Abstract
Systemic lupus erythematosus (SLE) is a chronic inflammatory disease typically diagnosed by a combination of physical findings and clinical laboratory testing. Several decades ago, the diagnosis of lupus included the lupus erythematosus (LE) cell assay. SLE is associated with pleuropulmonary manifestations in well over 50% of cases. Although pleural effusion is common but very rarely is the initial manifestation of disease. There are very few reports of SLE diagnosed in a cytopathology laboratory. We report an unusual case of SLE in a 16-year-old female who presented with acute shortness of breath, fever and cough. Her chest radiograph showed bilateral pleural effusion. This effusion was tapped and sent to the cytopathology laboratory. The cytological examination of the pleural fluid revealed numerous LE cells and led to the diagnosis of SLE. Autoimmune serology techniques such as anti-nuclear antibody staining have replaced the LE cell assay. However, as presented in this report and found in a review of the literature, the in vivo finding of LE cells by cytopathology can provide an important clue to the diagnosis of SLE, especially when associated with an uncommon presentation.
Keywords: LE cells, pleural effusion, systemic lupus erythematosus, tart cells
Introduction
Systemic lupus erythematosus (SLE) is a common autoimmune disorder that primarily affects women and can involve virtually any organ in the body.[1] In SLE, it is not uncommon to see pleuropulmonary involvement in isolation or along with the involvement of other organ systems. Lupus pleuritis is the most common manifestation of SLE in the chest but it occurs as an initial presentation in only 2.5–3% of patients. Pleural effusion itself can be very rarely the first manifestation of SLE, seen in 1–2% of patients. The prognosis of lupus pleuritis/effusion is generally good.[2] The case we present illustrates the importance of careful evaluation of serous effusion, as in vivo finding of LE cells can provide important clue to the diagnosis.
Case Report
In this report, we describe an unusual case of a 16-year-old female who presented with fever, chills and cough of 8 days. She also developed acute shortness of breath in the last 2 days. On examination, the patient was in mild distress with dullness of the percussion note and decreased breath sounds in both lower lung fields. A chest radiograph demonstrated blunting of costophrenic angles and bilateral pleural effusion. Worsening of dyspnea necessitated surgical drainage of the pleural effusion. Approximately, 700 mL of serosanguinous fluid was tapped and sent to cytopathology laboratory for evaluation.
On examination of the MGG-stained cytospin preparation of the pleural fluid, plenty of LE cells were seen, characterized by a homogenous nuclear material engulfed by neutrophils [Figure 1a]. These cells were present in the background of numerous segmented neutrophils, lymphocytes, plasma cells, and macrophages. Occasional tart cells (a cell characterized by a homogenous nuclear material engulfed by macrophage) were also seen [Figure 1b]. Other laboratory investigations included the WBC count (3.2 × 103/μL with a normal differential count), hematocrit (30%), platelet count (180 × 103/μL) and erythrocyte sedimentation rate (52 mm/h). Subsequently, the diagnosis of SLE was confirmed by antinuclear antibody (ANA) titre which showed the positive results. Treatment with prednisolone 20 mg daily was begun. There was a rapid clinical response including the resolution of the fever and pleural effusion.
Figure 1.
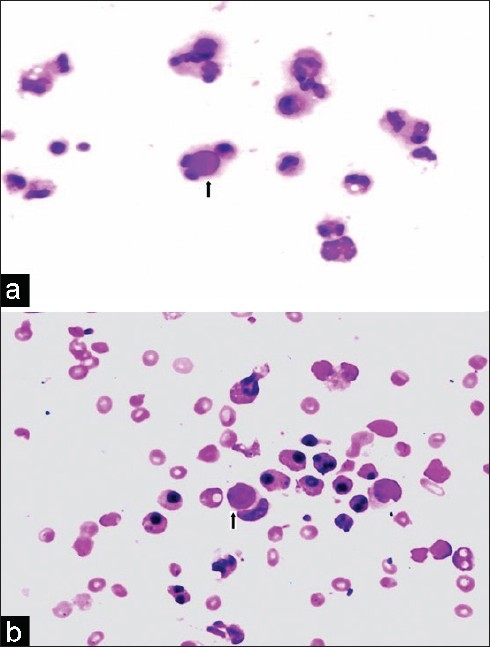
(a) Cytospin preparation of the pleural fluid showing plenty of lupus erythematosus (LE) cells (MGG, ×400). (b) Cytospin preparation of the pleural fluid showing tart cell (MGG, ×400)
Discussion
SLE is a chronic inflammatory autoimmune disorder that more commonly affects women. It is a multi-organ disease and may affect any organ system. It commonly presents with arthralgias, arthritis, a rash (which may be photosensitive), and renal involvement. Pulmonary involvement in SLE is common, pleuritis being the most frequent manifestation. Pleural inflammation is a common feature of SLE; however, as an initial presentation in SLE, it is very rare, reported only in 1–2% of cases.[3]
In an analysis of 520 patients with SLE by Dubois and Tuffanelli,[4] pleuritis occurred in 45% of patients, and a pleural effusion occurred in 30%. Pleurisy and pleural effusion were the initial manifestation in 3% and 1% of patients, respectively. However, in patients with late-onset (after the age of 50 years) SLE, pleuritis is even more common. In one study, it was the presenting manifestation in 27% of patients with late-onset SLE.[5]
Other pulmonary manifestations of SLE include pneumonitis, alveolar hemorrhage, bronchiolitis obliterans with organizing pneumonia, lymphocytic interstitial pneumonia, pulmonary hypertension, vasculitis, pulmonary embolism, and diaphragmatic weakness.[6]
In our case, the patient presented with dyspnea accompanied by fever and cough. Several diagnostic possibilities exist in such a case including pulmonary embolus, viral infection, parapneumonic effusion, tuberculosis, congestive heart failure, and collagen vascular disorders. A simple cytological preparation revealed plenty of LE cells and led to the diagnosis of SLE which was further confirmed by pleural fluid and serum ANA tests. Intravenous steroid therapy was initiated, after which the bilateral pleural effusions dramatically improved. Serous effusions as a result of SLE tend to be more common in the chronic stage of the disease, and the presence of LE cells in an effusion is associated with the presence of active disease.[3]
Pleural effusion due to lupus pleuritis is typically an exudate and may be unilateral or bilateral. In most cases, the glucose is >60 mg/dL and the complement levels are frequently low.[6,7]
The presence of LE cells in the pleural fluid is highly specific for SLE. LE cells are neutrophilic phagocytes that contain intracytoplasmic hematoxylin bodies. The hematoxylin bodies are thought to be formed by the opsonization of cells by ANA typically found in SLE patients. These antibodies lead to the denaturation of dead or injured cells, forming homogenous oval-shaped bodies that are referred to as “hematoxylin bodies’ because they stain blue with common cytological stains such as Wright-Giemsa, Papanicolaou, and hematoxylin and eosin stains. The hematoxylin bodies are engulfed by neutrophils, creating LE cells. In cytological preparations, LE cells must be distinguished from ‘tart cells’ or ‘pseudo-LE cells’, which result from the phagocytosis of nuclear debris by macrophages, rather than neutrophils, and are generally seen in effusion fluid – independent of the cause of the effusion. The phagocytosed debris within the tart cell is smaller, and has a non-homogenous (clumped) appearance in contrast to the smooth homogenous character of the hematoxylin bodies in true LE cells.[3,6] The incubation of the pleural fluid at room temperature for several hours may enhance the LE cell phenomenon.[6,7]
LE cells are also seen in the bone-marrow aspiration material, synovial fluid, cerebrospinal fluid, and pericardial fluid of SLE patients. The presence of LE cells in any of these specimens, in conjunction with the appropriate clinical picture and laboratory values, would contribute to the diagnosis of SLE.[3]
The prognosis of lupus serositis is generally good. Most patients with lupus pleuritis respond favorably to oral corticosteroids. The clinical and radiographic improvement is rapid and complete in most patients. Other immunosuppressive agents, such as azathioprine, may be used in patients whose response to steroids is slow or unsatisfactory.[2]
Conclusion
Several decades ago, the diagnosis of lupus included the LE cell assay. Autoimmune serology techniques such as anti-nuclear antibody staining have replaced this technique. However, as presented in this report, the in vivo finding of LE cells by cytopathology can provide important clue to the diagnosis of SLE, especially when associated with an uncommon presentation. The finding of the LE cells is helpful in establishing the previously unsuspected diagnosis of lupus pleuritis, as beneficial treatment could be initiated.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Park JY, Malik A, Dumoff KL, Gupta PK. Case report and review of lupus erythematosus cells in cytology fluids. Diagn Cytopathol. 2007;35:806–9. doi: 10.1002/dc.20758. [DOI] [PubMed] [Google Scholar]
- 2.Sarwar A, Dellaripa PF, Beamis JF., Jr A 51-year-old man with fever, ulnar neuropathy and bilateral pleural effusions.Lupus pleuritis. Chest. 1999;116:1105–7. doi: 10.1378/chest.116.4.1105. [DOI] [PubMed] [Google Scholar]
- 3.Wan KS. Pleuritis and pleural effusion as an initial presentation of systemic lupus erythematosus in a 23-year-old woman. Rheumatol Int. 2008;28:1257–60. doi: 10.1007/s00296-008-0598-4. [DOI] [PubMed] [Google Scholar]
- 4.Dubois EL, Tuffanelli DL. Clinical manifestations of systemic lupus erythematosus: Computer analysis of 520 cases. JAMA. 1964;190:104–11. doi: 10.1001/jama.1964.03070150014003. [DOI] [PubMed] [Google Scholar]
- 5.Baker SB, Rovira JR, Campion EW, Mills JA. Late onset systemic lupus erythematosus. Am J Med. 1979;66:727–32. doi: 10.1016/0002-9343(79)91109-4. [DOI] [PubMed] [Google Scholar]
- 6.Hepburn AL. The LE cell. Rheumatology (Oxford) 2001;40:826–7. doi: 10.1093/rheumatology/40.7.826. [DOI] [PubMed] [Google Scholar]
- 7.Kushwaha R, Shashikala P, Hiremath S, Basavaraj HG. Cells in pleural fluid and their value in differential diagnosis. J Cytol. 2008;25:138–43. [Google Scholar]


