Introduction
Endometrioid adenocarcinoma is the most common form (nearly 80%) of endometrial carcinoma. These tumors are referred to as ‘endometrioid’ because they resemble proliferative phase of the endometrium. It is common in post-menopausal women (>50 years) and presents as abnormal vaginal bleeding [1]. About 1–8% of these carcinomas occur in women less than 40 years. Small numbers of cases have been reported in women under the age of 30 years, the youngest being 15 years. It is unusual in younger age group and can be wrongly diagnosed [2, 3]. Majority of patients present with clinical evidence of polycystic ovarian disease but in some reports the patients lacked these features [4]. With this background we present a case of endometrial carcinoma in a young woman who presented with fibroid.
Case Report
Miss X, a 30 year old presented with complaints of menorrhagia since 6 months and abdominal pain since 2 months. No other significant complaints noted. Her previous menstrual history was normal and there was no history of diabetes, hypertension, and tuberculosis in the family. General physical examination was normal. Abdominal examination revealed a 14–16 week size uterus which was non-tender. On vaginal examination, the uterus was 14 weeks size and pushed to the right side.
Investigations
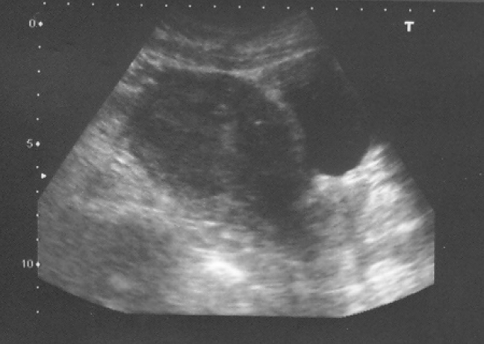
Blood investigations revealed Hb% of 7.6 g/dl, ESR of 24 mm/h with other blood counts being normal. Chest X-ray was normal. Ultrasound showed ante-verted uterus measuring 7.8 × 3 × 4.8 cm. Two fibroids noted, one in the anterior wall measuring 6.7 × 6 cm and the other in the posterior fundal area measuring 5 × 4.5 cm. Endometrium was 10 mm in thickness (Fig. 1).
Fig. 1.
TVS ultra-sound
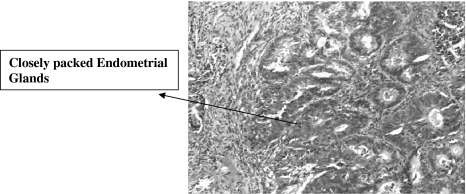
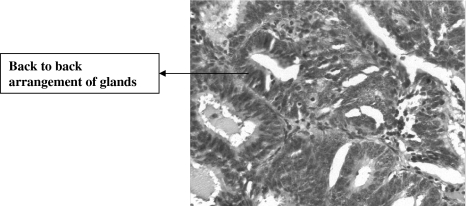
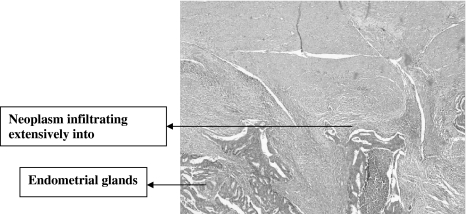
Case was posted for myomectomy following blood transfusion. Intra operative findings revealed a 14-week size uterus with an anterior wall fibroid measuring 10 cm × 10 cm for which myomectomy was done. Uterine cavity was opened to look for the posterior fibroid. A cheesy material was drained and sent for histopathology. Myomectomy cut-section showed whorled appearance with cystic and hemorrhagic areas. Endometrial curetting sections showed closely packed endometrial glands with back-to-back with no intervening stroma, pleomorphic stromal infiltration and areas of necrosis. Histopathological diagnosis was adeno-carcinoma (endometrioid) and leiomyoma (Figs. 2, 3).
Fig. 2.
Low power microscopy
Fig. 3.
High power microscopy
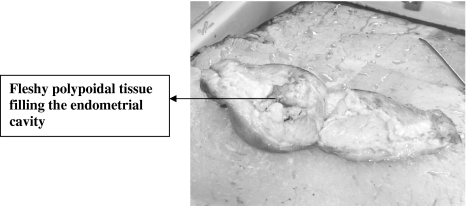
We were in dilemma for further management considering her age and fertility status. Patient was counseled regarding the management. Staging laparotomy was done with Total abdominal hysterectomy with bilateral salpingo oophorectomy and peritoneal sampling was negative. Gross pathology showed enlarged uterus with anterior myomectomy scar. Cut section showed fleshy polypoidal growth infiltrating myometrium and endocervical canal (Figs. 4, 5).
Fig. 4.
Gross pathology
Fig. 5.
Cut section of uterus
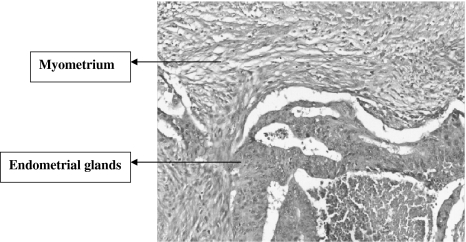
Surgicopathological staging was Adenocarcinoma endometrium well differentiated (G1) Involving >1/2 myometrium and endocervical canal (Stage II B) with normal adnexae (Figs. 6, 7). Post operative radiotherapy was given. Patient was advised for follow up treatment.
Fig. 6.
Low power microscopy
Fig. 7.
High power microscopy
Discussion
The median age group of patients with endometrial carcinoma is 61 years with 75–80% being post menopausal. Only 3–5% is less than 40 years. In the present case it was surprising to see endometrial carcinoma in the younger age group. Endometrial curette was not done pre operatively, keeping in mind the patient’s age, marital status and ultrasound diagnosis.
Endometrial cancer is an estrogen dependent disease. Chronic exposure to estrogen without accompanying balancing effect of progesterone is considered the major risk for endometrial cancers. Unopposed estrogen condition (premenopausal anovulatory phase like PCOD and functioning ovarian tumors) predisposes to endometrial cancers [4, 5].
There is considerable evidence that reproductive factors play a role in etiology of endometrial carcinoma [6]. Nulliparity/Nulligravida is associated with increased risk and there is positive association between infertility and endometrial cancer in young women [7]. Age related risk factors of endometrial cancer shows that there is known inverse association between age at menarche. Women who started menstruating at 15 years had about 1/3 risk of cancer compared to those at age 10 years or younger. Risk of endometrial cancer was higher among women who were older, heavier and had not been married.
High dose progesterone 200 mg/day has been reported successfully to reverse atypical hyperplasia and well differentiated endometrial adenocarcinoma in 16 (94%) premenopausal women younger than 40 years. Average treatment course required to achieve disease regression was 9 months [8, 9].
To conclude, in a case of fibroid, of more than a decade of menstrual life, an effort should be made to exclude associated neoplastic endometrial pathology, irrespective of the age.
References
- 1.Kaku T, Matsumura M, Sakai K, et al. Endometrial carcinoma in women 65 years of age or older: a clinical study. Eur J Gynaecol. 1996;17:35. [PubMed] [Google Scholar]
- 2.Farhi DC, Nosanchuk J, Silverberg SG. Endometrial adenocarcinoma in women under 25 years of age. Obstet Gynecol. 1986;68:741–775. [PubMed] [Google Scholar]
- 3.Brinton LA, Berman MH, Mortel R, et al. Reproductive, menstrual and medical risk factors for endometrial cancer results from a case control study. Am J Obstet Gynecol. 1993;81:265–271. doi: 10.1016/s0002-9378(11)91709-8. [DOI] [PubMed] [Google Scholar]
- 4.McPherson CP, Sellers TA, Potter JD, et al. Reproductive factors and risk of endometrial cancer: the Iowa women’s health study. Am J of Epidemiology. 1996;143:1195–1202. doi: 10.1093/oxfordjournals.aje.a008707. [DOI] [PubMed] [Google Scholar]
- 5.Dahlgren E, Freiberg LG, Johansson S, et al. Endometrial carcinoma ovarian dysfunction—a risk factors in young women. Eur J Obstet Gynecol. 1991;41:143–150. doi: 10.1016/0028-2243(91)90092-Y. [DOI] [PubMed] [Google Scholar]
- 6.La Vecchia C, Franceschi S, Decarli A, et al. Risk factors for endometrial carcinoma at different ages. J Natl cancer Inst. 1984;73:667–671. [PubMed] [Google Scholar]
- 7.Parazzini F, La Vecchia C, Bocciolone L, et al. The epidemiology of endometrial cancer. Gynaecol Oncol. 1991;41:1–16. doi: 10.1016/0090-8258(91)90246-2. [DOI] [PubMed] [Google Scholar]
- 8.Gal D. Hormone therapy for lesions of the endometrium. Semin Oncol. 1986;13:33–36. [PubMed] [Google Scholar]
- 9.Frenzy A, Gelfand M. The biologic significance of cytological atypia in progestin treated endometrial hyperplasia. Am J Obstet Gynecol. 1989;160:26–131. doi: 10.1016/0002-9378(89)90103-8. [DOI] [PubMed] [Google Scholar]