Abstract
Objectives
Background-Contraception is the intentional prevention of conception through the use of various devices, sexual practices, chemicals, drugs or surgical procedures. An effective contraception allows a physical relationship without fear of an unwanted pregnancy and ensures freedom to have children when desired. The aim is to achieve contraception in maximum comfort and privacy, with minimum cost and side effects. Some methods, like male and female condoms, also provide twin advantage of protection from sexually transmitted diseases. The burden of unsafe abortion lies primarily in developing countries. Here, contraceptive prevalence is measured among currently married women of reproductive age, and levels have not yet reached those that exist in developed countries.
Conclusion
In countries like India, there is a dire need for contraceptive methods to be more women friendly, accessible and provide adequate privacy. Providers also need to be sensitive to special needs of adolescents as they are at a critically vulnerable segment.
Keywords: Contraception, Condoms, Vasectomy, Tubectomy, STDs
Introduction
Contraception is defined as the intentional prevention of conception through the use of various devices, sexual practices, chemicals, drugs, or surgical procedures. Thus, any device or act whose purpose is to prevent a woman from becoming pregnant can be considered as a contraceptive. In any social context effective contraception allows a couple to enjoy a physical relationship without fear of an unwanted pregnancy and ensures enough freedom to have children when desired. The aim is to achieve this with maximum comfort and privacy, at the same time minimum cost and side effects. Some barrier methods, like male and female condoms, also provide twin advantage of protection from sexually transmitted diseases (STDs).
Need for Contraception
Protection Against Unwanted Pregnancy
A growing number of women and men of reproductive age wish to regulate their fertility and have fewer children. Between the ages of 20 and 44, a fertile, sexually-active woman is potentially capable of giving birth about 12 times, even if she breastfeeds each baby for 1 year. To avoid the need for an abortion, she has to successfully practice birth control for 16–20 of her roughly 25 childbearing years [1].
Couples are faced with conflicting goals of achieving satisfying sex life and keeping a small family, failure to do so results in unwanted pregnancy and abortions. When abortion seeking is risky, late or in the hands of unsafe providers or unhygienic conditions, it can lead to both reproductive morbidity and maternal mortality. World over, if contraception is accessible and used consistently and correctly by women wanting to avoid pregnancy, maternal deaths would decline by an estimated 25–35% [2, 3]. In India, the surveys suggest that abortions are responsible for 10–20% of all maternal deaths [4]. There is a need for awareness regarding effective contraceptive methods, their correct and consistent use.
Need for Protection Against Sexually Transmitted Diseases
The transmissibility of several STIs and HIV/AIDS is greater from infected man to uninfected woman than the reverse [5]. The vagina offers a large mucosal surface exposed to the partner’s sexual secretions and a more conducive environment for microbial growth than the penile surface in men, therefore biologically, women are more vulnerable to STIs than men. Since the infected semen stays in the vagina for a while, a man can infect the woman more effectively. Also semen contains higher concentration of virus than the woman’s sexual secretions. Thus, men are twice more effective as transmitters of STIs than women.
Vulnerability of Adolescents
Usually younger women, married or unmarried, are less likely to be using contraception than older women, even in countries where contraceptive prevalence rate (CPR) is high [6]. At macro level, laws, regulations and social policies that determine the access to contraception, affect adult and adolescent women alike in terms of the types of contraceptives that are permitted for distribution or prescription. But at the micro level, there are differences between adolescents and adult women, in fertility level, maturity, knowledge, negotiation in sexual relations and experience, coupled with social expectations affecting their behavioral patterns, as they relate to contraceptive acceptance and use. This increases their vulnerability to unprotected sex and its adverse consequences manifold.
Early sexual debut for adolescent girls means that chances of exposure to infections begin even before completing the process of physiological maturation. Though the systems have begun to function, the defense mechanisms are still evolving, particularly of the cervix. The cervical mucus acts as non-specific barrier for various ascending organisms in adult women. Adolescents do not have the benefit of this mucosal defensive mechanism till several years after menarche [7–9]. This increases their susceptibility to infection up to six times compared to their adult counterparts, particularly gonorrhoea, chlamydia and HIV [10].
Contraceptive Methods
Known methods of contraception include the following:
Traditional Methods
Coitus Interruptus or Withdrawal
Involves withdrawal of penis from the vagina just before ejaculation, thus preventing semen from entering the woman. This is perhaps the oldest contraceptive method known to man, but it depends on the cooperation of the male partner. This is not a reliable method and may fail if semen escapes before ejaculation or is left on external sex organs. Man needs good self-control, both emotionally and physically, for this method to succeed.
Lactational Amenorrhoea Method
Nursing women secrete hormones that prevent conception for about 6 months. It prevails if there is no menses and full breast-feeding day and night is maintained. This is more a myth as, breast-feeding is irregular, 60% women start menstruating by the third month. Not reliable in instances where baby sleeps through the night, or in case of sore, cracked or inverted nipples and breast abscess. Many unsuspecting women conceive during this period before return of menstruation.
Rhythm Method
This method requires predicting ovulation, the period when the woman is most fertile, by recording the menstrual pattern, or body temperature, or changes in cervical mucus, or a combination of these (symptom-thermal method). Intercourse is avoided on fertile days. Although a large number of people claim knowledge of this method, only a small proportion can actually identify the fertile period of the month. It cannot be used by women who have irregular periods, or after childbirth, or during menopausal years. Intercourse is limited to some days of the month only. The method requires careful record keeping for calculating the safe period.
Modern Methods
Male Condom
In this, a thin rubber or latex sheath (condom) is rolled on the erect penis before intercourse. It prevents semen (sperms) from entering the woman. The method is 95% effective if used correctly. It can be used by all age groups, safely. No prior medical examination is required and is easily available without prescription. It serves as the most effective method in providing twin protection of contraception and STI disease. The major drawback in this method is related to compliance, inconsistency and incorrect use. Total use by men in India varies from 2 to 14% in Punjab and 18% in Delhi [11]. There are disadvantages intrinsic to this method, as it may tear or slip if not used properly. Expired or perforated condoms should not be used. Extra supply should be maintained in readiness whenever required.
Female Condom
This is a vaginal pouch made of latex sheath, with one ring at each end. The closed end ring is inserted inside the vagina and works as the internal anchor. Outer portion covers and protects the external genitalia. It is reliable, hypo-allergic with high acceptance in test groups although its cost could be a major deterrent to use. It is a female controlled method and protects from both unwanted pregnancy and STDs. Size and hardness of inner ring may be uncomfortable to some users. Extensive promotion and persuasion among female users is required to make it popular.
Oral Contraceptive Pills
The combined pill consists of two hormones: estrogen and progesterone. This is to be taken everyday orally by the woman. The pill works by preventing the release of the egg, thickening of cervical mucus and by altering tubal motility. It is to be prescribed after a medical check-up. Almost 100% effective if taken regularly. It is an easy and convenient, woman-controlled method and does not interfere with love-making. There is regular monthly cycle often with reduced pain and bleeding. Can be discontinued when pregnancy is desired. The pills must be taken regularly and do not work when consumed later than 12 h. The pills are unsuitable for women over 35 years or those with family history of heart, liver diseases, hypertension, diabetes or unexplained vaginal bleeding. Failure rates are higher in younger, less educated women. Adolescents are less likely to take pills correctly and consistently.
Injectables
These inhibit ovulation and also increase the viscosity of the cervical secretions to form a barrier to sperms. It is a 99% effective, easily administered method, suitable during lactation too. It has non-contraceptive advantages, like recession of ovarian cysts or breast lumps. Menstrual cycle may become irregular, spotting or cease altogether as long as the injectables are used. There may be gain in weight and return to fertility may take time. Subsequent injections should not be delayed more than 2 weeks from the prescribed date. Counseling and support are needed for women when this method is chosen.
Emergency Contraceptive Pill
Here, two doses of the pill, separated by 12 h, are taken within 3 days (72 h) of unprotected intercourse. Depending on the time of menstruation it is taken, it can prevent ovulation, fertilization or implantation of the fertilized egg. It is available without prescription. Its uses include-prevention of pregnancy after condom tear/slips, when two oral pills are missed in succession, when an intra-uterine device is expelled and there is fear of conception, in case injectables are delayed by more than 2 weeks.
Surgical Methods
Intrauterine Devices (IUDs)
A small flexible, plastic device, usually with copper, is inserted into the womb by a qualified medical practitioner, after menstruation, abortion, or 4-6 weeks after delivery. It prevents the fertilized egg from settling in the womb. Copper ions have spermicidal activity. It is 95–98% effective, does not interfere with love-making and can be removed when pregnancy is desired. It may cause heavy bleeding in some women. Pelvic inflammation in women, especially those exposed to STDs, may occur. Sometimes the IUD loosens and detaches and hence should be checked periodically. It may increase risk of ectopic pregnancy. It is unsuitable for women with cervical or pelvic infection, uterine fibroids, heavy menstruation, or unexplained vaginal bleeding.
Female Sterilization (Tubectomy)
This is a permanent surgical method in which the fallopian tubes are cut and ends tied to prevent the sperms from meeting the eggs. It is a very reliable method requiring only 1 day of hospitalization and can be performed anytime, preferably after last child’s birth. Rarely, the tubes may join and fertility may return. A few women tend to have heavier periods after this method. Though this is a permanent method, the operation can be reversed, though the results may not be always successful. Hence the couple should be firm about their decision before opting for this method.
Male Sterilization (Vasectomy)
A permanent surgical method in which, the vasa deferentia which carry the sperms from the testes to the penis, are blocked. This prevents the sperms from being released into the semen at the time of ejaculation. It is a simple and reliable method not requiring hospitalization. Contrary to popular belief, it does not affect health or sexual vigour, neither does it interfere with intercourse.
Methods Available in Many Developed Countries
Diaphragm and Spermicides (Barrier/Chemical Method)
A soft rubber cap is fitted into the vagina shortly before the intercourse, to cover the cervix, thus preventing sperms from entering the uterus. It must be left in place for at least 6 h after intercourse. The method is much more effective, when used in combination with a spermicidal cream to inactivate the sperms. It does not interrupt love-making and can be used a few hours before intercourse. Insertion and removal are simple, once learnt from the doctor and there are no complications after use. The user must use additional spermicides if more than 3 h elapse between insertion and intercourse. The cap must be inserted before every intercourse. Different sizes suit different women and a correct size should be used. Size may change after childbirth or if there is weight gain or loss of more than three kilograms and so, must be checked every 6 months. Medical assistance is necessary to select right size and learn how to insert and remove it.
Implants-Hormonal
The Norplant capsule is implanted below the skin by minor surgery. It suppresses ovulation, creates thick cervical mucus which prevents sperms from entering the cervix and also creates a thin, atrophic endometrial lining. It is not related to coitus. It is suitable for women seeking continuous contraception. Its effect lasts for approximately 5 years and therefore it becomes a long term birth spacing method. When the capsule is removed using minor surgery, fertility is restored in 2–4 months. The woman must visit the clinic 2–3 times a year for periodic check-up. Not suitable for women with threatened malignancy of breast, cervix, uterus or ovaries, those suffering from blood disorders or heart diseases, pregnant or suspected to be pregnant women and also those suffering from liver infections and diseases.
Hormonal Contraception for Men
Hormonal approaches, which employ formulations of testosterone administered in combination with other hormones, have shown considerable promise in clinical trials, and they are currently at the forefront of research and development. However, the long-term effects of using hormones throughout a male’s reproductive life for contraception are unknown, and it may take time before this information becomes available [12].
Global Trends in Contraceptive Use
In many developing countries contraceptive prevalence measured among currently married women of reproductive age have been growing rapidly, but have not yet reached the levels that exist in the developed countries. Unsafe abortion rates are highest in Africa, Latin America and the Caribbean, followed closely by South and South-East Asia, while in Europe and North America the rates are negligible.
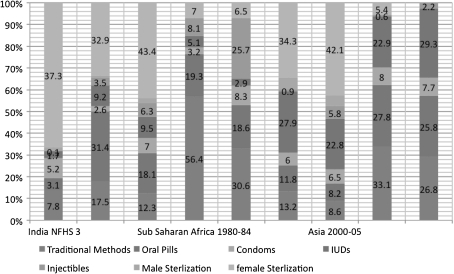
Traditional Methods
The proportion of traditional methods changed markedly over time in Sub-Saharan Africa. In surveys conducted in 1980–1984, 56% of users in this region reported employing traditional methods, while in 2000–2005 it declined to 31%. Traditional methods represented a much smaller proportion of the method mix in Asia (decreased from 13 to 9%) and in Latin America and the Caribbean, where it decreased from 18 to 12%, respectively. India’s current dependence on traditional methods is comparable to the Asian figures at 7.8% (Fig. 1).
Fig. 1.
Changes in contraceptive methods in developing countries compared with NFHS 3 Data of India. Source: summarized from [13]
Oral Pill
Overall, the proportion of all users relying on the pill fell, but the most dramatic decline—from 31 to 18%—occurred in Latin America and the Caribbean. In India utilization of this method is poor at 3%. In developed nations it is 25% of contraception.
Condoms
The proportion of married female contraceptive users relying on condoms rose in Latin America and the Caribbean, as well as in Sub-Saharan Africa, from 3% in the early 1980s to 7–8% in 2000–2005. While condom use is slowly increasing in developing countries, it has fallen from 8 to 7.7% in the developed world. India’s share too falls below the figures of developing countries.
Intra Uterine Devices (IUDs)
The proportion of IUD use decreased in Asia from 27.9 to 22.8%. According to NFHS 3 the IUD segment is currently being used by only 1.7% of married women.
Injectables
There was a small increase in Asia, Latin America and the Caribbean. The proportion of users relying on injectables climbed steadily over those using the pill. But, in India it is grossly underutilized at 0.1%.
Sterlization Male
Women’s reliance on male sterilization for contraception was low in all periods, with figures below 3% for all periods. In Asia, however, the proportion of users relying on vasectomies rose to 9% in 1990–1994, before dropping back to 5% in 2000–2005. This drop is contributed by three Asian countries (viz., from 9 to 4% in India, from 19 to 16% in Nepal and from 8 to 6% in Sri Lanka.
Sterilization Female
For the past 26 years, female sterilization has accounted for at least one-third of all contraceptive use in Asia, Latin America and the Caribbean (where it peaked at 48% in 1990–1994). In Asia, female sterilization rose from 34% in 1980–1984 to 42–43% in 1985–2005. In contrast, the share of female sterilization remained fairly level at 5–8% in Sub-Saharan Africa and developed countries. As is evident it is the favoured method in India at 37. 3%.
Contraception in India
In India, in order to achieve demographic targets the stress is on terminal surgical methods, applicable to women who have finished their child-bearing. Sterilization particularly of female, dominates all modern methods used [11–14]. Adolescents on the other hand have their reproductive careers ahead of them, their needs are rather to postpone or space pregnancies, which requires reversible and non-invasive methods. There is a shift from terminal to reversible methods. The focus on termination of fertility has led to an induced reduction in reproductive span of young Indian women.
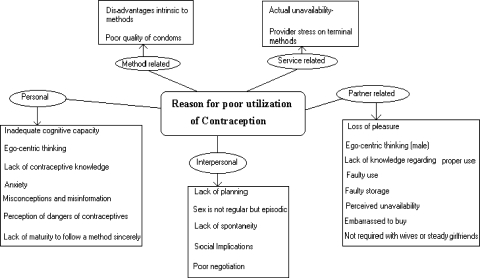
The explanations for delaying, underutilization and failure to use contraception appear to be numerous and complex (Fig. 2).
Fig. 2.
Reasons for poor utilization of contraception and skewed method mix
Personal
The intrinsic characteristics of the adolescent associated with contraceptive decision-making:
Inadequate Cognitive Capacity
A relationship requires logical, systematic and deductive decision-making to deal with various possibilities and consequences. In pre-adolescence, concrete thinking does not allow for complete understanding of risks involved in sexual indulgence. Only when the adolescent moves from concrete to more abstract thought processes, he or she is able to engage in responsible sexual decision-making.
Ego-Centric Thinking
Olson and Rollins [15] have used the Elkind theory, to argue that the very immature and impulsive adolescent is likely to be dominated by a form of egocentric thinking, which leads her to believe that “it can’t happen to her”. This leads them to take chances that their older counterparts will not take.
Lack of Contraceptive Knowledge
Chhabra in her study of abortion-seeking unmarried girls reported that 88% did not know the link between sexual relations and pregnancy [4]. Although most ever married adolescents know of at least one method of contraception (90%), this is most likely to be sterilization, which is unsuitable for the adolescents.
Anxiety
The cognitive problems are further accentuated by anxiety related to indulging in socially disapproved activity, which prevents adolescents from seeking reliable advice. Lack of essential sexual information increases anxiety and interferes with appropriate use of contraception resulting in contraceptive failure.
Misconceptions and Misinformation
Research on relation between adolescents’ knowledge of birth control and their utilization of contraception indicates that most sexually active adolescents in urban settings know about contraception but this apparent knowledge does not predict the actual use of birth control during coital activity [16]. Misconceptions about the safe period, possibility of conceiving without breaking hymen or in single chance are reasons for failure to use contraception.
Perception of Dangers of Contraceptives
The beliefs regarding dangers of birth control are distinct from actual exposure to birth control information and devices. Olson and Rollins [15] found that adolescents believed that condoms and IUDs could move upwards in the woman’s body and cause complications or pills cause permanent infertility.
Lack of Maturity to Follow a Method Sincerely
Most adolescents’ understanding of a method is usually incomplete and confused, contraceptive failure therefore is higher in adolescents compared to adult women. Adolescents find it difficult to take a pill everyday, at the same time, in an orderly manner and maintain a continuous supply of pills.
Partner Related
Partner-related failure mostly pertains to condom use or an indifference towards what their girl friends or wives resort to, and disadvantages of these methods in disease protection.
Loss of Pleasure
Generally men report that condoms reduce the pleasure of sexual intercourse [17, 18]. Interruption in foreplay is a source of displeasure. The thickness of the sheath reduces sensation and lack of lubrication makes it uncomfortable, and may cause vaginal irritation in female partners [19]. Commercial brands have brought thinner, textured and better lubricated varieties but they are expensive. These features, however, have increased acceptability in the middle and upper income groups.
Ego-Centric Thinking (Male)
Like women, younger men, are also prone to unreasonable optimism, a form of egocentric thinking which leads them to believe that they can avoid pregnancy solely depending upon natural methods.
Lack of Knowledge Regarding Proper Use
Most men do not know the right method to put on and take off a condom, and are shy to ask reliable sources. Condom is perceived as required by men with deviant sexual tendencies or those frequenting sex workers [20].
Faulty Use
Use of condoms requires that the penis should enter the vagina only after being protected and left when it is still erect and by holding the condom rim to avoid spillage back into the vagina. Often men enter unprotected during foreplay during this period little quantity of semen is produced that may cause pregnancy. Also condoms should be used with water-soluble lubricants. Petroleum jelly and Vaseline weaken or perforate the condom and render it useless [19].
Faulty Storage
People often hide condoms from children and family members by storing in cupboards, under clothes or mattresses, where due to pressure, heat and humidity, their quality deteriorates [19].
Perceived Unavailability
Young men usually express ignorance of places to find condoms or that they cannot afford the expenditure, but fail to access the public health facilities where these are available openly and free of cost [21].
Embarrassed to Buy
Partners often avoid use of condoms due to the embarrassment of purchasing them.
Not Required With Wives or Steady Girlfriends
There is a general belief that condom need only be used in risky relations like, with sex workers. Men rely mostly on natural methods with wives and steady partners [19]. At times condoms are used in the beginning of the relationship but gradually women are persuaded to shift to female methods [22].
Interpersonal
There are several other reasons that influence the decision to use or skip contraception.
Lack of Planning
The episodes of sex occur at times without planning, following dates, parties or use of alcohol. Couples also forget to carry condoms/pills when they travel.
Sex is not Regular but Episodic
At times when the male partner lives away, visits are erratic and pills are discontinued. [23].
Lack of Spontaneity
The adolescents complain that wearing a condom interrupts love-making and the spontaneity of the occasion is lost.
Social Implications
Women fear that asking a partner to use condom before sex would imply she is loose. Male claims that carrying a condom gives an impression, as if he had planned to have sex and tricked the partner into it [24].
Poor Negotiation
Women are usually more motivated to protect themselves against disease and pregnancy, yet men often return their resistance to refuse unprotected sex, with emotional or physical abuse [25]. Compared to sex workers, steady partners resign because unmarried women cannot afford to lose the partner and married women are socially and economically dependent on them [26].
Method Related
Poor Quality of Condoms
Condoms may fail due to poor quality, faulty packaging or storage and transit. Sometimes sealing machines might seal the pack such that the condom is pressed too; at times seal is incomplete and lubricant dries up [21].
Disadvantages Intrinsic to Methods
Every method has some disadvantages associated with it, which interferes with people successfully using it and result in discontinuation or faulty use.
Service Related
Actual Unavailability
Often there is erratic supply of condoms and pills at health centers [19].
Provider Stress on Terminal Methods
Providers are preoccupied with completing demographic targets and older clients are focused upon to accept terminal methods. They do not offer them complete information on choice of methods available [27–29].
Conclusion
The above account points to the fact that contraceptive usage is often biased towards female sterilization. Women are forced to rush child bearing and seek the terminal method once their desired parity is achieved. One can utilize the example of Africa and promote injectibles or educate women on oral pills like in developed nations. Better usage of government promoted condoms and pills is called for. The facilities need to be more women friendly, accessible and provide adequate privacy. Also, providers need to be sensitive to special needs of adolescents as they are at a critically vulnerable segment.
References
- 1.Sharing responsibility: women, society and abortion worldwide. New York: AGI; 1999. [Google Scholar]
- 2.Maternal mortality in 2005; Estimates Developed by WHO, UNICEF, UNFPA and The World Bank, WHO, Geneva 2007.
- 3.Lule E, Singh S, Chowdhury SA. Fertility regulation behavior and their costs: contraception and unintended pregnancies in Africa and Eastern Europe and Central Asia. Washington: World Bank; 2007. [Google Scholar]
- 4.Chhabra R, Nuna C. Abortion in India: an overview. New Delhi: Veerendra printers, Ford Foundation; 1994. [Google Scholar]
- 5.Washington AE, Cates W, Wasserheit J. Preventing pelvic inflammatory disease. JAMA. 1991;266(4):2574–2580. doi: 10.1001/jama.1991.03470180074041. [DOI] [PubMed] [Google Scholar]
- 6.Blanc AK, Tsui AO, Croft TN, Trevitt JL. Patterns and trends in adolescents’ contraceptive use and discontinuation in developing countries and comparisons with adult women. Int Perspect Sex Reprod Health. 2009;35(2):63–71. doi: 10.1363/3506309. [DOI] [PubMed] [Google Scholar]
- 7.Dehne KL, Riedner G. Sexually transmitted infections among adolescents: the need for adequate health services. Geneva: World Health Organization; 2005. [DOI] [PubMed] [Google Scholar]
- 8.Cowan FM, Mindel A. Sexually transmitted diseases in children: adolescents. Genitourin Med. 1993;69(2):141–147. doi: 10.1136/sti.69.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilot P and Islam MQ. Sexually transmitted diseases in the 1990s: global epidemiology and challenges for control. Sex Transm Dis. 1994; 21(supp 2): S7–S13. [PubMed]
- 10.Ramasubban R. Women’s vulnerability: recent evidence on sexually transmitted infections. In: Ramasubban R, Jejeebhoy SJ, editors. Women’s Reproductive Health in India. Jaipur: Rawat Publications; 2000. pp. 280–330. [Google Scholar]
- 11.IIPS & ORG Macro. National family health survey-2: India. 1998–99. Mumbai: International Institute for Population Sciences; 2000.
- 12.Cheng CY, Mruk DD. New frontiers in nonhormonal male contraception. Contraception. 2010;82(5):476–482. doi: 10.1016/j.contraception.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seiber EE, Bertrand JT, Sullivan TM. Changes in contraceptive method mix in developing countries. Int Fam Plan Perspect. 2007;33(3):117–123. doi: 10.1363/3311707. [DOI] [PubMed] [Google Scholar]
- 14.Jayaraman A, MishraV ArnoldF. The relationship of family size and composition to fertility desires, contraceptive adoption and method choice in South Asia. Int Perspect Sex Reprod Health. 2009;35(1):29–38. doi: 10.1363/3502909. [DOI] [PubMed] [Google Scholar]
- 15.Olson L, Rollins J. Psychological barriers to contraceptive use among adolescent women. In: Stuart I, Wells C, editors. Pregnancy in adolescence: needs, problems, and management. New York: Van Nostrand; 1982. [Google Scholar]
- 16.Gandotra MM, Das NP. Factors influencing choice of a contraceptive and the reason for it’s discontinuation. In: Khan ME, Cernada G, editors. Spacing as an alternative strategy: India’s family welfare programme. New Delhi: B.R. Publishing Corporation; 1996. pp. 94–114. [Google Scholar]
- 17.Nichter M, Nichter M. Modern methods of fertility regulation: when and for whom are they appropriate? In: Nichter M, editor. Anthropology and international health: South Asian case studies. Dordrecht: Kluwer Academic Publishers; 1989. pp. 57–82. [Google Scholar]
- 18.Kapur P. A study of changes in the sexual behaviour of call girls and their clients in India. Paper presented at the workshop on Sexual Aspects of AIDS/STD Prevention in India. Mumbai : Tata Institute of Social Sciences; 1993.
- 19.Nag M. Sexual behaviour and AIDS in India. New Delhi: Vikas Publishing House Pvt. Ltd; 1996. [Google Scholar]
- 20.Joshi C. AIDS awareness: transmitting embarrassment. New Delhi: India Today; 1994. pp. 114–115. [Google Scholar]
- 21.Gopalakrishnan K. Promoting condoms. Seminar. 1992;396:34–36. [Google Scholar]
- 22.Jejeebhoy SJ, Santhya KG, Verma RK, et al. Setting the stage. In: Jejeebhoy SJ, et al., editors. Looking back looking forward: a profile of sexual and reproductive health in India. New Delhi: Population Council; 2004. pp. 3–24. [Google Scholar]
- 23.Govinda P, Dahal SS, Padmadas S, AndrewHinde PR. Fertility-limiting behaviour and contraceptive choice among men in Nepal. Int Fam Plan Perspect. 2008;34(1):6–14. doi: 10.1363/3400608. [DOI] [PubMed] [Google Scholar]
- 24.Fisher HE. Lust, attraction and attachment in mammalian reproduction. Hum Nat. 1988;9:23–52. doi: 10.1007/s12110-998-1010-5. [DOI] [PubMed] [Google Scholar]
- 25.Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Population reports series L, No. 11. Baltimore: Johns Hopkins University School of Public Health, Population Information Program; 1999. [Google Scholar]
- 26.Elias CJ and Heise L. The development of microbicides: A new method of HIV prevention for women. Population council (programme division) Working Paper No. 6. New York: Population Council; 1993.
- 27.Barge S, Ramchander L. Provider and clients interactions in primary health care: a case study from Madhya Pradesh. In: Koening MA, Khan ME, editors. Improving quality of care in India’s family welfare programme: the challenge ahead. New York: Population Council; 1999. pp. 92–116. [Google Scholar]
- 28.Khan ME, Patel BC, Chandrasekhar R. Study of MTP acceptors and their subsequent contraceptive use. J Fam Welf. 1993;36(3):70–85. [Google Scholar]
- 29.Khan ME, Gupta RB, Bella CP. The quality of coverage of family planning services in Uttar Pradesh: Client perspectives. In: Michael AK, Khan ME, editors. Improving quality of care in India’s family welfare programme: The challenge ahead. New York: The Population Council; 1999. pp. 49–69. [Google Scholar]