Abstract
Objective
One important factor in adolescents’ development of problem alcohol use is their family environment. Yet, the mechanisms that relate parenting to youth alcohol use are not well characterized. This study employed a naturalistic laboratory-based approach to observe parenting behaviors (support, structure, criticism) and adolescents’ physiological and emotional responses to parent-adolescent interactions to examine associations with adolescent alcohol use.
Method
Fifty eight 10–16 year olds and their parents completed a 10 minute Parent Adolescent Interaction Task (PAIT) in which they discussed a mutually highly-rated conflict topic. Parental support, structure, and critcism were coded from the interaction. Adolescents’ heart rate (HR), blood pressure (BP), reported emotions, and salivary cortisol were assessed before, during, and after the interaction.
Results
Findings indicated that lower parental structure and support were associated with youth’s greater diastolic BP and anger arousal in response to the PAIT. Furthermore, higher HR, systolic BP, and cortisol responses to the interaction were associated with youth’s alcohol use.
Conclusions
Findings suggest that heightened emotional and physiological responses to parent-adolescent conflict interactions in youth may be one pathway by which parenting is associated with youth’s alcohol use and risk for abuse.
Keywords: alcohol use, adolescence, emotion, HPA axis, parent-child interaction, parenting
1. Introduction
Adolescence is a period of risk for the development of alcohol and substance use disorders (Chambers et al., 2003). National survey data indicate that one month rates of alcohol use increase from 15.9% in 8th grade to 28.8% in 10th grade to 43.1% in 12th grade (NIDA, 2009). Binge drinking (>=5 drinks per occasion) and heavy drinking also increase sharply across middle adolescence (see Masten et al., 2008).
One important factor in adolescents’ development of problem alcohol use is their family environment. Several questionnaire studies have found that a family history of alcohol abuse and poor self-reported parenting are linked with youth alcohol use/problem use (e.g., Chassin, Flora, & King, 2004; Tildesley & Andrews, 2008). Specifically, lower levels of parental monitoring, structure/appropriate discipline, and warmth/support have been associated with increases in alcohol use and problem use over time in adolescence (Clark, Thatcher, & Maisto, 2005; Dodge et al., 2009; Johnson & Pandina, 1991; Tildesley & Andrews, 2008; van der Vorst et al., 2006; Barnes, Reifman, Farrell, & Dintcheff, 2000).
Despite the established link between parenting and adolescent alcohol use, the mechanisms by which poor parenting relate to youth’s alcohol use are not well characterized. We theorize that adolescents’ emotional and physiological arousal responses to family interactions may help explain links between negative parenting and youth alcohol use. We propose that negative, critical, and unsupportive parenting may lead adolescents to feel uncomfortable and emotionally and physiologically aroused in family interactions. In turn, this discomfort may create risk for behaviors that diminish that discomfort, such as use of alcohol. In addition, youth who feel overly aroused by family discussions may avoid these discussions, leading to less close family relations, decreased parental monitoring, and risk for alcohol use. There may also be reciprocal child effects, in which youth who use alcohol elicit more negative parenting, which then leads to greater negative arousal. The present study examines cross-sectional associations between parenting behaviors, youth arousal responses, and adolescent alcohol use to begin to characterize the parenting behaviors and youth arousal responses that are linked to adolescent alcohol use.
Studies in early and middle childhood find that children’s altered physiological responses (e.g., cortisol, heart rate variability) to family conflict interactions are linked to externalizing and internalizing behavior problems (e.g., Erath et al., 2009; Granger et al., 1996). These behavior problems and associated personality traits such as hopelessness, anxiety sensitivity, and impulsivity in childhood are predictive of alcohol use in adolescence, (Mayzer, Fitzgerald, & Zucker, 2009; Krank et al., 2011). However, although altered physiological responses to family interactions are found in young children with behavior problems, and behavior problems are associated with alcohol use, few studies have explicitly examined associations between physiological arousal responses to family conflict interactions and alcohol or substance use in adolescence. To our knowledge, the only study of observed parent-adolescent interactions and substance use found that substance-using adolescents showed greater aversive affect (such as aggressive and irritable affect) when discussing conflict and substance use topics with parents, suggesting that these youth are emotionally aroused by the interactions (Hops et al., 1990).
Here we report on a laboratory-based study examining observed parenting behaviors (support, structure, criticism) in parent-adolescent conflict interactions, adolescents’ emotional, cardiovascular (heart rate, blood pressure), and hypothalamic pituitary adrenal (HPA) axis response to these interactions and current alcohol use in adolescents. First, we predicted that the parent-adolescent conflict task would produce an increase in emotional, cardiovascular, and HPA axis arousal in the youth as a whole. Second, we hypothesized that lower support, lower structure, and greater negative parenting behaviors in the task would be associated with greater emotional, cardiovascular, and HPA axis arousal responses to the task in the adolescents. Third, we proposed that greater emotional, cardiovascular, and HPA axis arousal responses would be positively associated with adolescent alcohol use.
2. Material and Methods
2.1 Participants
Participants were 58 primarily Caucasian 10–16 year olds (31 boys, 27 girls) and their parents. Demographic information on the participants is shown in Table 1. Parents were mostly biological mothers (51, 87.9%), with 1 adoptive mother, 5 biological fathers, and 1 maternal grandmother. Families were recruited through newspaper ads, flyers, and mailings to families with adolescents in a metropolitan area in the Northeastern United States.
Table 1.
Demographic and alcohol use information
| Race: Number (%) in each group | |
| Caucasian | 41 (70.7%) |
| Hispanic | 5 (8.6%) |
| Asian | 2 (3.4%) |
| Native-American/Alaska Native | 3 (5.2%) |
| Biracial | 1 (1.7%) |
| Other race | 2 (3.4%) |
| Not reported | 4 (6.9%) |
| Family Income: Number (%) in each level | |
| < $15,000/year | 2 (3.4%) |
| $15,000–24,000/year | 2 (3.4%) |
| $25,000–34,000/year | 2 (3.4%) |
| $35,000–44,000/year | 1 (1.7%) |
| $45,000–59,000/year | 3 (5.2%) |
| $60,000–74,000/year | 11 (19.0%) |
| > $75,000/year | 28 (48.0%) |
| Don’t know | 2 (3.4%) |
| Not reported | 7 (12.0%) |
| Sex: Number (%) male | 31 (53.4%) |
| Child’s Age: Mean (SD) years | 13.02 (1.92) |
| Lifetime alcohol use: Number (%) used | 12 (20.7%) |
| Number of days used in lifetime: Number and % of users | |
| 1–2 days | 3 (25.0%) |
| 3–9 days | 3 (25.0%) |
| 10–19 days | 4 (33.3%) |
| 20–39 days | 1 (8.3%) |
| 40–99 days | 1 (8.3%) |
| Past 30 day alcohol use: Number (%) used | 5 (8.6%) |
Procedures
Adolescents attended three sessions, each spaced about one week apart. In the first session, youth completed questionnaires, computer tasks, and interviews assessing cognitive and emotional functioning, psychological symptoms, and alcohol and substance use. During the second session, adolescents completed alcohol breathalyzer screens and urine screens to confirm alcohol and substance use reports and then completed an EEG study of neural correlates of stress-induced reward behavior and decision-making. In the third session, the focus of this report, adolescents and primary caregivers completed the Parent-Adolescent Interaction Task (PAIT) as well as alcohol breathalyzer and urine drug screens. Informed parental consent and adolescent assent were obtained, and the study protocol was approved by the university’s Institutional Review Board.
2.2 PAIT Session
The Parent Adolescent Interaction Task (PAIT) sessions were scheduled in the late afternoon (4:00 p.m.). Adolescents were asked to have a snack 30 minutes to 1 hour prior to the start of the session and were not allowed to eat during the session. Youth were asked to refrain from alcohol or drug use prior to the session to control for acute drug effects on physiology and HPA axis functioning. Youth completed alcohol breathalyzer and urine drug screens on the day of the session and all were negative. Girls who were menstruating regularly (N = 10) were scheduled for the PAIT laboratory visit during days 5–10 of their cycle to minimize hormone effects.
Adolescents and parents arrived at the session ½ hour early (3:30 p.m.). Upon arriving, adolescents and parents went to two separate laboratory rooms and met with separate trained research assistants (referred to as “parent RA” and “child RA” throughout). Adolescents and parents were seated in comfortable chairs. They completed breath and urine tests and then completed the Issues Checklist (IC; Prinz et al. 1979), a checklist of common family conflict topics (e.g., cleaning bedroom). Participants endorsed topics discussed in the past month and the anger level they felt during the discussion (on a scale from 1–5). This checklist has been used in previous research on parent-adolescent conflict interactions (Sheeber et al., 1997).
At 4pm, there was a 25-minute adaptation/relaxation period. A blood pressure cuff was placed on each participant’s preferred arm and a pulse sensor on a finger. Participants listened to two 5-minute relaxation tapes which led them through progressive muscle relaxation and relaxing imagery. At 4:25 p.m., baseline (“pre-task”) heart rate (HR), blood pressure (BP), reported emotion, and salivary cortisol measurements were collected from the parent and adolescent. HR was measured every 10 seconds for 1 minute (and then averaged) to calculate a stable baseline.
At 4:30 p.m., the parent was brought into the adolescent’s room and seated next to him/her. The PAIT was performed, as described below. The PAIT procedure lasted 10 minutes. During the PAIT, the child RA recorded parent and adolescent HR every 30 seconds. After the PAIT, parents returned to their rooms. Measures of HR, BP, reported emotion, and salivary cortisol were taken immediately post-task and then every 15 minutes through a recovery period of 60 minutes.
2.2.1. PAIT procedure
The PAIT task was based on family conflict tasks used in previous research on adolescent emotion regulation and depression (e.g., Sheeber et al., 1997). For the task, the parent and adolescent had a 10-minute discussion about a conflict topic. The dyad was asked to discuss their mutual highest-rated conflict issue from the Issues Checklist. If the parent and adolescent chose different top-rated topics, the highest rated parent topic was used. The dyad was asked to “use the next 10 minutes to discuss the issue and to try to reach a solution that you think will work for you.” They were also instructed to talk about it as they would if they were at home. The PAIT was coded in person by the parent RA. The PAIT was also videotaped so that the parent RA could check their coding by reviewing the videotape and so that reliability could be calculated, with a second coder rating the interaction from videotape. If the family finished the discussion in less than 10 minutes, they were reminded of the directions and asked to keep talking for the full time.
2.3. Measures
2.3.1. Observed parenting behavior
Parenting behavior during the PAIT was coded using the PAIT Coding System (Chaplin, 2010). Parental warmth/support (e.g., nods head, appears to listen to the youth, provides hugs or other physical comfort, praises the youth), structuring/involvement (e.g., clearly states the problem, discusses solutions, sets limits/rules, explains rules), and criticism/negative parenting (e.g., makes disparaging comment/put-down of child, mocks child, interrupts child) were coded, based on theory and empirical findings in the parenting literature (e.g., Gottman, Katz, & Hooven, 1997). Coders viewed the 10-minute discussions and rated each parenting behavior on a scale from 1–5 (“none present” to “high level”), based on parents’ facial expressions, behaviors, tone of voice, and content of speech. Coders underwent 6 hours of training by the first author in the system and met for bi-monthly coding meetings to discuss coding questions. Nineteen of the videotapes (33%) were randomly chosen, double-coded and checked for inter-rater reliability. Reliability was acceptable, with average intra-class correlation coefficient (ICC) = .70 (ICC for support = .74, for structure = .63, and for negative/critical parenting = .73).
We also measured global self-reported parenting practices in order to assess correlations between observed parenting in the interaction task and self-reported parenting. Parents completed the Alabama Parenting Questionnaire (APQ; Shelton, Frick, & Wootton, 1996). The APQ is a widely used report of parenting that shows adequate internal consistency and good validity and discriminates between families with and without children with disruptive behavior problems (Shelton et al., 1996). We used three subscales of the APQ to assess correlations with similar observed parenting behaviors in the PAIT. The APQ subscales were: positive parenting (to correlate with observed support), poor monitoring/supervision (to correlate with observed structure), and corporal punishment (to correlate with observed critical/negative parenting).
2.3.2. Adolescent cardiovascular response
A Critikon Dinamap 120 Patient Monitor was used to assess systolic and diastolic BP. A pulse sensor on the index finger connected to the Dinamap Monitor provided a measure of HR. HR was measured at pre-task, every 30 seconds during the PAIT (in analyses, we use the peak of these “during task” measures), immediately after the PAIT, and 15 minutes post-task. BP was measured at pre-task, immediately after the PAIT, and 15 and 30 minutes post-task. HR and BP data were only examined through 15 or 30 minutes of follow-up because cardiovascular responses are brief.
2.3.3. Adolescent emotional response
Adolescents’ self-rated emotions were assessed with the Differential Emotions Scale-Revised short form (DES-R, Izard, 1972) plus Izard’s scale for anxiety ratings (Izard, 1972). Each emotion subscale is made up of 5 adjectives describing the emotion state. The DES-R shows good psychometric properties (Izard, 1972) and has been used with adolescents (Chaplin, 2006). Emotions were examined at pre-test, immediately after the PAIT, and 15 and 30 minutes post-task. Emotion was only examined through 30 minutes of recovery because emotional arousal responses are typically short-lived. For this report, we aimed to examine three emotions- anxiety, anger, and sadness. However, as is common in studies of emotional responses, over half of the participants reported no sadness. Due to this limited variability, we only examined anxiety and anger response.
2.3.4. Adolescent HPA axis response
Salivary cortisol levels were measured as a marker of HPA axis activation. Saliva was collected using a cotton swab which participants were instructed to place between their tongue and cheek for approximately 2 minutes until the swab was completely saturated. The saliva swab was collected in a plastic tube, which was placed directly on ice and stored at −20 Celsius. Saliva samples were assayed in duplicate following standard radioimmunoassay kits with no modifications (Coat-A-Count Cortisol Kit, Diagnostic Products Corporation, Los Angeles, CA) at a University laboratory. The intra-assay coefficients of variation for the kit range from 3.0 to 5.1%. Saliva samples were taken at pre-task, immediately after the PAIT, and at 15, 30, 45, and 60 minutes post-task.
2.3.5. Adolescent alcohol use
Lifetime alcohol use was assessed with a combination of self-report on the Youth Risk Behavior Survey (YRBS; Brener et al., 2002) and a breath screen for alcohol use at the second study session- a separate occasion from the PAIT session. Adolescents were considered positive for lifetime alcohol use if they endorsed lifetime use of alcohol on the questionnaire or if they had a positive breath screen at that session. As stated previously, no youth had positive breathalyzer results on the day of the PAIT laboratory session.
Several measures were taken to increase the honesty of adolescents’ reporting about alcohol use. First, at the start of the study, youth were told that their responses to questions about alcohol and drug use were confidential and would not be shared with their parent (except in cases of concerns about them harming themselves or others). Second, a Certificate of Confidentiality (COC) was obtained for the study and youth were told that the confidentiality of their reports of illegal behaviors (including substance use) was protected by the COC. Third, the YRBS was self-administered by computer to increase a sense of privacy.
2.3.6. Missing data
Data was missing at one or more time-point(s) for 2 youth for BP (due to equipment malfunction) and 2 for cortisol (due to insufficient saliva). These subjects are excluded from analyses involving those variables.
2.4. Data Analysis Plan
2.4.1. Main analyses
Repeated measures ANOVAs were conducted to examine change from pre- to post-PAIT in response variables in the group overall (Hypothesis 1), associations between parenting behaviors and PAIT response variables (Hypothesis 2), and to examine differences between alcohol use group (use/no use) on PAIT response variables (Hypothesis 3), using SPSS statistical software. To test hypothesis 1, the within-subjects factor of time (pre-task, post-task, and varying follow-up time-points) was used to predict the PAIT response variables (HR, BP, emotions, cortisol). To test hypothesis 2, the within-subjects factor of time (pre-task, post-task, and varying follow-up time-points) and the predictor variable of parenting behavior (support, structure, or negative parenting) were used to predict the PAIT response variables. To test hypothesis 3, the within-subjects factor of time (pre-task, post-task, and varying follow-up time-points) and the between-subjects factor of alcohol use history (use, no use) were used to predict the PAIT response variables. If there was significant sphericity present in the repeated measures ANOVAs, as indicated by a significant Mauchley’s W test, we used the F tests from the multivariate tests output. If not, we used the F test from the tests of within-subjects effects (as recommended by Field, 2005). If there were significant or trend-level (p < .10) interactions between the predictor variable (parenting behavior, alcohol use) and time, these were followed up using separate correlations (for parenting behavior) or t-tests (for alcohol use) at each time-point. For significant follow-up contrasts, Cohen’s d effect sizes were also calculated. For Cohen’s d effect sizes, .2 – .3 is considered a small, .4 a medium, and .8 or above a large effect.
2.4.2. Covariates
If there were associations between parenting behavior or alcohol use group and pre-task HR, BP, emotion, or cortisol scores, then pre-task scores were covaried in the repeated measures ANOVAs. We also considered age, gender, and family history of alcohol problems (as reported by the parent) as possible control variables by examining them as predictor variables in separate repeated measures ANOVAs predicting PAIT response variables. If they showed a significant prediction of change in the PAIT response variables, then we included them as covariates in the main analyses.
2.4.3. Mediation
If a response variable showed a significant association with parenting and with alcohol use, it was considered as a potential mediator of an association between parenting behaviors and alcohol use, using steps recommended by Baron and Kenny (1985) and Sobel (1982).
3. Results
3.1. Descriptive Information
Demographic and alcohol use information for the sample are presented in Table 1. As shown in the Table, 12 (21%) of youth reported or tested positive for lifetime alcohol use. This is consistent with national norms for alcohol use in early to middle adolescence (Johnston et al., 2010). Besides these 12 youth, an additional 4 adolescents reported or tested positive for other drug use in the initial study session, including tobacco use (2 youth) and inhalant use (2 youth).
The 12 youth who were positive for alcohol use were not different from the other 46 youth on gender, mother education level, pubertal timing (early vs. late onset, by self-report), or on externalizing and internalizing symptoms measured by the parent-reported Child Symptom Inventory (CSI; Sprafkin et al., 2002). Alcohol-using youth reported more advanced pubertal development on the Physical Development Scale (PDS; Petersen, Crockett, Richards, & Boxer, 1988) than non-using youth, F[55]= −5.02, p < .001.
3.2. Data Inspection and Transformations
Data were examined for normality. The emotion variables (anxiety, anger) were positively skewed and so square root transformations were used in analyses, although untransformed scores are used in figures for ease of interpretation. For HR, BP, and cortisol, there were a few outlier cases with data points greater than three SDs above the mean (two for HR, one for systolic BP, two for diastolic BP, and one for cortisol). These data points were reassigned a value equal to three standard deviations above the mean (similar procedures have been used in other studies of physiological stress response, e.g., Kertes & Gunnar, 2004; Susman et al., 2007).
3.3. Conflict Topic
The three most frequently chosen conflict topics to discuss were “fighting with brother or sister” (22.4%), “cleaning bedroom” (20.7%) and “getting low grades in school” (10.3%). The alcohol use groups were not different in their choice of topic, Chi2 (3, n = 58) = 4.36, ns. Adolescents’ mean rating of the chosen conflict topic was 3.09 (SD = 1.19) out of 5, with 1 being “calm” and 5 being “angry.” Parents’ mean rating was 3.67 (SD = 1.15). There were not significant differences in topic ratings for the alcohol use groups (for adolescent rating, t = −1.65, ns; for parent rating, t = 1.42, ns).
3.4. Possible Covariates
There were no significant associations between parenting behavior or alcohol use and the PAIT response measures (HR, BP, emotion, cortisol) at pre-task. There were also no significant age, gender, or family history of alcohol problems predictions of PAIT response measures and so we did not include these as covariates.
3.4. Associations between Observed Parenting in the PAIT and Self-Reported Overall Parenting
Observed parental support in the interaction task showed a small, non-significant correlation with reported positive parenting, r = .12, ns. Observed parental structuring in the PAIT showed a significant small-magnitude negative correlation with parent-reported poor monitoring/supervision, r = −.29, p < .05. Observed critical/negative parenting in the PAIT showed a significant medium correlation with corporal punishment, r = .40, p < .01. These correlations were in the expected directions, supporting the validity of the observed parenting measure. Further, the correlations were small to moderate, suggesting that the observed parenting measure is unique and not entirely overlapping with reported parenting.
3.5. Associations between Parenting Behaviors and Alcohol Use
There were not significant associations between adolescent alcohol use group (use/no use) and parenting behaviors (t’s < .25, ns).
3.6. Hypothesis 1: PAIT Increases Arousal Responses Overall
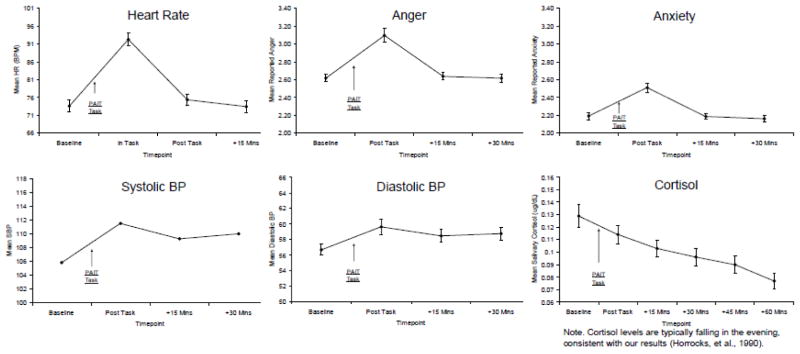
In the sample as a whole, the PAIT induced an arousal response. For HR, BP, and emotion (anxiety and anger), there were significant time main effects, with each measure increasing after the PAIT task and then decreasing across the follow-up recovery timepoints, for HR, F(3, 55) = 71.24, p < .001, for systolic BP, F(3, 165) = 10.54, p < .001, for diastolic BP, F(3, 165) = 6.60, p < .001, for anxiety, F(3, 55) = 16.40, p < .001, and for anger, F(3, 55) = 14.66, p < .001 (see Figure 1). For cortisol, there was also a significant time main effect, but rather than increasing, cortisol levels decreased and then slightly leveled out about 15 minutes after the task, F(5, 51) = 7.04, p < .001. Cortisol levels typically decrease in the evening (Horrocks et al., 1990), which is consistent with these results. Notably, for the alcohol using group, cortisol levels remained elevated (see section 3.8.3.).
Figure 1.
Response to the PAIT in the Full Sample
3.7. Hypothesis 2: Parenting Behaviors and PAIT Response
3.7.1. Heart rate and blood pressure
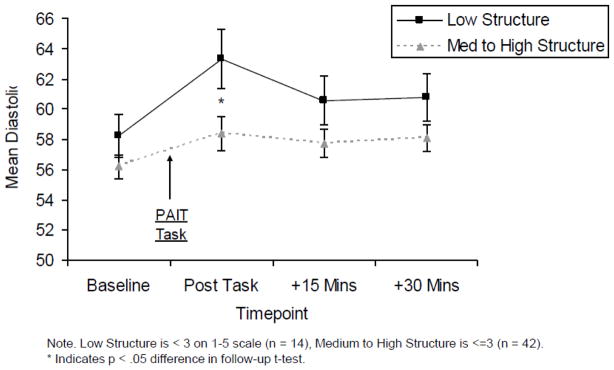
Findings revealed a significant structuring/involvement X time-point interaction for diastolic BP, F(3, 162) = 2.68, p < .05. Follow-up correlations at each time-point indicated lower structuring/involvement by parents was associated with greater diastolic BP immediately post-task (r = −.27, p < .05, Cohen’s d = .56) and at 15 minutes post-task at a trend level (r = −.23, p < .10, d = .47) (see Figure 2a). There were no significant parenting behavior X time-point interactions predicting HR or systolic BP.
Figure 2.
Figure 2a. Diastolic BP Response by Parental Structuring
Figure 2b. Anger Response by Parental Support
3.7.2. Emotions
Findings revealed a trend for a support/warmth X time-point interaction for anger, F(3, 54) = 2.63, p < .10. Follow-up correlations at each time-point indicated lower parental support/warmth was associated with adolescents’ greater reported anger immediately post-task, r = −.29, p < .05, Cohen’s d = .61 (see Figure 2b). The parenting behavior X time-point interaction was not significant for anxiety.
3.7.3. Cortisol
The parenting behavior X time-point interaction was not significant for cortisol.
3.8. Hypothesis 3: Alcohol Use History and PAIT Response
3.8.1. Heart rate and blood pressure
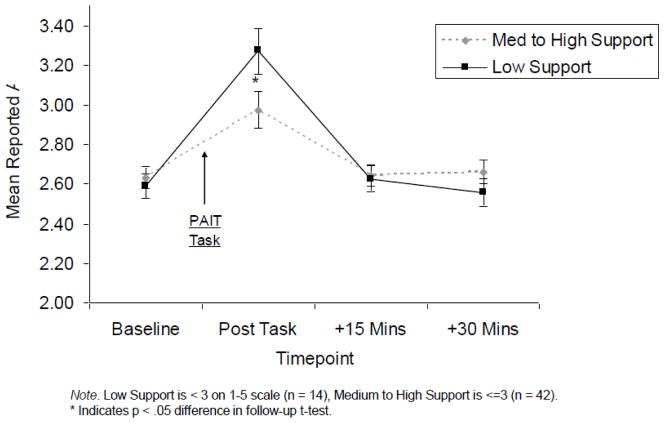
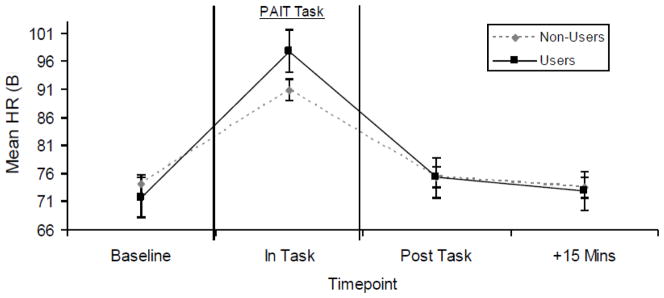
Findings revealed a significant alcohol use group X time-point interaction for heart rate, F(3, 54) = 3.02, p < .05. Follow-up contrasts at each time-point were not significant, although the pattern of means suggested higher heart rate among alcohol users than non-users during the task, with a medium effect size (Cohen’s d = .47) (see Figure 3a).
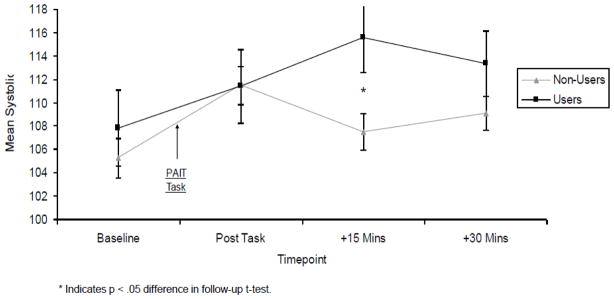
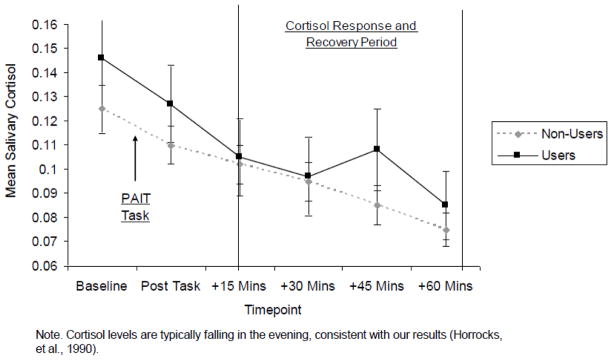
Figure 3.
Figure 3a. Heart Rate Response for Alcohol Users vs. Non-Users
Figure 3b. Systolic BP Response for Alcohol Users vs. Non-Users
Figure 3c. Cortisol Response for Alcohol Users vs. Non-Users
Findings also revealed a significant alcohol use group X time-point interaction for systolic BP, F(3, 162) = 3.74, p < .05. Follow-up contrasts at each time-point indicated higher systolic BP for alcohol users than non-users at 15 minutes post-task, t(54) = −2.40, p < .05, Cohen’s d = .77 (see Figure 3b). The alcohol use group X time-point interaction was not significant for diastolic BP.
3.8.2. Emotion
The alcohol use X time-point interactions were not significant for anger or anxiety response.
3.8.3. Cortisol
Findings revealed a trend for an alcohol use group X time-point interaction for cortisol, F(5, 50) = 2.03, p < .10. Follow-up contrasts at each time-point were not significant, but the pattern of means suggested higher cortisol for alcohol users than non-users 45 minutes after the task, with a small to medium effect size (Cohen’s d = .37) (see Figure 3c). Given that the graph suggested that there may be different time courses of cortisol response for alcohol users versus non-users, we tested this possibility. For non-users, there was a significant main effect of time (F[5, 37] = 5.36, p < .01), with cortisol levels dropping over the course of the session, as would be expected at this time of day (evening). For users, the main effect of time was not significant (F[5, 9] = 1.54, p = .27), with cortisol levels remaining elevated, even at this time of day. This may suggest a more sustained cortisol response in alcohol using youth.
4. Discussion
This study found that parent-adolescent conflict discussions produced increased emotional and physiological responses in adolescents and that less supportive and structuring parenting behaviors observed in these interactions were associated with higher blood pressure and anger responses. Furthermore, youth’s higher arousal responses were associated with their history of alcohol use. That is, those who had initiated alcohol use showed greater cardiovascular arousal and a trend for greater HPA axis arousal following the parent-adolescent interaction task. This suggests that adolescent emotional and physiological arousal in response to family interactions may be one pathway by which parenting that is low in support and structure/limit-setting is associated with adolescent alcohol use.
We found that parenting during a conflict interaction that was characterized by low levels of structure and involvement- including setting limits and explaining rules- was associated with higher blood pressure response to the interaction. In addition, low levels of warm and supportive parenting in the conflict interaction was associated with greater anger in response to the interaction in youth. Taken together, these findings suggest that the way that parents handle conflict situations may exacerbate an adolescent’s negative arousal response. Parenting that lacks warmth and structure may lead youth to feel physiologically aroused, uncomfortable, and angry. This discomfort could lead youth to avoid interactions with parents in the future and consequently have a less close family relationship, which may lead to decreased monitoring of youth, increased involvement with deviant peers, and initiation of or increase in alcohol use and possibly alcohol abuse (Brook et al., 1990).
In contrast, positive parenting characterized by structure and warmth may help adolescents to cope well with conflict, leading to less anger and blood pressure arousal. This positive coping may help youth to regulate their emotional and physiological response to family-related and other stressful interactions and may be a protective factor against their development of problem behaviors, including alcohol and substance use. Of course, our findings are correlational in nature and thus it may also be the case that youth who show greater emotional arousal elicit negative parenting. Future longitudinal studies should examine the association between parenting behaviors and youth arousal responses to parent-adolescent conflict interactions over time.
It is interesting that parenting behaviors predicted blood pressure and anger, but not heart rate, cortisol or anxiety response. It may be that blood pressure and anger are more specifically related to an anger-based “fight” responses, consistent with studies in adults linking blood pressure with poor anger regulation (e.g., Bongard & al’Absi, 2003). In contrast, heart rate, cortisol and reported anxiety may be more related to a fear or anxiety-based “flight” or withdrawal response to the interaction (Fortunato, Dribin, Granger, & Buss, 2008). Thus, negative parenting may particularly induce an angry, externalizing, outward-directed emotional response to parent-child interactions.
Our study also found important associations between youths’ physiological arousal response to the parent-adolescent conflict interaction and their history of alcohol use. Adolescents who were positive for lifetime alcohol use showed greater heart rate, systolic blood pressure, and a trend for higher cortisol response to the interaction than non-users. As noted above, feeling overly aroused by family conflict interactions may lead youth to avoid those interactions and could contribute to a disaffiliation from family and risk for alcohol use. Also, youth who feel very aroused by family conflicts (or youth who are generally overly aroused and who responded to family conflicts in the way that they respond to most stressors) may respond to conflict by engaging in alcohol use as a way to reduce stress and anxiety, consistent with the tension reduction theory of alcohol abuse (Cappell & Herman, 1972). It is also possible that youth who use alcohol may have more conflictual interactions with parents, which then lead them to feel greater arousal. In the present study, however, there were no differences in the type of conflict or the intensity of the conflict between the alcohol use groups.
In addition, it is possible that the association between adolescent response to family conflict interactions and alcohol use is due to a shared third variable. We indeed found that alcohol users had more advanced pubertal maturation and greater maturation has been associated with more conflictual parent-child relations (Paikoff & Brooks-Gunn, 1991). In addition, although the alcohol users did not differ from non-users on parent-reported externalizing or interanlizing symptoms, alcohol users may have personality traits, such as impulsivity and hopelessness, that explain their greater arousal responses. Future research with larger samples should investigate the complex (and often bi-directional) relationships between alcohol use, behavior problems, personality-related risk profiles, and youth response to family interactions. Finally, although all youth had negative breathalyzers on the day of the interaction task, adolescents’ past alcohol use may have altered their physiological response systems, leading to greater arousal responses. This is unlikely, given the low frequency of use in these youth; however, it is a possibility. Future research should control for this by observing family interactions in youth with no history of alcohol use in analyses of predictors of initiation of use. If this research finds that youth arousal responses are a pathway by which negative parenting leads to alcohol use, alcohol abuse prevention programs could target youth with high arousal responses and could isolate and help modify the specific parenting behaviors in conflict interactions that lead to high arousal responses. It is interesting that adolescent reported emotional (anxiety and anger) responses to the parent-adolescent interaction were not associated with their history of alcohol use. Previous studies have shown links between alcohol/substance use and high negative emotional arousal in daily life (Wills, Sandy, & Yeager, 2002) and in parent-adolescent interactions (Hops et al., 1990). The present study did find links between heart rate, blood pressure, and cortisol response and youth’s alcohol use, which may indicate that alcohol using youth were aroused internally by the interaction but were not aware of or did not admit their heightened arousal in their self-reports of emotional arousal. Given that being aware of one’s emotional arousal is a central component of emotional competence (Denham, 2007), this may suggest that adolescent alcohol users lack emotoinal competence, which may have negative implications for their ability to regulate emotions appropriately.
It is also notable that the present study did not find gender differences in alcohol use or adolescent arousal response to the interactions. Our study may have been under-powered to detect gender differences. Given the important gender differences in emotional and physiological stress responses found in the literature (e.g., Chaplin & Aldao, 2011), future studies with larger samples should examine gender effects.
4.1. Conclusions
This study was the first to examine associations between parenting behaviors, adolescents’ emotional, cardiovascular, and HPA axis response to parent-adolescent conflict interactions, and alcohol use initiation. We found that parenting that is low in support and structure was associated with higher arousal responses to family interactions and, furthermore, that greater arousal in response to these interactions was associated with youth’s alcohol use. Our study is limited to the examination of associations cross-sectionally and in a community sample of youth. Future longitudinal research should examine parenting and adolescent arousal responses to family interactions in early adolescence as these predict initiation of and increases in alcohol use across adolescence and alcohol abuse in later adolescence and adulthood. If arousal responses to family interactions do indeed predict alcohol and substance use, this could help to inform alcohol and substance abuse prevention programs. Such programs could focus on helping youth learn to regulate their stress responses to family conflicts and helping to foster a parenting environment that is sensitive to and helps reduce youth’s arousal.
Fig. 4.
Fig. 5.
Fig. 6.
Highlights.
We observed parent-adolescent conflict interactions.
We examined links between adolescent responses to interactions and alcohol use.
Negative parenting predicted higher blood pressure and anger response.
Higher heart rate, blood pressure, and cortisol response were linked to alcohol use.
Responses to family conflict may play a role in initiation of addictive behavior.
Acknowledgments
Role of Funding Sources
Funding for this project was provided by the National Institutes of Health (NIH) through grants K01-DA-024759 and UL1-DE19586 pilot grant and by grants from the ABMRF/Foundation for Alcohol Research and from the American Academy of Child and Adolescent Psychiatry. The study sponsors had no involvement in the study design, collection, analysis, and interpretation of data; the writing of the manuscript; or the decision to submit the manuscript for publication.
Support for this project was provided by the National Institutes of Health (NIH) through grants K01-DA-024759 (PI: First Author) and UL1-DE19586 pilot grant (PI: Last Author) and by grants from the ABMRF/Foundation for Alcohol Research (PI: First Author) and from the American Academy of Child and Adolescent Psychiatry (PI: 6th Author). The authors gratefully acknowledge these study sponsors, the participating families, and the research staff, particularly the following assistants who helped to conduct the laboratory sessions: Cameron Grey, Mary Piepmeier, Emily Cook, Gillian Ritter, Naaila Panjwani, Chetna Chandrasekaran, Jenny Robb, Hayley Grunebaum, Taylor Stavely, and Devon Testa.
Footnotes
Contributors
Tara Chaplin designed the study, analyzed the data, and wrote the first draft of the manuscript. Rajita Sinha contributed to the study design and data analysis approach. Jessica Simmons and Stephen Healy oversaw the conduct of the laboratory sessions and contributed to interpretation of findings. Linda Mayes, Rebecca Hommer, and Michael Crowley recruited participating families and oversaw collection of self-report data. All authors contributed to and have approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Author Disclosure
The four statements of the author disclosure document are described below. Statements should not be numbered. Headings (i.e., Role of Funding Sources, Contributors, Conflict of Interest, Acknowledgements) should be in bold with no white space between the heading and the text. Font size should be the same as that used for references.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tara M. Chaplin, Email: tara.chaplin@yale.edu.
Rajita Sinha, Email: Rajita.sinha@yale.edu.
Jessica Simmons, Email: Jessica.simmons@yale.edu.
Stephen Healy, Email: Stephen.healy@yale.edu.
Linda C. Mayes, Email: Linda.mayes@yale.edu.
Rebecca E. Hommer, Email: Rebecca.hommer@yale.edu.
Michael J. Crowley, Email: michael.crowley@yale.edu.
References
- Barnes GM, Reifman AS, Farrell MP, Dintcheff BA. The effects of parenting on the development of adolescent alcohol misuse: A six-year wave latent growth model. Journal of Marriage & the Family. 2006;62(1):175–186. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bongard S, al’Absib M. Domain-specific anger expression assessment and blood pressure during rest and acute stress. Personality and Individual Differences. 2003;34:1383–1402. [Google Scholar]
- Brener ND, Kann L, McManus T, Kinchen SA, Sundberg EC, Ross JG. Reliability of the 1999 Youth Risk Behavioral Survey Questionnaire. Journal of Adolescent Heath. 2002;31:336–342. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- Cappell H, Herman CP. Alcohol and tension reduction: A review. Quarterly Journal of Studies on Alcohol. 1972;33:33–64. [PubMed] [Google Scholar]
- Chambers R, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: A critical period of addiction vulnerability. The American Journal of Psychiatry. 2003;160:1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplin TM. Anger, happiness, and sadness: Associations with depressive symptoms in late adolescence. Journal of Youth and Adolescence. 2006;35:977–986. [Google Scholar]
- Chaplin TM. Unpublished manual. Yale University School of Medicine; 2010. Parent-Adolescent Interaction Task (PAIT) Coding System. [Google Scholar]
- Chaplin TM, Aldao A. Gender differences in emotion expression in children: A meta-analytic review. Psychological Bulletin. 2011 doi: 10.1037/a0030737. In revision. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. Journal of Abnormal Psychology. 2004;113(4):483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Clark DB, Thatcher DL, Maisto SA. Supervisory neglect and adolescent alcohol use disorders: Effects of AUD onset and treatment outcome. Addictive Behaviors. 2005;30(9):1737–1750. doi: 10.1016/j.addbeh.2005.07.017. [DOI] [PubMed] [Google Scholar]
- Denham SA. Dealing With Feelings: How Children Negotiate the Worlds of Emotions and Social Relationships. Cognitie Creier Comportament. 2007;11:1–48. [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, Miller S, Pettit GS, Bates JE. A dynamic cascade model of the development of substance-use onset. Monograghs of the Society for Research in Child Development. 2009;74:71–74. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erath SA, El-Sheikh M, Cummings EM. Harsh parenting and child externalizing behavior: Skin conductance level reactivity as a moderator. Child Development. 2009;80:578–592. doi: 10.1111/j.1467-8624.2009.01280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field A. Discovering statistics using SPSS (Introducing statistical methods series) London: SAGE Publications, Inc; 2005. [Google Scholar]
- Fortunato CK, Dribin AE, Granger DA, Buss KA. Salivary alpha-amylase and cortisol in toddlers: Differential relations to affective behavior. Developmental Psychobiology. 2008;50(80):807–818. doi: 10.1002/dev.20326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion: How families communicate emotionally. Mahwah, NJ: Lawrence Erlbaum Associates; 1997. [Google Scholar]
- Granger DA, Weisz JR, McCracken JM, Ikeda SC, Douglas P. Reciprocal influences among adrenocortical activation, psychosocial processes, and the behavioral adjustment of clinic-referred children. Child Development. 1996;67:3250–3262. [PubMed] [Google Scholar]
- Hops H, Tildesley E, Lightensten E, Ary D, Sherman L. Parent-adolescent problem-solving interactions and drug use. American Journal of Drug and Alcohol Abuse. 1990;16(3 & 4):239–258. doi: 10.3109/00952999009001586. [DOI] [PubMed] [Google Scholar]
- Horrocks PM, Jones AF, Ratcliffe G, Holder A, White R, Holder JG, Ratcliffe, London DR. Patterns of ATCH and cortisol pulsatility over twenty-four hours in normal males and females. Clinical Endocrinology. 1990;32:127–134. doi: 10.1111/j.1365-2265.1990.tb03758.x. [DOI] [PubMed] [Google Scholar]
- Izard CE. Patterns of emotions: A new analysis of anxiety and depression. New York: Academic Press; 1972. [Google Scholar]
- Johnson V, Pandina RJ. Effects of the family environment on adolescent substance use, delinquency, and coping styles. The American Journal of Drug and Alcohol Abuse. 1991;17:71–88. doi: 10.3109/00952999108992811. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national resulys on adolescent drug use: Overview key findings, 2010. Ann Arbor: Institute for Social Research, University of Michigan; 2011. [Google Scholar]
- Kertes DA, Gunnar MR. Evening activities as a potential confound in research on the adrenocortical system in children. Child Development. 2004;75(1):193–204. doi: 10.1111/j.1467-8624.2004.00663.x. [DOI] [PubMed] [Google Scholar]
- Masten A, Faden VB, Zucker RA, Spear LP. Underage drinking: A developmental framework. Pediatrics. 2008;121(4):S235–S251. doi: 10.1542/peds.2007-2243A. [DOI] [PubMed] [Google Scholar]
- Mayzer R, Fitzgerald HE, Zucker RA. Anticipating problem drinking risks from preschoolers’ antisocial behavior: Evidence for a common delinquency-related diathesis model. Journal of the American Academy of Child & Adolescent Psychiatry. 2009;48(8):820–827. doi: 10.1097/CHI.0b013e3181aa0383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA) Smoking and drinking continue to decline, but marijuana stalls in latest MTF survey. NIDA Notes. 2009;22:19. [Google Scholar]
- Paikoff RL, Brooks-Gunn J. Do parent-child relationships change during puberty? Psychological Bulletin. 1991;110:47–66. doi: 10.1037/0033-2909.110.1.47. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of Applied Behavioral Analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25:333–334. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child & Adolescent Psychology. 1996;25:317–329. [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1982. pp. 290–293. [Google Scholar]
- Sprafkin J, Gadow KD, Salisbury H, Schneider J, Loney J. Further evidence of reliability and validity of the Child Symptom Inventory-4: Parent Checklist in clinically referred boys. Journal of Clinical Child and Adolescent Psychology. 2002;31:513–524. doi: 10.1207/S15374424JCCP3104_10. [DOI] [PubMed] [Google Scholar]
- Susman EJ, Dockray S, Schiefebein VL, Herwehe S, Heaton JA, Dorn LD. Morningness/eveningness morning-to-afternoon cortisol ratio and antisocial behavioral problems during puberty. Developmental Psychology. 2007;43:811–822. doi: 10.1037/0012-1649.43.4.811. [DOI] [PubMed] [Google Scholar]
- Tildesley EA, Andrews JA. The development of children’s intentions to use alcohol: Direct and indirect effects of parent alcohol use and parenting behaviors. Psychology of Addictive Behaviors. 2008;22(3):326–339. doi: 10.1037/0893-164X.22.3.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Vorst H, Engels RCME, Meeus W, Dekovic M. Parental attachment, parental control, and early development of alcohol use: A longitudinal study. Psychology of Addictive Behaviors. 2006;20:107–116. doi: 10.1037/0893-164X.20.2.107. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM. Stress and smoking in adolescence: A test of directional hypotheses. Health Psychology. 2002;21:122–130. [PubMed] [Google Scholar]