Skin cancers commonly occur on the cheek and nose and, depending on several factors, multiple approaches to excision and surgical reconstruction are available. Although skin grafts, among other techniques, are perceived to be simpler methods of reconstruction, the authors describe the bilobed flap as an effective solution to skin defects in this region and highlight some key features of the procedure.
Keywords: Bilobed flap, Lateral cheek reconstruction, Local skin flaps
Abstract
The cheek and nose are common areas for skin cancers. There are multiple approaches to surgical excision and reconstruction, depending on the size of defect, tissue quality, adjacent cosmetic units and hairline. An effective solution to skin defects of the lateral cheek is the bilobed flap. This flap tends to be underused in the lateral cheek area because primary closure and skin grafts are perceived to be easier methods of reconstruction. However, the use of the bilobed flap for lateral cheek and other defect closures is encouraged. There are several basic principles that are key when performing this flap. These components of the procedure are highlighted.
Abstract
La joue et le nez sont des zones courantes de cancer de la peau. Il existe de multiples modes d’excision et de reconstruction chirurgicales, selon la dimension de l’anomalie, la qualité des unités esthétiques adjacentes et la ligne des cheveux. Le lambeau bilobé constitue une solution efficace aux anomalies cutanées de la joue latérale. Ce lambeau tend à être sous-utilisé dans cette zone, parce que la fermeture primaire et les greffes cutanées sont perçues comme des modes de reconstruction plus simples. Cependant, les auteurs encouragent l’utilisation du lambeau bilobé pour refermer les anomalies de la joue latérale et d’autres anomalies. Il faut respecter plusieurs principes de base lorsqu’on utilise ce lambeau. Les éléments de l’intervention sont soulignés.
Head and neck skin cancer excision and reconstruction provide endless challenges and opportunities for the reconstructive surgeon. There are many, well-documented methods of excision and reconstruction. These methods are based on the principles of the reconstructive ladder and on geometric principles. Factors such as tissue quality, size of defect and relevant anatomical structures, as well as cosmetic subunits, must all be considered.
The bilobed flap was first described by Esser in 1918 (1) for use in nasal tip defect reconstruction. Others, such as Zimany (2) and McGregor and Soutar (3), expanded on its principles and described how it could be applied to many areas of reconstruction (4). This method of reconstruction is very useful for several reasons; for example, it covers the primary defect by ‘spreading the load’ of tissue loss over two adjacent skin flaps, and enables the preservation of skin creases and skin folds when used in areas around the nose and ear.
The original bilobed flap technique consisted of reparing a tissue defect using two adjacent skin flaps at 90° to one another. The surgical technique that we use for reconstruction involves using the Zitelli modification of the traditional bilobed skin flap (5). The Zitelli technique uses flaps that are rotated by 45° to 55°, with a total rotation of 90° to 110°, compared with the 180° of the original design (6).
We describe the usefulness of the Zitelli bilobed flap for lateral cheek reconstruction, and highlight some key features, which are illustrated in the case example. This use of this flap has been well documented in the repair of nasal defects, and should also be considered for reconstruction of lateral cheek defects and other areas, where appropriate.
TECHNIQUE
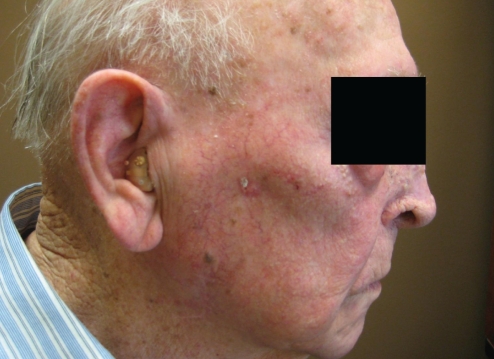
The lesion is identified (Figure 1) and marked with appropriate margins from the clinically visible tumour border (Figure 2). Loupe magnification may be used to help delineate the lesion border. The skin should be assessed for laxity, tethering and mobility. In this case, areas of laxity were assessed. Due to the nature of the skin and previous treatments, the best area of recruitment was on the lower cheek and inferior preauricular region. Proximal to the lesion (superior), the skin was taut and unsuitable for easy closure. A ‘pinch test’ also provides an estimate of the thickness of the skin and subcutaneous tissues.
Figure 1).
Lesion of the right cheek inferior to zygomatic arch
Figure 2).
The lesion is outlined
The two lobes of the skin flap are then planned and outlined adjacent to the lesion. The lobe distal to the wound is smaller in size than the proximal lobe. The bilobed flap is outlined with a surgical marker (Figure 3).
Figure 3).
The bilobed skin flap is outlined
The first or proximal lobe, used for reconstructing the defect, usually lies with its midmark at 45° or less to that of the defect. The distal or second lobe used to repair the defect resulting from the first lobe is taken from the loose skin donor site. This lobe is transposed 45° to the defect from the first lobe.
The bilobed flap has a random-based vascular supply. Thus, flaps should be planned based on traditional length-to-width ratios, which are based on the site of the body where the flap is being used. Generally, a 2:1 to 4:1 length-to-width ratio is used.
During reconstruction and flap planning, the surgeon should also make an effort to maintain the cosmetic units of the face. The defect and the skin flaps should all involve the same aesthetic subunit of the face, when possible. In the example shown, we restrict the two flaps to the lateral cheek area. This is the location of the original skin defect, and makes use of the skin laxity at the inferior preauricular area of this particular patient.
Local anesthesia is used with epinephrine for hemostasis, creating a tumesencent bed over the entire surgical area including the defect, flaps both flaps and surrounding tissues that will need to be undermined to facilitate skin movement and closure. The local anesthetic will have time to take effect while the patient and the the surgical field are prepared.
The lesion is then excised and sent for pathology to verify clear margins (Figure 4). Hemostasis is obtained with bipolar cautery forceps.
Figure 4).
The lesion is removed
The first/proximal lobe is then incised (Figure 5) and elevated (Figure 6). This flap is then placed in the primary defect to confirm that the size of the flap approximates that of the wound, and to assess vectors of tension. It is imperative that the second/distal lobe not be incised and elevated until complete elevation of the first lobe, for two reasons. First, this enables the surgeon to properly assess the size and vectors of the first lobe before committing to the size and vectors of the second. Second, the surgeon is also able to assess the skin rotation and elasticity. This information enables the surgeon to make adjustments to the second lobe of the skin flap as needed. The skin laxity and tension at the flap pivot point can also be better determined after elevating the first flap. At this point, adjustments and other options are still feasible. Incising the outline of the second lobe of the flap before elevating the first lobe may cause the surgeon to commit to a skin flap that may not be of appropriate size.
Figure 5).
The first lobe is incised
Figure 6).
The first lobe is elevated
The second key step in this procedure is undermining the primary defect to avoid pin cushioning. Pin cushioning is caused by either an excessively large flap, or scar contraction, which leads to constricting forces developing along the inner aspect of a curved scar (4). With time, the tissue or flap within the curve bunches together and protrudes, leading to the pin cushion phenomenon. Pin cushioning can be avoided by undermining the tissue of the primary defect and ensuring that the flap is not too large for the defect. This allows the defect to expand outwards, and the undermining provides room for the new flap skin to settle in the same plane as the primary defect.
At this point, the surgeon may make necessary adjustments to the second lobe of the skin flap, and then incise (Figure 7) and elevate the second lobe (Figure 8). As previously mentioned, the second skin lobe should be slightly smaller than the first. The mobility at the base of the flap should be assessed and any adjustments made by further undermining.
Figure 7).
The second lobe is incised
Figure 8).
The second lobe is elevated
After the second lobe is elevated, the surgeon can inset the two lobes (Figure 9). The defect left from the second lobe should be closed primarily. Sometimes a Burrow’s triangle or V-Y advancement flap may be used to close this defect if the edges will not come together without tension. Trimming the flaps and the dog ears or cone defect resulting from the rotation may be necessary (4). Suture selection usually consists of absorbable 4-0 inverted interrupted sutures in the deep dermis, while nonabsorbable 5-0 monofilament sutures are usually used to close the epidermis in simple fashion (Figure 10). The skin sutures are removed five to seven days postoperatively.
Figure 9).
The lobes are inset
Figure 10).
The lobes are inset and primary closure is performed at the second flap site
When performing a layered closure, it is important to handle the tissue edges with care and to and to ensure that the vessels supplying the flap are not compromised.
The bilobed flap technique is useful to physicians excising superficial skin cancers followed by anatomical reconstruction. Physician specialties to benefit from this technique commonly include plastic surgery, otolaryngology and surgical dermatology, but could include general surgery and other specialties.
CONCLUSION
We presented a case report demonstrating the application of the bilobed flap in the setting of cheek reconstruction. The case features a number of points that we believe to be, important for the reconstructive surgeon performing this procedure. These include avoiding the incision of the second lobe until the first lobe is entirely elevated, and undermining the lesion defect to avoid pin cushioning. We recommend using the modified bilobed flap as per Zitelli (5), in which the angle between the lobes is less than 90°. This creates less stress on the flap pivot point when the flaps are moved. A benefit of this flap for lateral cheek reconstruction is that skin is recruited from the inferior preauricular region, which is well matched for texture and colour of local skin. We suggest that the bilobed flap is a good choice for reconstruction areas involving lateral cheek and preauricular areas because it recruits lax skin and is versatile in its application.
REFERENCES
- 1.Esser FS. Gestielte Lokale Nasenplastik mit Zweizipfligem Lappen. Deckung des Sekundaren Defektes vom ersten Zipfel durch den Zweitzen. Dtsch Z Chir. 1918;143:385. [Google Scholar]
- 2.Zimany A. The bilobed flap. Plast Reconstr Surg. 1953;11:424–34. doi: 10.1097/00006534-195306000-00002. [DOI] [PubMed] [Google Scholar]
- 3.McGregor C, Soutar DS. A critical assessment of the bilobed flap. Br J Plast Surg. 1981;34:197–205. doi: 10.1016/s0007-1226(81)80094-x. [DOI] [PubMed] [Google Scholar]
- 4.Jackson IT. Local Flaps in Head and Neck Reconstruction. St Louis: Quality Medical Publishing Inc; 2002. Missouri. [Google Scholar]
- 5.Zitelli JA. The bilobed flap for nasal reconstruction. Arch Dermatol. 1989;125:957–9. [PubMed] [Google Scholar]
- 6.Salgarelli A, Cangiano A, Sartorelli F, Bellini P, Collini M. The bilobed flap in skin cancer of the face: Our experience on 285 cases. J Craniomaxillofac Surg. 2010;38:460–4. doi: 10.1016/j.jcms.2009.10.022. [DOI] [PubMed] [Google Scholar]