth year mean 0.97 h, second year mean 0.64 h and first year mean 0.5 h in the 37 schools with some curriculum.
Fig. 2.
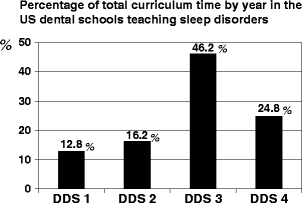
Mean distribution of sleep disorder teaching hours over the 4-year DDS training program in the 37 schools reporting teaching time in this subject area
Didactic vs. clinical teaching
Of the 37 schools with pre-doctoral SM educational time, the majority was didactic (sample average of 78.4% of the percentage of didactic to total hours). The didactic percent ranged from 0% didactic in 2 schools (that had a clinical experience only) to a 100% didactic experience in 22 schools which was the mode value.
Observational and clinical experiences were reported by only 13 (35%) of the 37 schools, ranging from 1 to 5 h, (mean 2.19 h). Broken down, this was: seven schools reporting some general clinic time, range 1–3 h (mean 1.5 h); five schools reporting clinical observation time, range 1–3 h (mean 1.8 h); and five schools with a rotation or selective experience in dental SM, range 1–4 h (mean 1.8 h). A hands-on clinical laboratory experience was reported by 3 (8.1%) of the 37 schools, range 1–8 h (mean 3.7 h).
Figure 3 shows which dental departments provide some education in somnology in the pre-doctoral curriculum. In 40.5% (15 of 37), sleep disorders were taught by a single dental discipline. However, in most schools (59.5%), SM teaching was by more than one discipline, with two disciplines teaching in 40.5% (15 of 37), three disciplines in 13.5% (5 of 37), and four disciplines in 5.4% (2 of 37). Dental specialty postdoctoral programs in temporomandibular disorder (TMD)/orofacial pain, orthodontics, and oral surgery contributed to this multiple discipline teaching in four schools. The survey did not ask whether multiple discipline teaching was coordinated, or resulted from separate department or faculty effort. However, two completed surveys were received from one school, one reported 0 h and one reported 11 h, indicating a lack of coordination or communication in this evolving curriculum. In this regard there is a likelihood of underreporting of total hours taught. SM teaching was reported as taught exclusively at the postdoctoral level in two schools (one school by postdoctoral oral surgery and one school by a combination of postdoctoral TMD/orofacial pain and prosthodontics but reported no pre-doctoral hours).
Fig. 3.
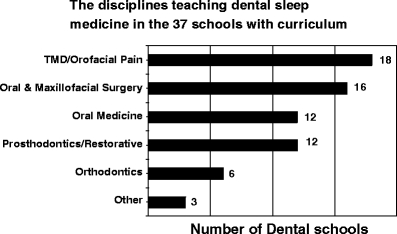
Number of US dental schools reporting the involvement of disciplines in pre-doctoral sleep disorders teaching
Figure 4 explores the percentage of the 37 schools introducing other contemporary topics in somnology. Importantly, 43.2% of the 37 dental schools recognized the importance of coordinating care with sleep physicians, and 54.1% the diagnostic need for PSGs and their interpretation, supporting the multidisciplinary model of dental sleep medicine. Of interest, 6 of 37 (16%) have some time devoted to the concept of home sleep testing (HST, Fig. 4). This is relevant as more dentists and physicians become familiar with objective sleep testing and titration retesting options, especially since HST became a covered benefit under Centers for Medicare and Medicaid Services (CMS) [9].
Fig. 4.
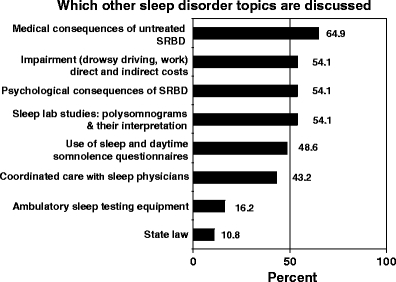
Range of other topics mentioned or included in discussion
Figures 5 and 6 show the pre-doctoral educational engagement in a wide spectrum of sleep-related topics and diagnoses.
Fig. 5.
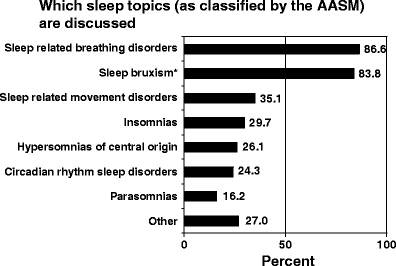
Topic areas in sleep disorders, as classified by the AASM (plus sleep bruxism), reported in the pre-doctoral teaching survey
Fig. 6.
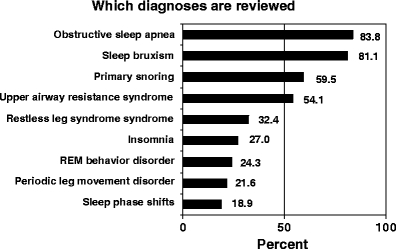
Shows which diagnoses are reviewed in the pre-doctoral education in somnology
Figure 7 shows which therapies for SRBD are discussed including dental and nondental-based approaches, and Fig. 8 focuses on various aspects of OAT provided by dentists treating SRBD.
Fig. 7.
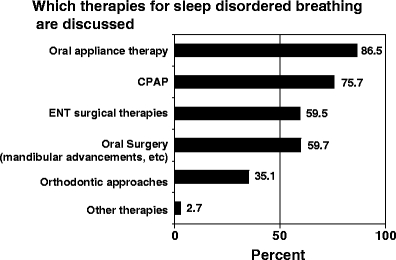
Shows which therapies for SRBD are presented including oral appliance therapy
Fig. 8.
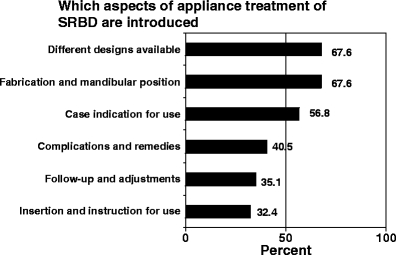
Shows which aspect of oral appliance therapy for SRBD are introduced
Discussion
Dental sleep medicine is viewed by practicing dentists to be an evolving normal part of modern dental practice. The questions are how much foundational education is being provided by dental schools and how much organized dental education is setting the model and competency standards. As an indication of need and demand for treatment, a survey of predominantly general dentists, members of the Sleep Disorder Dental Society, reported providing focused evaluation or treatment for 5% of their total patients for problem snoring or obstructive sleep apnea (OSA) [10]. However, in terms of educational preparedness, a survey of Indiana dentists [11] reported general lack of education in OSA and treatment experience with oral appliances despite 93% of dentists agreeing that OSA constitutes a life-threatening illness. Only 16% reported any formal pre-doctoral and 30% postdoctoral training in this field, whereas 32% endorsed they were self-taught. While 58% of respondents could not identify common signs and symptoms of OSA, 40% admitted knowing little or nothing about OSA.
SM education at the pre-doctoral level in the US in medicine and dentistry shows a slow trend to an increased number of hours. However, the average hours are not enough to qualify as more than an introduction. Less than 1 h of education was spent during the four-year MD program in 1978 [12] with the authors concluding that 93% of American medical schools then had “essentially no preparation of physicians to deal with clinical sleep disorders.” The results from a 1991 survey showed that pre-doctoral medical educational hours had increased to just under 2 h [13], and the percentage of schools listing the topic of sleep disorders had increased to 63% up from 54% in 1978. To address the deficiency, the American Sleep Disorders Association, precursor to the American Academy of Sleep Medicine (AASM), met in 1995 and developed the Taskforce 2000 with a long term goal to “ensure adequate teaching on sleep and sleep disorders in the curriculum of all medical schools by the year 2000.” Similar projects have yet to be initiated by organized dentistry such as by The American Academy of Dental Sleep Medicine (AADSM) or by the American Dental Education Association (ADEA). However, by 1998, Rosen et al. [14] reported achieving only 2.11 h for pre-doctoral medical education in sleep (1.6 h preclinical and 0.9 h in the clinical years), and 4.8 h in postdoctoral programs such as psychiatry, neurology, and pediatrics. Additionally, a review of medical textbooks by page allocation [15] showed about 2% of pages devoted to SM in 1999 and this has stayed the same or decreased through 2007. Haponik et al. [16] consequently reported that a sleep history is a commonly neglected diagnostic information and that major changes in physician education and behavior are essential to raising the importance of SM. Namen et al. [17] reported that sleep histories are seldom documented by medical house officers and that the simple use of a medical record reminder generated increased frequency of sleep history documentation Furthermore, 90% of a sample of 580 US primary care physicians in 2002 rated their own knowledge of sleep disorders as fair or poor [18]. Even US specialty chest physicians, and pulmonologists with additional training in SM, with >30% directing sleep laboratories and >65% either directing or on staff of sleep laboratories, did poorly when tested on diagnosis and management of “non-pulmonary” sleep disorders cases [19].
The Taskforce 2000 competency-based goals for pre-doctoral medical education in sleep medicine [20] published in 1998 have therefore yet to be met. Fortunately, there is an encouraging level of interest in this topic, and doctors are aware of their need for improvement to their pre-doctoral basic science foundational and clinical education [21]. Medical students, postgraduate physicians, and medical specialists admitted to poor knowledge in SM [22], but revealed a positive attitude toward the topic of SM indicating a need for better medical school education in this field. In this regard, 20 fourth year medical students that chose an integrated selective in sleep medicine improved their test scores from 56% preprogram to 86% post-program, and evaluated the rotation well above other rotations [23].
The US is not alone with this problem. In the United Kingdom, education in SM in 1998 [24] showed only about 20 min in physician training. Other international studies report that less than 10% of medical school seniors scored >70% on questions in SM [25]. In another study only 2% of third and fourth year medical students, when tested, scored >66% in basic SM [26] and yet another study found second year medical students and physician specialists recorded an equally poor knowledge of SM [27]. Other medically related fields report a similar lack of education in the somnology. US nursing recognized there was no established curriculum for sleep in both their undergraduate and postgraduate education and made major and probably realistic recommendations for up to 40 h of “sleep education” rotations in nursing undergraduate training, in addition to establishing seven learning objectives and suggested readings [28]. The interest but reported deficiency in sleep education also includes pharmacy undergraduates and practicing community pharmacists [29].
This current study of dental school education found that 75.5% of the responding US pre-doctoral DDS programs (37 of 49) are providing some teaching time in somnology (3.92 h), and that the majority of US dental schools are engaged in the topic (Fig. 1). However, only a few schools appear to extend the curriculum experience past the introductory level. Conversely, 24.5% (12 of 49) of the responding dental schools reported no educational time in sleep disorders, which rises to 34% (19 of 56) if all the non-responding schools were assumed to have no teaching time. This represents an increase in dental schools teaching somnology over Ivanhoe’s 2003 report which indicated 42% (18 of 43) responding dental schools taught somnology. Conversely, 58% (25 of 43) of responding dental schools had no teaching time, which rose to 72% (46 of 64) if all the non-responding schools were assumed to have no teaching time.
A high 87.5% response rate was achieved in this survey. However, it is difficult to interpret whether the non-responding schools, or the responding schools reporting no curriculum hours in dental sleep medicine, truly had no dental sleep medicine curriculum hours. Recognizing somnology education depended upon identifying appropriate faculty member(s) or department(s) associated with this subject, and determining whether any discussion of SM categories was informal (not formally listed in the curriculum) and these may have been potentially missed by the survey responder. Traditionally, schools do spend time covering SB education, which should be attributed SRMD as classified by the International Classification of Sleep Disorders [30]. This is of increased relevance as various interrelations of bruxism, SRBD, and sleep pathophysiology become understood [31–36]. For example, a reduction in SB has been observed with successful application of CPAP in SRBD patients [31, 32], adenotonsillectomy [33], medication management [34] using a REM behavior disorder drug [35], and after OAT [36], indicating that an expansion of the dental curriculum to include SRBD with SRMD is inevitable in dentistry. It is suspected that currently most of the pre-doctoral dental education emphasis on bruxism is in the clinical management of dental occlusal trauma and attrition.
This study also found most of the dental education in SM was didactic (78.4%), and a 100% didactic experience was the most frequent report (mode) by 22 schools. Carrying this to clinical practice would therefore be problematic for most students without offering additional clinical labs, selectives, and hands-on experiences. In fact observational and clinical experiences were reported by only 35% (13 of 37) of schools (mean 2.19 h, range 1–5 h). Only 8% (3 of 37) of the schools offered a clinical laboratory hands-on experience (mean 3.7 h, range 1–8 h), which the authors have found to be a very meaningful training experience for SRBD screening. It is expected that a tipping point can only be achieved when routine simple sleep disorder screening protocols and an algorithm for disposition of identified potential SRBD patients becomes a routine part of oral diagnosis clinic patient intake in dental schools.
The mean hours in dentistry in sleep education now appears comparable if not slightly more than the 2.11 number of hours most recently reported in pre-doctoral medical curricula [13]. However, in dentistry, the focus is on SRBD and the SRMD of sleep bruxism. Although an encouraging beginning for dentistry, and a measurable increase over the hours reported by Ivanhoe in 2003 [4], the authors believe the current total average hours were taught only fulfill an introduction, and require evolution to develop any competency (defined as the ability to use and apply knowledge).
The increase in SM training in dental schools with more schools participating and more hours per program as compared to the Ivanhoe 2003 survey may build the confidence for increased multidisciplinary collaboration as members of a sleep medicine team, and ultimately better patient care outcomes. While it is noted that nursing [27] suggests 40 h of clinical rotation and more didactic experience for adequate training in their field, treatment competency beyond screening and co-diagnosis seems an unrealistic goal for the DDS curriculum, unless a major elective experience is provided. However, the authors believe it is the responsibility of DDS programs to establish a reasonable and a correct medical and dental basic science and clinical foundation upon which to build postdoctoral treatment experience with further training following graduation.
There are not yet any formal US pre-doctoral educational accreditation standards in SM for DDS programs, but according to the Commission on Dental Accreditation [37], the accreditation standards for general dentistry state that “the program goals must prepare the graduates to begin the practice of general dentistry.” De facto this already includes dental sleep medicine (as gauged by the interest and activity of dental practitioners and for example by the steady yearly increase in the membership of the AADSM from 250 in 2001 to 1,600 members at the end of 2009 [38] and as of December 2010 over 2,100). Meanwhile, it is up to each dental school to define the competencies needed for graduation and to reflect contemporary practice. Certainly, the current engagement of 75.5% of the reporting US dental schools in some sleep disorder teaching indicates that foundational standards of care defined by training are becoming a responsibility of general dentistry training programs.
Future directions
Establishing DDS curriculum foundational standards in the DDS training programs would now appear a reasonable next goal by involvement of the ADEA with input from the American Academy of Dental Sleep Medicine. The next phase could be organizational by transition into agreed competency-based goals. The authors suggest the following US DDS educational standards be considered:
- The DDS general dental graduate should demonstrate competency in conducting a routine screening for SRBD and the SRMD of sleep bruxism in all dental patients. This includes:
- Taking a screening sleep history: using questions selected to screen for daytime somnolence, problem snoring, pauses in breathing during sleep, and sleep qualities
- □ Including a familiarity with validated if limited questionnaire indices that can be used to quantify sleep disorder symptoms
- The clinical ability to identify oropharyngeal anatomic and mechanical factors that can relate to collapse and obstruction of the upper airway
- Being prompted to conduct a SRBD screening in patients with potential comorbidities including hypertension, cardiovascular disease, metabolic disorders, diabetes, CNS effects such as cognitive deficits and depression, GERD, headache on waking, and obesity, to rule out sleep disorder as a cofactor
- Having sufficient knowledge to discuss the medical consequences of non-treatment of SRBD and the benefits of treatment with their patients
- Having sufficient knowledge to discuss the available treatment options with their patients
- Understanding that habitual snoring cannot be dismissed as just a social issue, unless first ruled out as a benign symptom of SRBD by appropriate medical testing and diagnosis.
- The DDS general dental graduate should be familiar with how to refer suspected SRBD patients for more testing, further evaluation, and possible treatment.
- □ Including understanding that evaluation of SRBDs requires a sleep study with sleep specialist interpretation for adequate diagnosis
The DDS general dental graduate should have acquired sufficient foundational applied basic science and clinical understanding in somnology to support competencies 1 and 2, and upon which to build future treatment competencies after additional training in selectives and post-graduation education.
Competencies 1 and 2 are considered the primary public health objectives and the authors believe these could be implemented in routine screening in oral diagnosis in dental school clinics and dental practice along with patient referral algorithms.
The authors firmly believe that the epidemiology of SRBD necessitates a screening and treatment model that includes all general practice dentists and is not just limited to the much fewer dental specialty practices. For example, there are over 181,700 professionally active dentists in the USA [2] for approximately 40 million of the US population conservatively estimated to have SRBD [39, 40].
This survey showed that education in SM in US DDS programs is being taught by several dental departments or disciplines, but was not the purview of any specific dental specialty or program (Fig. 3). This reflects that SM is a multidisciplinary issue within the field of dentistry in addition to the greater multidisciplinary nature within the whole field of health care.
The source of training of sufficient educators in this emerging dental field is an issue. The current study did not specifically survey the sleep medicine training in the dental specialty programs. Currently, only the postdoctoral programs in prosthodontics [41] and orofacial pain [42] list any advanced educational standards in SM, but the number of these graduates is limited. The authors point out that addition of SRBD competencies and training to the Dental General Practice Residency (GPR) programs would seem very beneficial since these programs are mostly hospital based, and would maintain a general rather than dental specialty viewpoint. Numerically, there were 944 first year dental GPR positions in the USA in the year 2008/2009 [43???]. If somnology education was also added to the US Advanced Education in General Dentistry (AEGD), this would bring the total such trainees from GPR and AEGD to 1,488 per year, which could have major impact in dental education and practice of dental sleep medicine.
Conclusions
The authors summarize the following three conclusions from this study and review.
While this study shows an increase in number of dental schools teaching SM and also an increase in the average hours taught in SM, the numbers of individuals with sleep problems in the US are far larger than the existing trained health providers can identify and manage and education hours in somnology continues to be inadequate.
Of dental school DDS programs, 74.5% report providing some teaching time in SM averaging 3.92 h that is primarily didactic with only a few schools extending the curriculum to a clinical screening experience and education is not provided by a specific dental discipline.
Dental pre-doctoral education in SM primarily addresses SRBDs and SB but also presents an array of SM topics as foundational understanding to potentially enable collaboration as members of a multidisciplinary sleep medicine team.
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix 1
Questionnaire—Education in Sleep Disorders
Footnotes
Work was performed at UCLA School of Dentistry and Dr. Simmons private dental practice.
References
- 1.Philipson EA. Sleep disorders. In: Murray JF, Nadel JA, editors. Textbook of respiratory medicine. Philadelphia: Saunders; 1988. pp. 1841–1860. [Google Scholar]
- 2.Annual Survey by ADA (2009) Report on the distribution of dentists in the United States by region and state
- 3.Manski RJ, Moeller JF, Maas WR. Dental services: an analysis of utilization over 20 years. J Am Dent Assoc. 2001;132:655–664. doi: 10.14219/jada.archive.2001.0243. [DOI] [PubMed] [Google Scholar]
- 4.Ivanhoe JR, Frazier KB, Parr GR, Haywood VB. The teaching and treatment of upper airway sleep disorders in North American dental schools. J Prosthet Dent. 2003;89:292–296. doi: 10.1067/mpr.2003.52. [DOI] [PubMed] [Google Scholar]
- 5.(1988) Report of task force on medical school curriculum: consensus document. Sleep 11:566–570 [PubMed]
- 6.Public Policy Recommendations to the US congress from the National Commission of Sleep Disorders Research (1990–1992)
- 7.Dement WC (1998) The current status of sleep disorders in America and the National Center on Sleep Disorders Research (of 1992 Public Policy Recommendations to the US congress from the National Commission of Sleep Disorders Research)
- 8.Dement WC, Koenigsberg R. Impediments to access to care. Sleep Rev. 2006;7:20–22. [Google Scholar]
- 9.Centers for Medicare & Medicaid Services (2007) Decision memo for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). https://www.cms.hhs.gov/mcd/viewdraftdecisionmemo.asp?id20448
- 10.Loube DI, Strauss AM. Survey of oral appliance practice among dentists treating obstructive sleep apnea patients. Chest. 1997;111:382–386. doi: 10.1378/chest.111.2.382. [DOI] [PubMed] [Google Scholar]
- 11.Bian H. Knowledge, opinions, and clinical experience of general practice dentists toward obstructive sleep apnea and oral appliances. Sleep Breath. 2004;8:85–90. doi: 10.1055/s-2004-829633. [DOI] [PubMed] [Google Scholar]
- 12.Orr WC, Stahl ML, Dement WC, Reddington D. Physician education in sleep disorders. J Med Educ. 1980;55:367–369. doi: 10.1097/00001888-198004000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Rosen RC, Rosekind M, Rosevear C, Cole WE, Dement WC. Physician education in sleep and sleep disorders: a national survey of US medical schools. Sleep. 1993;16:249–254. doi: 10.1093/sleep/16.3.249. [DOI] [PubMed] [Google Scholar]
- 14.Rosen R, Mahowald M, Chesson A, Doghramji K, Goldberg R, Moline M, Millman R, Zammit G, Mark B, Dement W. The Taskforce 2000 survey on medical education in sleep and sleep disorders. Sleep. 1998;21:235–238. doi: 10.1093/sleep/21.3.235. [DOI] [PubMed] [Google Scholar]
- 15.Teodorescu MC, Avidan AY, Teodorescu M, Harrington JJ, Artar AO, Davies CR, Chervin RD. Sleep medicine content of major medical textbooks continues to be underrepresented. Sleep Med. 2007;8:271–276. doi: 10.1016/j.sleep.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Haponik EF, Frye AW, Richards B, Wymer A, Hinds A, Pearce K, McCall V, Konen J. Sleep history is neglected diagnostic information. Challenges for primary care physicians. J Gen Intern Med. 1996;11:759–761. doi: 10.1007/BF02598994. [DOI] [PubMed] [Google Scholar]
- 17.Namen AM, Wymer A, Case D, Haponik E. Performance of sleep histories in an ambulatory medicine clinic. Chest. 1999;115:1558–1563. doi: 10.1378/chest.116.6.1558. [DOI] [PubMed] [Google Scholar]
- 18.Papp KK, Penrod CE, Strohl KP. Knowledge and attitudes of primary care physicians toward sleep and sleep disorders. Sleep Breath. 2002;6:103–109. doi: 10.1055/s-2002-34317. [DOI] [PubMed] [Google Scholar]
- 19.Phillips B, Collop N, Goldbert R. Sleep medicine practices, training, and attitudes. A wake-up call for pulmonologists. Chest. 2000;117:1603–1607. doi: 10.1378/chest.117.6.1603. [DOI] [PubMed] [Google Scholar]
- 20.Strohl KP, Haponik EE, Sateia MJ, Veasy S, Chervin RD, Zee P, Papp K. The need for a knowledge system in sleep and chronobiology. Acad Med. 2000;8:819–821. doi: 10.1097/00001888-200008000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Owens J. Introduction to special section: NIH sleep academic award program. Sleep Med. 2005;6:45–46. doi: 10.1016/j.sleep.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 22.Bandla H, Franco R, Statza T, Feroah T, Rice TB, Poindexter K, Simpson D. Integrated selective: an innovative teaching strategy for sleep medicine instruction for medical students. Sleep Med. 2007;8:144–148. doi: 10.1016/j.sleep.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Stores G, Crawford C. Medical student education in sleep and its disorders. Medical student education in sleep and its disorders. J R Coll Physicians Lond. 1998;32:149–153. [PMC free article] [PubMed] [Google Scholar]
- 24.Sivagnanam G, Thirumalaikolundusubramanian P, Sugirda P, Rajeswari J, Namasivayam K, Gitanjali B. Study of the knowledge, beliefs, and practice of sleep among medical undergraduates of Tamilnadu. MedGenMed. 2004;12(6):5. [PMC free article] [PubMed] [Google Scholar]
- 25.Mahendran R, Subramaniam M, Chan YH. Medical students’ behaviour, attitudes and knowledge of sleep medicine. Singapore Med J. 2004;45:587–589. [PubMed] [Google Scholar]
- 26.Kovacić Z, Marendić M, Soljić M, Pecotić R, Kardum G, Dogas Z, Pecotić R, Kardum G, Dogas Z. Knowledge and attitude regarding sleep medicine of medical students and physicians in Split, Croatia. Croat Med J. 2002;43:71–74. [PubMed] [Google Scholar]
- 27.Lee KA, Landis C, Chasens ER, Dowling G, Merritt S, Parker KP, Redeker N, Richards KC, Rogers AE, Shaver JF, Umlauf MG, Weaver TE. Sleep and chronobiology: recommendations for nursing education. Nurs Outlook. 2004;53:126–133. doi: 10.1016/j.outlook.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Ang KT, Saini B, Wong K. Sleep health awareness in pharmacy undergraduates and practicing community pharmacists. J Clin Pharm Ther. 2008;33:641–652. doi: 10.1111/j.1365-2710.2008.00963.x. [DOI] [PubMed] [Google Scholar]
- 29.American Academy of Sleep Medicine . International classification of sleep disorders: diagnostic and coding manual. 2. Westchester: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 30.Oksenberg A, Arons E. Sleep bruxism related to obstructive sleep apnea: the effect of continuous positive airway pressure. Sleep Med. 2002;3:513–515. doi: 10.1016/S1389-9457(02)00130-2. [DOI] [PubMed] [Google Scholar]
- 31.Simmons J, Prehn R. Airway protection: the missing link between nocturnal bruxism and obstructive sleep apnea [abstract 0668] Sleep. 2009;32:A218. [Google Scholar]
- 32.DiFrancesco RC, Junqueira PA, Trezza PM, de Faria ME, Frizzarini R, Zerati FE. Improvement of bruxism after T & A surgery. Int J Pediatr Otorhinolaryngol. 2004;68:441–445. doi: 10.1016/j.ijporl.2003.11.022. [DOI] [PubMed] [Google Scholar]
- 33.Saletu A, Parapatics S, Saletu B, Anderer P, Prause W, Putz H, Adelbauer J, Saletu-Zyhlarz GM. On the pharmacotherapy of sleep bruxism: placebo-controlled polysomnographic and psychometric studies with clonazepam. Neuropsychobiology. 2005;51:214–225. doi: 10.1159/000085917. [DOI] [PubMed] [Google Scholar]
- 34.Schenck CH, Mahowald MW. Rapid eye movement sleep parasomnias. Neurol Clin. 2005;23:1107–1126. doi: 10.1016/j.ncl.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Landry ML, Rompré PH, Manzini C, Guitard F, de Grandmont P, Lavigne GJ. Reduction of sleep bruxism using a mandibular advancement device: an experimental controlled study. Int J Prosthodont. 2006;19:549–556. [PubMed] [Google Scholar]
- 36.Commission on Dental Accreditation . Accreditation standards for dental education programs. Chicago: American Dental Association; 2007. [Google Scholar]
- 37.American Academy of Dental Sleep Medicine (2009) Membership report. http://www.aadsm.org/pdfs/AnnualReport.pdf
- 38.Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol. 2005;99:1592–1599. doi: 10.1152/japplphysiol.00587.2005. [DOI] [PubMed] [Google Scholar]
- 39.Jelic S, Le Jemtel TH. Inflammation, oxidative stress, and the vascular endothelium in obstructive sleep apnea. Trends Cardiovasc Med. 2008;18:253–260. doi: 10.1016/j.tcm.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 40.Commission on Dental Accreditation . Accreditation standards for advanced specialty education programs in prosthodontics, standard 4–9d. Chicago: American Dental Association; 2008. [Google Scholar]
- 41.Commission on Dental Accreditation . Accreditation standards for advanced general education programs in orofacial pain, standard 2–5e, 2–10e3, 2–11. Chicago: American Dental Association; 2009. [Google Scholar]
- 42.American Dental Association (2010) 2008–09 Survey of advanced dental education


