Abstract
Background
Three competing goals at academic medical centers are to increase efficiency, to optimize clinical care, and to train residents. The goal of this project was to compare day surgery operating room (OR) efficiency measures for anesthesiologists working alone, working with residents, and working with certified nurse anesthetists in a tertiary multisubspecialty teaching hospital to determine if trainees significantly impact OR efficiency.
Methods
We retrospectively evaluated operating room times data for 2,427 day surgery cases, comparing first case on-time starts, anesthesia-controlled times, induction times, emergence times, and turnover times for the 3 anesthesiologist groups.
Results
Compared to the solo anesthesiologist group, anesthesiologists working with residents had significantly longer induction, emergence, and total anesthesia-controlled times (20.2 ± 8.0 vs 18.4 ± 7.0 minutes). However, the anesthesiologists working with residents had more on-time starts (65% vs 53%) and lower turnover times 47.3 ± 13.6 vs 50.8 ± 14.5 minutes) than the solo anesthesiologist group.
Conclusion
The pairing of anesthesiology residents with anesthesia staff has mixed effects on OR efficiency measures in a day surgery unit.
Keywords: Ambulatory anesthesia, operating room management, turnover times
INTRODUCTION
Operating room (OR) efficiency has become a high priority for many institutions.1-4 OR delays can increase costs, decrease patient and surgeon satisfaction,5-7 and delay the delivery of patient care,8 so improving OR efficiency is critical in today's managed care environment with decreasing reimbursements and increasing costs. Ambulatory surgery has experienced exponential growth over the past 20 years.9,10 OR efficiency is key to a successful ambulatory practice, resulting in decreased overnight hospital stays, the ability to fast-track patients through the recovery phases, and increased patient convenience.4,11
Competing with the goal to increase efficiency at academic institutions is the need to train residents and to simultaneously optimize clinical care. We have previously shown that the introduction of new anesthesiology trainees into the OR minimally increases anesthesia-controlled measures of efficiency when looking at the OR suite as a whole.12,13 Little or no work has been done to evaluate whether anesthesia residents change OR efficiency measures of anesthesia-controlled times, first case on-time starts, or turnover times in ambulatory surgery. These changes can be potentially significant because cases are short, and the high priority given to efficiency can have a significant impact on the way cases are scheduled. For example, although little research exists to support the request, limiting or eliminating anesthesia resident participation in ambulatory surgery may be requested because of concerns about decreasing efficiency.
The goal of this study was to examine day surgery OR efficiency data to evaluate whether anesthesiologists working with residents or nurses differed in efficiency compared to when they worked solo. Based on our earlier work,12 we hypothesized that anesthesiologists working solo or with nurse anesthetists would be significantly more efficient because of the greater time inexperienced residents require to accomplish tasks and the time required of anesthesiologists to teach the residents.
METHODS
All OR data were collected at the Brigham and Women's Hospital in Boston, Massachusetts, a 754-bed, academic tertiary-care hospital with 43 ORs. This retrospective, observational study was approved by the Institutional Review Board at the Brigham and Women's Hospital in July 2005. The data were collected on 2,427 day surgery cases from September 1, 2005, to March 30, 2007. Patients included were American Society of Anesthesiologists (ASA) 1 and 2 outpatients undergoing common ambulatory procedures under general anesthesia. Patients were excluded from the study if they had a history of chronic pain medication use and significant comorbidities (ie ASA status of ≥3).
We evaluated 3 groups: anesthesiology staff working solo (S), anesthesiology staff working with a certified nurse anesthetist (SNA), and anesthesiology staff working with a resident (SR). We compared OR efficiency outcomes for these 3 anesthesiologist groups.
Basic demographic data collected included the patient's age, gender, and weight. Type and duration of surgery were also recorded. To provide a more accurate comparison among the study groups, only patients undergoing common ambulatory procedures under general anesthesia were included. Although the anesthesia techniques for most of the surgical procedures studied are standardized at our institution, we did not attempt to control or modify the specific anesthetic techniques the groups used. The anesthesiologists, nurse anesthetists, and residents involved in the care of study patients were not aware of the study or of any specific parameters being measured. Thus, each anesthesiologist or team developed and executed an anesthetic plan according to their usual practice.
OR nursing staff entered OR times according to American Association of Clinical Directors definitions.14 Induction time (IT) was defined as the period starting when the patient entered an OR to when the airway was secured and the patient was turned over to the surgical team. Emergence time (ET) was defined as the time starting when the surgical dressing was completed to when the patient left the OR. Anesthesia-controlled time (ACT) is the sum of the 2 times: ACT = IT + ET.
In addition to ACT, the OR nurses also captured first case start time and turnover time. Data extracted from the computerized OR information system included (1) time the room is deemed ready by the OR nurses; (2) time the patient enters the room; (3) time anesthesia induction is complete and surgical preparation may start; (4) end of surgery time; (5) time the patient is ready for transfer; and (6) time the patient leaves the room. ACTs and turnover times were controlled for surgery type and duration.
Statistical Analysis
Means or percentages of intraoperative characteristics are presented for all patients and for each group. The means of continuous variables were compared between groups using independent sample t test, and the percentages for dichotomous and categorical variables were compared using the chi-square test. Least squares regression was used to assess the differences in times among the three groups, controlled for type of surgery or duration of surgery, as appropriate. Actual time differences were also calculated by subtracting the means or percentages for the S group from the SNA and SR groups. Power analysis conducted to detect a mean difference of 10% in turnover times with alpha = 0.05 and beta = 0.8 estimated a need to have 370 patients in each group. All analyses were performed using SAS 9.1 (SAS Institute, Cary, NC).
RESULTS
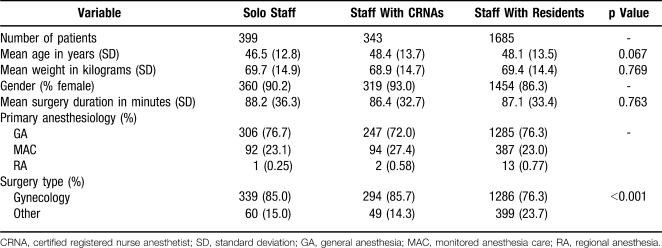
Of the 2,427 cases studied, 399 were performed by solo staff, 343 by staff working with a certified nurse anesthetist, and 1,685 by staff working with residents. Table 1 depicts patient characteristics for the 3 study groups.
Table 1.
Characteristics of Intraoperative Variables
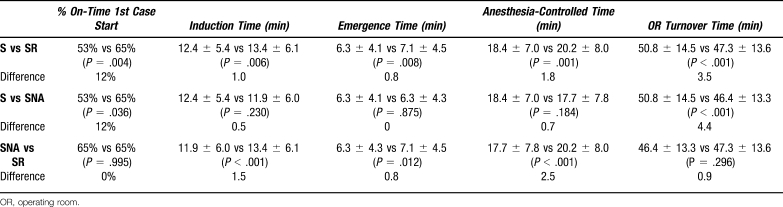
Compared to the anesthesiologists working alone (S) or with nurse anesthetists (SNA), anesthesiologists working with residents (SR) had longer induction times (12.4 ± 5.4 [S] vs 13.4 ± 6.1 [SR] [P = .006] vs 11.9 ± 6.0 minutes [SNA] [P < .001]), longer emergence times (6.3 ± 4.1 [S] vs 7.1 ± 4.5 [SR] [P = .008] vs 6.3 ± 4.3 minutes [SNA] [P = .012]), and longer ACTs (18.4 ± 7.0 [S] vs 20.2 ± 8.0 [SR] [P = .001] vs 17.7 ± 7.8 minutes [SNA] [P < .001]).
Interestingly, the S group had worse first case on-time starts compared to the SR and SNA groups (53% vs 65% [P = .004] vs 65% [P = .036]) and longer turnover times than either the SR or SNA group (50.8 ± 14.5 vs 47.3 ± 13.6 [P < .001] vs 46.4 ± 13.3 minutes [P < .001]). There were no differences in turnover time between the SNA and SR groups, but the SNA group did have faster induction times, emergence times, and ACTs compared to the SR group. Table 2 summarizes these results.
Table 2.
Efficiency Measures for Solo Anesthesiologist Staff (S), Staff Working With Certified Registered Nurse Anesthetists (SNA), and Staff Working With Residents (SR)
DISCUSSION
Although modifications to improve turnover times, first case on-time starts, and ACTs typically yield negligible or small improvements, OR management committees devote much time and many resources to them.15-17
The factors involved in turnover time and ACT are complex and multifunctional, but specific anesthesia-related modifications can improve or detract from the overall time efficiency in the OR.5,13 Our results in this OR data analysis show that staff working with residents experienced statistically significant time increases in induction time and emergence time. On the other hand, perhaps not surprisingly, solo anesthesiologists had significantly longer turnover times and fewer first case on-time starts than staff working with residents or nurse anesthetists. The actual time differences are small, with turnover time approximately 1-2 minutes slower with the resident group and 3 minutes slower with the solo staff group. Because those working solo had fewer first case on-time starts, in an average day at our institution, the differences would largely cancel each other out. Staff working with nurse anesthetists was the most efficient pairing in our study, yielding a 10-15 minute daily advantage in efficiency for 3-4 cases in the operating room.
Our current study is similar to our earlier work showing that the introduction of new residents to the OR does not significantly change efficiency or ACT. Hospital administrators and surgeons argue for greater efficiency, especially in ambulatory surgery settings, and for consequently limiting the training component in these settings. Results of our current study indicate that little reason exists to justify limiting anesthesia resident training in ambulatory operating rooms in a large academic OR service. The small increase in induction and emergence times is understandable and predictable for trainees and remains consistent with prior research. The faster turnover times and better first case on-time starts for both the staff-resident and staff-nurse anesthetist combinations over the solo staff group make a compelling efficiency argument for the team model of care. Again, it seems logical that two people can be more efficient than one when accomplishing a number of tasks, especially tasks in a series (eg, taking a patient to the postanesthesia care unit, starting an intravenous line for the next patient, setting up the room, and so on). We would argue that having residents or nurse anesthetists paired with staff anesthesiologists leads to greater efficiencies in these components of care.
One reason that we did not see a more significant improvement for the resident and nurse anesthetist groups may be because the systems in place in our ambulatory division compel all who work there to function at similar levels of efficiency. Thus when either solo staff or staff with residents or nurse anesthetists work in the ambulatory area, they cannot adversely (or positively) change the already established processes in place to optimize efficiency. The factors leading to efficiencies in turnover time or first case on-time starts are complex and multifactorial, and it is well recognized that isolated changes by one group (anesthesiologists, surgeons, nurses, ancillary staff) can rarely lead to significant efficiency improvements.13,18
Our study has a number of limitations. Because the different groups were not randomized to their cases, the solo anesthesiologists or the anesthesiologist-nurse anesthetist groups may have been scheduled to work with the more routine cases while the resident groups were assigned to the more challenging cases. Although we could not detect any differences in the patients, types of cases, or surgeons assigned to the groups, such differences are possible and could explain the small increases in ACT seen in the anesthesiologist-resident group. We believe a more likely cause is that the inexperienced member of the team works a little bit slower. Some evidence in the literature supports the idea that trainees decrease operating room efficiency.19,20 Also, the solo anesthesiologists and nurse anesthetists may have been more attuned to the entry of efficiency times by nurses and may have paid greater attention when nurses with whom they were unfamiliar were entering times, leading to more accurate results. We have no way of distinguishing between these factors, but we believe that this bias was prevented because neither the anesthesiologists nor the nurses entering the times were aware of the study. Our previous published report argues that this issue would not make a difference in our academic setting.12
There are, of course, potential non-efficiency-related benefits to having anesthesia-specific staffing. For example, patient safety and patient satisfaction may be improved19 and complication rates such as postoperative nausea and vomiting may be reduced when experienced nurse anesthetists work with anesthesiologists or when anesthesiologists work alone. Our current study does not evaluate these aspects of training-specific staffing.
CONCLUSIONS
Results of our study suggest that an anesthesiologist-resident care team in an academic setting has slightly worse efficiency measures for induction and emergence times than solo or anesthesiologist-nurse anesthetist teams for ambulatory patients, but the better turnover times for the resident-anesthesiologist team make up for this difference. For overall efficiency in ambulatory operating rooms, the nurse anesthetist-anesthesiologist team may be the best model.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Interpersonal and Communication Skills, and Systems-Based Practice.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
REFERENCES
- 1.Gordon T, Paul S, Lyles A, Fountain J. Surgical unit time utilization review: resource utilization and management implications. J Med Syst. 1988 Jun;12(3):169–179. doi: 10.1007/BF00996639. [DOI] [PubMed] [Google Scholar]
- 2.Steele JT, Hoyt DB, Simons RK, Winchell RJ, Garcia J, Fortlage D. Is operating room resuscitation a way to save time. Am J Surg. 1997 Dec;174(6):683–687. doi: 10.1016/s0002-9610(97)00194-3. [DOI] [PubMed] [Google Scholar]
- 3.Valenzuela RC, Johnstone RE. Cost containment in anesthesiology: a survey of department activities. J Clin Anesth. 1997 Mar;9(2):93–96. doi: 10.1016/S0952-8180(97)00230-4. [DOI] [PubMed] [Google Scholar]
- 4.Overdyk FJ, Harvey SC, Fishman RL, Shippey F. Successful strategies for improving operating room efficiency at academic institutions. 1998 Apr;86(4):896–906. doi: 10.1097/00000539-199804000-00039. [DOI] [PubMed] [Google Scholar]
- 5.McIntosh C, Dexter F, Epstein RH. The impact of service-specific staffing, case scheduling, turnovers, and first-case starts on anesthesia group and operating room productivity: a tutorial using data from an Australian hospital. Anesth Analg. 2006 Dec;103(6):1499–1516. doi: 10.1213/01.ane.0000244535.54710.28. [DOI] [PubMed] [Google Scholar]
- 6.Strum DP, Vargas LG, May JH. Surgical subspecialty block utilization and capacity planning: a minimal cost analysis model. Anesthesiology. 1999 Apr;90(4):1176–1185. doi: 10.1097/00000542-199904000-00034. [DOI] [PubMed] [Google Scholar]
- 7.Harders M, Malangoni MA, Weight S, Sidhu T. Improving operating room efficiency through process redesign. Surgery. 2006 Oct;140(4):509–514; discussion 514-516. doi: 10.1016/j.surg.2006.06.018. Epub 2006 Aug 28. [DOI] [PubMed] [Google Scholar]
- 8.Weinbroum AA, Ekstein P, Ezri T. Efficiency of the operating room suite. Am J Surg. 2003 Mar;185(3):244–250. doi: 10.1016/s0002-9610(02)01362-4. [DOI] [PubMed] [Google Scholar]
- 9.White PF, Smith I. Ambulatory anesthesia: past, present, and future. Int Anesthesiol Clin. 1994 Summer;32(3):1–16. [PubMed] [Google Scholar]
- 10.Pasternak LR. Preanesthesia evaluation and testing. In: Twersky RS, Philip BK, editors. Handbook of Ambulatory Anesthesia. 2nd ed. New York, NY: Springer; 2008. pp. 1–23. [Google Scholar]
- 11.Joshi GP. Efficiency in ambulatory surgery center. Curr Opin Anaesthesiol. 2008 Dec;21(6):695–698. doi: 10.1097/ACO.0b013e328311d1b2. [DOI] [PubMed] [Google Scholar]
- 12.Eappen S, Flanagan H, Bhattacharyya N. Introduction of anesthesia resident trainees to the operating room does not lead to changes in anesthesia-controlled times for efficiency measures. Anesthesiology. 2004;101(5):1210–1214. doi: 10.1097/00000542-200411000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Eappen S, Flanagan H, Lithman R, Bhattacharyya N. The addition of a regional block team to the orthopedic operating rooms does not improve anesthesia-controlled times and turnover time in the setting of long turnover times. J Clin Anesth. 2007 Mar;19(2):85–91. doi: 10.1016/j.jclinane.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Donham RT, Mazzei WJ, Jones RL. Glossary of times used for scheduling and monitoring of diagnostic and therapeutic procedures. Am J Anesthesiol. 1997;22(5S):3–12. [Google Scholar]
- 15.Wachtel RE, Dexter F. Influence of the operating room schedule on tardiness from scheduled start times. Anesth Analg. 2009 Jun;108(6):1889–1901. doi: 10.1213/ane.0b013e31819f9f0c. [DOI] [PubMed] [Google Scholar]
- 16.Wachtel RE, Dexter F. Reducing tardiness from scheduled start times by making adjustments to the operating room schedule. Anesth Analg. 2009 Jun;108(6):1902–1909. doi: 10.1213/ane.0b013e31819f9fd2. [DOI] [PubMed] [Google Scholar]
- 17.Macario A. Are your hospital operating rooms “efficient”? A scoring system with eight performance indicators. Anesthesiology. 2006 Aug;105(2):237–240. doi: 10.1097/00000542-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Mariano ER, Chu LF, Peinado CR, Mazzei WJ. Anesthesia-controlled time and turnover time for ambulatory upper extremity surgery performed with regional versus general anesthesia. J Clin Anesth. 2009 Jun;21(4):253–257. doi: 10.1016/j.jclinane.2008.08.019. Epub 2009 Jun 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Posner KL, Freund PR. Resident training level and quality of anesthesia care in a university hospital. Anesth Analg. 2004 Feb;98(2):437–442, table of contents. doi: 10.1213/01.ANE.0000097173.20740.06. [DOI] [PubMed] [Google Scholar]
- 20.St. Jacques P, James H, Higgins M. Level of training of anesthesiology resident or nurse anesthetist affects anesthesiology controlled intraoperative time periods. J Clin Anesth. 2003 Feb;15(1 Abstract):77. [Google Scholar]