Abstract
Objectives
The differential roles of psychotherapy and pharmacotherapy in the management of bipolar (BP) II depression are unknown. As a first step toward exploring this issue, we conducted a pilot study to evaluate the feasibility and acceptability of comparing a bipolar-specific psychotherapy [Interpersonal and Social Rhythm Therapy (IPSRT)] to quetiapine as treatments for BP-II depression.
Methods
Unmedicated individuals (n = 25) meeting DSM-IV criteria for BP-II disorder, currently depressed, were randomly assigned to weekly sessions of IPSRT (n = 14) or quetiapine (n = 11), flexibly dosed from 25–300 mg. Participants were assessed with weekly measures of mood and followed for 12 weeks. Treatment preference was queried prior to randomization.
Results
Using mixed effects models, both groups showed significant declines in the 25-item Hamilton Rating Scale for Depression [F(1,21) = 44, p < 0.0001] and Young Mania Rating Scale [F(1,21) = 20, p = 0.0002] scores over time but no group × time interactions. Dropout rates were 21% (n = 3) and 27% (n = 3) in the IPSRT and quetiapine groups, respectively. Overall response rates (defined as ≥ 50% reduction in depression scores without an increase in mania scores) were 29% (n = 4) in the IPSRT group and 27% (n = 3) in the quetiapine group. Measures of treatment satisfaction were high in both groups. Treatment preference was not associated with outcomes.
Conclusions
Outcomes in participants with BP-II depression assigned to IPSRT monotherapy or quetiapine did not differ over 12 weeks in this small study. Follow-up trials should examine characteristics that predict differential response to psychotherapy and pharmacotherapy.
Keywords: bipolar II disorder, pharmacotherapy, psychotherapy, treatment
Bipolar (BP) II disorder is a highly recurrent disorder (1) associated with elevated levels of psychosocial impairment (2, 3), disability (4), comorbidity (3, 5), and suicidal ideation/behaviors (6, 7) . Despite the significant suffering associated with BP-II disorder, relatively little is known about how best to treat this illness (8). Uncertainty about management of BP-II is complicated by the fact that depression is the dominant pole of BP-II disorder (1), a phase of the disorder for which we have relatively few effective treatments (9, 10).
Despite the large side effect burden associated with medications used to treat BP disorders (8, 11) and the large lacunae in the evidence base with respect to their efficacy (12), alternatives to pharmacotherapy are rarely considered in mainstream treatment algorithms (8, 13). Psychotherapy, which arguably has no side effects (14), may play an important role in the management of BP-II disorder as many individuals suffering from the illness struggle with issues that lend themselves to psychosocial remediation. For instance, recognition and treatment of BP-II disorder often lags years behind initial manifestation of symptoms (15), a problem which is associated with a chronic course of illness (1) and subsequent erosion in psychosocial functioning (2, 4). Further, individuals with BP-II disorder typically have difficulty distinguishing among rapid mood shifts and subtle mood states (i.e., hypomania) that characterize BP-II (16), and yet ability to recognize mood symptoms likely constitutes the first step toward effective disease management. Bipolar-specific psychotherapies can provide patients with strategies for understanding their illness, managing symptoms, and enhancing psychosocial functioning (17, 18).
Although use of psychotherapy alone as an alternative to pharmacotherapy is likely contraindicated in BP-I disorder, it is not unreasonable to consider this approach in BP-II disorder where individuals are at low risk of experiencing fully syndromal manic episodes or psychosis. Despite the compelling argument to be made for its inclusion in the therapeutic armamentarium for BP-II disorder, the literature on psychotherapy for the treatment of BP-II disorder is sparse. When used in combination with mood stabilizers, bipolar-specific psychotherapies have been shown to shorten time to recovery in patients suffering from BP disorders, including a subset of individuals diagnosed with BP-II disorder (19). A small group of individuals meeting criteria for BP-II disorder who received group psychoeducation in addition to pharmacotherapy had better long term (five year) outcomes than patients receiving a control psychosocial intervention (20). We have previously demonstrated feasibility of treating patients meeting criteria for BP-II depression with psychotherapy alone (21). There are no comparative trials of psychotherapy and pharmacotherapy.
Interpersonal and Social Rhythm Therapy (IPSRT) is an evidence-based psychotherapy for bipolar disorder (22). In randomized clinical trials where IPSRT was used in combination with medication, IPSRT has been shown to reduce time to recovery from an episode of depression (19), decrease the likelihood of mood episode recurrence (23), and improve psychosocial and occupational functioning (24, 25). We have modified IPSRT for use as monotherapy with individuals who have BP-II disorder (16, 21).
In order to advance understanding of the roles of psychotherapy and pharmacotherapy in the management of BP-II depression, we conducted a small randomized trial of IPSRT versus quetiapine, a second generation antipsychotic that has demonstrated efficacy as treatment for BP-II depression (26–28). The primary goal was to evaluate the feasibility and acceptability of this approach. A secondary goal was to examine symptomatic and functional outcomes over a 12-week period in patients assigned to the two treatment conditions.
Methods
Study design
All study procedures were reviewed and approved by the Biomedical Institutional Review Board of the University of Pittsburgh, Pittsburgh, PA, USA. Potential participants provided informed written consent after receiving a complete description of the study. Participants were recruited by word of mouth from other investigators and clinicians.
Seventy-six potential participants consented to screening for inclusion in the protocol during the study period (December 9, 2006 through July 1, 2010). A total of 25 participants were deemed eligible for inclusion in the protocol based on the following criteria: (i) age 18 to 65 years; (ii) lifetime diagnosis of BP-II disorder, currently depressed; (iii) Hamilton Rating Scale for Depression (HRSD-17) (29) score ≥ 15; (iv) Young Mania Rating Scale (YMRS) (30) score ≤ 10; and (v) willingness to accept randomization to medication or psychotherapy. Individuals were excluded from the study if they met any of the following criteria: (i) concurrent treatment with psychoactive medications; (ii) diagnosis of substance abuse or dependence within the prior six months; (iii) diagnosis of borderline or antisocial personality disorder; and (iv) unstable medical condition that could produce symptoms that would confound accurate assessment of mood symptoms (e.g., untreated thyroid disease). Six of the 25 eligible participants were receiving psychotropic medication(s) prior to study entry. They were tapered off of medication and reassessed to determine continued eligibility. One week off of psychotropic medications, all six participants continued to meet eligibility criteria (five assigned to IPSRT and one assigned to quetiapine; this difference was not statistically significant, p = 0.18).
Demographic data and psychiatric treatment history were recorded on standardized research forms. Lifetime and current psychiatric diagnoses were assigned using the Structured Clinical Interview for DSM-IV–clinician version [SCID-I (31) and SCID-II (32)]. Depressive symptoms were assessed using the 17-item HRSD, the expanded 25-item version of the HRSD that includes reverse neurovegetative symptoms (33), and the Montgomery-Åsberg Depression Rating Scale (MADRS) (34). Mania symptoms were rated using the YMRS. Global functioning was evaluated using the Clinical Global Impressions Scale–Bipolar version (CGI-BP) which includes separate clinician ratings for depression and mania on two 7-point likert-type scales (35). Anxiety symptoms were assessed using the self-report Beck Anxiety Inventory (BAI) (36). Research assessments were conducted by raters who were not involved in the participants’ treatment. Inter-rater reliability as measured by intraclass correlations (ICC) were excellent: ICC = 0.99, 0.99, and 0.98 for YMRS, HRSD-25, and HRSD-17, respectively. Satisfaction with the intervention was assessed at visit 12 with the Client Satisfaction Questionnaire (CSQ) (37) which yields scores ranging from 8 to 32 with higher scores indicating greater levels of satisfaction. Weight was measured at each treatment visit. Participants were asked prior to randomization whether they preferred treatment with psychotherapy or medication.
Participants were randomly assigned using a permuted block strategy (38) to either IPSRT (n = 14) or quetiapine (n = 11). The trial ended prior to completing expected enrollment (n = 30), and therefore the cell sizes were uneven (truncation of randomization occurred in the middle of a block).
IPSRT
Those assigned to IPSRT received weekly, 45-minute, individual psychotherapy sessions. IPSRT is described in greater detail in the manual (22). Briefly, IPSRT combines a focus on interpersonal relationships (39) with psychoeducation and a behavioral intervention designed to modify social rhythms. Psychoeducation in IPSRT focuses on understanding BP-II disorder with a focus on identification of hypomania and mixed or dysphoric mood states. The social rhythm component of IPSRT postulates that disordered circadian biology contributes to the development and maintenance of psychiatric symptoms and that helping patients to develop more regular routines and social patterns can help regulate underlying circadian abnormalities, thereby reducing symptoms and improving outcomes. Patients complete a weekly self-report assessment, the Social Rhythm Metric (SRM) (40), to track the regularity of their social routines. Patients are encouraged to develop more regular sleep and activity patterns and modify their social interactions in order to promote mood stability. Special issues arising in the use of IPSRT for BP-II disorder are described elsewhere (16). IPSRT sessions were delivered by three master’s level therapists, and all therapy sessions were audio- or video- recorded for fidelity monitoring.
Quetiapine
Those assigned to quetiapine met weekly with a psychiatrist for medication management. Quetiapine was flexibly dosed with a starting dose of 50 mg per day, increased weekly by 50 mg/day as tolerated to a maximum of 300 mg/day.
Participants in either condition who experienced sleep disturbances that could not be managed with study treatments alone could receive low doses of lorazepam at any point during the study at the discretion of the treating psychiatrist.
Data analysis
For baseline demographic and clinical characteristics, Wilcoxon tests and Fisher Exact tests were used to compare continuous and categorical variables, respectively. Longitudinal data were analyzed using an intent-to-treat approach with mixed effect models with fixed terms including group and time, and group by time interaction. Time was treated as a continuous variable for those variables measured frequently and as a repeated factor for those variables taken only at baseline and 12 week follow-ups. Individual variabilities were taken into account by including random intercept and random slope for linear mixed models and participant as a random term for repeated measures mixed models.
Results
There were no significant differences in baseline demographic and clinical characteristics of the two groups (Table 1). When asked about treatment preference prior to randomization, 40% (10/25) expressed a preference for medication, 40% (10/25) a preference for psychotherapy, and 20% (5/25) no preference. Two participants met all study eligibility requirements but did not come to a single treatment session (one in each treatment condition). In the IPSRT condition, fifteen percent (n = 2) dropped out after having had at least one study visit (mean number of visits prior to drop out = 3.5 ± 2.1; range: 2–5). In the quetiapine condition, 20% (n = 2) dropped out after having had at least one study visit (mean number of visits prior to drop out, 4 ± 1.4; range: 3–5). Mean number of IPSRT sessions over 12 weeks was 8.5 (± 2.8). Mean number of medication management sessions attended by those assigned to quetiapine was 8.0 (± 2.6). Mean dose of quetiapine at week 12 (n = 8) was 243.8 mg (± 67.8; range: 25–300). Twenty-one percent (n = 3) of the IPSRT group received adjunctive lorazepam (mean dose 1.3 ± 0.6 mg) versus 0% assigned to quetiapine, but this was not statistically significant.
Table 1.
Baseline demographic and clinical characteristics of participants assigned to Interpersonal and Social Rhythm Therapy (IPSRT) and quetiapine
| Variable | IPSRT (n = 14) | Quetiapine (n = 11) | p-value | ||
|---|---|---|---|---|---|
| Mean (SD) or n (%) |
Median [range] | Mean (SD) or n (%) |
Median [range] | ||
| Age, mean (SD) | 40.1 (11.7) | 36.9 [26.0–63.6] | 32.1 (12.8) | 25.6 [19.4–59.3] | 0.08 |
| Female, n (%) | 7 (50) | 8 (73) | 0.41 | ||
| White, n (%) | 13 (93) | 11 (100) | 1.00 | ||
| Education, years, mean (SD) | 14.7 (2.1) | 14.0 [12–18] | 16.1 (2.4) | 15.5 [13–21] | 0.19 |
| Marital status, n (%) | 0.90 | ||||
| Married | 5 (36) | 3 (27) | |||
| Never married | 7 (50) | 8 (73) | |||
| Separated or divorced | 1 (7) | 0 (0) | |||
| Employment, n (%) | |||||
| Full time, part time, homemaker | 7 (50) | 5 (45) | 0.83 | ||
| Student | 1 (7) | 2 (18) | |||
| Disabled, unemployed | 4 (29) | 2 (18) | |||
| HRSD-17 score, mean (SD) | 20.0 (3.7) | 20.0 [15–26] | 18.2 (2.1) | 18.5 [15–21] | 0.27 |
| HRSD-25 score, mean (SD) | 25.0 (3.5) | 25.0 [20–31] | 24.6 (2.7) | 25.0 [21–29] | 0.44 |
| YMRS score, mean (SD) | 6.5 (3.0) | 6.5 [2–13] | 7.8 (4.2) | 6.5 [2–16] | 0.58 |
| MADRS score, mean (SD) | 25.1 (6.4) | 24.5 [14–41] | 25.7 (4.8) | 25.5 [20–33] | 0.75 |
| BAI score, mean (SD) | 13.8 (9.1) | 15.0 [0–32] | 12.2 (7.9) | 14.0 [1–25] | 0.74 |
| GAF score, mean (SD) | 55.1 (2.9) | 55.0 [51–60] | 58.0 (2.2) | 58.0 [55–60] | 0.07 |
| Weight (pounds) | 187 (56) | 177 [106–274] | 173 (67) | 156 [107–336] | 0.35 |
| Duration of index depressive episode (weeks) | 53 (100) | 23 [2–392] | 19 (27) | 11 [3–92] | 0.11 |
| No. of prior depressive episodes (lifetime) | 5.1 (3.7) | 4.0 [1–12] | 12.3 (17.7) | 4.0 [1–50] | 0.60 |
| No. of prior hypomanic episodes (lifetime)a | 3.6 (3.3) | 2.0 [1–11] | 19.7 (26.3) | 6.0 [3–50] | 0.15 |
| DSM-IV Axis I comorbidities, n (%) | |||||
| Substance use disorder (lifetime)b | 2 (14) | 5 (45) | 0.18 | ||
| Anxiety disorder (current)c | 8 (57) | 5 (45) | 0.70 | ||
HRSD = Hamilton Rating Scale for Depression; YMRS = Young Mania Rating Scale; MADRS = Montgomery-Åsberg Depression Rating Scale; BAI = Beck Anxiety Inventory; GAF = Global Assessment of Functioning.
Excluded individuals reporting too many episodes to count, therefore, only eight participants in IPSRT group and three in quetiapine group were included.
Includes alcohol, cannabis, cocaine, hallucinogen/PCP, opioid, and stimulant use disorders.
Includes generalized anxiety disorder, panic disorder, obsessive compulsive disorder, and social phobia.
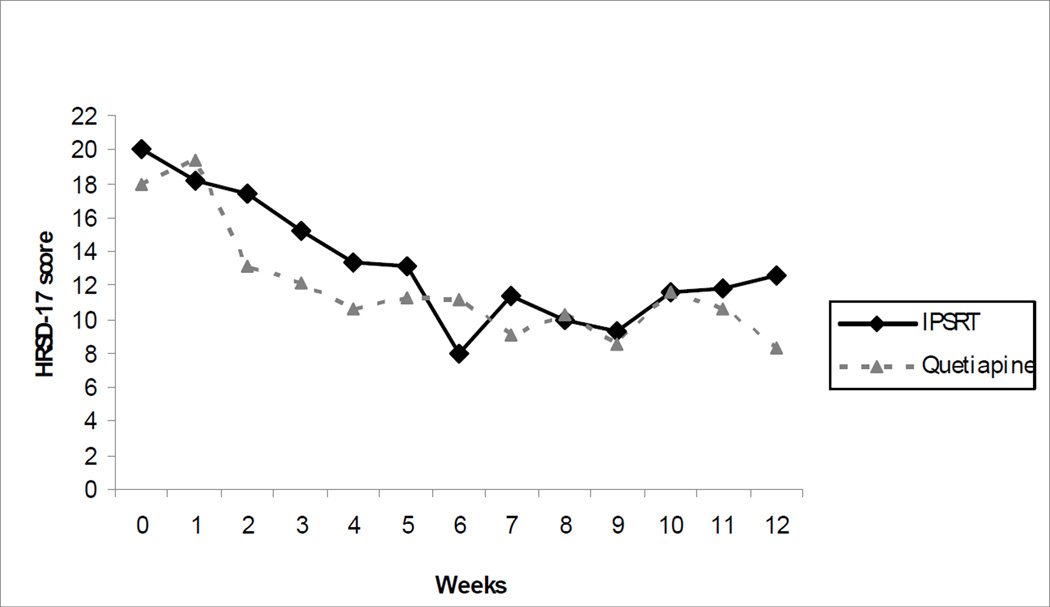
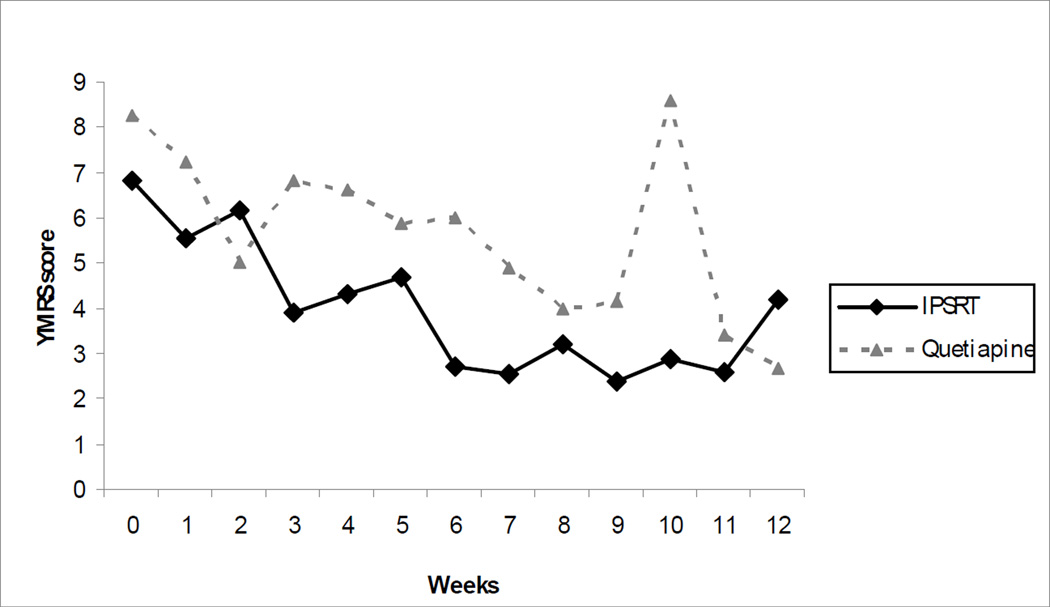
As shown in Figures 1 and 2, there were significant improvements over time in both depressive and hypomanic symptoms in both treatment conditions. Mixed-effects analyses showed significant time effects for symptoms as measured by HRSD-25 [F(1,21) = 44, p < 0.0001], HRSD-17 [F(1,21) = 49, p < 0.0001], YMRS [F(1,21) = 20, p = 0.0002], BAI [F(1,20) = 15, p = 0.001], and MADRS [F(1,23) = 35, p < 0.0001], and in overall illness severity as measured by CGI-severity [F(1,20) = 31, p < 0.0001]. Weight also increased significantly over time in both groups [F(1,20) = 5.9, p = 0.03]. There was no significant time by group interaction on any variable. Treatment preference was initially included as a covariate in these models and found to be significantly correlated only with BAI scores [F(2,105) = 3.18, p = 0.05] with individuals who preferred medication having significantly lower BAI scores relative to those preferring psychotherapy [t(105) = −2.49, p = 0.015]. There was no significant interaction with time, however. Considering the relatively small sample size, treatment preference was therefore dropped as a covariate in subsequent analyses.
Fig. 1.
Mean 17-item Hamilton Rating Scale for Depression (HRSD-17) scores over 12 weeks. IPSRT = Interpersonal and Social Rhythm Therapy.
Fig. 2.
Mean Young Mania Rating Scale (YMRS) scores over 12 weeks. IPSRT = Interpersonal and Social Rhythm Therapy.
Using categorical outcomes, 29% (n = 4) of the sample responded to IPSRT monotherapy and 27% (n = 3) responded to quetiapine (defined as ≥ 50% reduction in HRSD-25 scores and YMRS ≤10) by visit 12. There were no significant differences in response rates between groups. CSQ scores at week 12 were 26.6 ± 3.7 and 27.1 ± 3.8 in the IPSRT (n = 11) and quetiapine (n = 8) completer groups, respectively, with no differences between groups.
Discussion
In this study, we found no differences in outcomes among participants with BP-II depression assigned to either medication or psychotherapy over 12 weeks. Treatment satisfaction was high in both conditions and dropout rates were relatively low compared to other BP-II clinical trials (26). Individuals who preferred psychotherapy to medication had higher anxiety scores, but this is not surprising given the heightened sensitivity of those with anxiety to somatic experiences (41), including medication side effects. Nevertheless, the sample was evenly divided with respect to treatment preference (40% expressed a preference for medication and 40% a preference for psychotherapy prior to randomization), and treatment preference was not associated with treatment outcomes. Both treatment groups experienced significant reductions in mood and anxiety symptoms over time, but there were no group × time interactions. Weight gain was seen in the entire sample, independent of treatment assignment. This underscores the importance of attending to latent metabolic risk factors in individuals with BP disorders (42), including those with BP-II disorder.
The small sample size limits conclusions that can be drawn about efficacy from this trial (43). Observed response rates across groups are lower than those seen in prior trials of quetiapine for BP-II depression (26) which may reflect either real differences in the populations or an artifact of a small trial. Nevertheless, absence of differences between the two groups on all outcome measures and the high degree of acceptability across groups (as measured by high scores on the CSQ and 25% dropout rates) should raise questions about whether pharmacotherapy is necessary for all individuals with BP-II disorder. Future trials should examine factors that predict differential response to psychotherapy and medication since the most important question, inevitably, will be what works for whom.
Acknowledgements
This work was supported by grants from the National Alliance for Research in Schizophrenia and Affective Disorders (NARSAD Young Investigator Award to HAS) and the National Institute of Mental Health (R01 MH084831).
Footnotes
Disclosures
HAS has received honoraria for CME presentations from Servier, International and AstraZeneca, France; and royalties from UpToDate. EF serves on an advisory board for Servier, International; and receives royalties from Guilford Press for Treating Bipolar Disorder: A Clinician’s Guide to Interpersonal and Social Rhythm Therapy and from the American Psychological Association. YC has no conflicts of interest to report.
References
- 1.Judd LL, Akiskal HS, Schettler PJ, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Archiv Gen Psychiatry. 2003;60:261–269. doi: 10.1001/archpsyc.60.3.261. [DOI] [PubMed] [Google Scholar]
- 2.Ruggero CJ, Chelminski I, Young D, Zimmerman M. Psychosocial impairment associated with bipolar II disorder. J Affect Disord. 2007;104:53–60. doi: 10.1016/j.jad.2007.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merikangas KR, Jin R, He J-P, et al. Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey Initiative. Arch Gen Psychiatry. 2011;68:241–251. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Judd LL, Schettler PJ, Solomon DA, et al. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord. 2008;108:49–58. doi: 10.1016/j.jad.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 5.Vieta E, Colom F, Martinez-Aran A, Benabarre A, Reinares M, Gasto C. Bipolar II disorder and comorbidity. Comprehen Psychiatry. 2000;41:339–343. doi: 10.1053/comp.2000.9011. [DOI] [PubMed] [Google Scholar]
- 6.Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1–9. doi: 10.1111/j.1399-5618.2009.00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vieta E, Benabarre A, Colom F, et al. Suicidal behavior in bipolar I and bipolar II disorder. J Nerv Ment Dis. 1997;185:407–409. doi: 10.1097/00005053-199706000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Yatham LN, Kennedy SH, Schaffer A, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disord. 2009;11:225–255. doi: 10.1111/j.1399-5618.2009.00672.x. [DOI] [PubMed] [Google Scholar]
- 9.Vieta E. Long-term treatment of bipolar depression and other issues. J Clin Psychiatry. 2010;71:e07. doi: 10.4088/JCP.8125tx4c. [DOI] [PubMed] [Google Scholar]
- 10.Sidor MM, MacQueen GM. Antidepressants for the acute treatment of bipolar depression: A systematic review and meta-analysis. J Clin Psychiatry. 2011;72:156–167. doi: 10.4088/JCP.09r05385gre. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Practice guidline for the treatment of patients with bipolar disorder (revision) Am J Psychiatry. 2002:159. (April Suppl.) [PubMed] [Google Scholar]
- 12.Swartz HA, Thase ME. Pharmacotherapy for the treatment of acute bipolar II depression: current evidence. J Clin Psychiatry. 2011;72:356–366. doi: 10.4088/JCP.09r05192gre. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodwin GM, Anderson I, Arango C, et al. ECNP consensus meeting. Bipolar depression. Nice, March 2007. European Neuropsychopharmacol. 2008;18:535–549. doi: 10.1016/j.euroneuro.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Dimidjian S, Hollon SD. How would we know if psychotherapy were harmful? Am Psychol. 2010;65:21–33. doi: 10.1037/a0017299. [DOI] [PubMed] [Google Scholar]
- 15.Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- 16.Swartz HA, Frank E, Frankel D. Psychothérapie interpersonnelle et des rythmes sociaux (PTIRS) dans le trouble bipolaire II : structure du traitement et exemples cliniques. Sante Mentale au Quebec. 2008;33:151–184. doi: 10.7202/019673ar. [DOI] [PubMed] [Google Scholar]
- 17.Miklowitz DJ. Adjunctive psychotherapy for bipolar disorder: state of the evidence. Am J Psychiatry. 2008;165:1408–1419. doi: 10.1176/appi.ajp.2008.08040488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miklowitz DJ, Goodwin GM, Bauer MS, Geddes JR. Common and specific elements of psychosocial treatments for bipolar disorder: a survey of clinicians participating in randomized trials. J Psychiatric Prac. 2008;14:77–85. doi: 10.1097/01.pra.0000314314.94791.c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression: A 1-year randomized trial from the Systematic Treatment Enhancement Program. Archiv Gen Psychiatry. 2007;64:419–427. doi: 10.1001/archpsyc.64.4.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Colom F, Vieta E, Sanchez-Moreno J, et al. Psychoeducation for bipolar II disorder: an exploratory, 5-year outcome subanalysis. J Affect Disord. 2009;112:30–35. doi: 10.1016/j.jad.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 21.Swartz HA, Frank E, Frankel DR, Novick D, Houck P. Psychotherapy as monotherapy for the treatment of bipolar II depression: a proof of concept study. Bipolar Disord. 2009;11:89–94. doi: 10.1111/j.1399-5618.2008.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frank E. Treating bipolar disorder: A clinician's guide to interpersonal and social rhythm therapy. New York: Guilford Press; 2005. [Google Scholar]
- 23.Frank E, Kupfer DJ, Thase ME, et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archiv Gen Psychiatry. 2005;62:996–1004. doi: 10.1001/archpsyc.62.9.996. [DOI] [PubMed] [Google Scholar]
- 24.Frank E, Soreca I, Swartz HA, et al. The role of interpersonal and social rhythm therapy in improving occupational functioning in patients with bipolar I disorder. Am J Psychiatry. 2008;165:1559–1565. doi: 10.1176/appi.ajp.2008.07121953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miklowitz DJ, Otto MW, Frank E, et al. Intensive psychosocial intervention enhances functioning in patients with bipolar depression: results from a 9-month randomized controlled trial. Am J Psychiatry. 2007;164:1340–1347. doi: 10.1176/appi.ajp.2007.07020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suppes T, Hirschfeld RM, Vieta E, Raines S, Paulsson B. Quetiapine for the treatment of bipolar II depression: analysis of data from two randomized, double-blind, placebo-controlled studies. World J Biol Psychiatry. 2007:8. doi: 10.1080/15622970701317265. [DOI] [PubMed] [Google Scholar]
- 27.McElroy SL, Weisler RH, Chang W, et al. A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II) J Clin Psychiatry. 2010;71:163–174. doi: 10.4088/JCP.08m04942gre. [DOI] [PubMed] [Google Scholar]
- 28.Young AH, McElroy SL, Bauer M, et al. A double-blind, placebo-controlled study of quetiapine and lithium monotherapy in adults in the acute phase of bipolar depression (EMBOLDEN I) J Clin Psychiatry. 2010;71:150–162. doi: 10.4088/JCP.08m04995gre. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;25:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young RC, Biggs JT, Zeigler VE, Meyer DA. A rating scale for mania: reliability, validity, and sensitivity. Br J Psychiatry. 1987:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clincal Interview for DSM-IV Axis I Disorders (SCID) New York: New York State Psychiatric Institute, Biometrics Research; 1995. [Google Scholar]
- 32.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV personality disorders, (SCID-II) Washington, D.C.: American Psychiatric Press, Inc.; 1997. [Google Scholar]
- 33.Thase ME, Carpenter L, Kupfer DJ, Frank EF. Clinical significance of reversed vegetative subtypes of recurrent major depression. Psychopharmacology Bulletin. 1991;27:17–22. [PubMed] [Google Scholar]
- 34.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 35.Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73:159–171. doi: 10.1016/s0165-1781(97)00123-6. [DOI] [PubMed] [Google Scholar]
- 36.Beck AT, Steer RA. Manual for the revised Beck Anxiety Inventory. San Antonio: Psychological Corporation; 1990. [Google Scholar]
- 37.Attkisson CC, Greenfield TK. The client satisfaction questionnaire-8 and the service satisfaction questionnaire-30. In: Maruish M, editor. The use of psychological testing for treatment planning and outcome assessment. Hillsdale: Lawrence Earlbaum Associates; 1994. pp. 402–422. [Google Scholar]
- 38.Matts JP, Lachin JM. Properties of permuted-block randomization in clinical trials. Control Clin Trials. 1988;9:327–344. doi: 10.1016/0197-2456(88)90047-5. [DOI] [PubMed] [Google Scholar]
- 39.Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal Psychotherapy of Depression. New York: Basic Books; 1984. [Google Scholar]
- 40.Monk TH, Flaherty JF, Frank E, Hoskinson K, Kupfer DJ. The Social Rhythm Metric: an instrument to quantify the daily rhythms of life. J Nerv Men Dis. 1990;178:120–126. doi: 10.1097/00005053-199002000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Frank E, Shear MK, Rucci P, et al. Influence of panic-agorophobic spectrum symptoms on treatment response in patients with recurrent major depression. Am J Psychiatry. 2000;157:1101–1107. doi: 10.1176/appi.ajp.157.7.1101. [DOI] [PubMed] [Google Scholar]
- 42.Leboyer M, Kupfer DJ. Bipolar disorder: new perspectives in health care and prevention. J Clin Psychiatry. 2010;71:1689–1695. doi: 10.4088/JCP.10m06347yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Archiv Gen Psychiatry. 2006;63:484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]