Abstract
Background:
There is a need for telemedicine, particularly in countries with large geographical areas and widely scattered low-density communities as is the case of the Canadian system, particularly if equality of care is to be achieved or the difference gap is to be narrowed between urban centers and more peripheral communities.
Aims:
1. To validate teledermatopathology as a diagnostic tool in under-serviced areas; 2. To test its utilization in inflammatory and melanocytic lesions; 3. To compare the impact of 20× (0.5 μm/pixel) and 40× (0.25 μm/pixel) scans on the diagnostic accuracy.
Materials and Methods:
A total of 103 dermatopathology cases divided into three arms were evaluated by two pathologists and results compared. The first arm consisted of 79 consecutive routine cases (n=79). The second arm consisted of 12 inflammatory skin biopsies (n=12) and the third arm consisted of 12 melanocytic lesions (n=12). Diagnosis concordance was used to evaluate the first arm. Whereas concordance of preset objective findings were used to evaluate the second and third arms.
Results:
The diagnostic concordance rate for the first arm was 96%. The concordance rates of the objective findings for the second and third arms were 100%. The image quality was deemed superior to light microscopy for 40× scans.
Conclusion:
The current scanners produce high-resolution images that are adequate for evaluation of a variety of cases of different complexities.
Keywords: Teledermatopathology, telepathology, virtual microscopy, VM, whole slide imaging, WSI
INTRODUCTION
There is a need for telemedicine, particularly in countries of large geographical areas and widely scattered low-density communities as is the case of the Canadian system, particularly if equality of care is to be achieved or the difference gap is to be narrowed between urban centers and more peripheral communities. In this model hiring and retaining pathologists for instance in remote areas particularly with subspecialty training is almost impossible.
Telepathology is a branch of telemedicine, whereby a pathologist is able to review pictures (of variable formats depending on the technique used) at a distance. For this reason, telepathology has a great potential to allow easier access to subspecialties that are otherwise not available within a particular geographical area.
Dermatopathology is an ideally suited specialty to the implementation of telepathology for the following reasons:
There is fairly a limited number of trained dermatopathologists.
The slide/case ratio is relatively small compared to other areas of pathology.
There is relatively high case volume.
The aims of our study are:
To validate teledermatopathology as a diagnostic tool in underserviced areas;
To test its utilization in inflammatory and melanocytic lesions;
To compare the impact of 20× (0.5 μm/pixel) and 40× scans (0.25 μm/pixel) on the diagnostic accuracy.
MATERIALS AND METHODS
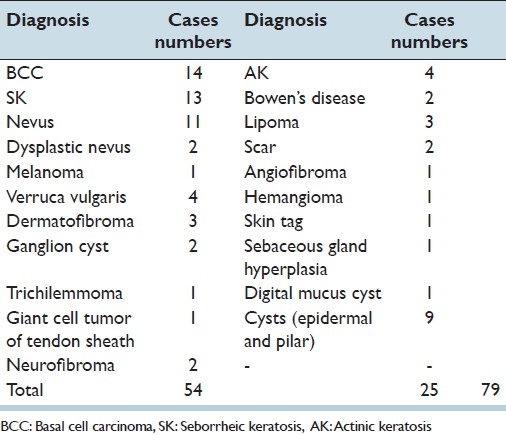
A total of 103 dermatopathology cases were divided into three arms. The first arm Table 1 consisted of consecutive routine skin cases (n=79) from Timmins and District Hospital, Timmins, Ontario, Canada, which were scanned at 20× using Aperio CS ScanScope. These cases were reviewed by a primary pathologist who diagnosed the cases using light microscopy. Subsequently, the same cases were reviewed by a University Health Network (UHN) pathologist along with the clinical information as provided by the requisition was available to both pathologists. The pathologist was blinded to the diagnoses. For cases that contained more than 1 slide, the primary pathologist picked the most representative slide for scanning. The diagnoses were compared, and only cases with discrepancies were reviewed under a multiheader microscope. The reviewed cases involved the glass slide that was originally scanned. Any difference in diagnosis between the two pathologists was considered as a discrepancy that required joint examination under the multihead microscope to discuss the findings and reach an agreement. For each case, concordance is considered achieved when both pathologists give the same diagnosis.
Table 1.
Cases in the first arm
The second arm consisted of 12 cases of inflammatory skin biopsies (IS) and the third arm consists of 12 melanocytic lesions (ML) (1 slide/case each) from our teaching/consultation archives, which were retrieved and scanned at 20× and 40× with an emphasis on assessing objective findings rather than diagnoses. The combined three arms provided an accurate representation of typical dermatopathology work including general routine cases, and consultation material.
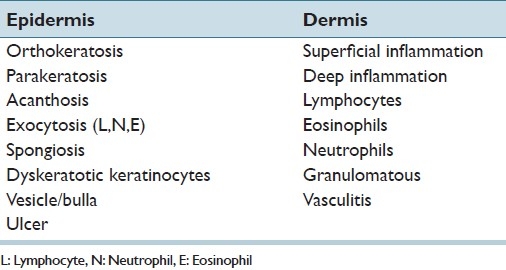
For IS, these findings were divided into three main categories: epidermal, dermal, and other findings. Under each column objective findings were listed [Table 2].
Table 2.
The objective checklist used to evaluate cases in the second arm of the study; the medical dermatoses
The selected inflammatory cases covered a wide range of cases as follows: arthropod bite, acute spongiotic dermatitis, Sweet's syndrome, bullous pemphegoid cell poor variant, Pityriasis lichenoides, pustular psoriasis, sarcoidosis, Lichen simplex chronicus, gouty tophus, subacute spongiotic dermatitis, leukocytoclastic vasculitis, and stasis dermatitis.
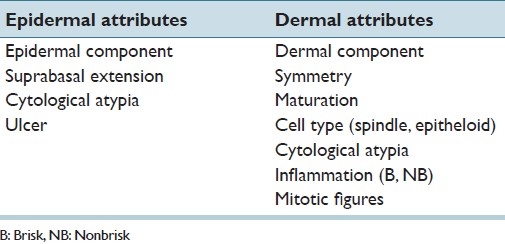
For ML, benign and malignant cases were mixed and objective findings were evaluated utilizing epidermal and dermal attributes in a checklist format indicating the presence or absence of these predetermined objective findings Table 3. The quality of the diagnostic image was assessed in the second and third arms after each case in a scale from 1 to 3 (1=inferior, 2= Similar, and 3= Superior quality compared to light microscopy). The UHN pathologist was blinded to the clinical information and the final diagnoses. The assessment started with the 20× scans and proceeded to 40× scans. There were six cases of melanoma (1 metastatic), 2 compound nevi, 2 junctional nevi, 1 dysplastic compound nevus, and 1 atypical Spitz tumor.
Table 3.
The checklist used to evaluate the third arm of the study; the melanocytic lesions
Pathologist #1 collected the cases, reviewed them under a light microscope, compared the original report for potential omissions, and filled the corresponding tables, and the results were compared with the UHN pathologists-completed tables. Concordance is defined for every objective finding if both pathologists identified the presence or absence of the predetermined set of objective findings as compared between glass slides vs. 20× and glass slides vs 40×.
The workstation consisted of a PC powered with Pentium 4 processor (3GHz), 1 MB RAM, and 20¢ LCD monitor (HP 2035) with the following setup: resolution 1152 × 864 pixels at 32 bit true color. The scanned images are viewed as compressed JPEG files with a compression ratio of 30.
RESULTS
The concordance rate for the routine cases in the first arm was (96%). There were minor discrepancies between the two pathologists in three cases. All deemed minor with no clinical significance. These were intradermal nevus vs. compound nevus, actinic keratosis vs. in situ squamous cell carcinoma, and seborrheic keratosis vs. verruca vulgaris. After the 2 pathologists reviewed these cases under the multihead microscope, the discrepancies were attributed to interpretation rather than poor image resolution.
For the second arm, all the inflammatory skin findings corresponded to the original pathology report/light microscopy except one case where leukocytoclastic vasculitis was originally reported but was not recorded by the UHN pathologist using WSI, though it was suggested under other findings. Since it is our routine to include three levels for small punch biopsies in the same glass slide, the scanned level did not show the focus of fibrinoid wall necrosis, and hence the discrepancy was deemed to be due to partial sampling of the slide during scanning.
The 20× scans were given a score of 2 each (equivalent to light microscopy); however, 40× scans were given a score of 3 (superior to light microscopy). The resolution at 40× is definitely superior however; it showed no tangible difference in the inflammatory dermatoses evaluated in our study.
The melanocytic lesions showed 100% concordance rate for both the 20× and 40× scanned slides. However, in malignant and atypical melanocytic lesions 40× gave a superior resolution with detailed nuclear features and easier identification of mitoses that added an extra level of diagnostic confidence, but similar to IS did not yield any tangible difference.
DISCUSSION
Currently we use telepathology routinely to cover the frozen section service in Timmins and District hospital, located in Timmins, Ontario, at a distance of around 550 km northeast of Toronto.
Telepathology has wide application in education and research (probably the most common use currently);[1,2] and its utilization for routine surgical pathology is still limited to certain centers[3,4] and maybe practical only to handle low volume.[4] Virtual microscopy has been in routine use since 1996 in the Veteran Integrated Service Network (VISN) 12 headquartered in Chicago, IL, USA, which covers a wide geographic area (320 miles north-south × 100 miles east-west). They utilized a hybrid dynamic store and forward (HDSF) telepathology network using a high-speed wide area network (WAN) which combines robotic and nonrobotic telepathology systems to achieve a wide range of functionality in surgical pathology, autopsy pathology, clinical pathology as well as other uses.[5,6]
This study was designed to simulate typical academic dermatopathology workload covering a wide range of cases of different complexities. One of the major hindrances in adopting this technology in the pathology community is the perception that such a technique may produce suboptimal images that can carry adverse outcomes.[4]
Although there are myriads of studies that indicate high diagnostic concordance rates with excellent image quality, there is however a wide-range of documented concordance rates anywhere between 73% and 96.4%.[3,7,8] However, most of these studies measure diagnostic concordance rates and each has a different study design with variable case complexities making objective comparison almost impossible.
Since diagnostic concordance rate is an indirect measure of image quality, it can be affected by other factors such as individual pathologist experience, and the clinical information provided. In addition the projected image is also a function of the particulars of the workstation personal computers (PC) and monitors. The Aperio web site suggests a reasonably fast PC with 256 MB of RAM for best results (http://www.aperio.com/other/FAQs-pathology-slide-scanning.asp).
That is why we decided to design our study with the emphasis on evaluating objective findings to get a better measure of image quality. In this way, hopefully, the uncertainty regarding the image quality will be eliminated or minimized. The concordance rates in the three arms in this study are very high (96-100%) which makes WSI ideal as a primary and a secondary diagnostic tool.
The second arm of the current study demonstrates that WSI is feasible for inflammatory skin diseases, which is at odds with Massone et al.'s findings,[7] in which they evaluated inflammatory skin disease using virtual microscopy (VM). They had 46 biopsies of inflammatory skin disease, evaluated by 12 tele-consultant in six countries. They reported a 73-74% concordance rate. They concluded that the technology is not feasible for inflammatory skin diseases, although they acknowledged the intrinsic difficulty of inflammatory skin diseases and the impact of the provided clinical information on the accuracy of diagnosis. Our model in this study of assessing objective findings rather than measuring diagnoses’ concordance rates circumvents these challenges, which can significantly skew the results in a negative way.
Concerns about the difficulty of detecting eosinophils, neutrophils, and mitotic figures using 20 scans have been raised;[1] however in this study no such difficulties were observed.
A study by Velez et al.[9] evaluated two different applications (viewing software packages) and compared the workflow by measuring the time spent on each slide, time spent on each magnification, and diagnostic concordance. They had a total of 45 cases divided into three arms in the study: glass slide and light microscopy, digital images viewed by the vendors viewing application, and digital images viewed by their in-house developed application (digital images scanned at × 20). For consistency, predetermined diagnoses were selected covering inflammatory, nonmelanocytic neoplasms, and melanocytic neoplasms. Triplicate cases of each diagnosis were selected and randomly assigned to each of the different arms. They excluded any case of more than 10 HandE slides or required immunohistochemical stains to reach a diagnosis. Three dermatopathologists (two staff and one fellow) evaluated these cases in each of the different arms while being videotaped. They concluded that there was no statistically significant difference in time spent between the glass slides and the digital images, nor were there any differences between the two applications. They also determined that there were three main issues with the image quality: (1) identifying eosinophils (and neutrophils), (2) identifying apoptosis, (3) grading melanocytic dysplasia. They concluded that image quality might be responsible for inability to accurately evaluate melanocytic atypia or maybe due to lack of experience with digital images. They also reported 8.6% out of focus digital slides that required rescanning. Our study is at odds with their study, as we did not notice any difficulty picking up apoptosis, eosinophils, and neutrophils, although we acknowledge the superior images produced by 40× scans.
A study by Leinweber et al.,[8] evaluated 560 melanocytic lesions (280 melanoma and 280 benign nevi) by 4 dermatopathologists. The concordance rate was 94.4--96.4%. They excluded consultation cases from their study, which could explain the relatively high concordance rate. However, we have demonstrated 100% concordance rate in the third arm of this study evaluating objective findings.
40× scans definitely produce superior image quality; our study failed to demonstrate any tangible difference between 40× scans and 20× scans. However, 40× scans produced images that were superior to light microscopy as evaluated in both the second and third arms of this study. 40× scans may play a role as an option to enhance the diagnostic confidence if needed particularly in difficult melanocytic lesions and suspected cases of lympho-proliferative disorders.
Although we did not compare the impact of WSI on the turn around time, we think that with familiarization of this technique, the difference, if it exists, would be negligible.
There is a growing interest to apply automated image analysis to achieve various goals. As Krenacs et al. pointed out, such automation can increase reproducibility and reliability and decease the impact of interobserver variability in immunohiostochemical interpretation in the cases of Her2/Neu, ER, and PR.[2]
This technique, though useful, probably needs further improvements for it to be utilized for high-volume work. The use of a mouse for navigation is less than optimal. Automated integration of scanned images with existing pathology software packages would be needed as well.
CONCLUSION
Although measuring diagnostic concordance rates is a very useful indirect measure for evaluating the photographic resolution, it harbors other factors such as the pathologist's experience and the adequacy of clinical history provided, which can have profound effects on the final concordance rates. Evaluating objective findings (when possible) rather than diagnoses is a far better direct measure of the image resolution.
Our study shows that the current resolution obtained is sufficient to evaluate the objective findings accurately.
WSI is adequate for primary dermatopathology diagnosis which can be utilized for remote areas. Also the images produced are sufficient for both melanocytic and inflammatory skin disease. And although there was no tangible difference between 20× and 40× scans, probably, resorting to 40× scans may be needed in certain instances to provide a far superior image and thus boosts confidence when needed in difficult cases.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2012/3/1/2/93399
REFERENCES
- 1.Koch LH, Lampros JN, Delong LK, Chen SC, Woosley JT, Hood AF. Randomized comparison of virtual microscopy and traditional glass microscopy in diagnostic accuracy among dermatology and pathology residents. Hum Pathol. 2009;40:662–7. doi: 10.1016/j.humpath.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 2.Krenacs T, Zsakovics I, Diczhazi C, Ficsor L, Varga VS, Molnar B. The potential of digital microscopy in breast pathology. Pathol Oncol Res. 2009;15:55–8. doi: 10.1007/s12253-008-9087-z. [DOI] [PubMed] [Google Scholar]
- 3.Wienert S, Beil M, Saeger K, Hufnagl P, Schrader T. Integration and acceleration of virtual microscopy as the key to successful implementation into the routine diagnostic process. Diagn Pathol. 2009;4:3. doi: 10.1186/1746-1596-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evans AJ, Chetty R, Clarke BA, Croul S, Ghazarian DM, Kiehl TR, et al. Primary frozen section diagnosis by robotic microscopy and virtual slide telepathology: the University Health Network experience. Hum Pathol. 2009;40:1070–81. doi: 10.1016/j.humpath.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Dunn BE, Choi H, Almagro UA, Recla DL. Combined robotic and nonrobotic telepathology as an integral service component of a geographically dispersed laboratory network. Hum Pathol. 2001;32:1300–3. doi: 10.1053/hupa.2001.29644. [DOI] [PubMed] [Google Scholar]
- 6.Dunn BE, Choi H, Almagro UA, Recla DL, Davis CW. Telepathology networking in VISN-12 of the veterans health administration. Telemed J E Health. 2000;6:349–54. doi: 10.1089/153056200750040200. [DOI] [PubMed] [Google Scholar]
- 7.Massone C, Peter Soyer H, Lozzi GP, Di Stefani A, Leinweber B, Gabler G, et al. Feasibility and diagnostic agreement in teledermatopathology using a virtual slide system. Hum Pathol. 2007;38:546–54. doi: 10.1016/j.humpath.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Leinweber B, Massone C, Kodama K, Kaddu S, Cerroni L, Haas J, et al. Teledermatopathology: a controlled study about diagnostic validity and technical requirements for digital transmission. Am J Dermatopathol. 2006;28:413–6. doi: 10.1097/01.dad.0000211523.95552.86. [DOI] [PubMed] [Google Scholar]
- 9.Velez N, Jukic D, Ho J. Evaluation of 2 whole-slide imaging applications in dermatopathology. Hum Pathol. 2008;39:1341–9. doi: 10.1016/j.humpath.2008.01.006. [DOI] [PubMed] [Google Scholar]


