Abstract
Increasing attention is being focused on sleep duration as a potential modifiable risk factor associated with obesity in children and adolescents. We analyzed data from the national Youth Risk Behavior Survey to describe the association of obesity (self-report BMI ≥95th percentile) with self-reported sleep duration on an average school night, among a representative sample of US high school students. Using logistic regression to control for demographic and behavioral confounders, among female students, compared to 7 hours of sleep, both shortened (≤4 hours of sleep; adjusted odds ratio (95% confidence interval), AOR = 1.50 (1.05–2.15)) and prolonged (≥9 hours of sleep; AOR = 1.54 (1.13–2.10)) sleep durations were associated with increased likelihood of obesity. Among male students, there was no significant association between obesity and sleep duration. Better understanding of factors underlying the association between sleep duration and obesity is needed before recommending alteration of sleep time as a means of addressing the obesity epidemic among adolescents.
1. Introduction
During the past century, the average amount of time that Americans sleep has decreased by approximately 20 percent [1]. According to sleep duration guidelines suggested by the National Sleep Foundation, insufficient sleep, defined as <8 hours for children and <7 hours for adults on a weeknight, is experienced by 45% of children ages 11–17 years and 37% of adults [2, 3]. It is currently estimated that 50 to 70 million Americans chronically suffer from disorders of sleep and wakefulness which adversely affect daily functioning, health, and longevity [4]. The cumulative effects of chronic sleep deprivation and sleep disorders have been associated with increased mortality and increased risk for a wide range of chronic diseases including depression, hypertension, stroke, type 2 diabetes, heart disease, and obesity [4, 5].
The relationship between sleep and obesity has become a topic of great interest as obesity rates reach record levels and chronic sleep deprivation affects increasing numbers of adolescents and adults in the United States [4–7]. The two most commonly reported associations between sleep duration and obesity are (1) a U-shaped curve where the lowest obesity risk is found at about 7-8 hours of sleep per night, with the odds of obesity rising for shorter and longer sleep duration, leading to the optimal dose theory of habitual sleep duration and (2) a negative linear pattern where the longest sleep durations are associated with the least likelihood and the shortest sleep durations are associated with the greatest likelihood of obesity, leading to the more sleep is better theory of habitual sleep duration [5].
Although there are few proposed mechanisms for how longer sleep duration might predispose toward obesity, there is experimental evidence for metabolic pathways whereby shortened sleep duration might lead to increased obesity. Sleep restriction in healthy adults has been shown to result in decreased leptin levels and increased ghrelin levels, which result in decreased satiety and increased appetite, respectively [8, 9]. Alterations in these hormone levels may lead to increases in subsequent caloric intake and weight gain. Sleep restriction also has been shown to alter carbohydrate metabolism, resulting in increased insulin resistance and impaired glucose tolerance, which may also affect weight status [8, 10, 11]. Another recognized link between obesity and sleep deprivation is obstructive sleep apnea, a condition which may be caused by obesity and which results in sleep disruption. An analysis of 20 years of data on obesity-associated diseases among children ages 6–17 years found that hospital discharges for sleep apnea have increased more than 400% [12].
Recent reviews of cross-sectional and longitudinal studies that examined the association between sleep duration and obesity found no consistent pattern of association among adults, with studies that reported a U-shaped association, studies that reported a negative linear association, and studies that reported no association [5, 8]. Unlike adult studies, pediatric studies involving young children have consistently found a negative linear association between sleep duration and obesity [5, 8, 13]. Findings from studies involving adolescents are less consistent and sometimes exhibit sex differences [13]. The purpose of this study was to describe the association between habitual sleep duration and obesity among a nationally representative sample of high school students, controlling for demographic characteristics and behavioral confounders. Specifically, we sought to determine whether the association was a negative linear association, such as typically found in studies involving younger children, or a U-shaped association such as sometimes reported in studies of adults and whether that association varied by sex, race/ethnicity, or grade.
2. Methods
2.1. Sample and Survey Administration
Since 1991, the biennial, national Youth Risk Behavior Survey (YRBS) has used a three-stage cluster sample design to produce nationally representative samples of students in grades 9–12 attending public and private schools. Student participation in the survey was anonymous and voluntary, and local parental permission procedures were followed. Students completed a self-administered questionnaire during a regular class period. Responses were recorded directly on computer-scannable questionnaire booklets. A weighting factor was applied to each record to adjust for nonresponse and the oversampling of black and Hispanic students. Sampling strategies and the psychometric properties of the questionnaire have been reported previously [14–17]. The Centers for Disease Control and Prevention (CDC) Institutional Review Board granted approval for the national YRBS.
Data on sleep duration was collected in the national YRBS for the first time in 2007. To increase the sample size of students reporting long or short sleep durations, we combined data from the 2007 and 2009 national YRBS. Individual students were not followed longitudinally, but rather each survey represented an independently selected, nationally representative, cross-sectional sample of public and private school students. School response rates for both surveys were 81%. Student response rates for 2007 and 2009 were 84% and 88%, respectively. Overall response rates (defined as school response rate × student response rate) were 68% and 71%, respectively. A small number of surveys (62 in 2007 and 50 in 2009) failed data edit checks leaving final sample sizes of 14,041 and 16,410, respectively [14, 15]. Thus, a total of 30,451 students were surveyed and provided usable data during 2007–2009.
2.2. Measures
2.2.1. Demographic Characteristics
Demographic characteristics included sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and others), and grade (9th, 10th, 11th, and 12th).
2.2.2. Sleep
Students were asked, “On an average school night, how many hours of sleep do you get?” Response options were “4 or less hours,” “5 hours,” “6 hours,” “7 hours,” “8 hours,” “9 hours,” or “10 or more hours.” Consistent with the guidelines of the National Sleep Foundation, students who reported sleeping less than 8 hours on a school night were considered to have insufficient sleep [2].
2.2.3. Obesity
Self-reported height and weight (without shoes on) were used to calculate body mass index (BMI), expressed as body weight in kilograms divided by the square of height in meters (kg/m2). Using reference data from growth charts produced by CDC, students with a BMI greater than or equal to the 95th percentile for sex and age (in months) were considered to be obese [18]. The questionnaire asked students to report their age in years as a whole number between 13 and 17 with additional options for 12 or younger (assigned a value of 12 years) and 18 or older (assigned a value of 18 years). Half a year (6 months) was added to the age since, for example, students who reported their age as 16 years would, on average, be approximately 16 years and 6 months (198 months) old.
2.2.4. Behavioral Confounders
To identify potential confounding variables to control for in our final analyses, we examined the literature for health-related behaviors which might be associated with both obesity and sleep duration [19–29]. We identified 8 behaviors assessed in the YRBS which might confound the association between sleep duration and obesity. We then tested whether each behavior was associated with sleep duration and obesity in our sample using logistic regression models that controlled for sex, race/ethnicity, and grade. Five behaviors were significantly associated with both sleep duration and obesity and were included, along with demographic variables, as potential confounders in final models. These behaviors included feeling sad and hopeless (prevalence, 95% CI: 27.2%, 26.2%–28.2%), being a current smoker (19.7%, 18.3%–21.2%), drinking nondiet soda or pop (31.3%, 29.6%–33.1%), using a computer or playing video games for 3 or more hours on an average school day (24.9%, 23.5%–26.4%), and being physically active for at least 60 minutes daily (17.8%, 17.0%–18.6%).
2.3. Missing Data
Of the 30,451 observations in the combined dataset, a total of 2,211 (7.3%) were missing data on BMI, and 3,515 (11.5%) were missing data on sleep duration. Missing data on demographic characteristics ranged from 549 (1.8%) for race/ethnicity to 78 (0.3%) for sex, and missing data on behavioral confounders ranged from 1,366 (4.5%) for current smoking to 502 (1.6%) for being physically active. Missing data were not imputed. A total of 23,579 students had complete data on all variables. Compared to students with complete data on all variables, those with missing data on at least 1 variable (n = 6, 872) had similar prevalence estimates for obesity (12.4% versus 12.3%, resp.) and insufficient sleep (69.2% versus 68.1%). Prevalence estimates for sex, current smoking, drinking nondiet soda or pop, time spent playing video games, and using a computer for something other than schoolwork, and being physically active also did not vary significantly between these two groups. Compared to students with complete data, students with some missing data were more likely to report very long or short sleep durations, were more likely to be Hispanic or other race/ethnicity, were more likely to be in lower grade levels, and were more likely to report feeling sad or hopeless (data not shown).
2.4. Analysis
All analyses were conducted using SUDAAN [30] to account for the complex sample design. Prevalence estimates in our analyses are unadjusted. Students who reported sleeping ≤4 hours were considered to sleep 4 hours, and students who reported sleeping ≥10 hours were considered to sleep 10 hours. Using logistic regression, we tested for the presence of linear and quadratic (U-shaped) associations between obesity (dependent variable) and sleep duration (independent variable), controlling for sex, race/ethnicity, grade, and confounding behaviors. Finally, we calculated crude and adjusted odds ratios with 95% confidence intervals (CIs) for each level of sleep duration and each demographic and behavioral variable entered into the final model. Associations were considered statistically significant at P < 0.05.
3. Results
3.1. Sample Characteristics
The total sample size for the combined 2007 and 2009 national YRBS datasets was 30,451. Weighted prevalence estimates for demographic groups included 51.4% male, 48.6% female, 59.4% white, 14.7% black, 17.8% Hispanic, 8.1% other racial and ethnic minorities, 28.5% 9th grade, 26.2% 10th grade, 23.5% 11th grade, and 21.8% 12th grade students.
3.2. Sleep Duration
The distribution of sleep duration on an average school night approximated a bell-shaped curve among female and male students (Figure 1). Mean sleep duration was shorter among female (6.7 hrs; 95% CI: 6.7-6.8) than male (6.9 hrs; 95% CI: 6.8-6.9) students (t = 8.78, P < 0.001). Approximately 7 of 10 (69.0%) students reported getting insufficient (i.e., ≤7 hrs) sleep on an average school night (Table 1). The prevalence of insufficient sleep was greater among female (71.6%) than male (66.6%) students (t = 8.05, P < 0.001). Insufficient sleep was more prevalent among white (69.2%; t = 2.42, P = 0.018) and black (70.5%; t = 3.24, P < 0.002) than Hispanic (65.8%) students. The prevalence of insufficient sleep increased with grade (59.1%, 9th; 68.2%, 10th; 74.1%, 11th; 76.8%, and 12th). All pairwise comparisons by grade level were significant (t-test statistics ranged from 2.70 to 17.78, all P < 0.01).
Figure 1.
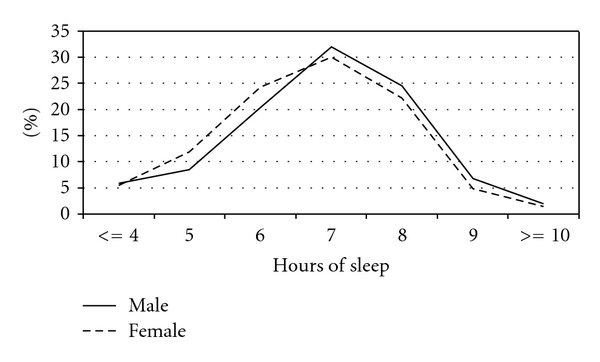
Distribution of sleep duration on an average school night, by sex—US high school students.
Table 1.
Prevalence of insufficient and long sleep duration and obesity—US high school students.
| Demographic subgroup | Sleep durationa | Insufficient (≤7 hours) | Long (≥9 hours) | Obese (BMI ≥ 95th percentile)b | ||||
| (N) | % | 95% CI | % | 95% CI | (N) | % | 95% CI | |
| Total | (26,936) | 69.0 | 67.8–70.3 | 7.6 | 7.1–8.1 | (28,240) | 12.4 | 11.7−13.2 |
| Sex | ||||||||
| Female | (13,575) | 71.6 | 70.3–72.8 | 6.2 | 5.6– 6.9 | (14,096) | 8.9 | 8.1−9.7 |
| Male | (13,297) | 66.6 | 65.2–68.1 | 8.9 | 8.1– 9.7 | (14,144) | 15.7 | 14.5−17.0 |
| Race/ethnicity | ||||||||
| White | (11,728) | 69.2 | 67.7–70.7 | 6.7 | 6.1–7.3 | (12,032) | 10.5 | 9.5−11.7 |
| Black | (5,114) | 70.5 | 68.7–72.3 | 8.7 | 7.6–10.0 | (5,357) | 16.6 | 15.3−18.1 |
| Hispanic | (7,296) | 65.8 | 63.2–68.3 | 9.7 | 8.5–11.0 | (7,863) | 15.7 | 14.5−17.1 |
| Other | (2,357) | 72.5 | 68.3–76.2 | 7.1 | 5.1– 9.9 | (2,605) | 11.4 | 9.8−13.3 |
| Grade | ||||||||
| 9th | (6,615) | 59.1 | 57.4–60.7 | 12.5 | 11.2–13.8 | (6,922) | 12.7 | 11.7−13.9 |
| 10th | (6,485) | 68.2 | 66.3–70.1 | 7.1 | 6.2–8.0 | (6,877) | 12.0 | 10.9−13.1 |
| 11th | (6,808) | 74.1 | 72.2–76.0 | 5.4 | 4.8–6.2 | (7,130) | 12.2 | 11.1−13.4 |
| 12th | (6,878) | 76.8 | 74.9–78.7 | 4.3 | 3.7–5.1 | (7,256) | 12.8 | 11.4−14.4 |
N = unweighted sample size. CI = confidence interval.
aOn an average school night.
bBased on self-reported height and weight, body mass index (BMI = weight [kg]/height [m]2) ≥95th percentile using growth charts developed by the Centers for Disease Control and Prevention for youth aged 2–20 years.
3.3. Obesity
Approximately 12.4% of students were obese (Table 1). The prevalence of obesity was greater among male (15.7%) than female (8.9%) students (t = 9.81, P < 0.001). Obesity was more prevalent among black (16.6%; t = 6.46, P < 0.001) and Hispanic (15.7%; t = 6.89, P < 0.001) than white (10.5%) students. The prevalence of obesity did not vary significantly with grade.
3.4. Behavioral Confounders
We tested 8 behaviors assessed in the YRBS which might confound the association between sleep duration and obesity using logistic regression models that controlled for sex, race/ethnicity, and grade (Table 2). For this analysis, behavioral variables were coded dichotomously using cut-points consistent with national guidelines, health objectives, and surveillance categories [14, 31, 32]. Behaviors significantly associated with either insufficient (≤7 hours) or long (≥9 hours) sleep duration and obesity were identified as confounders and included along with demographic variables in final models. These 5 behaviors included feeling sad and hopeless, being a current smoker, drinking nondiet soda or pop, using a computer or playing video games for 3 or more hours on an average school day, and being physically active for at least 60 minutes daily. Feeling sad and hopeless was different from the other confounders in that it was more likely to occur at both short (AOR = 1.79) and long (AOR = 1.26) sleep durations.
Table 2.
Associations of insufficient and long sleep duration, and obesity with other health-related behaviors—US high school students.
| Health-related Behavior | Insufficient sleep duration (≤7 hours)a | Long sleep duration (≥9 hours)a | Obese (BMI ≥ 95th percentile)b | ||||||
| AOR | 95% CI | P value | AOR | 95% CI | P-value | AOR | 95% CI | P value | |
| Felt sad and hopelessc | 1.79 | 1.61–1.99 | 0.0000 | 1.26 | 1.08–1.46 | 0.0032 | 1.26 | 1.11−1.43 | 0.0006 |
| Current smokerd | 1.63 | 1.45–1.84 | 0.0000 | 1.10 | 0.90–1.34 | 0.3604 | 1.31 | 1.15–1.50 | 0.0001 |
| Drank nondiet sodae | 1.26 | 1.17–1.36 | 0.0000 | 1.14 | 0.96–1.34 | 0.1292 | 1.15 | 1.02–1.29 | 0.0237 |
| Computer/video gamesf | 1.61 | 1.46–1.77 | 0.0000 | 1.10 | 0.91–1.33 | 0.2992 | 1.29 | 1.15–1.44 | 0.0000 |
| Television viewingg | 1.02 | 0.93–1.11 | 0.6490 | 1.08 | 0.93–1.27 | 0.2999 | 1.48 | 1.33–1.64 | 0.0000 |
| Physically activeh | 0.82 | 0.75–0.90 | 0.0000 | 1.28 | 0.99–1.65 | 0.0571 | 0.63 | 0.55–0.72 | 0.0000 |
| Ate fruits and vegetablesi | 0.83 | 0.75–0.92 | 0.0008 | 1.50 | 1.27–1.76 | 0.0000 | 1.02 | 0.90–1.15 | 0.7393 |
| Drank milkj | 0.86 | 0.77–0.97 | 0.0145 | 1.41 | 1.16–1.71 | 0.0008 | 1.10 | 0.95–1.28 | 0.1926 |
AOR = odds ratio adjusted for sex, race/ethnicity, and grade. Referent for insufficient (≤7 hours) and long (≥9 hours) sleep duration is 8 hours of sleep.
CI = confidence interval.
aOn an average school night.
bBased on self-reported height and weight, body mass index (BMI = weight [kg]/height [m]2) ≥95th percentile using growth charts developed by the Centers for Disease Control and Prevention for youth aged 2–20 years.
cAlmost every day for 2 or more weeks so that they stopped doing some usual activities.
dSmoked cigarettes on at least 1 day during the 30 days before the survey.
eDrank a can, bottle, or glass of soda or pop, not including diet soda or diet pop, at least one time per day during the 7 days before the survey.
fUsed a computer for something that was not school work or played video games for 3 or more hours per day on an average school day.
gWatched television for 3 or more hours per day on an average school day.
hWere physically active doing any kind of physical activity that increased their heart rate and made them breathe hard some of the time for at least 60 minutes per day on all 7 days during the 7 days before the survey.
iAte fruits and vegetables 5 or more times per day during the 7 days before the survey.
jDrank 3 or more glasses of milk per day during the 7 days before the survey.
3.5. Association between Sleep Duration and Obesity
Using logistic regression models which controlled for sex, race/ethnicity, grade, and confounding behaviors, we detected a significant quadratic (U-shaped) association (P = 0.0330) between sleep duration and obesity, but no evidence of a linear association (P = 0.4977) (Table 3). The unadjusted prevalence of obesity was approximately 12% among students who reported sleeping between 6 and 9 hours on an average school night and increased slightly among students who reported shorter (16.5% at ≤4 hrs) or longer (15.1% at ≥10 hrs) sleep duration.
Table 3.
Linear and quadratic associations between obesity and sleep duration—US high school students.
|
Demographic subgroup (N) |
Prevalence of obesitya by sleep durationb | ||||||||
| ≤4 hrs | 5 hrs | 6 hrs | 7 hrs | 8 hrs | 9 hrs | ≥10 hrs | P Value for trendc | ||
| % 95% CI (N) |
% 95% CI (N) |
% 95% CI (N) |
% 95% CI (N) |
% 95% CI (N) |
% 95% CI (N) |
% 95% CI (N) |
Linear | Quadratic | |
| Total Population (23,579) | 16.5 14.2–19.2 (1,355) | 13.9 12.4–15.5 (2,428) | 11.5 10.5–12.5 (5,306) | 12.2 10.9–13.6 (7,124) | 12.1 10.9–13.4 (5,513) | 12.4 10.4–14.7 (1,431) | 15.1 10.6–21.1 (422) | .4977 | .0330 |
| Sex | |||||||||
| Female (11,939) | 14.6 11.3–18.7 (665) | 10.3 8.6–12.4 (1,401) | 8.3 7.2–9.5 (2,842) | 7.5 6.3–9.0 (3,522) | 8.3 7.0–9.9 (2,650) | 12.1 9.3–15.6 (657) | 14.1 8.8–21.8 (202) | .9653 | .0004 |
| Male (11,640) | 18.4 14.6–23.0 (690) | 18.4 16.1–21.1 (1,027) | 15.1 13.3–17.1 (2,464) | 16.2 14.0–18.8 (3,602) | 15.3 13.2–17.6 (2,863) | 12.5 9.8–15.9 (774) | 15.9 9.8–24.7 (220) | .3432 | .8428 |
CI = confidence interval. N = unweighted sample size.
aBased on self-reported height and weight, body mass index (BMI = weight [kg]/height [m]2) ≥95th percentile using growth charts developed by the Centers for Disease Control and Prevention for youth aged 2–20 years.
bOn an average school night.
cAdjusted for sex, race/ethnicity, grade, feeling sad and hopeless, current smoking, drinking nondiet soda or pop daily, using computers (non-school-related) or playing video games 3 or more hours per day, and being physically active for at least 60 minutes 7 days per week.
Next, we tested whether the association between sleep duration and obesity varied by sex, race/ethnicity, or grade. A significant interaction was detected for the quadratic (U-shaped) association by sex (Wald F = 9.84, P = 0.0024), but not race/ethnicity (Wald F = 0.51, P = 0.6763) or grade (Wald F = 1.40, P = 0.2480). Because of the significant interaction by sex, we ran separate analyses for females and males (Table 3). We found no evidence of significant interactions for a linear association by sex, race/ethnicity, or grade.
Among female students, controlling for demographic characteristics and confounding behaviors we detected a significant quadratic (U-shaped) association (P = 0.0004) between sleep duration and obesity, but no evidence of a linear association (P = 0.9653). The prevalence of obesity was lowest (approximately 8%) among female students who reported sleeping between 6 and 8 hours on an average school night and increased among those who reported shorter (14.6% at ≤4 hrs) or longer (14.1% at ≥10 hrs) sleep duration (Table 3). Among male students, controlling for demographic characteristics and confounding behaviors, we did not detect a significant linear or quadratic association between sleep duration and obesity (Table 3).
Finally, because of the significant quadratic association between sleep duration and obesity among females, we compared crude odds ratios (ORs) and adjusted odds ratios (AORs) for obesity by sleep duration among female students (Table 4). We chose the sleep duration with the lowest prevalence of obesity (7 hours) as the referent group. Compared to females who slept 7 hours on an average school night, those who slept fewer hours (OR = 2.10, ≤4 hrs; OR = 1.41, 5 hrs) and those who slept more hours (OR = 1.69, 9 hrs; OR = 2.00, ≥10 hrs) were more likely to be obese. Controlling for demographic characteristics and confounding behaviors attenuated, but did not eliminate, the statistical significance of adjusted odds ratios for obesity at shorter and longer sleep durations. Compared to female students who slept 7 hours on an average school night, those who slept ≤4 hours (AOR = 1.50) and those who slept 9 hours (AOR = 1.55) were more likely to be obese. The AOR for ≥10 hours (AOR = 1.50) was similar in magnitude to the odds ratio for 9 hours of sleep and probably fell short of statistical significance because of small numbers of females who slept ≥10 hours (n = 202). Combining sleep duration categories of 9 hours and ≥10 hours, we found that females who slept ≥9 hours were more likely to be obese (AOR = 1.54; 95% CI: 1.13–2.10) than females who slept 7 hours. Because there was no statistical evidence for a significant linear or quadratic association between sleep duration and obesity (after controlling for potential confounders) among male students, we did not compare crude and adjusted odds ratios for obesity at different sleep durations among male students.
Table 4.
Odds ratios for obesity, aby sleep duration—US female high school students.
| Independent variables | (N = 11,939) | % | OR | 95% CI | AOR | 95% CI |
|---|---|---|---|---|---|---|
| Sleep duration (hours)b | ||||||
| ≤4 | (665) | 14.6 | 2.10 | 1.47−2.99 | 1.50 | 1.05−2.15 |
| 5 | (1,401) | 10.3 | 1.41 | 1.06−1.88 | 1.17 | 0.87–1.58 |
| 6 | (2,842) | 8.3 | 1.10 | 0.87−1.39 | 1.00 | 0.78–1.27 |
| 7 | (3,522) | 7.5 | 1.00 | (referent) | 1.00 | (referent) |
| 8 | (2,650) | 8.3 | 1.11 | 0.87−1.42 | 1.11 | 0.86–1.43 |
| 9 | (657) | 12.1 | 1.69 | 1.17−2.42 | 1.55 | 1.07–2.25 |
| ≥10 | (202) | 14.1 | 2.00 | 1.21−3.30 | 1.50 | 0.91–2.49 |
| Race/ethnicity | ||||||
| White | (5,389) | 6.8 | 1.00 | (referent) | ||
| Black | (2,391) | 15.1 | 2.46 | 1.85–3.27 | ||
| Hispanic | (3,132) | 11.8 | 1.81 | 1.44–2.27 | ||
| Other | (1,027) | 8.0 | 1.17 | 0.79–1.75 | ||
| Grade | ||||||
| 9th | (2,828) | 9.0 | 0.89 | 0.70–1.12 | ||
| 10th | (2,860) | 8.7 | 0.87 | 0.70–1.09 | ||
| 11th | (3,132) | 8.5 | 0.86 | 0.66–1.13 | ||
| 12th | (3,119) | 9.4 | 1.00 | (referent) | ||
| Felt sad and hopelessc | ||||||
| Yes | (4,266) | 11.5 | 1.35 | 1.14–1.61 | ||
| No | (7,673) | 7.5 | 1.00 | (referent) | ||
| Current smokerd | ||||||
| Yes | (2,135) | 12.2 | 1.63 | 1.35–1.97 | ||
| No | (9,804) | 8.1 | 1.00 | (referent) | ||
| Drank nondiet sodae | ||||||
| Yes | (3,303) | 11.0 | 1.14 | 0.95–1.36 | ||
| No | (8,636) | 8.2 | 1.00 | (referent) | ||
| Computer/video gamesf | ||||||
| Yes | (2,438) | 11.3 | 1.26 | 1.05–1.51 | ||
| No | (9,501) | 8.3 | 1.00 | (referent) | ||
| Physically activeg | ||||||
| Yes | (1,272) | 6.8 | 0.75 | 0.57–0.99 | ||
| No | (10,667) | 9.2 | 1.00 | (referent) |
N = unweighted sample size. OR = unadjusted odds ratio. AOR = adjusted (for other variables in the model) odds ratio. CI = confidence interval.
aBased on self-reported height and weight, body mass index (BMI = weight [kg]/height [m]2) ≥95th percentile using growth charts developed by the Centers for Disease Control and Prevention for youth aged 2–20 years.
bOn an average school night.
cAlmost every day for 2 or more weeks so that they stopped doing some usual activities.
dSmoked cigarettes on at least 1 day during the 30 days before the survey.
eDrank a can, bottle, or glass of soda or pop, not including diet soda or diet pop, at least one time per day during the 7 days before the survey.
fUsed a computer for something that was not school work or played video games for 3 or more hours per day on an average school day.
gWere physically active doing any kind of physical activity that increase their heart rate and made them breathe hard some of the time for at least 60 minutes per day on all 7 days during the 7 days before the survey.
4. Discussion
Nearly 7 out of 10 high school students reported sleeping less than 8 hours on an average school night. This finding is consistent with the high prevalence of insufficient sleep reported in other studies [2, 33]. In our study, the association between sleep duration and obesity differed by sex, but not by race/ethnicity or grade. Controlling for demographic characteristics and behavioral confounders, we found a significant quadratic (U-shaped) association between sleep duration on an average school night and obesity among female students, but not among male students. No significant linear associations were found among any demographic subgroups. Among female students, the lowest obesity prevalence occurred at approximately 7 hours of sleep with greater obesity prevalence occurring at shorter and longer sleep durations. This type of U-shaped association is often seen between sleep duration and mortality, heart disease, type 2 diabetes, and obesity among adults [5]. Previous studies of the association between sleep duration and obesity among adults have sometimes found differences by sex, with a negative linear association among males and a U-shaped association among females [8, 13]. One previous study involving a nationally representative sample of middle and high school students found differences by sex, with a negative linear association between sleep duration and obesity among male students and no association among female students [33]. Factors responsible for differences in the findings from that study compared to our study may include the addition of 7th and 8th grade students to the Add Health Study population [33]. Also, that study controlled for parental education and physical activity and inactivity, but not for depressive symptoms, smoking, or soda consumption [33].
While there is experimental evidence for metabolic pathways whereby shortened sleep duration might lead to obesity, there are currently no clearly delineated mechanisms proposed for how longer sleep duration might lead to the onset of obesity [5, 8–11]. Sleep restriction in healthy adults has been shown to result in decreased leptin levels which result in decreased satiety and increased ghrelin levels which result in increased appetite [8, 9]. Alterations in these hormone levels may subsequently lead to increased caloric intake and weight gain among persons with shortened sleep duration. A possible explanation for the association between prolonged sleep duration and obesity among females involves the dysfunctional sleep patterns often associated with both obesity and depression. Prospective studies of children and adolescents have found that obesity is associated with later development of depressive symptoms, and juvenile onset of depression increases risk for becoming overweight in adulthood [34, 35]. More than 90% of children and adolescents with major depressive disorder report subjective sleep complaints and obese children experience more fragmented sleep, with frequent awakenings and episodes of sleep apnea, compared to normal-weight children [12, 35]. It is possible that the dysfunctional sleep patterns experienced by depressed and/or obese youth may, in some cases, result in extended sleep durations in an attempt to compensate for poor-quality and/or interrupted sleep. In our study, having feelings of sadness and hopelessness was more likely to occur at both short and long sleep durations. Controlling for demographic and behavioral confounders (including sadness/hopelessness) in our logistic regression model attenuated, but did not eliminate, the increased odds of being obese among female students who reported sleeping either 4 or less hours or 9 or more hours (compared to 7 hours) on an average school night.
Age-dependent effects, such as the decreased sleep needs of adults compared to young children, may account for the different patterns of association (e.g., U-shaped among adults versus negative linear among children) between sleep duration and obesity [5]. For example, if there is an adverse effect on obesity risk from “long sleep duration” in excess of physiological needs, this could be evidenced among adults who sleep as much as 10 or 12 hours per day. Young children, with much longer physiological sleep needs, might not show an adverse effect of “long sleep duration” until 18 hours of sleep per day, which very few children would be able to accrue [5]. Explanations for sex-related differences in the association between sleep duration and obesity may include sex-related differences in the physiology of puberty, particularly with respect to body composition, for example, the increasing adiposity typically seen among females and decreasing adiposity typically seen among males as they pass through puberty [33]. Sex-related differences in sleep physiology, the psychosocial correlates of obesity and physiologic pathways mediating the association between depression and BMI have been noted as well [20, 33].
Our study has several strengths. The data are from nationally representative samples of students in grades 9–12, a population which includes older adolescents for whom nationally representative data on sleep duration and obesity are relatively limited. In our analyses, we were able to control for a variety of health behaviors found to be associated both with sleep duration and obesity, and which might therefore confound their relationship. Finally, by combining two large national datasets, we obtained increased statistical power enhancing our ability to characterize the association between sleep duration and obesity at the extremes of long and short sleep duration and among demographic subgroups.
Many of the limitations of our study, such as the lack of objective measures of sleep duration, are shared by other published studies examining the association between sleep duration and obesity [5, 8, 13]. We relied on a single self-report for sleep duration on an average school night. Also, data were not available on other potentially important factors such as variation in sleep duration through the week, including weekends, actual bedtime, and wake times, and sleep quality, including the presence of snoring or breathing difficulties that might suggest undiagnosed obstructive sleep apnea. In addition, we used BMI based on self-reported height and weight to classify students with respect to obesity. A national study of adolescents found the correlation (r =.92) of BMI and the specificity (0.996) of obesity status (BMI ≥ 95th percentile) based on BMI calculated from self-reported versus measured height and weight was very high [36]. Although sensitivity (0.722) of obesity status based on self-report was not as high, using self-reported height and weight correctly classified 96% of teens with respect to obesity, and girls were no more likely than boys to be misclassified using self-reported height and weight [36]. Finally, our study is cross-sectional in design, and therefore direction of causality cannot be inferred. Sleep duration could affect weight gain, but obesity could also impact the duration of sleep. Indeed, the association between short and long sleep duration and obesity may not necessarily reflect a causal relationship, but could be a marker indicating that naturally short or long sleepers are at-risk populations for obesity, chronic disease, and mortality [37].
5. Conclusion
The high prevalence of insufficient sleep among adolescents, with its deleterious effects on neurobehavioral function (i.e., mood, memory, attention, and cognition) and associated increases in motor vehicle accidents and impaired school performance, provides a strong rationale to promote greater duration and quality of sleep among teens [5, 38, 39]. However, with respect to obesity prevention, the current literature suggests that sex-related differences (such as found in our study) and other inconsistencies in the association between sleep duration and obesity among children, adolescents, and adults, coupled with the lack of clearly defined causal pathways, make it premature to recommend alteration of sleep patterns as an effective intervention to prevent the onset of obesity in the general population or enhance weight loss among the clinically obese [5]. There are currently no interventional or observational studies showing that weight loss can be achieved in the general community or particular subpopulations, through advice to change sleep duration. Still, the consistent negative linear association between sleep duration and obesity seen among younger children and the positive impact of adequate sleep generally have led some to suggest adequate sleep as an adjunct to other lifestyle measures in the prevention of childhood obesity [37]. In the absence of definitive evidence as to what constitutes “adequate” sleep for the purpose of promoting healthy weight, one approach is to provide the appropriate circumstances and environment for sleep and reduce external interference with sleep through the maintenance of bedtime routines and limiting television viewing and use of electronic devices near bedtimes and in bedrooms [37, 40]. While there may be little risk in taking such a pragmatic approach to the promotion of adequate sleep as an adjunct strategy in the fight against childhood obesity, it is clear that more needs to be known about the association between sleep and obesity. In addition to a better understanding of the mechanisms underlying the association, further research is needed to determine the characteristics of sleep patterns that may promote healthy weight and whether behavioral programs aimed at changing sleep duration as a means of weight control are safe and effective.
Confilct of Interests
The authors have no conflict of interests to declare.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.National Commission on Sleep Disorders Research. Wake UP American: A National Sleep Alert. Vol. 2. Washington, DC, USA: Government Printing Office; 1994. (Working Group Reports). [Google Scholar]
- 2.National Sleep Foundation. 2006 Sleep in America Poll. Washington, DC, USA: National Sleep Foundation; 2006. [Google Scholar]
- 3.Wheaton AG, Liu Y, Perry GS, Croft JB. Effect of short sleep duration on daily activities-United States, 2005–2008. Morbidity and Mortality Weekly Report. 2011;60(8):239–242. [PubMed] [Google Scholar]
- 4.Institute of Medicine. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington, DC, USA: National Academies Press; 2006. [PubMed] [Google Scholar]
- 5.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Medicine Reviews. 2008;12(4):289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. Journal of the American Medical Association. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. Journal of the American Medical Association. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 8.Knutson KL, Spiegel K, Penev P, van Cauter E. The metabolic consequences of sleep deprivation. Sleep Medicine Reviews. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spiegel K, Tasali E, Penev P, van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 10.Spiegel K, Leproult R, van Cauter E. Impact of sleep debt on metabolic and endocrine function. The Lancet. 1999;354(9188):1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 11.Spiegel K, Tasali E, Leproult R, van Cauter E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology. 2009;5(5):253–261. doi: 10.1038/nrendo.2009.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang G, Dietz WH. Economic burden of obesity in youths aged 6 to 17 years: 1979–1999. Pediatrics. 2002;109(5):p. E81. doi: 10.1542/peds.109.5.e81. [DOI] [PubMed] [Google Scholar]
- 13.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008;16(2):265–274. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 14.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2009. Morbidity and Mortality Weekly Report. 2010;59(5):1–142. [PubMed] [Google Scholar]
- 15.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2007. Morbidity and Mortality Weekly Report. 2008;57(4):1–131. [PubMed] [Google Scholar]
- 16.Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 youth risk behavior survey questionnaire. Journal of Adolescent Health. 2002;31(4):336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 17.Brener ND, Kann L, Kinchen SA, et al. Methodology of the youth risk behavior surveillance system. Morbidity and Mortality Weekly Report. 2004;53(12):1–13. [PubMed] [Google Scholar]
- 18.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Advance Data. 2000;2000(314):1–27. Hyattsville, Md, USA, National Center for Health Statistics, 2000; DHHS publication no. (PHS) 2000-1250. [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. The Surgeon General’s Vision for a Healthy and Fit Nation. Rockville, Md, USA: U.S. Department of Health and Human Services, Office of the Surgeon General; 2010. [PubMed] [Google Scholar]
- 20.Dockray S, Susman EJ, Dorn LD. Depression, cortisol reactivity, and obesity in childhood and adolescence. Journal of Adolescent Health. 2009;45(4):344–350. doi: 10.1016/j.jadohealth.2009.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lowry R, Galuska DA, Fulton JE, Wechsler H, Kann L. Weight management goals and practices among U.S. high school students: associations with physical activity, diet, and smoking. Journal of Adolescent Health. 2002;31(2):133–144. doi: 10.1016/s1054-139x(01)00408-6. [DOI] [PubMed] [Google Scholar]
- 22.Tomeo CA, Field AE, Berkey CS, Colditz GA, Frazier AL. Weight concerns, weight control behaviors, and smoking initiation. Pediatrics. 1999;104(4):918–924. doi: 10.1542/peds.104.4.918. [DOI] [PubMed] [Google Scholar]
- 23.Utter J, Scragg R, Schaaf D, Fitzgerald E, Wilson N. Correlates of body mass index among a nationally representative sample of New Zealand children. International Journal of Pediatric Obesity. 2007;2(2):104–113. doi: 10.1080/17477160601127988. [DOI] [PubMed] [Google Scholar]
- 24.Dehghan M, Akhtar-Danesh N, Merchant AT. Childhood obesity, prevalence and prevention. Nutrition Journal. 2005;4, article 24 doi: 10.1186/1475-2891-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27(7):1351–1358. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 26.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug and Alcohol Dependence. 2001;64(1):1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 27.Weiss A, Xu F, Storfer-Isser A, Thomas A, Ievers-Landis CE, Redline S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep. 2010;33(9):1201–1209. doi: 10.1093/sleep/33.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaina A, Sekine M, Hamanishi S, et al. Daytime sleepiness and associated factors in Japanese school children. Journal of Pediatrics. 2007;151(5):518.e4–522.e4. doi: 10.1016/j.jpeds.2007.04.036. [DOI] [PubMed] [Google Scholar]
- 29.Chen MY, Wang EK, Jeng YJ. Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health. 2006;6, article 59 doi: 10.1186/1471-2458-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Research Triangle Institute. SUDAAN, version 10.0.1 [computer program]. Version 10.0.1. Triangle Park, NC, USA, Research Triangle Institute, 2008.
- 31.US Dept of Health and Human Services. Healthy People 2010. 2nd edition. Vol. 2. Washington, DC, USA: US Government Printing Office; 2000. (With Understanding and Improving Health and Objectives for Improving Health). [Google Scholar]
- 32.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC, USA: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 33.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. Journal of Pediatrics. 2005;147(6):830–834. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 34.Boutelle KN, Hannan P, Fulkerson JA, Crow SJ, Stice E. Obesity as a prospective predictor of depression in adolescent females. Health Psychology. 2010;29(3):293–298. doi: 10.1037/a0018645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wojnar J, Brower KJ, Dopp R, et al. Sleep and body mass index in depressed children and healthy controls. Sleep Medicine. 2010;11(3):295–301. doi: 10.1016/j.sleep.2009.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106(1):52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 37.Taheri S, Thomas GN. Is sleep duration associated with obesity—where do U stand? Sleep Medicine Reviews. 2008;12(4):299–302. doi: 10.1016/j.smrv.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 38.Dahl RE, Lewin DS. Pathways to adolescent health: sleep regulation and behavior. Journal of Adolescent Health. 2002;31(6):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 39.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. British Medical Journal. 2002;324(7346):1125–1130. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Archives of Disease in Childhood. 2006;91(11):881–884. doi: 10.1136/adc.2005.093013. [DOI] [PMC free article] [PubMed] [Google Scholar]


