Abstract
Background:
Cervical cytology by Papanicolaou (Pap) smears is an effective means of screening for cervical premalignant and malignant conditions. Cervical intra-epithelial neoplasia (CIN) and cervical cancer remain important health problems for women worldwide.
Aim:
To study the role of Pap smear in detecting premalignant and malignant lesions of cervix; and to determine the prevalence of various lesions.
Materials and Methods:
This study is based on 300 patients who attended the out-patient Department of Obstetrics and Gynaecology. Pap smears were prepared from patients presenting with complaints like vaginal discharge, post-coital bleeding, inter-menstrual bleeding, dyspareunia, and pain lower abdomen. After fixation and staining, each smear was carefully examined.
Results:
Epithelial cell abnormalities were found in 5% smears, atypical squamous cells of undetermined significance (ASCUS) in 0.3%, squamous intraepithelial lesion (SIL) in 3.4% which includes low grade squamous intraepithelial lesion (LSIL) (2.7%) and high grade squamous intraepithelial lesion (HSIL) 0.7%. Invasive carcinoma was seen in 1.3% cases. Mean age of the patients with diagnosis of LSIL was 32.3 years and for HSIL, it was 40.5 years. The mean age of the patients with invasive carcinoma was 57 years.
Conclusion:
Premalignant and malignant lesions of cervix are not uncommon in our set up and can be diagnosed early by Pap smears.
Keywords: Cervical cancer, cervical intraepithelial neoplasia, papanicolaou smear
Introduction
Cancer cervix is the second most common cancer in women in the world, while it is the leading cancer in women in the developing countries. Globally, 15% of all cancers′ in females are cervical cancers′, while in Southeast Asia, cancer cervix accounts for 20%-30% of all cancers′. Cancer of cervix is a major cause of death in women living in developing countries.[1] In 2007, the estimated number of new cases of cancer cervix according to national cancer registry of India was 90,708 with five-year survival rate of about 48%.[2] It is estimated that in India 1,26,000 new cases occur each year.[3] Unlike most other malignancies, cancer of cervix is readily preventable when effective programmes are conducted to detect and treat its precursor lesions. Since the introduction of Pap test, a dramatic reduction has been observed in the incidence and mortality of invasive cervical cancer worldwide.[4]
Materials and Methods
This study was conducted on 300 Pap smears prepared from patients presenting with complaints like vaginal discharge, post-coital bleeding, inter-menstrual bleeding, dyspareunia and pain lower abdomen. Relevant history of illness was obtained from the patient and recorded on the proforma.
It was ensured that no local douche, antiseptic cream and no local internal examination was done on the day of test. The patient was placed in dorsal lithotomy position and a Cusco's bivalve speculum was introduced through vagina and cervix was visualized. The longer projection of the Ayre's spatula was placed in the cervix near squamo-columnar junction and rotated through 360°. The cellular material thus obtained was quickly, but gently smeared on a clean glass slide. The glass slide was then immediately put into the coplin jar containing 95% ethyl alcohol which acted as a fixative.
The prepared smears were then stained according to Papanicolaou's technique. The cytological interpretation of the smears was made according to the New 2001 Bethesda system.
Results
Maximum number of patients (45.3%) were in the age group of 31-40 years (fourth decade) followed by 33.3% in third, 17.7% in fifth, 2% in sixth decade and 1.7% in seventh decade . The most common presenting complaint was discharge per vaginum present in 177 (59%) patients. History of pain in the lower abdomen was present in 58 (19.3%), inter menstrual bleeding in 30 (10%), and 17 (5.7%) patients had complaint of dyspareunia. Post-coital bleeding was the chief complaint in 15 (5%) patients. Only three patients (1%) presented with post menopausal bleeding.
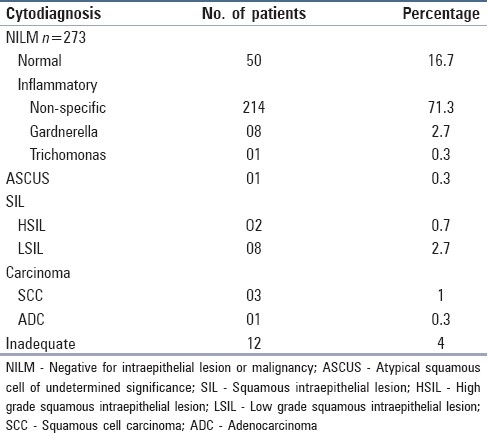
Fifteen cases were positive for malignancy, 273 were negative, and in 12 smears, the material was inadequate. Out of the 273 smears negative for any intra epithelial lesion or malignancy, 50 (16.7%) showed normal cytological findings and 223 (74.3%) were inflammatory. Out of 223 inflammatory smears, 214 (71.3%) showed non-specific inflammation, 8 (2.7%) had features of Gardnerella infection, and 1 (0.3%) had evidence of Trichomonas infection. Diagnosis of atypical squamous cells of undetermined significance (ASCUS) was made in one (0.3%) case. Squamous intraepithelial lesion was seen in 10 (3%) patients, out of which, 8 (2.7%) had low grade squamous intraepithelial lesion (LSIL) exhibiting koilocytic atypia in majority of the smears [Figure 1a]. In two cases (0.3%) of high grade squamous intraepithelial lesion (HSIL), the smears showed severely dyskaryotic cells with irregular hyperchromatic nuclei with coarsely clumped chromatin. Invasive cancer was detected in four (1.3%) cases. Three (1%) smears showed squamous cell carcinoma [Figure 1b] and one (0.3%) smear showed adenocarcinoma. Twelve (4.1%) smears were found to be inadequate [Table 1].
Figure 1.
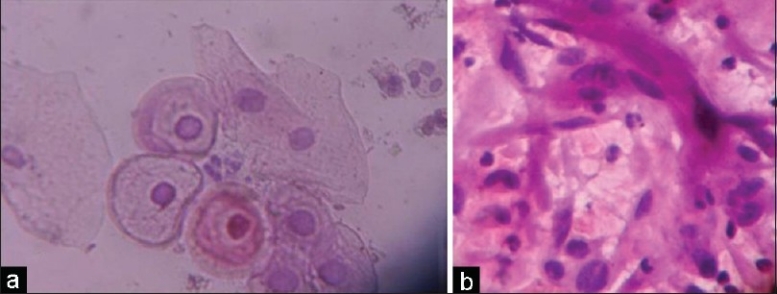
(a) Koilocytic atypia showing perinuclear halo, hyperchromatic nuclei with prominent nucleoli (Pap, ×400); (b) Squamous cell carcinoma showing strap cells signifying stromal invasion (Pap, ×400)
Table 1.
Categorisation of cytodiagnosis
Mean age of cases with low grade squamous intraepithelial lesion (LSIL) was 32.3 years and those with HSIL and invasive carcinoma were 40.5 years and 57 years, respectively. There was sequential progression in the development of LSIL to HSIL to invasive carcinoma with advancing age.
Mean age at marriage for patients with LSIL, HSIL and invasive carcinoma was 18.5 years, 19.5 years, and 18.3 years, respectively. A total of 92.9% (13 out of 14) patients with SIL and invasive carcinoma had parity.
The most common presenting complaint associated with SIL and carcinoma was vaginal discharge (71.4%) followed by post menopausal bleeding (14.4%). Most common clinical lesion seen in patients with SIL and carcinoma was erosion (35.7%) followed by cervix bleeding on touch (28.6%). Inflamed and congested cervix seen in 21.5%, hypertrophied cervix in 7.1%, and 7.1% had healthy cervix.
Discussion
Cancer cervix is considered to be an ideal gynaecological malignancy for screening as it meets both test and disease criteria for screening. It has a long latent phase during which it can be detected as identifiable and treatable premalignant lesions which precede the invasive disease and the benefit of conducting screening for carcinoma cervix exceeds the cost involved.[5]
In our study, mean age of patients with LSIL was 32.3 years, and those with HSIL and invasive carcinoma were 40.5 years and 57 years, respectively. Elhakeem et al.,[6] also recorded a progressive increase in development of LSIL to invasive carcinoma with increasing age. LSIL had peak between 20-29 years, HSIL between 30-39 years and invasive carcinoma had peak incidence in age group of 50-59 years. Afrakhteh et al.,[4] found mean age of patients with LSIL, HSIL and invasive cancer to be 37.7, 41.7 and 54.5 years, respectively. The results are in concordance with present study.
Khattak et al.,[7] and Sherwani et al.,[8] found LSIL and HSIL on cytology to be more prevalent in patients who started sexual activity before 20 years of age. The results correspond with present study as the mean age at marriage for LSIL, HSIL and carcinoma patients was 18.5, 19.5 and 18.3 years, respectively.
Present study emphasized the significance of vaginal discharge and its association with neoplastic changes in the cervix. The results correspond with many previous studies.[7,9,10]
In present series, epithelial cell abnormalities were found in 5% smears. Prevalence of ASCUS was 0.3% (1 case), SIL was seen in 3.4% (10 cases), out of which LSIL was 2.7% (8 cases) and HSIL accounted for 0.7%. Invasive cancer was seen in 1.3% cases. The results are comparable to those obtained by Patel et al.,[11] and Anuradha and Sinha.[12] Few studies[13,14] have documented a lower prevalence rate for SIL and invasive carcinoma. Possible cause for difference is that we screened only symptomatic women and thus more chances of positive results.
Conclusions
While reviewing all the results, it is concluded that premalignant and malignant lesions of cervix are not uncommon in our set up. Cervical cytology by Pap smear is a simple, safe and effective test to detect premalignant and malignant lesions of cervix at an early stage, and thus help the clinicians in early and more efficient management of the patients.
Acknowledgments
We thank the patients and technical staff of Pathology Department GMC Patiala for processing the Pap smears.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Verma K. Early diagnosis of cancer cervix- epidemiology and incidence. J Cytol. 2001;18:73–89. [Google Scholar]
- 2.Nandakumar A, Ramnath T, Chaturvedi M. The magnitude of cancer cervix in India. Indian J Med Res. 2009;130:219–21. [PubMed] [Google Scholar]
- 3.Shankaranarayan R, Nene BM, Dinshaw K. Early detection of cervical cancer with visual inspection methods: A summary of completed and ongoing studies in India. Salud Publica Mex. 2003;45:S399–407. doi: 10.1590/s0036-36342003000900014. [DOI] [PubMed] [Google Scholar]
- 4.Afrakhteh M, Khodakarami N, Moradi A, Alavi E, Shirazi FH. A study of 13315 papanicolaou smear diagnoses in Sohada hospital. J Fam Reprod Health. 2007;1:75–9. [Google Scholar]
- 5.Kerkar RA, Kulkarni YV. Screening for cervical cancer: An overview. J Obstet Gynecol India. 2006;56:115–22. [Google Scholar]
- 6.Elhakeem HA, Al-Ghamdi AS, Al-Maghrabi JA. Cytopathological pattern of cervical Pap smear according to the Bethesda system in Southwestern Saudi Arabia. Saudi Med J. 2005;26:588–92. [PubMed] [Google Scholar]
- 7.Khattak ST, Khattak I, Naheed T, Akhtar S, Jamal T. Detection of abnormal cervical cytology by pap smears. Gomal J Med Sci. 2006;4:74–7. [Google Scholar]
- 8.Sherwani RK, Khan T, Akhtar K, Zeba A, Siddiqui FA, Rahman K, et al. Conventional Pap smear and liquid based cytology for cervical cancer screening - A comparative study. J Cytol. 2007;24:167–72. [Google Scholar]
- 9.Pradhan N, Giri K, Rana A. Cervical cytology study in unhealthy and healthy looking cervix. N J Obstet Gynaecol. 2007;2:42–7. [Google Scholar]
- 10.Kenneth DH, Yao SF. Cervical and vaginal cancer. In: Novak's Gynecology. 13th ed. Philadelphia: Lipincott Williams and Wilkins; 2002. pp. 471–93. [Google Scholar]
- 11.Patel TS, Bhullar C, Bansal R, Patel SM. Interpreting epithelial cell abnormalities detected during cervical cancer screening: A cytohistologic approach. Eur J Gynaecol Oncol. 2004;25:725–8. [PubMed] [Google Scholar]
- 12.Anuradha, Sinha A. Conventional pap smear screening for human papilloma virus related lesions of cervix. J Cytol. 2005;22:32–4. [Google Scholar]
- 13.Luthra UK, Prabhakar AK, Seth P, Agarwal SS, Murthy NS, Bhatnagar P, et al. Natural history of precancerous and early cancerous lesions of the uterine cervix. Acta Cytol. 1987;31:226–34. [PubMed] [Google Scholar]
- 14.Kapila K, George SS, Al-Shaheen S, Al-Ottibi MS, Pathan SK, Sheikh ZA, et al. Changing spectrum of squamous cell abnormalities observed on Papanicolaou smears in Mubarak Al-Kabeer Hospital, Kuwait, over a 13-year period. Med Princ Pract. 2006;15:253–9. doi: 10.1159/000092986. [DOI] [PubMed] [Google Scholar]


