Abstract
Background:
Utilization of the transforaminal lumbar interbody fusion (TLIF) approach for scoliosis offers the patients deformity correction and interbody fusion without the additional morbidity associated with more invasive reconstructive techniques. Published reports on complications associated with these surgical procedures are limited. The purpose of this study was to quantify the intra- and postoperative complications associated with the TLIF surgical approach in patients undergoing surgery for spinal stenosis and degenerative scoliosis correction.
Methods:
This study included patients undergoing TLIF for degenerative scoliosis with neurogenic claudication and painful lumbar degenerative disc disease. The TLIF technique was performed along with posterior pedicle screw instrumentation. The average follow-up time was 30 months (range, 15–47).
Results:
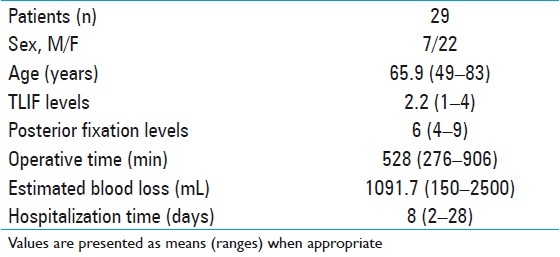
A total of 29 patients with an average age of 65.9 years (range, 49–83) were evaluated. TLIFs were performed at 2.2 levels on average (range, 1–4) in addition to 6.0 (range, 4–9) levels of posterolateral instrumented fusion. The preoperative mean lumbar lordosis was 37.6° (range, 16°–55°) compared to 40.5° (range, 26°–59.2°) postoperatively. The preoperative mean coronal Cobb angle was 32.3° (range, 15°–55°) compared to 15.4° (range, 1°–49°) postoperatively. The mean operative time was 528 min (range, 276–906), estimated blood loss was 1091.7 mL (range, 150–2500), and hospitalization time was 8.0 days (range, 3–28). A baseline mean Visual Analog Scale (VAS) score of 7.6 (range, 4–10) decreased to 3.6 (range, 0–8) postoperatively. There were a total of 14 (49%) hardware and/or surgical technique related complications, and 8 (28%) patients required additional surgeries. Five (17%) patients developed pseudoarthrosis. The systemic complications (31%) included death (1), cardiopulmonary arrest with resuscitation (1), myocardial infarction (1), pneumonia (5), and pulmonary embolism (1).
Conclusion:
This study suggests that although the TLIF approach is a feasible and effective method to treat degenerative adult scoliosis, it is associated with a high rate of intra- and postoperative complications and a long recovery process.
Keywords: Adult scoliosis, complications, degenerative spine, lumbar stenosis, transforaminal lumbar interbody fusion
INTRODUCTION
The necessity to perform surgery for degenerative adult scoliosis continues to be a controversial issue and to this day no prospective controlled clinical trial exists comparing non-surgical to surgical treatment methods. In addition, this population tends to be elderly with multiple comorbidities, which can make major operations and the subsequent rehabilitation more complicated.
New and less invasive surgical techniques for scoliotic deformity correction are being investigated in clinical settings.[1,2,12,14,17] The utilization of theoretically less invasive approaches for scoliosis may offer comparable clinical improvement and radiographic deformity correction with fewer or diminished complications as compared to traditional techniques. The transforaminal lumbar interbody fusion (TLIF) approach also enables interbody grafting without the morbidity associated with more invasive anterior reconstructive surgeries.[7] While the advances in surgical technology have increased the capability to correct spinal deformity using less invasive approaches, the complexity of these procedures has also increased. Currently, our knowledge about the rates of complications associated with these surgical techniques is limited. We intuitively believe that less invasive techniques will result in fewer complications, but this is not necessarily true. The main objective of this study was to analyze the complications in a patient population that underwent TLIF surgery for a primary indication of degenerative scoliosis with spinal stenosis.
MATERIALS AND METHODS
Patients
Twenty-nine patients who matched the defined criteria underwent surgery from February 2003 to October 2009. The mean follow-up time was 30 months (range, 15–47). Selected demographic patient parameters are presented in Table 1. The patients had exhausted all conservative treatment options and were diagnosed with painful degenerative disc disease, radiculopathy, and spinal canal stenosis. Thirteen (44.8%) patients had severe and 16 (55.2%) had moderate central canal stenosis. Only patients who underwent surgery for de novo degenerative scoliosis were included in this analysis. The main indications determining the necessity of surgery were the severity of spinal canal stenosis and symptoms of neurogenic claudication, along with progression of the deformity. Clinical findings were supported by imaging studies [plain films, magnetic resonance imaging (MRI), computed tomography (CT) myelogram].
Table 1.
Selected demographic and surgical patient data
All patients underwent TLIF procedure with posterior fixation. Selected surgical parameters are presented in Table 1. Posterolateral levels included T9 to S1 vertebral bodies. The upper instrumented vertebra ranged from T9 to L2 and lower instrumented vertebra was either L5 or S1. The length of fusion depended on the clinical findings (the level of significant laterolisthesis, apex of the curve), patient anatomy, size, and body habitus of the patient and amount of correction required.
The safety of the TLIF approach was evaluated by prospectively recording all intraoperative and postoperative complications. Complications were defined as any adverse events that required symptomatic treatment or intervention and occurred intraoperatively and/or during a follow-up period and were related to surgery. All complications were further divided into systemic medical complications or hardware and surgical technique-related complications.
Clinical and radiographic outcomes
Pre- and postoperative anterior–posterior standing radiographs were used to measure alignment in the coronal plane and lateral neutral radiographs were used to measure lumbar lordosis in the sagittal plane using the Cobb method. The coronal plane deformities were measured using the endplates of maximally angled vertebrae cranially and caudally [Figure 1a and b]. For the lumbar lordosis, the Cobb angle was measured from the superior endplate of L1 to the superior endplate of S1 vertebral bodies.
Figure 1.
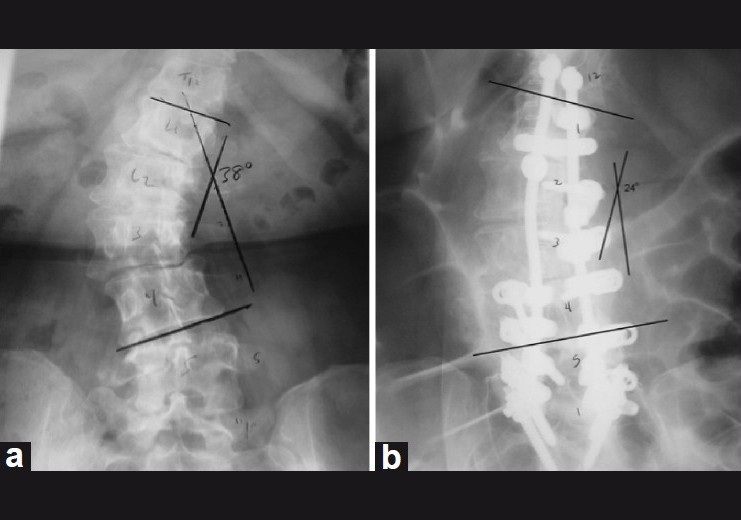
Coronal Cobb angle measurements: (a) preoperative and (b) postoperative plain radiographs
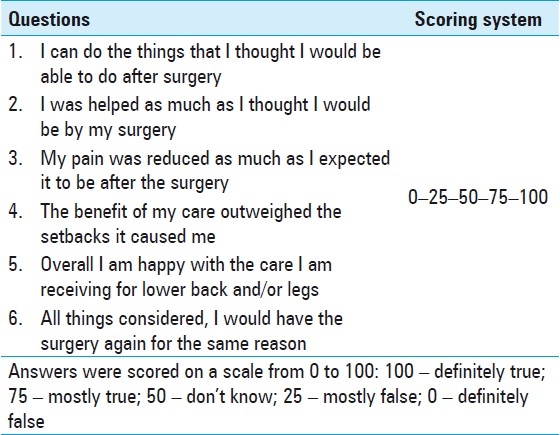
Clinical outcomes were assessed using a combined back and lower extremity pain score measured on the Visual Analog Scale (VAS; 0–10). Overall clinical success was measured using postoperative questionnaires. Macnab criteria[10] were used to evaluate the clinical outcomes as a patient's perceived global effect of the surgical treatment. The results were classified as: excellent – free from all pain and back to all activities, good – minor intermittent pain not interfering with normal activities, fair – improvement in symptoms, but persistent low back and/or sciatica interfering with capacity to engage in full normal activities, and poor – no change or worsening in symptoms. Excellent/good and fair/poor clinical outcomes were combined for analysis purposes. Satisfaction with results was evaluated postoperatively using the Patient Satisfaction with Results Survey [Table 2]; the mean total score was determined for each patient.
Table 2.
The Patient Satisfaction with Results Survey
RESULTS
Complications
All complications are listed in Table 3. A total of 19 out of 29 (66%) patients had at least one complication. The overall systemic complication rate was 31%. One 59-year-old female died in the ICU after surgery due to multisystem failure. Another patient (75-year-old female) had cardiopulmonary arrest and was taken back to the OR the same day for wound exploration and in order to rule out continued postoperative bleeding. This patient also developed pneumonia postoperatively. A 69-year-old man had myocardial infarction. A 66-year-old female was hospitalized 2 weeks after undergoing surgery; she was found to have a pulmonary embolism and was treated with anti-coagulation therapy.
Table 3.
Complications
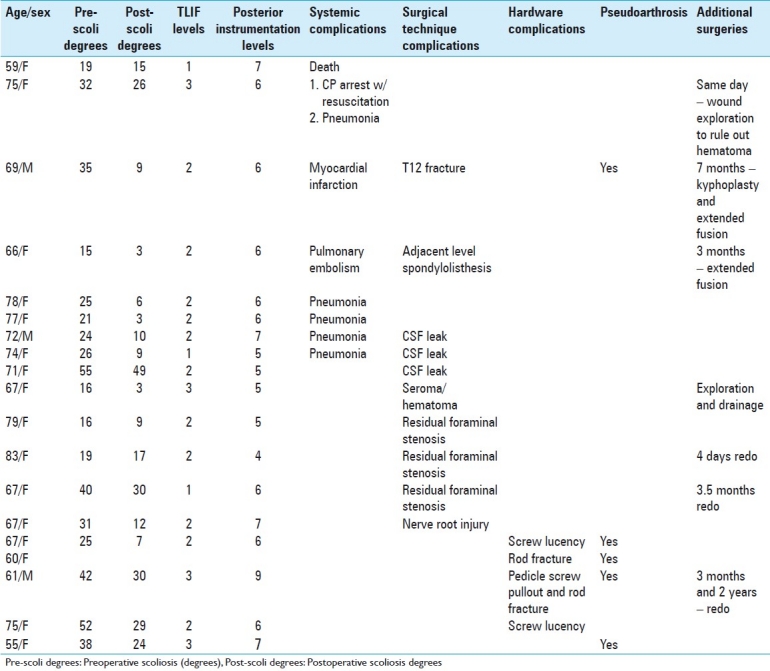
There were a total of 10 (35%) hardware and 4 (14%) surgical technique related complications, 8 (28%) of which required additional surgeries. Cerebrospinal fluid (CSF) leaks were all repaired intraoperatively under a high-power microscope with Prolene sutures followed by application of DuraGen Dural Graft Matrix (Integra LifeSciences, Plainsboro, NJ, USA) and DuraSeal (Covidien, Mansfield, MA, USA) with no subsequent postoperative intervention required. One patient developed increasing pain in legs and pain in posterior thighs with numbness and tingling and was diagnosed with a large subfascial fluid collection consistent with seroma or hematoma, and was taken back to surgery during the third postoperative week. The patient's incision was explored, the fluid was evacuated, and a subfascial drain was placed. Three patients had residual foraminal stenosis: two patients underwent exploration and foraminotomy and one patient was diagnosed with intractable neuropathic pain and was treated conservatively. Three months after the initial surgery, one patient underwent an additional surgery for adjacent level spondylolisthesis at the S1/S2 level. One patient had postoperative weakness and dysesthetic symptoms, which were potentially caused by nerve root irritation, and was treated conservatively with symptom resolution in 2.5 months. Another patient was reoperated on for hardware failure secondary to fracture at the top level of the construct (T12) and pseudoarthrosis 6 months after initial surgery. This patient's fusion was extended two levels and reinforced with bone cement.
A total of 5 (17%) patients developed pseudoarthrosis. Four patients had hardware-related complications, which included screw lucency (n = 3) and rod fracture (n = 1) associated with pseudoarthrosis (n =3), and three out of these four patients underwent redo surgeries.
Clinical and radiographic outcomes
Clinical outcomes were evaluated at an average time of 30 months (range, 15–47), and using Macnab criteria were determined to be excellent/good in 22 (76%) and fair in 7 (24%) out of 29 patients. We did not have any patients who rated the outcome of their surgical treatment as poor. The overall mean patient satisfaction rate was 77% (range, 42–100). The mean back and leg VAS scores decreased from 7.6 (range, 4–10) preoperatively to 3.6 (range, 0–8) postoperatively. This improvement in patients’ pain scores was statistically significant (P = 0.0001).
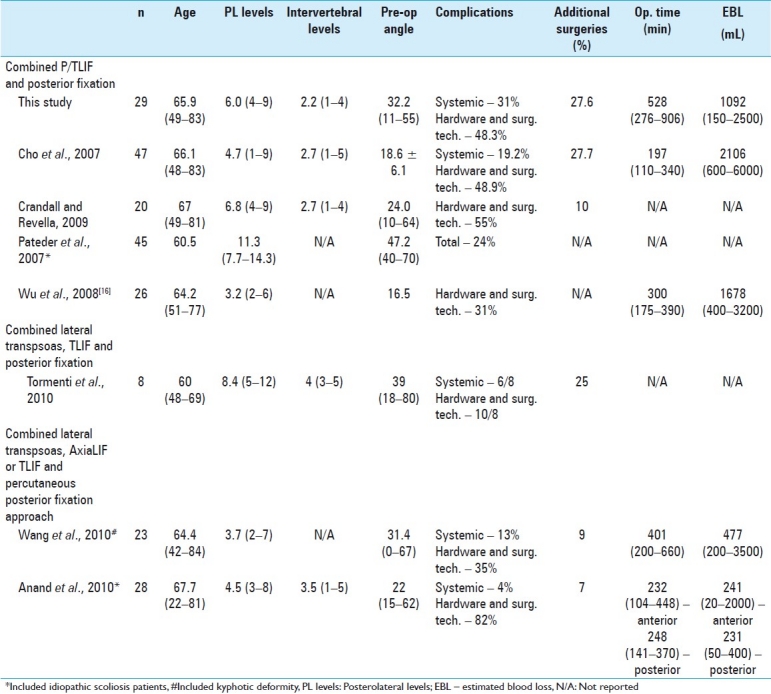
The mean preoperative coronal Cobb angle was 32.3° (range, 15°–55°) compared to the mean of 15.4° (range, 1°–49°) postoperatively, which was a statistically significant improvement (P = 0.0001). The graph [Figure 2] schematically presents the degree of deformity correction for each patient. The average correction of the deformity achieved for each patient was 15.9° (range, 2°–37°), which is 57% (range, 11–94) improvement when compared to preoperative measurements.
Figure 2.
Schematic representation of the deformity correction for each patient (pre-op angle – preoperative angle; post-op angle – postoperative angle; x axis – degrees)
The mean preoperative lumbar lordosis was 37.6° (range, 16°–55°) compared to the mean of 40.5° (range, 26°–59.2°) postoperatively. There were four patients who had a loss of lumbar lordosis of 7° on average (range, 4.3°–10.4°) postoperatively. Three of these four patients had preoperative lumbar lordosis ranging from 51.8° to 55.0°. Lumbar lordosis for this subgroup of patients was changed to a mean value of 42.5° (range, 32.1°–48.6°). Another group of patients (n = 4) that preoperatively had lumbar lordosis of less than 35° (mean 22.9°; range, 16°–30.5°) had an average of 34% improvement in their lumbar lordosis or 7.0° (range, 5.6°–10.3°) with an average postoperative lumbar lordosis of 30.0° (range, 26°–36.5°).
DISCUSSION
Traditionally, combined anterior-posterior reconstructive surgery has been associated with a high complication rate in patients undergoing surgery for painful degenerative disc disease,[9,13] and especially in patients undergoing scoliotic deformity correction surgeries.[3–5,15] Less invasive surgery techniques can reduce soft tissue trauma, intraoperative blood loss, and recovery time, which led us to hypothesize that use of the TLIF technique could translate into reduced complication rates. However, a higher than expected complication rate was reported in our study: 31% of patients encountered systemic complications including one death. In addition, there were 49% hardware or surgical technique related complications and 28% of all patients who had these complications required additional surgeries.
There are currently no published prospective clinical trials that report intra- and postoperative complications in patients undergoing TLIF surgery for degenerative scoliotic deformity correction. Although patients with degenerative scoliotic deformities tend to have smaller curves than those with idiopathic adolescent scoliosis, these curves are typically more rigid and can be very difficult to reduce. Patients also tend to be much older and often have associated comorbidities including osteoporosis. These two groups of patients and two distinct pathologies cannot be evaluated and compared as equals. A recent systematic review[17] that included patients who underwent surgery for adult scoliosis correction (mean age 47.7 years) reported a 41.2% complication rate in 2175 patients, including a 12.9% pseudoarthrosis rate in 2469 patients. The incidence of reported complications ranged from 0 to 53% and that of pseudoarthrosis ranged from 0 to 41%. Another large retrospective study that analyzed radiographic outcomes in anterior–posterior and posterior-only approach patient groups was reported by Patender et al.[11] This study reported a 24% rate of major complications in the P/TLIF approach patient group, but this group of 80 patients included 35 patients with idiopathic scoliotic deformity. Table 4 gives a brief summary comparing the results of our study with those of other studies.
Table 4.
Comparison of selected studies of spinal fusion for scoliosis
The complication rates found in our study were consistent with those reported in 2007 by Cho et al.[6] The authors evaluated complications in patients undergoing posterior fusion and instrumentation surgeries for degenerative adult scoliosis correction. They reported 48.9% hardware and surgical technique related complications, in addition to 19.2% systemic complications. 27.7% of all treated patients needed revision surgeries to correct complications or revise previous fusion for pseudoarthrosis, hardware malfunctions, or adjacent level disease. Before drawing any further conclusions, a few significant differences in surgical technique should be taken into account: the mean preoperative coronal deformity angle was lower (18.6° ± 6.1°), the posterior fixation segment was shorter (4.7 ± 2.2), and there was significantly shorter operative time (197.4 ± 60.7 min) and higher estimated blood loss (2106 ± 1083 mL) reported in the Cho et al. study. Crandall and Revella[7] compared TLIF and anterior lumbar interbody fusion (ALIF) techniques in this patient population. The authors concluded that there was a tendency for more complications and revision surgeries in the ALIF patient group, but the reported hardware-related complication rate in the TLIF group was also high (55%).
A smaller group of similar patients was reported by Tormenti et al.[12] in a study where the authors compared radiographic outcomes and complications in four patients who underwent TLIF surgery for deformity correction with those of eight patients who had TLIF combined with eXtreme lateral interbody fusion (XLIF) surgeries . The authors made a very valuable observation in regards to performing this theoretically less invasive XLIF approach in degenerative scoliotic deformity correction surgeries. The rotatory component of the scoliotic deformity considerably increases the risk of injury to abdominal structures, which resulted in one emergency exploratory laparotomy and segmental bowel resection for cecal perforation in this series. A total of 16 systemic and hardware or surgical technique-related complications were encountered in eight patients.
Another study that evaluated 28 patients undergoing surgery for degenerative or idiopathic adult scoliosis was reported by Anand et al.[2] Eighty-two percent of patients suffered from hardware or surgical technique related complications, the majority of which were transient sensory deficits. Other complications included quadriceps palsy, renal retrocapsular hematoma, and pedicle screw prominence or fracture. Interbody fusions were performed through a lateral transpsoas approach or axial lumbar interbody fusion (AxiaLIF) technique supplemented with percutaneous pedicle screw placement. Surgeries of three or more levels were staged 2 or 3 days apart, resulting in 10-day hospital stays on average. Similar surgical technique was reported by Wang et al.,[14] except that the TLIF approach was used instead of AxiaLIF. Their complication rates mostly consisted of transient sensory deficits as well. The authors excluded patients with severe central canal stenosis and spondylolisthesis from the study and admitted that such a minimally invasive approach limits the degree of deformity correction when compared to open surgeries. In addition, the follow-up time was limited and longer follow-up is potentially needed to fully evaluate the benefits of this approach.
Gupta,[8] in his review paper on degenerative scoliosis surgical treatment options, pointed out that studies on complications in this patient population are lacking as most studies to date suffer from interference with the inclusion of adult idiopathic scoliosis patients. It may be difficult to make generalized conclusions from our results as we had a small number of patients and surgeries were performed at only one surgical center. The main objective of this study was to determine the complication rates in this patient population. Radiographic and clinical outcomes for this patient population were not prospectively studied, but were provided to illustrate the fact that despite the high complication rate in this population, the majority of patients had improvement of their symptoms and were satisfied with the surgery results. Similar findings were also confirmed by Zimmerman et al.[18] in a prospective study that evaluated functional outcomes and complications and they found that there were no differences in ODI, SRS-22, SF-36 between patients with or without complications. The knowledge of complication rates associated with even less invasive surgeries for degenerative scoliosis correction allows both doctor and patients a more accurate representation of the risk/benefit profile of such surgeries, which may change surgical planning.
CONCLUSIONS
This study suggests that although the TLIF approach is feasible and effective in treating degenerative adult scoliosis, it is associated with a high rate of intra- and postoperative complications and a long recovery process that is very similar to anterior–posterior reconstructive surgery for degenerative scoliosis.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/25/92933
Contributor Information
Sigita Burneikiene, Email: sigitab@bnasurg.com.
E. Lee Nelson, Email: nelson@bnasurg.com.
Alexander Mason, Email: mason@bnasurg.com.
Sharad Rajpal, Email: rajpal@bnasurg.com.
Benjamin Serxner, Email: bserxner@bnasurg.com.
Alan T. Villavicencio, Email: atv@bnasurg.com.
REFERENCES
- 1.Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: A technique and feasibility study. J Spinal Disord Tech. 2008;21:459–67. doi: 10.1097/BSD.0b013e318167b06b. [DOI] [PubMed] [Google Scholar]
- 2.Anand N, Rosemann R, Khalsa B, Baron EM. Mid-term to long-term clinical and functional outcomes of minimally invasive correction and fusion for adults with scoliosis. Neurosurg Focus. 2010;28:E6. doi: 10.3171/2010.1.FOCUS09272. [DOI] [PubMed] [Google Scholar]
- 3.Baron EM, Albert TJ. Medical complications of surgical treatment of adult spinal deformity and how to avoid them. Spine (Phila Pa 1976) 2006;31:S106–18. doi: 10.1097/01.brs.0000232713.69342.df. [DOI] [PubMed] [Google Scholar]
- 4.Boachie-Adjei O, Dendrinos GK, Ogilvie JW, Bradford DS. Management of adult spinal deformity with combined anterior-posterior arthrodesis and Luque-Galveston instrumentation. J Spinal Disord. 1991;4:131–41. doi: 10.1097/00002517-199106000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Bridwell KH, Lenke LG, Baldus C, Blanke K. Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients. Incidence and etiology at one institution. Spine (Phila Pa 1976) 1998;23:324–31. doi: 10.1097/00007632-199802010-00008. [DOI] [PubMed] [Google Scholar]
- 6.Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232–7. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 7.Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: Three year clinical and radiographic outcomes. Spine (Phila Pa 1976) 2009;34:2126–33. doi: 10.1097/BRS.0b013e3181b612db. [DOI] [PubMed] [Google Scholar]
- 8.Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003;34:269–79. doi: 10.1016/s0030-5898(03)00029-4. [DOI] [PubMed] [Google Scholar]
- 9.Hee HT, Castro FP, Jr, Majd ME, Holt RT, Myers L. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: Analysis of complications and predictive factors. J Spinal Disord. 2001;14:533–40. doi: 10.1097/00002517-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53:891–903. [PubMed] [Google Scholar]
- 11.Pateder DB, Kebaish KM, Cascio BM, Neubaeur P, Matusz DM, Kostuik JP. Posterior only versus combined anterior and posterior approaches to lumbar scoliosis in adults: A radiographic analysis. Spine (Phila Pa 1976) 2007;32:1551–4. doi: 10.1097/BRS.0b013e318067dc0e. [DOI] [PubMed] [Google Scholar]
- 12.Tormenti MJ, Maserati MB, Bonfield CM, Okonkwo DO, Kanter AS. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus. 2010;28:E7. doi: 10.3171/2010.1.FOCUS09263. [DOI] [PubMed] [Google Scholar]
- 13.Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ. Perioperative complications in transforaminal lumbar interbody fusion versus anterior-posterior reconstruction for lumbar disc degeneration and instability. J Spinal Disord Tech. 2006;19:92–7. doi: 10.1097/01.bsd.0000185277.14484.4e. [DOI] [PubMed] [Google Scholar]
- 14.Wang MY, Mummaneni PV. Minimally invasive surgery for thoracolumbar spinal deformity: Initial clinical experience with clinical and radiographic outcomes. Neurosurg Focus. 2010;28:E9. doi: 10.3171/2010.1.FOCUS09286. [DOI] [PubMed] [Google Scholar]
- 15.Winter RB, Denis F, Lonstein JE, Dezen E. Salvage and reconstructive surgery for spinal deformity using Cotrel-Dubousset instrumentation. Spine (Phila Pa 1976) 1991;16:S412–7. [PubMed] [Google Scholar]
- 16.Wu CH, Wong CB, Chen LH, Niu CC, Tsai TT, Chen WJ. Instrumented posterior lumbar interbody fusion for patients with degenerative lumbar scoliosis. J Spinal Disord Tech. 2008;21:310–5. doi: 10.1097/BSD.0b013e318148b256. [DOI] [PubMed] [Google Scholar]
- 17.Yadla S, Maltenfort MG, Ratliff JK, Harrop JS. Adult scoliosis surgery outcomes: A systematic review. Neurosurg Focus. 2010;28:E3. doi: 10.3171/2009.12.FOCUS09254. [DOI] [PubMed] [Google Scholar]
- 18.Zimmerman RM, Mohamed AS, Skolasky RL, Robinson MD, Kebaish KM. Functional outcomes and complications after primary spinal surgery for scoliosis in adults aged forty years or older: A prospective study with minimum two-year follow-up. Spine (Phila Pa 1976) 2010;35:1861–6. doi: 10.1097/BRS.0b013e3181e57827. [DOI] [PubMed] [Google Scholar]


