Abstract
Objective
To compare maternal and neonatal outcomes of vacuum versus forceps application in assisted vaginal delivery.
Material and Method
Women in labor with vertex presentation were delivered by vacuum and forceps. A total of 120 cases were included in this prospective study. Maternal and neonatal morbidity were compared in terms of perineal lacerations, episiotomy extension, post-partum hemorrhage, Apgar score, instrumental injuries, NICU admissions PNM etc. χ2 test was used to analyze the data.
Observations
Maternal morbidity viz. episiotomy extension as well as first and second degree perineal tear were significant in the forceps group (P = 0.0001 and P = 0.02, respectively). With regards to neonatal morbidity, no statistically significant difference was noted.
Conclusion
Vacuum and forceps should remain appropriate tools in the armamentarium of the modern obstetrician. However, ventouse may be chosen first (if there is no fetal distress) as it is significantly less likely to injure the mother.
Keywords: Vacuum extraction, Forceps, Maternal morbidity, Neonatal outcome
Introduction
Modern obstetrics practice has witnessed an increase in the caesarean section rates everywhere. Assisted vaginal delivery, with the use of forceps and vacuum extraction, offers the option to accomplish safe delivery for the mother and the clinician. A successful assisted vaginal delivery avoids caesarean section, its attendant uterine scar and its implications for future pregnancy. Reintroduction of this art will definitely find a place in emergency obstetric care.
The present study was designed to assess the feto-maternal outcome by comparing vacuum with forceps.
Materials and Methods
A total of 120 cases were included in this prospective study carried out from Aug 2007 to Feb 2009. The various indications for instrumental delivery were fetal distress, non progressive second stage of labor, to cut short second stage of labor, poor maternal efforts. After case selection, written and informed consent was taken, prerequisites fulfilled and women were randomly assigned for either vacuum or forceps application.
A detailed history was taken and obstetric examination done. Data on women giving birth by vacuum and forceps deliveries were analyzed and compared in terms of parity, gestational age, station of fetal head at the commencement of extraction, presentation, indications.
Silastic cup was used in vacuum extraction. Forceps deliveries were performed using short curved outlet Wrigley’s forceps.
Maternal morbidity was analysed in terms of perineal, vaginal, cervical lacerations, episiotomy extension, urinary incontinence, traumatic postpartum haemorrhage.
Neonatal complications in both groups including low Apgar score, unexplained convulsions, jaundice, scalp and facial injuries, cephalhematoma, birth asphyxia, neonatal sepsis, were investigated and compared.
Condition of mother and baby at the time of discharge was noted. χ2 test was used to analyze the data.
Results and Discussion
Although deliveries by vacuum extraction and forceps are certainly not a substitute for caesarean delivery, they are safe obstetric practices with many benefits when protocols are followed. United States have the instrumental delivery rates between 10 and 15% [1].
The mean age of women in our study was 23.81±3.6 years. The two groups did not vary significantly with respect to age and parity. 64.1% women required delivery by assisted methods. This was also observed in a population based retrospective analysis in the United States [2] (Photograph 1).
Photograph 1.
Ventose bruise mark
Mean birth weight in our study was 2.80 ± 0.39 kg. We observed that birth weight >3.5 kg was significantly common in the forceps group. (P = 0.015) (Table 1). The use of instruments is more frequent in infants with higher birth weight and gestational age [3].
Table 1.
Neonatal characteristics
| Characteristics | Ventouse (n = 60) | Forceps (n = 60) | P value | |
|---|---|---|---|---|
| Gestational age (weeks) | <37 | 1 | 1 | – |
| 37–40 | 52 | 49 | 0.10 (NS) | |
| >40 | 7 | 10 | 0.21 (NS) | |
| Birth weight (gm) | <2,000 | 4 | 2 | 0.06 (NS) |
| 2,001–2,500 | 11 | 16 | 0.10 (NS) | |
| 2,501–3,000 | 32 | 26 | 0.12 (NS) | |
| 3,001–3,500 | 11 | 16 | 0.10 (NS) | |
| 3,501–4,000 | 2 | 7 | 0.015 (S) | |
| >4,000 | – | – | ||
| Apgar score (at 1 min) | 0–3 | – | 2 | |
| 4–6 | 13 | 18 | 0.121 (NS) | |
| 7–10 | 47 | 40 | 0.151 (NS) | |
| Apgar score (at 5 min) | 0–3 | – | 2 | |
| 4–6 | 9 | 10 | 0.694 (NS) | |
| 7–10 | 51 | 48 | 0.584 (NS) | |
We found no significant difference in Apgar scores between the two study groups. Similar observations were made in a Malaysian study by Archanna [4] (Photograph 2).
Photograph 2.
Forceps abrasion mark
Most common indication was to cut short second stage of labour (pre-eclampsia, previous caesarean section, heart disease, anaemia) followed by prolonged second stage of labour, fetal distress and maternal exhaustion. Forceps was the chosen method in cases of fetal distress in significantly more no. of parturient (35%) as compared to ventouse (8.33%) (Table 2).
Table 2.
Indications for application
| Indications | Ventouse (n = 60) | Forceps (n = 60) | P value |
|---|---|---|---|
| Prolonged second stage | 12 | 8 | 0.06 (NS) |
| Poor maternal effort | 5 | 2 | 0.006 (S) |
| Fetal distress | 5 | 21 | 0.001 (S) |
| Heart disease | 1 | 1 | – |
| Severe anaemia | 7 | 2 | 0.001 (S) |
| Pre-eclampsia | 19 | 18 | 0.77 (NS) |
| Previous C. S. | 11 | 3 | 0.001 (S) |
| Eclampsia | – | 1 | – |
| Face | – | 1 | – |
| Failure of descent | – | 2 | – |
| Preterm (twin) | – | 1 | – |
There are no universal guidelines to describe the time taken to deliver once the decision has been made. The decision-to-delivery interval was 8.6 ± 5.4 min for forceps and 13.8 ± 6.2 min for vacuum deliveries in our study (P = 0.0001). It appears that it is quicker to accomplish forceps delivery in cases of fetal distress than VE.
In Okunwobi’s study, the decision-to-delivery interval was 23.3 min for forceps and 29.2 min for vacuum extraction (P = 0.04) [5].
The figures in Table 3 reveals that vacuum can be applied in less than full cervical dilatation (10 cm). Use of the vacuum extractor before full cervical dilatation still is accepted by some authorities, but only in highly selected circumstances. These include delivery of a second baby of twin, multipara and when caesarean section carries a very high risk of maternal morbidity and mortality [6].
Table 3.
Cervical dilatation at the time of application of ventouse
| Cx dilatation (in cm) | No. of cases (n = 60) | Successful VE (n = 52) | Unsuccessful VE (n = 8) |
|---|---|---|---|
| 10 | 52 | 48 | 4 |
| 9 | 6 | 3 | 3 |
| 8 | 2 | 1 | 1 |
| 7 | – | – | – |
| 6 | – | – | – |
Patel also concluded that vacuum is more useful in multigravida especially when dilatation is 8–9 cm and rim is present [7].
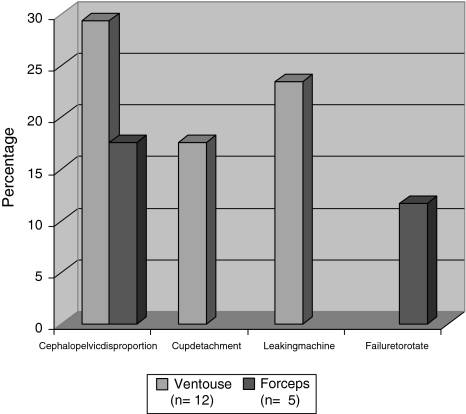
Figure 1 summarizes failure rates of assisted delivery. Unexpected failure of instrumental delivery is not rare. In the present study, 12 cases in the ventouse group and five cases in the forceps group were failed (14.1%). Cephalopelvic disproportion was the cause in majority (47%). Trial of instrumentation should be bypassed in cases of absolute feto-pelvic disproportion with or without fetal distress and/or more than one-fifth of the fetal head above the pelvic brim. This is an indication of primary caesarean section. Of greater concern is the fact that serious neonatal and maternal injuries have been attributed to the use of multiple instruments. RCOG guidelines states that sequential use of instruments should be avoided wherever possible and should not be attempted by inexperienced operators [8]. Similarly, SOGC clinical practice guidelines suggest that failure of the chosen method vacuum and/or forceps in a reasonable time should be considered an indication for abandonment of the method [9].
Fig. 1.
Reasons for failure in the two study groups
The maternal morbidity was significantly less in VE group as compared to forceps group (P = 0.002) (Table 4). Perhaps, the strongest evidence in favour of the vacuum extractor comes from the results of meta-analyses published by Cochrane Database (1999). showed that the vacuum extractor was associated with a lower caesarean section rate, a lower usage of regional and general anaesthesia, with apparently less pain at delivery, significantly less pain at 24 h and significantly less likely to cause serious maternal injury than forceps. It seemed that the vacuum extractor could ‘do no wrong’ [10].
Table 4.
Maternal morbidity in instrumental deliveries
| Morbidity | Ventouse | Forceps | P value |
|---|---|---|---|
| Episiotomy | 48 | 56 | 0.17 (NS) |
| Episiotomy extension | 8 | 24 | 0.0015 (S) |
| Vaginal wall tear | – | 10 | |
| Periurethral tear | – | 4 | |
| Extension to fornices | – | 2 | |
| Cervical tear | – | 8 | |
| First and second degree perineal tear | 3 | 8 | 0.02 (S) |
| Third and fourth degree perineal tear | – | 2 | |
| Postpartum haemorrhage | – | 2 | |
| Length of hospital stay | 24 h | 36 h | |
| Blood transfusion needed | – | 4 |
In a randomised controlled trial in 2002, Eason E showed that a decrease of 4.9 in adjusted relative risk in anal spinchter injury when vacuum was used over forceps [11].
The risk of neonatal morbidity was similar between infants delivered by vacuum or forceps (Table 5). A study by Prapas, documented that the rate of neonates with Apgar scores ≤5 at 1 min was significantly higher after forceps compared with vacuum delivery (18% vs. 5.2%, respectively, P = 0.0003). However the rate of neonatal trauma did not differ significantly between the two groups [12]. RCOG, concluded that: obstetricians should be competent, and confident, in the use of both vacuum and forceps, but, in view of reduction of maternal injuries the vacuum should be considered to be the instrument of first choice [8].
Table 5.
Neonatal morbidity and mortality
| Variables | Ventouse | Forceps | P value |
|---|---|---|---|
| Cephalhematoma | 10 | 1 | 0.0001 (S) |
| Instrumental marks and bruising | 6 | 23 | 0.0001 (S) |
| Subconjunctival hemorrhage | – | 3 | |
| Brachial plexus injury | – | – | |
| Convulsions | 2 | 4 | 0.193 (NS) |
| Neonatal hyperbilirubinemia | 10 | – | |
| Use of phototherapy | 4 | – | |
| Feeding difficulty | 1 | 1 | |
| Irritability | – | – | |
| Neonatal ICU admissions | 4 | 4 | |
| PNM | – | – |
Conclusion
Our study analysed maternal and fetal outcomes in assisted vaginal deliveries and suggests that ventouse application is associated with significantly less maternal trauma than with forceps. There seems to be no difference in neonatal outcome. The major factor which determines the safety of the instrument is the operator rather than the instrument. Either method can be used in the hands of a skilled operator with an appropriate level of expertise and good judgement. Encouraging operative vaginal deliveries may help to reduce the unwarranted and raised caesarean section rates.
That is why, the art of Instrumental delivery using either vacuum or forceps should be taught to the residents. Also, those who have learnt its usage, but are not using it any longer, should undergo training programme/workshops to update themselves so as to reach the WHO recommendation of a 10–15% caesarean section rate set to achieve optimal maternal and perinatal safety.
References
- 1.ACOG Practice Bulletin. Clinical management guidelines for obstetricians-gynecologists. Number 17. 2000.
- 2.Demissie K, Rhoads GG, Smulian JC, et al. Operative vaginal delivery, neonatal, infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329:24. doi: 10.1136/bmj.329.7456.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wen S, Shiliang L, Kramer SM, et al. Comparison of maternal and infant outcomes between vacuum extraction and forceps deliveries. Am J Epidemiol. 2001;153:103–107. doi: 10.1093/aje/153.2.103. [DOI] [PubMed] [Google Scholar]
- 4.Archanna S, Monga D. Outcome of forceps delivery versus vacuum extraction—a review of 200 cases. Singapore Med J. 1994;35:605–608. [PubMed] [Google Scholar]
- 5.Okunwobi YS, Cooke I, Mackenzie IZ. Decision to delivery intervals for assisted vaginal vertex delivery. BJOG. 2000;107:467–471. doi: 10.1111/j.1471-0528.2000.tb13263.x. [DOI] [PubMed] [Google Scholar]
- 6.Miksovsky P, Watson WJ. Obstetric vacuum extraction: state of the art in the new millennium. Obstet Gynaecol Surv. 2001;56:736–751. doi: 10.1097/00006254-200111000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Patel BS, Pandya NC, Sahram AS. Maternal and perinatal outcome in forceps and ventouse extraction delivery: a comparative study. Obstet Gynaecol Surv. 2000;5:614–619. [Google Scholar]
- 8.Royal College of Obstetricians & Gynaecologists. Instrumental vaginal delivery. Guideline No. 26. London: RCOG; 2005.
- 9.Cargill YM, Mackinnon CJ.Guidelines for operative vaginal birth. Society of obstetrician & gynecologists of Canada, SOGC clinical practice guidelines no. 148 J Obstet Gynecol Can 200426747–753.15307980 [Google Scholar]
- 10.Johnson RB, Menon V. Vacuum extraction versus forceps for assisted vaginal delivery. Cochrane Database of Systematic Reviews; 1999 (issue 2). [DOI] [PubMed]
- 11.Eason E, Labraque M, Marioux S, et al. Anal incontinence after childbirth. CMAJ. 2002;166:326–330. [PMC free article] [PubMed] [Google Scholar]
- 12.Prapas N, Kalogiannidis I, Masoura S, et al. Operative vaginal delivery in singleton term pregnancies: short term maternal and neonatal outcomes. Hippokratia. 2009;13:41–45. [PMC free article] [PubMed] [Google Scholar]