Abstract
Background
Early detection of an impending flood and the availability of countermeasures to deal with it can significantly reduce its health impacts. In developing countries like India, public primary health care facilities are frontline organizations that deal with disasters particularly in rural settings. For developing robust counter reacting systems evaluating preparedness capacities within existing systems becomes necessary.
Objective
The objective of the study is to assess the functional capacity of the primary health care system in Jagatsinghpur district of rural Orissa in India to respond to the devastating flood of September 2008.
Methods
An onsite survey was conducted in all 29 primary and secondary facilities in five rural blocks (administrative units) of Jagatsinghpur district in Orissa state. A pre-tested structured questionnaire was administered face to face in the facilities. The data was entered, processed and analyzed using STATA® 10.
Results
Data from our primary survey clearly shows that the healthcare facilities are ill prepared to handle the flood despite being faced by them annually. Basic utilities like electricity backup and essential medical supplies are lacking during floods. Lack of human resources along with missing standard operating procedures; pre-identified communication and incident command systems; effective leadership; and weak financial structures are the main hindering factors in mounting an adequate response to the floods.
Conclusion
The 2008 flood challenged the primary curative and preventive health care services in Jagatsinghpur. Simple steps like developing facility specific preparedness plans which detail out standard operating procedures during floods and identify clear lines of command will go a long way in strengthening the response to future floods. Performance critiques provided by the grass roots workers, like this one, should be used for institutional learning and effective preparedness planning. Additionally each facility should maintain contingency funds for emergency response along with local vendor agreements to ensure stock supplies during floods. The facilities should ensure that baseline public health standards for health care delivery identified by the Government are met in non-flood periods in order to improve the response during floods. Building strong public primary health care systems is a development challenge. The recovery phases of disasters should be seen as an opportunity to expand and improve services and facilities.
Keywords: public, health Facility, flood, preparedness, response, India, Orissa, primary health care, natural disasters, disaster management, humanitarian crisis, climate change, extreme weather
Over 216 hydrological disasters (85.2% floods) were reported in 2010 across the world with about 189 million victims. The occurrence of these disasters increased by 20% over 2009 and was above the annual average of 192 for the last decade (1). Furthermore, the intensity of flooding is expected to rise with the changes in climate (2 3). The health impacts of floods are most pronounced in developing countries, where weak health care systems are already overburdened. The impacts on the health care systems are twofold – direct impacts on infrastructure for instance structural damage to health facilities resulting in primary failures and secondary failures that result mainly from exhaustion of supplies and staff burn outs (4 5). Systemic failures irrespective of the type prevent the much required early response.
Patients with limited options in their choice of health care are at greater risk to suffer worsened health impacts (6). When public hospitals are impacted the poor are more likely to be disproportionally affected. Private health care facilities have the option to close shop adding to the burden on public facilities which are seldom in a position to sustain (7). In low and middle income countries like India, public primary health care facilities are frontline organizations that deal with disasters particularly in rural settings (8 9). During flooding, the increased frequency of diseases, injured, together with new patients seeking care, compounded by minimal resource availability, significantly reduces the ability of the system to respond adequately (10 11).
Preparedness holds the key. Early detection of an impending flood and the availability of countermeasures within health systems to deal with it can significantly reduce the health impacts on a population (12). However, health systems are labour intensive and require qualified and experienced staff to function well. In order to develop robust counter reacting systems, evaluating preparedness capacities within existing systems becomes necessary (3). Initial assessments should focus on identifying vulnerable facilities and populations; anticipate needs; and investigate the average disruption time in order to prepare for the next event (13).
Surge capacity is defined as ‘the ability to rapidly meet increased demand for medical care and absorb the increase in number of patients. It consists of three essential components namely staff, supplies, and structure’ (14 15). Each disaster event may or may not require surge. There are no standardized measures for surge capacity and quantifying and standardizing surge in these conditions is a complex process. Each facility is independent and should assess its own vulnerabilities and plan realistically according to its unique needs (16 17).
The impacts of floods on the use of primary and secondary health care services have not been extensively investigated (2). Over 62% of the 547 publications in the US from 1997 to 2008 in the field of emergency preparedness in public health systems were commentaries or reviews rather than primary research (18). Furthermore, very little has been said about internal disasters in facilities and how they cope with these situations (19). Often planning assumptions in health care facilities of most low and middle income countries including India, are based on conventional wisdom than evidence (8).
The WHO advocates strengthening of the six building blocks of the health system namely service delivery; health workforce; information; medical products, vaccines and technologies; financing; and leadership and governance (stewardship) to improve health outcomes which also serves as an important point of departure in creating sustainable health systems to combat disasters such as floods (20).
The objective of the study is to assess the functional capacity of the primary health care system in Jagatsinghpur district of rural Orissa in India to respond to the devastating flood of September 2008. The study aims to serve as a baseline for comparisons to future evaluations.
Methods
Study area
Orissa is situated on the Eastern coast of India along the Bay of Bengal. Due to its sub-tropical littoral location and long coastline, the state is prone to post monsoon flooding, tropical cyclones, and storm surges. The September 2008 flood was due to heavy rainfall in the upper as well as lower catchments of the Mahanadi River System and lasted from the 16th to 21st September 2008. The magnitude and severity of this event surpassed the ferocities of 1982 and 2001 floods which were known to be the worst. As per preliminary report PWD roads were damaged with over 97 breaches across 1,927.60 km and 956 rural roads measuring 2,925 km were washed away. Twenty one districts including 8062 villages and over 4.5 million people were affected. Ninety six human lives were lost and over 213,000 houses were damaged in the state. In Jagatsinghpur district, with a population of 1,058,894, all the eight blocks including 188 villages and 147,427 people were severely affected. Over 8,072 houses were completely damaged in the flood. (21). We conducted the study in Jagatsinghpur which has been affected by eleven floods in the last two decades. The five worst affected blocks (Governmental administrative units) namely Erasama, Kujang, Tirtol, Balikuda and Biridi were included in the study (See Fig. 1).
Fig.1.
Study site.
The Chief District Medical Officer (CDMO) of Jagatsinghpur district was in-charge of organizing the response that included setting up – a control room, mobile health unit, stock indenting, and coordination of the 29 public health care centres in the district. The CDMO together with the medical officers, sanitary inspectors and field health workers were also responsible to monitor, control and prevent outbreaks. The team faced difficulties with reaching remote places with relief.
Study design and participants
Public sector health care system in India is organized at three levels. The general hospital at the district constitutes the apex of system. The next level is the community health centre (CHC) a 30 bed hospital covering a population of 100,000 and serving as the first referral level (22). The next level includes primary health centre (PHC) covering a population of 30,000. Conceptually, the PHC is the organizational pivot through which the integrated services are delivered at the community level to the entire population. The PHCs are expected to provide out- and in-patient services. However these centres do not have sophisticated diagnostic equipments or OT facilities (23). Each PHC has 4–5 sub-centre's attached to them that cover a population of 5,000 and are expected to provide out-patient services with field services in the area of community health through Auxiliary Nurse Midwives (ANMs); multi-purpose health workers (MPWs) and ASHA (Accredited Social Health Activists)(24).
A list of all the health centres in the five identified blocks was procured. A total of 31 health centres were listed in the five blocks. Of which two were non functional and therefore excluded. An onsite survey was conducted in all the 29 public health care facilities (PHC) available in the study area which was predominantly rural. The interviewees included 29 chief medical officers. A No Objection Certificate was obtained from the relevant government authorities to conduct the study. Informed consent was obtained from all the participants before commencing the interviews.
Instruments and data collection
The pre-tested structured questionnaire was administered face to face. The interviewer visited the assigned centre a maximum of three times to obtain data. No incentives were offered for participation. The questionnaire investigated routine workload and services provided at the facilities; bed capacity; quality of care provided; Health Information Management systems including routine and emergency surveillance; functioning of accessory systems such as electricity, solid waste, and access roads; and contingency and preparedness activities and plans in the facility. The time frame of the disaster was set as before = 1 month before onset of the flood, during disaster = September–October 2008 and after disaster = at the time of interview (15th November–18th December 2008). The Voluntary Health Association of India (VHAI) team who were the official project partners in India led the study.
Data analysis
Data obtained from the onsite survey was recorded on the paper based collection forms. The data was entered, processed and analyzed using STATA®10. Descriptive analyses were tabulated for the survey items.
Results
Health services provision
Health conditions treated
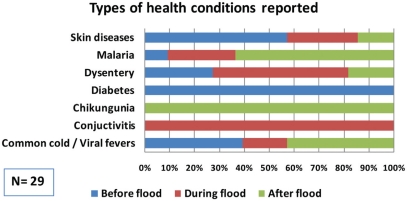
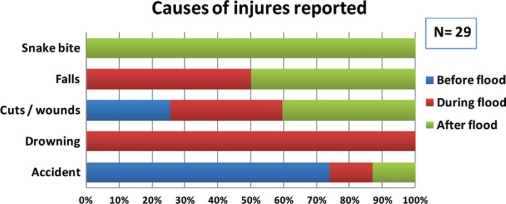
Some of the most prevalent diseases in the area before the flood in 2008 were skin diseases, viral fevers, diarrhea, common cold and malaria. The frequencies fluctuated during and after the flood. During the time of the flood diarrhea, dysentery, conjunctivitis, and viral fever with pain were the most common types of diseases reported. Common cold / viral fevers; malaria; diarrhea; and chikungunya were some of the most common conditions after the flood. Conjunctivitis emerged as a major health care challenge during the flood. Chikungunya which was not endemic to the district was reported for the first time following this flood. Injuries emerged as the most common health conditions treated during the flood. The most common reasons of injuries were cuts / wounds, snake bites, and minor accident related injuries. Snake bites presented as major logistic challenge particularly with the transport of anti-venom from the district headquarter to the facilities (Figs. 2 and 3).
Fig. 2.
Health conditions treated at the facilities.
Fig. 3.
Main causes of injuries reported.
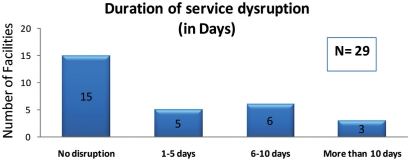
Dysfunction vs. service interruption
Fifteen of the 29 (51.7%) healthcare facilities stated that services offered were not interrupted but they experienced dysfunction. Of these 22.7% attributed the dysfunction to the buildings being damaged by flood waters and 77.3% attributed it, to equipment damage. Referrals both secondary and tertiary were absent in all the facilities during the flood period due to the damaged roads (Fig. 4).
Fig. 4.
Duration of service disruption.
Functioning of support systems
Eight facilities (27.5%) reported break down of electricity supply after the flood and 93% of these facilities did not have back up supply for total period of breakdown. The breakdown lasted between 8 and 15 days in three of the facilities that reported it. All the surveyed facilities stated that the sewage system was damaged or affected but the damage did not cause any public health problems. Similarly all 29 facilities reported that the garbage/solid waste management system was dysfunctional during the flood period although it did not cause any public health problems. Hospital waste disposal, e.g. sharps, syringes, bio waste etc was a challenge for 16 (55.2%) of the facilities during the flood.
Communication systems both internal and external form the backbone of disaster management systems. About 20 (69%) of the 29 facilities replied that there was no interruption of the communication systems within the facility. Over 19 (65.5%) of the responding facilities said that the road access was disrupted during the flood.
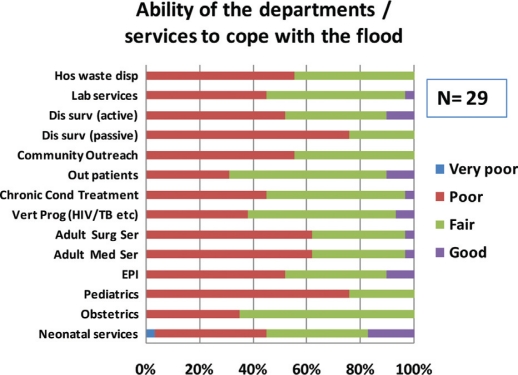
Ability of the health care system to cope
Only 11 (37.9%) facilities reported that they are able to fairly handle the flood. The majority rated their performance as poor. Pediatric services were the most poorly equipped to handle the flood with 22 (76%) of the facilities rating the current status as poor. The adult medical and surgical services were rated as poorly equipped by 18 (62.1%) of the respondents. Treatment of chronic conditions like hypertension, diabetes, and stroke, were rated as poor by 13 (44.8%) of the respondents (Fig. 5).
Fig. 5.
Ratings of health care service performance.
Vertical programmes like HIV, TB, and immunization programs fared better and 16 (55.2%) of the facilities coped fairly in running them. Obstetrics services were in the best position with 19 (64.5%) facilities stating the performance as fair. Out patient's services also appeared relatively better off to cope with the flood with 17 (58.6%) rating it fair.
About 24 (83%) of the facilities said that they did not procure any assistance or coordinate efforts with external agencies like the national armed forces, local or international NGOs, UN agencies etc. Representatives of all 29 facilities thought that there was sufficient supervision of the staff within the facility for adequate performance during the flood.
Human resources availability
The mean number of daily in-patients and out-patients treated in a facility was 1.90 and 67.07 respectively during the flood period. There is a dearth of all types of health care personnel particularly lab technicians and nurses even during non flood periods. There was no change in the mean number of health staff available and stood at Nurses (0.64, 0.66); Physicians (1.38, 1.59); Lab Technicians (0.25, 0.25); Public Health Workers (8.24, 8.38); and Pharmacists (1.07, 1.0) before and during the flood respectively. 96.6% of the 29 facilities stated that they experienced staff shortage during the time of flood.
Although a majority of the facilities had a license bed capacity of at least one bed for adult medical and surgical treatment under the certificate of need, there was no operational adult medical, surgical or paediatric bed in any of the facilities visited. The facilities only offered day care and basic obstetrics and gynaecological services. None of the facilities were able to scale up the number of available patient beds as required. Further, over 36% of the employees were absent from work for more than a week either due to their family being affected (65.5%) or damaged roads (34.5%) during the time of the flood.
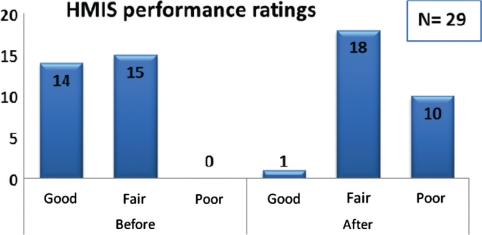
Surveillance and Health Information Management Systems (HIMS)
The Health Information Management System (HIMS) involves data collection on routine basis from the Primary Health Centres and Community Health Centres for five vertical disease control projects along with the Monthly Information System (MIS). The performance of maintaining these functions before the disaster was rated as good (48.3%) and fair (51.7%) respectively. The same was rated poor by 75.9% facilities during and after the flood. None of them were able to follow the expected data reporting standards during the flood period and none of them received any feedback from the district headquarters or the state surveillance cell regarding reporting quality or status.
All facilities are a mandatory part of the Integrated Disease Surveillance System and follow standard reporting formats. Syndromic surveillance is carried out at the sub-centres, presumptive at PHCs and CHCs and lab confirmed (at facilities where labs are available) under the program for early detection of outbreaks. About 62.1% of the facilities rated their syndromic surveillance activities after the flood as fair and 34. 5% rated it as poor. Community outreach programs were at a literal halt and 55.2% facilities rated their performance as poor. Laboratory services are essential component of disease surveillance for case and outbreak confirmation. These services were rated as poor by 44.8% of the facilities (Fig. 6).
Fig. 6.
Performance of the Health Management Information System.
Essential supplies and emergency stock piles
An overwhelming majority of facilities (21; 72.4%) reported that they maintain emergency supply stockpiles of essential medicines. An equal number reported that they experienced stock outs during the flood days. About 76% of the respondents, who said that their health facility experienced stock outs, attributed the main reason to a sudden increase in the number of patients seeking care.
Financial and legal structures
All the health facilities reported that functioning was hindered due to lack of emergency financial resources and due to interruption of the routine cash flows. Officials of these facilities are legally authorized to obtain and/or seek additional state/national/ international funding only through the state government which involves time consuming bureaucratic procedures. It also emerged that none of the 29 surveyed health facilities waived the fees for the patients during the flood period.
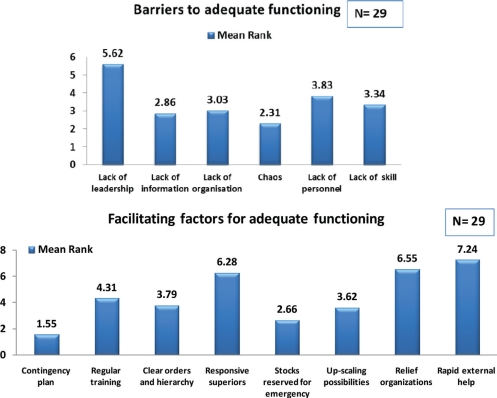
Governing the response – barriers and facilitators for mounting an adequate response
The respondents were asked about the factors that determine their ability to adequately respond to the flood. Preparing a contingency plan for such a situation emerged as the most critical factor followed by stocks reserved for emergency response. This was followed (in order of importance) by other factors such as provisions for up scaling in the event of flood, clear orders from immediate supervisors, more responsive superiors, presence of relief organizations and access to rapid external help (Fig. 7).
Fig. 7.
Barriers and facilitating factors identified for optimal performance during floods.
The main factor that negatively influenced the ability of the facilities to respond adequately was the situation of chaos that existed during the flood period. Nobody knew exactly what to do. All facilities functioned as independent standalone structures. Lack of clear information emerged as the second important factor negatively influencing the performance of the facilities followed by lack of organization. Other factors included (in order of importance) lack of skills within the team, lack of personnel and lack of leadership. The mean numbers of the responding facilities identifying barriers and facilitating factors are shown in Fig. 7.
Furthermore, 28 (96.5%) of the facilities reported that they did not have any emergency preparedness plan in place and that they do not have any early warning mechanisms for a flood. When asked about the existence of specific job descriptions within the organization for handling floods, an overwhelming 26 (89.7%) of the facilities replied in the affirmative but none were able to produce a physical copy of a manual describing standard operating procedures. When asked about the designated person responsible for coordinating public health emergency responses at the local level of government, all the facilities were aware that it was the Chief District Medical Officer (CDMO).
About 26 (89.7%) of the facilities stated that they were not enabled with adequate legal authority to develop and / or implement public health emergency training exercises. None of them have powers to evacuate a given area, redirect the distribution of health care supplies, or to collaborate with other health care providers in the community and assign them additional responsibilities for a coordinated response. Institutional learning from the flood experience was poor and it emerged that there were no changes or modification in the existing policies following the flood experiences.
Discussion and recommendations
Data from our primary survey clearly shows that the healthcare facilities are ill prepared to handle the flood situation despite being faced by them regularly. Basic utilities like electricity backup and essential medical supplies are lacking during floods. Missing standard operating procedures; human resources; pre-identified communication systems; incident command systems; and weak financial structures are the main hindering factors in mounting an adequate response to the floods.
Service delivery
In our study most facilities routinely over operate to their capacity and are forced to implement daily surge due to the lack of resources. Anticipation and preparedness are keys to planning a response. It is therefore necessary to understand the patient flow during the disaster to align the health care service delivery accordingly (9). However, inadequate documentation during the 2008 flood made this difficult for us to review, like in several other studies (25 26). Although the health conditions remained similar in our study the frequencies changed before, during and after the flood. Skin disease was the main health condition treated before the floods. This is probably because scabies is a major public health problem and accounts for the top five disease burden in rural Orissa (27). Snake bites were the most common injury after the floods. The essential drug list for the district should be updated and anti-venom for snake bites should be indented in it and should be procured locally to prevent the delays in transport from the district during floods. Chikungunya emerged as a new disease in the Jagatsinghpur district following the 2008 flood. Orissa has reported emergence of Chikungunya since 2006 particularly in the neighboring districts of Kendrapara and Cuttuck (28). Appropriate diagnostic tests (serum test for anti-CHIK antibody (immunoglobulin M)) and treatments along with vector control activities should be reinstated to prevent disease transmission during the annual flooding. Chikungunya has now been included in the Integrated Disease Surveillance System (IDSP) for routine surveillance which is an important step in its control ()29. However, in the absence of outreach programs during floods early detection of a developing outbreak may still be difficult.
Despite most respondents conforming that the everyday system might have been extended in the post flood situation, they did not assume a qualitative difference in the health care services provided during the flood. In most facilities it was perceived as altered care – in previously inadequate care – like in other developing countries (30). Existing guidelines for altered standards of care in mass casualty events such as the SPHERE standards should be circulated to the facilities and be referred to during floods as a first step to investigate the changes in care provision. The SPHERE standards allow accountability of care provided to victims in disasters and maintains minimum acceptable quality of care and serve as an important reference when formulating preparedness and response plans (31).
Structural damage to the building and damaged supplies were reported as the main causes for dysfunction in our study. The PAHO guidelines for protecting new health facilities from natural disasters should be referred to and implemented in the state to prevent structural damages to new facilities in the future (32). Additionally essential supplies and important hospital equipments should be stored in places not prone to flooding (33).
Health services provision is heavily dependent on preparedness of other supporting sectors such as transport, communication, electricity supplies and water and sanitation systems (34). All of the facilities reported dysfunction of one or the other type of supporting system in our study. None of these were reported to lead to any public health impacts. However, these dysfunctions should be nonetheless prevented. It is necessary that alternate sources for water, electricity, waste disposal transport, and road communications are identified in the planning process for the next events (25).
Health workforce
Human resources are a challenge during all disasters and more pronounced in rural settings (35). The facilities we surveyed are clearly under-staffed to handle burden of outpatient visitors (with an average of 60 patients per doctor per day) even in the non-flood periods. This situation is worsened during floods with additional influx of those affected. Further, none of the facilities were able to procure additional staff to deal with the situation. Given that over 80–90% of health care demands in the first 24 hrs following floods are treatable on ambulatory basis, augmenting regular staff with trained volunteers from the community is an option(7 30 36 37).In Orissa, for example the Auxiliary Nurse Midwife (ANM), Multi-purpose Health Workers (MPWs) and ASHA (Accredited Social Health Activists) are community health workforces that are trained in basic public health care provision. If trained further in mass casualty management they can be deployed usefully during floods.
Reduced access to health care facilities due to loss of vehicles, damaged roads or absent public transportation are common reasons for staff absenteeism following several disasters (10). A large number of the employees were absent from the health centres for more than a week in our study. Provisions to house available staff and their families close to the facility while the flood lasts should be planned through agreements with guest houses or community homes in the area (14).
Training of staff in management of mass casualty incidents holds the key to effective and optimum use of available resources. Lack of trained staff in the backdrop of ill-equipped health care facilities, poses a special challenge during floods (38). Practical drills, evidence based theory sessions, policy analysis activities, and most essentially regular updating of knowledge should be done through trainings (39). Experience after each flood should be used to update individual facility as well as district and state level preparedness policies. Additionally, a mere update will not suffice. They need to be heavily monitored and regularly evaluated for implementation, alignment to advances in technologies and performance of identified indicators. A majority of the facilities stated that they are not enabled with adequate legal authority to develop and / or implement public health emergency training exercises. This mandates serious reconsideration.
Information management
Hampered external or internal communications can potentially threaten disaster response (19). Majority of the facilities did not report any internal communication system interruption in our study. Although encouraging, steps to maintain these conditions and to improve road access to facilities should be made.
The syndromic surveillance system and the laboratory reporting systems were weak and limited data was available during the flood in our study. Health management information system procedures went from being good to poor and did not return to baseline for a considerable time after the flood (2 months). The facilities focused on maintaining vertical programmes and community outreach services were neglected. This was probably because the reporting schedules for national vertical programs are stringent; performance indicators are regularly monitored and result in strict disciplinary action in case of unsatisfactory performance. Outreach programs should be maintained during floods as they aid in reducing the morbidity and mortality from flood related diseases, help reduce the influx of patients to the facility, and are essential in developing early warnings signals for outbreaks (12 34). Stronger regulatory actions are mandated for local outreach programs like the vertical programs to ensure appropriate functioning during floods.
Medical products and supplies
Facilities reported stock-outs for 6–10 days in our study mainly due to sudden increase in the number of patients and disrupted supplies due to damaged roads. This is attributable to the central procurement policy where orders for the drugs are placed and payments are made at the state level, but supplies are delivered at the district level. Each institution has an pre-agreed entitlement of drugs and is given a passbook (27). Alternate mechanisms for local procurement should be made. Pre-disaster preferred ‘vendor agreements’ at block levels would be an effective way to deal with stock outs and delays in procurement from the district headquarters (11 14 16). Setting up accounts with advance security deposit payments as assurance should be considered (40). Local pharmacists associations can also be involved in setting up these arrangements. Additionally, kits with basic medical supplies should be developed and maintained at facility level for initiating a quick response given that the earliest that outside assistance arrives to the affected community is pegged at 24–96 hrs (7). It is advisable that the health facilities should be self sufficient at least for 3 days (ideally for a week) and should protect all supplies from damage until supply resumption (14 25).
Financing
Optimal functioning of the financial structures during a flood is necessary to surge capacity and to mount resources. All facilities reported hindrance in functioning due to lack of adequate finances and did not have access to additional resources to deal with the emergency. Existing resources were clearly inadequate. Additionally, given the limited resources, the flood non-exposed community experienced neglect as the focus of intervention, and rightly so, was on the flood exposed communities. User fees were not waived during the flood even for the poor, which should be reconsidered. Funding requirements for flood response should be calculated on past experiences and each facility should be granted contingency funds in their annual budget for use during an emergency (14).
Leadership and governance: developing preparedness plans and preparing to react
During the survey lack of leadership that affected the decision making process during the flood emerged as the single significant challenge. In the absence of clear line of command during disasters even the best resources will fail to deliver (35). Considerable communication gap existed between the employees. Absence of proper feedback of the ground realities to the authorities for a considerable period of time after the flood was also observed. There was lack of clear communication from the state level to district level and from district to the block and health centre level. All three levels were functioning in an isolated manner. The medical officers are on a rotation duty of 2 years and lack the required expertise and administrative powers to take decisions in flood situation. They often waited for permissions and instructions from the higher authorities leading to further uncertainty. Inter-institutional coordination and cooperation is indispensible in mounting a response to floods and consensus should be built in this regard (16).
A majority of the respondents considered contingency plan would help them in confronting this situation. However, the current plans are just a list of inventory rather than a plan to meet the issues identified. They even do not include a list of emergency phone numbers for reference during the floods which ideally should be clearly displayed in facilities (25). Few facilities surveyed had undertaken realistic evaluation of their strengths and weaknesses for dealing with severe floods despite facing them regularly. Preparedness plans are unique to a facility and detailed exercise to identify individual needs should be undertaken immediately. It is also necessary that all stakeholders are involved in developing and updating these plans regularly (16 17).
Limitations of the study
The study was conducted in one of the 30 districts of the state and included only public health care facilities. Although all primary health care centres in the district were included in the study the limited sample size has local relevance and limits the generalizability of the study to the state. Limited documentation during the time of the flood did not allow detail assessment of morbidity and mortality data. The grading of performance as good, poor and fair was left to the interpretation of the respondents and was therefore subjective. The systems preparedness for mental health care service provision could not be assessed as these services are not provided at the primary health care level. The study included a single flood incident (September 2008). Given that the district experiences annual flooding, accumulated impacts need to be reviewed alongside risk perceptions of the health care services staff.
Conclusions
The 2008 flood challenged several aspects of the primary curative and preventive health care services in Jagatsinghpur, Orissa. The results of this study indicate that although the facilities stretched their capacities and pulled through, it may not be pragmatic to continue doing so every year. Simple steps like developing facility specific preparedness plans which detail out standard operating procedures during disasters and identify clear lines of command will go a long way in strengthening the response to future floods. De-centralized decision making infrastructures should be reinstated at the periphery. This will eliminate the current time spent for acquiring required clearances from the higher level which delays responses significantly.
Performance critiques provided by the grass roots workers like this one should be used for institutional learning and effective preparedness planning. Most essentially it is necessary to recognize that having written disaster plans does not equate to preparedness! Trainings should be held regularly at all levels. Additionally each facility should maintain contingency funds for emergency response along with local vendor agreements to ensure stock supplies during floods. The facilities should also ensure that baseline standards for public health care delivery identified by the Government are met in non-flood periods in order to improve response during floods.
Building strong public primary health care systems is a development challenge. The recovery phases of disasters should be seen as an opportunity to expand and improve services and facilities.
Conflict of interest and funding
The authors declare no conflict of interest. The study was supported by the MICRODIS project (GOCT-CT-2007-036877) and funded by the European Commission under the 6th Framework Programme.
References
- 1.Guha-Sapir D, Vos F, Below R, Ponserre S. Annual Disaster Statistical Review : the numbers and trends. Brussels: Centre for Research on the Epidemiology of Disasters (CRED), Université catholique de Louvain; 2010. p. 2010. [Google Scholar]
- 2.Hajat S, Ebi KL, Kovats RS, Menne B, Edwards S, Haines A. The human health consequences of flooding in Europe: a review. In: Kirch W, Bertollini R, Menne B, editors. Extreme weather events and public health responses. Berlin, Heidelberg: Springer; 2005. pp. 185–96. [Google Scholar]
- 3.Ebi KL, Schmier JK. A stitch in time: improving public health early warning systems for extreme weather events. Epidemiol Rev. 2005;27:115–21. doi: 10.1093/epirev/mxi006. [DOI] [PubMed] [Google Scholar]
- 4.Louis V, Phalkey R, le Polain de Waroux O, Wind T, Komproe I, Luotomo M. The health and health care system impacts of earthquakes, windstorms and floods – a systematic review. In: Thwg-P MICRODIS, editor. MICRODIS paper series. Brussels, : Center for Research on the Epidemiology of Disasters; 2008. pp. 1–62. [Google Scholar]
- 5.Phalkey R, Reinhardt JD, Marx M. Injury epidemiology after the 2001 Gujarat earthquake in India: a retrospective analysis of injuries treated at a rural hospital in the Kutch district immediately after the disaster. Glob Health Action. 2011;4:7196. doi: 10.3402/gha.v4i0.7196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karras N, Hemenway C. Hurricane Katrina's impact on pediatric and adult patients with sickle cell disease. J Health Care Poor Underserved. 2007;18:382–93. doi: 10.1353/hpu.2007.0036. [DOI] [PubMed] [Google Scholar]
- 7.Stratton SJ, Tyler RD. Characteristics of medical surge capacity demand for sudden-impact disasters. Acad Emerg Med. 2006;13:1193–7. doi: 10.1197/j.aem.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Barbera JA, Yeatts DJ, Macintyre AG. Challenge of hospital emergency preparedness: analysis and recommendations. Disaster Med Public Health Prep. 2009;3(Suppl. 2):S74–82. doi: 10.1097/DMP.0b013e31819f754c. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy ML, Aronsky D, Kelen GD. The measurement of daily surge and its relevance to disaster preparedness. Acad Emerg Med. 2006;13:1138–41. doi: 10.1197/j.aem.2006.06.046. [DOI] [PubMed] [Google Scholar]
- 10.Axelrod C, Killam P, Gaston M, Stinson N. Primary health care and the Midwest flood disaster. Public Health Rep. 1994;109:601–5. [PMC free article] [PubMed] [Google Scholar]
- 11.Baker MS. Creating order from chaos: part II: tactical planning for mass casualty and disaster response at definitive care facilities. Mil Med. 2007;172:237–43. doi: 10.7205/milmed.172.3.237. [DOI] [PubMed] [Google Scholar]
- 12.Estacio PL. Surge capacity for health care systems: early detection, methodologies, and process. Acad Emerg Med. 2006;13:1135–7. doi: 10.1197/j.aem.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Howard E, Wiseman K. Emergency and disaster planning: patient education and preparation. Nephrol Nurs J. 2001;28:527–8. [PubMed] [Google Scholar]
- 14.Hanfling D. Equipment, supplies, and pharmaceuticals: how much might it cost to achieve basic surge capacity? Acad Emerg Med. 2006;13:1232–7. doi: 10.1197/j.aem.2006.03.567. [DOI] [PubMed] [Google Scholar]
- 15.Kaji AH, Koenig KL, Bey T. Surge capacity for health care systems: a conceptual framework. Acad Emerg Med. 2006;13:1157–9. doi: 10.1197/j.aem.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 16.Kaji AH, Lewis RJ. Hospital disaster preparedness in Los Angeles county. Acad Emerg Med. 2006;13:1198–203. doi: 10.1197/j.aem.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Strauss R, Muchl R, Kunze M, Hrabcik H. The role of public health officers in preparedness planning and management of health crises; Euro Surveill; 2008. pp. 1–3. [DOI] [PubMed] [Google Scholar]
- 18.Savoia E, Massin-Short S, Rodday A, Aaron L, Higdon M, Stoto M. Public health systems research in emergency preparedness: review of the literature; Am J Prev Med; 2009. pp. 150–156. [DOI] [PubMed] [Google Scholar]
- 19.Nates JL. Combined external and internal hospital disaster: impact and response in a Houston trauma center intensive care unit. Crit Care Med. 2004;32:686–90. doi: 10.1097/01.ccm.0000114995.14120.6d. [DOI] [PubMed] [Google Scholar]
- 20.WHO Everybody business: strengthening health systems to improve health outcomes. WHO's framework for action; Geneva, : World Health Organization; 2007. Available from: http://www.who.int/healthsystems/strategy/en/ [cited 3 September 2011] [Google Scholar]
- 21.OSDMA. Floods Authority TOSDM; Bhubaneshwar, : Government of Odisha; 2008. Avaliable from. http://www.osdma.org/ViewDetails.aspx?vchglinkid=GL047&vchplinkid=PL060. cited 2 February 2012. [Google Scholar]
- 22.GOI . Services DGoH. New Delhi, : Ministry of Health & Family Welfare, Government of India; 2010. Indian Public Health Standards (IPHS) for Community Health care Centres (CHC): revised guidelines 2010; pp. 2–4.pp. 2–4. [Google Scholar]
- 23.GOI . Indian Public Health Standards (IPHS) for Primary Health care Centres (PHC): revised guidelines 2010. In: Services DGoH, editor. New Delhi, : Ministry of Health & Family Welfare, Government of India; 2010. pp. 1–7. [Google Scholar]
- 24.GOI . Indian Public Health Standards (IPHS) for Sub-Centres: revised guidelines 2010. In: Services DGoH, editor. New Delhi, : Ministry of Health & Family Welfare, Government of India; 2010. pp. 3–5. [Google Scholar]
- 25.Counts CS. Disaster preparedness: is your unit ready? Nephrol Nurs J. 2001;28:491–9. [PubMed] [Google Scholar]
- 26.Hsu EB, Thomas TL, Bass EB, Whyne D, Kelen GD, Green GB. Healthcare worker competencies for disaster training. BMC Med Educ. 2006;6:19. doi: 10.1186/1472-6920-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta M. State health systems: Orissa. Working Paper No. 89; New Delhi, : Indian council for Research on International Economic Relations; 2002. p. 8. 13. Available from: http://www.icrier.org/pdf/WP__89.pdf [cited 18 July 2011]. [Google Scholar]
- 28.Dwibedi B, Mohapatra N, Beuria MK, Kerketta AS, Sabat J, Kar SK, et al. Emergence of chikungunya virus infection in Orissa, India. Vector Borne Zoonotic Dis. 2010;10:347–54. doi: 10.1089/vbz.2008.0190. [DOI] [PubMed] [Google Scholar]
- 29.Orissa M. Programs and schemes: integrated disease surveillance project. Vol. 2011; Bhubaneshwar, : Department of Health and Family Welfare, Government of Orissa; 2010. Available from: http://www.orissa.gov.in/health_portal/programme/IDSP/main.html [cited 18 July 2011] [Google Scholar]
- 30.Phillips S. Current status of surge research. Acad Emerg Med. 2006;13:1103–8. doi: 10.1197/j.aem.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 31.SPHERE Sphere handbook: Humanitarian charter and minimum standards in humanitarian response. Rugby, UK: The Sphere Project; 2011. Available from: http://www.sphereproject.org/content/view/720/200/lang,english/ [cited 01 February 2012]. [Google Scholar]
- 32.PAHO . Washington, DC: Pan American Health Organization and The World Bank Group; 2003. Protecting new health facilities from natural disasters: guidelines for the promotion of disaster mitigation. [PubMed] [Google Scholar]
- 33.Meusel D, Kirch M. Lessons to be learnt from the 2002 floods in Dresden, Germany. In: Kirch M, Menne B, Bertollini R, editors. Extreme weather events and public health responses. Berlin, Heidelberg, New York: Springer; 2005. pp. 175–83. [Google Scholar]
- 34.Few R. Floods, health and climate change: responses to the health risks from flooding; 2004. In. Health and climate change: A strategic review. Working Paper 63. Tyndall Centre for Climate Change Research. Available from: www.tyndall.ac.uk/publications/working_papers/wp63.pdf [cited 27 September 2011]. [Google Scholar]
- 35.Neil R. A call for help. Collaboration with community officials is key. Mater Manag Health Care. 2003;12:22–6. [PubMed] [Google Scholar]
- 36.Nuffer K, Wilson- Ramirez G. A comparison of patient needs following two hurricanes. Prehosp Disaster Med. 2004;19:146–9. doi: 10.1017/s1049023x00001655. [DOI] [PubMed] [Google Scholar]
- 37.Mahoney LE, Reutershan TP. Catastrophic disasters and the design of disaster medical care systems. Ann Emerg Med. 1987;16:1085–91. doi: 10.1016/s0196-0644(87)80764-3. [DOI] [PubMed] [Google Scholar]
- 38.Gausche-Hill M. Pediatric disaster preparedness: are we really prepared? J Trauma. 2009;67(Suppl. 2):S73–6. doi: 10.1097/TA.0b013e3181af2fff. [DOI] [PubMed] [Google Scholar]
- 39.Kaji AH, Lewis RJ. Assessment of the reliability of the Johns Hopkins/Agency for Healthcare Research and Quality hospital disaster drill evaluation tool. Ann Emerg Med. 2008;52:204–10–e201–8. doi: 10.1016/j.annemergmed.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 40.McFarland HF. Surviving a 500-year flood. Nephrol Nurs J. 2001;28:504–6–509–10. [PubMed] [Google Scholar]