Abstract
Background
The 2010 international guidelines for CPR recently recommended an increase in the minimum compression depth from 38 to 50 mm, although there are limited human data to support this. We sought to study patterns of CPR compression depth and their associations with patient outcomes in out-of-hospital cardiac arrest (OOHCA) cases treated by the 2005 guideline standards.
Methods and Results
We studied emergency medical services treated OOHCA patients from the Resuscitation Outcomes Consortium Epistry - Cardiac Arrest for whom electronic CPR compression depth data were available, from May 2006 to June 2009. We calculated anterior chest wall depression in millimeters and the period of active CPR (chest compression fraction) for each minute of CPR. We controlled for covariates including compression rate and calculated adjusted odds ratios for any return of spontaneous circulation (ROSC), 1-day survival, and hospital discharge.
We included 1,029 adult patients from 7 U.S. and Canadian cities with these characteristics: mean age 68 years; male 62 %; bystander witnessed 40%; bystander CPR 37%; initial rhythms - VF/VT 24%, PEA 16%, asystole 48%, other non-shockable 12%; outcomes - ROSC 26%, 1-day survival 18%, discharge 5%. For all patients, median compression rate was 106 per minute, median compression fraction 0.65, and median compression depth 37.3 mm with 52.8% of cases having depth < 38 mm and 91.6% having depth < 50 mm. We found an inverse association between depth and compression rate (P<0.001). Adjusted odds ratios for all depth measures (mean values, categories, and in range) showed strong trends towards better outcomes with increased depth for all three survival measures.
Conclusions
We found suboptimal compression depth in half of patients by 2005 guideline standards and almost all by 2010 standards, as well as an inverse association between compression depth and rate. We found a strong association between survival outcomes and increased compression depth but no clear evidence to support or refute the 2010 recommendations of > 50 mm. While compression depth is an important component of CPR and should be measured routinely, the most effective depth is currently unknown.
Keywords: cardiac arrest, cardiopulmonary resuscitation, compression depth, emergency medical services
B>INTRODUCTION
Out-of-hospital cardiac arrest (OOHCA) is a very common problem with an estimated 330,000 cases occurring each year in the United States and Canada.1 Overall, survival to hospital discharge for OOHCA patients treated by emergency medical services (EMS) remains poor with survival rates ranging from 3.0% to 16.3%, for all rhythms combined. Variation in patient survival rates among communities can be mostly attributed to local differences in the implementation of the five links in the chain of survival, as described by the American Heart Association: 1) rapid access, 2) early cardiopulmonary resuscitation (CPR), 3) early defibrillation, 4) early advanced cardiac life support (ACLS), and 5) post-resuscitation care. 2-6
Recently, there has been a renewed realization that the quality, quantity, and timeliness of CPR are key determinants for survival from cardiac arrest and that delivery of chest compressions is often suboptimal.7;8 Recent technological advances now allow the detailed measurement and review of key compression parameters.9;10 Using this technology, Christenson demonstrated a clear association between survival for ventricular fibrillation (VF) patients and the proportion of each resuscitation minute during which compressions were delivered (chest compression fraction).11
Current CPR guidelines for compression rate and depth have been, for the most part, derived with relatively little robust human data to support them.3;12 The 2005 guidelines recommended a depth range of 38-50 mm whereas the new 2010 guidelines recommend a depth of at least 50 mm. For compression depth, clinical studies to date have been small with insufficient power to evaluate clinically important outcomes and have tended to focus on VF patients only.7;13-15 There is a need for larger studies to evaluate the association of compression depth with survival in all rhythm groups.9;16 The Resuscitation Outcomes Consortium (ROC) is comprised of 10 U.S. and Canadian universities and their regional EMS systems and has a mandate to conduct large controlled trials of prehospital interventions for cardiac arrest and trauma. ROC has established the ROC Epistry-Cardiac Arrest, a prospective multicenter observational registry of OOHCA in EMS agencies and receiving institutions in seven US and three Canadian sites.17 ROC Epistry includes patient outcomes and electronic data on CPR process. The objective of this study was to examine patterns of CPR compression depth and their associations with patient outcomes in out-of-hospital cardiac arrest cases treated by the 2005 guideline standards.
METHODS
Design and Setting
The ROC EMS network consists of 36,000 EMS professionals within 260 EMS agencies, provides coverage to an estimated 24 million persons from urban, suburban, and rural communities, and transports patients to 287 different hospitals.18 This study represents an analysis of a convenience sample of ROC Epistry-Cardiac Arrest cases treated by EMS and for whom electronic compression depth were available. Sites that did not have the technical capacity to measure compression depth were not included and, hence, this study included data from 58 participating EMS agencies affiliated with seven U.S. and Canadian ROC sites. At the time of the study, OOHCA patients were being treated according to the 2005 guideline standards for compression depth (38-50 mm).
Population
We included all persons from the ROC Epistry, aged 18 or older, who suffered non-traumatic cardiopulmonary arrest outside of the hospital within the catchment area of a participating ROC EMS agency and were treated with defibrillation and/or delivery of chest compressions by EMS providers. For this study we excluded patients who did not have attempts at resuscitation by EMS, with an obvious cause of arrest, whose arrests were EMS witnessed, who received a shock from a bystander applied AED, and anyone who had more than 5 minutes of CPR before the pads were applied. We also excluded patients for whom at least one minute of electronic CPR compression depth data was not available. These data may have been unavailable because some EMS agencies do not use defibrillators with accelerometers capable of measuring compression depth or because of inadvertent failure to capture and transmit the data. We included patients with any initial cardiac rhythm.
The ROC Epistry was reviewed and approved by the appropriate local institutional review boards (U.S.) or research ethics boards (Canada) without the need for informed consent from subjects as the registry was considered minimal risk. Strict confidentiality was maintained at all times and no personal identifiers were retained in the database.
Data Collection
The characteristics of chest compressions were measured via an accelerometer interface between the rescuer and the patient’s chest using commercially available defibrillators. Tracings were acquired and downloaded from Phillips (N=482; Andover, MA, USA) and ZOLL (N=547; Chelmsford, MA, USA) defibrillators.10;19 CPR process measures, including compression rate, chest compression fraction, and compression depth, were calculated by proprietary automated external defibrillator analytic software. Chest compression fraction was defined as the proportion of resuscitation time without spontaneous circulation during which chest compressions were administered. Compression depth was defined as the posterior depression of the anterior chest wall in mm. Most cases included the one-minute interval during which the first rhythm analysis was performed and all recorded one-minute intervals prior to the first analysis (including time before and after the first shock if a shock was delivered). The mean compression values for all minute intervals were averaged for each patient. For compression depth, we defined within recommended range as per the 2005 international guidelines with an average mean depth greater than 38 mm. We described the case as “within recommended depth” if the mean depth was 38 mm or more for more than 60% of minutes recorded.
Patient and clinical data were abstracted from EMS and hospital records using standardized definitions for patient characteristics, EMS process, and outcome at hospital discharge. Data were abstracted locally, coded without personal health information, and transmitted to the data coordinating center electronically. Site-specific quality assurance included initial EMS provider training in data collection, and continuing education of EMS providers. The data coordinating center assured the quality of the data by a variety of techniques.1
Outcome Measures
The primary outcome was survival to hospital discharge, defined as discharged alive from hospital after the index OOHCA. Patients who were transferred to another acute care facility (e.g. to undergo implantable cardioverter defibrillator placement) were considered to still be hospitalized. Patients were considered discharged if transferred to a non-acute ward or facility. The secondary outcomes were survival for one day and return of spontaneous circulation. Survival for one day meant that the patient was still alive one day past the date of the event. Return of spontaneous circulation refers to the presence of a palpable pulse for any duration of time prior to arrival at hospital. Data were abstracted from collated EMS and hospital source documents.
Statistical Analysis
All statistical analyses were performed with commercially available statistical packages (SAS, version 9.1.3, Cary, NC; R, version 2.5.1, Vienna, Austria). Summary results are presented as mean (±SD) or median (IQR). To test differences in baseline characteristics between subjects who did and did not survive to discharge, likelihood ratio chi-squared tests or t-tests were used as appropriate. Analysis of variance was used to compare mean compression depths across study sites. The distribution of depth categories across sites was compared with likelihood ratio chi-squared test, as was the test for association between depth and rate categories. The association between compression depth and outcomes of interest was quantified using multivariate logistic regression. Smoothing splines were used to explore the relationship between average compression depth and outcome.14
RESULTS
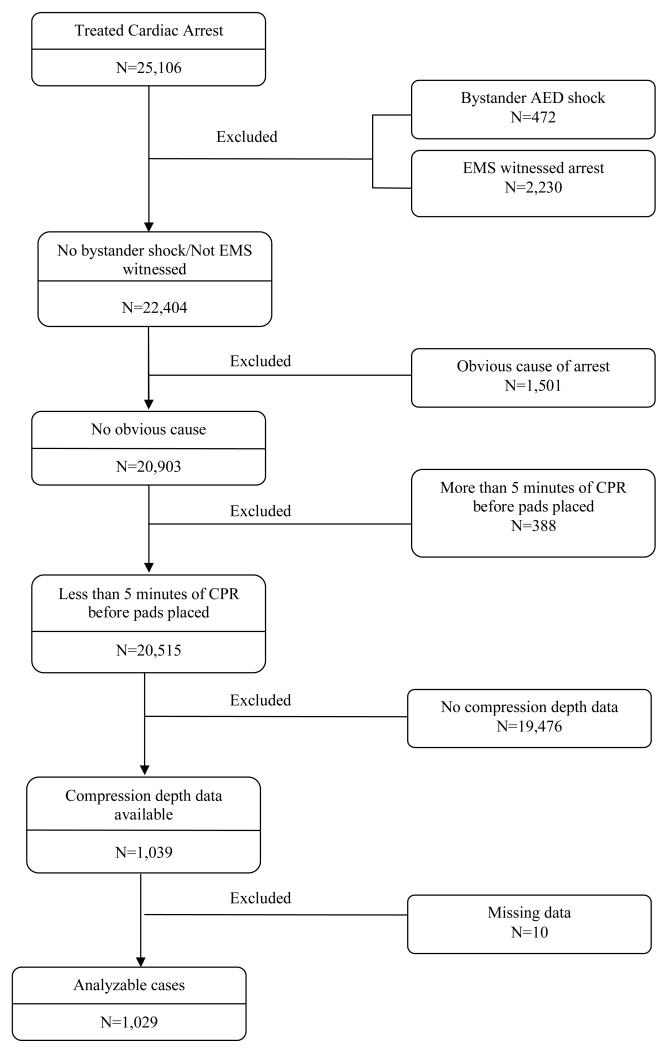
During the study period from May 2006 to June 2009, EMS agencies in the 11 participating ROC sites treated 25,106 cases of cardiac arrest who were not enrolled in a ROC clinical trial. Of these patients, all but 1,029 were excluded from the current analysis for the reasons indicated in Figure 1. Four ROC sites could not measure compression depth and contributed no cases to the study. The 1,029 patients in the final study cohort were very similar in characteristics and outcomes to those excluded except they had quicker response time intervals and were more likely to be treated by an ALS EMS crew.
Figure 1. Patient flow.
The patients in the study were typical of OOHCA cases with only 13% from a public location, 40% bystander witnessed, 37% bystander CPR, 99% having an ALS EMS crew in attendance (Table 1). The median values for CPR process measures were 106 (IQR 96-117) for compression rate and 0.65 (IQR 0.56-0.75) for chest compression fraction. Of all patients, 25.7% had return of spontaneous circulation, 18.2% survived one day, and 4.9% survived to hospital discharge.
Table 1.
Baseline Patient Characteristics
| Characteristics | N=1029 |
|---|---|
| Age - mean (SD) | 67.9 (16.7) |
| Male - n (%) | 640 (62.2%) |
| Public location – n (%) | 133 (12.9%) |
| Bystander witnessed – n (%) | 413 (40.1%) |
| Bystander CPR – n (%) | 377 (36.6%) |
|
| |
| Site - n (%) | |
| Dallas, Texas, USA | 10 (1.0%) |
| Milwaukee, Wisconsin, USA | 62 (6.0%) |
| Ottawa-OPALS, Ontario, Canada | 140 (13.6%) |
| Pittsburgh, Pennsylvania, USA | 394 (38.3%) |
| Portland, Oregon, USA | 46 (4.5%) |
| Seattle-King County, Washington, USA | 33 (3.2%) |
| Toronto, Ontario, Canada | 344 (33.4%) |
|
| |
| EMS Response | |
| Time in minutes from 911 to scene – median (Q1, Q3) | 5.4 (4.1, 6.8) |
| Time in minutes from 911 to first EMS shock assessment – median (Q1, Q3) | 10.5 (8.5, 12.7) |
|
| |
| ALS first on scene – n (%) | 314 (30.8%) |
| ALS on scene – n (%) | 1,019 (99.0%) |
| Number responding EMS units1 - mean (SD) | 2.8 (0.8) |
|
| |
| CPR process measures | |
| CPR prior to first analysis – n (%) | 60.6% (624) |
| CPR fraction – median (Q1, Q3) | 0.65 (0.56, 0.75) |
| Chest compression rate – median (Q1,Q3) | 106.0 (95.9, 117.1) |
|
| |
| Initial cardiac rhythm (%) | |
| VF/VF | 243 (23.8%) |
| PEA | 160 (15.7%) |
| Asystole | 489 (47.8%) |
| AED no shock, no strip | 122 (11.9%) |
| Cannot Determine | 8 (0.8%) |
|
| |
| EMS Interventions | |
| Intubation attempted - n (%) | 768 (74.6%) |
| Shocks delivered - n (%) | 398 (38.7%) |
| Epinephrine - n (%) | 846 (82.2%) |
|
| |
| Outcomes | |
| Any pre-hospital ROSC – n (%) | 264 (25.7%) |
| Survived at least one day – n (%) | 187 (18.2%) |
| Survived to hospital discharge – n (%) | 50 (4.9%) |
Information was only available about the first four EMS units at the scene.
Note: percentages are of cases with non-missing data
Table 2 displays compression depth data with all measures showing significant variation across the seven participating sites. The median chest compression depth was 37.3 mm (IQR 32-43) with 52.8% of cases having a mean value less than 38 mm. In addition, we calculated that 59.3% of cases were not within the 2005 recommended range for depth and, on average, 52.7% of all CPR minutes within a case had a mean depth less than 38 mm.
Table 2.
Compression Depth Measurements
| Total N=1029 |
Site A | Site B | Site C | Site D | Site E | Site F | Site G | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| Chest compression depth (mm) - median (Q1, Q3) - mean (SD) |
37.3 (31.6, 43.5) 37.9 (10.0) |
39 (33, 46) 40 (10) |
39 (33, 44) 40 (9) |
36 (30, 44) 37 (11) |
35 (30, 42) 36 (9) |
39 (30, 44) 37 (8) |
39 (34, 43) 38 (8) |
39 (30, 42) 36 (9) |
<0.001 |
|
| |||||||||
| Compression Depth Category - % (n) | |||||||||
| <38 mm | 52.8% (543) | 46% | 44% | 59% | 61% | 43% | 42% | 40% | |
| 38-51 mm | 38.7% (398) | 40% | 44% | 31% | 35% | 54% | 55% | 60% | |
| >51 mm | 8.6% (88) | 14% | 13% | 10% | 4% | 2% | 3% | 0% | <0.001 |
|
| |||||||||
| Within Depth Range1 - % (n) | 40.7% (419) | 47% | 45% | 36% | 35% | 48% | 45% | 40% | 0.018 |
|
| |||||||||
| Percent of minutes in recommended range - mean (SD) |
47.3% (41%) | 54% (43%) | 53% (38%) | 42% (41%) | 42% (39%) | 54% (42%) | 50% (43%) | 43% (39%) | 0.003 |
Average depth at least 38 mm for more than 60% of minutes with CPR process measures available.
In Table 3 we see that compression rate and depth are inversely related (P< 0.001) such that for the 20% of cases with a mean compression rate greater than 120 per minute, the majority (70%) had inadequate compression depth.
Table 3.
Compression Rate versus Compression Depth
| Average Compression Rate / Minute | |||||
|---|---|---|---|---|---|
| 0 to 80 | 81 to 120 | 121+ | Total | ||
|
Average
Compression Depth |
<38 mm | 44 (52%) | 351 (48%) | 148 (70%) | 543 (53%) |
| 38-51 mm | 25 (29%) | 315 (43%) | 58 (28%) | 398 (39%) | |
| >51 mm | 16 (19%) | 68 (9%) | 4 (2%) | 88 (9%) | |
| Total | 85 (100%) | 734 (100%) | 210 (100%) | 1029 (100%) | |
Chi-square test for association: p<0.001
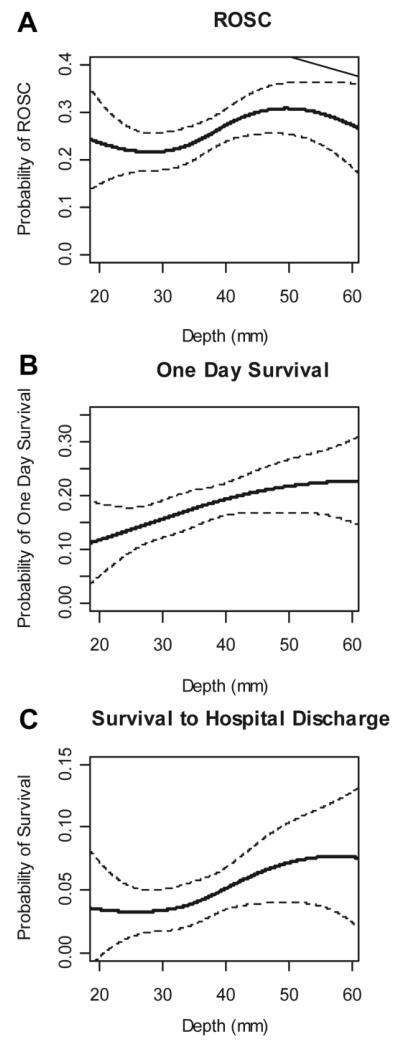
A smoothed spline plot of compression depth versus the three outcome measures (Figure 2) shows much poorer outcomes for patients with the lowest mean compression values and a gradual increase in the probability of good outcome as average depth increases.
Figure 2. Plots of Outcomes versus Average Compression Depth.
We compared the univariate characteristics of the 50 patients who survived to discharge with those who did not (Table 4) and found better outcomes if the compression depth was greater than 38 mm (P=0.05). We conducted multivariate analyses (Table 5) to evaluate the impact of compression depth and other covariates on the three survival measures. Not unexpectedly, the factors most strongly associated with good outcomes were arrest in a public location and bystander witnessed cases. All depth measures (mean values, categories, and within recommended range) showed strong trends towards better outcomes for all three survival measures. The adjusted odds ratios with 95% CIs for each 5mm increment in compression depth and the outcomes were: ROSC 1.05 (0.98-1.14), 1-day survival 1.08 (0.99, 1.18), 3) discharge 1.09 (0.94, 1.27). The respective odds ratios for cases with depth 38-51 mm were ROSC 1.24 (0.90, 1.70), 1-day survival 1.52 (1.06, 2.18), 3) discharge 1.91 (0.95, 3.83). Interestingly, adjusted odds ratios for cases with depth > 51 mm were not better than those for cases with depth 38-51 mm, although CIs were wide. Finally the odds ratios for within recommended depth range were ROSC 1.25 (0.92, 1.71), 1-day survival 1.36 (0.96, 1.93), 3) discharge 1.50 (0.79, 2.84).
Table 4.
Univariate comparison of clinical characteristics of patients who did and did not survive to hospital discharge
| Outcome | |||
|---|---|---|---|
| Deaths | Survivors | p-value from Chi- squared or t-test |
|
| N=979 | N=50 | ||
| Age - mean (sd) | 68.1 (16.6) | 63.2 (17.1) | 0.052 |
| Male - n (%) | 604 (62%) | 36 (72%) | 0.135 |
| Public location – n (%) | 114 (12%) | 19 (38%) | <0.001 |
| Bystander witnessed – n (%) | 379 (39%) | 34 (68%) | <0.001 |
| Bystander CPR – n (%) | 355 (36%) | 22 (44%) | 0.273 |
| ALS first on scene – n (%) | 297 (31%) | 17 (35%) | 0.790 |
| ALS on scene – n (%) | 969 (99%) | 50 (100%) | 0.317 |
| Epinephrine - n (%) | 822 (84%) | 24 (48%) | <0.001 |
| Time from 911 call to scene – median (Q1, Q3) | 5.5 (4.2, 6.8) | 5.2 (4.0, 6.8) | 0.160 |
| Time from 911 Call to first EMS shock assessment – median (Q1, Q3) | 10.6 (8.6, 12.7) | 8.6 (7.6, 11.2) | 0.190 |
|
| |||
| CPR prior to first analysis – n (%) | 596 (61%) | 28 (56%) | 0.493 |
| CPR fraction – median (Q1, Q3) | 0.66 (0.56, 0.75) | 0.55 (0.43, 0.69) | <0.001 |
| Chest compression rate – median (Q1,Q3) | 106 (96, 117) | 105 (90, 112) | 0.013 |
|
| |||
| Chest compression depth (mm) – median (Q1, Q3) | 37 (31, 43) | 39 (34, 46) | 0.079 |
| Compression Depth Category - % (n) | 0.050 | ||
| <38 mm | 54% (525) | 36% (18) | |
| 38-51 mm | 38% (372) | 52% (26) | |
| >51 mm | 8% (82) | 12% (6) | |
| Within Recommended Depth Range1 - % (n) | 40% (394) | 50% (25) | 0.174 |
| Percent of minutes in depth range - mean (SD) | 47% (41%) | 58% (38%) | 0.046 |
|
| |||
| First rhythm – n (%) | <0.001 | ||
| VF/VF | 207 (21%) | 36 (72%) | |
| PEA | 151 (16%) | 9 (18%) | |
| Asystole | 488 (50%) | 1 (2%) | |
| AED no shock, no strip | 118 (12%) | 4 (8%) | |
| Cannot Determine | 8 (1%) | 0 (0%) | |
Note: percentages are of cases with non-missing data
Table 5.
Multivariate adjusted odds ratios for covariates associated with outcomes
| Pre-hospital ROSC | Survival to day after arrest |
Survival to discharge |
|
|---|---|---|---|
| Adjusted OR (CI)1 | Adjusted OR (CI)1 |
Adjusted OR (CI)1 |
|
| Compression Depth (5mm increments) | 1.05 (0.98, 1.14) | 1.08 (0.99, 1.18) | 1.09 (0.94, 1.27) |
|
| |||
| Compression Depth Category | |||
|
| |||
| <38 mm | reference | reference | reference |
| 38-51 mm | 1.24 (0.90, 1.70) | 1.52 (1.06, 2.18) | 1.91 (0.95, 3.83) |
| >51 mm | 1.43 (0.82, 2.49) | 1.23 (0.65, 2.34) | 1.52 (0.52, 4.45) |
|
| |||
| Within Depth Range2 | 1.25 (0.92, 1.71) | 1.36 (0.96, 1.93) | 1.50 (0.79, 2.84) |
|
| |||
| Percent of minutes in depth range (10% change) | 1.03 (1.00, 1.07) | 1.04 (1.00, 1.09) | 1.06 (0.98, 1.15) |
|
| |||
| Age (one year increase) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 0.99 (0.97, 1.01) |
|
| |||
| Male | 0.77 (0.56, 1.06) | 0.79 (0.55, 1.14) | 0.96 (0.47, 1.96) |
|
| |||
| Public location | 1.90 (1.24, 2.89) | 2.35 (1.51, 3.66) | 3.65 (1.79, 7.43) |
|
| |||
| Bystander witnessed | 2.68 (1.96, 3.66) | 2.11 (1.48, 3.00) | 3.29 (1.64, 6.59) |
|
| |||
| Bystander CPR | 0.99 (0.72, 1.36) | 1.08 (0.76, 1.55) | 1.21 (0.63, 2.35) |
|
| |||
| Time from 911 call to EMS on scene | 0.98 (0.92, 1.05) | 0.95 (0.88, 1.02) | 0.91 (0.78, 1.05) |
|
| |||
| CPR Fraction (10% increase) | 0.99 (0.89, 1.10) | 0.94 (0.83, 1.06) | 0.69 (0.55, 0.86) |
|
| |||
| Chest compression rate (10 compressions/minute increase) | 1.00 (0.92, 1.08) | 0.97 (0.88, 1.06) | 0.89 (0.76, 1.04) |
Adjusted for age, sex, public location, bystander witnessed arrest, bystander CPR, CPR fraction, chest compression rate, site, and time from 911 call to EMS at scene.
Average depth at least 38 mm for at least 60% of minutes with CPR process measures available.
Fifty-five subjects missing the time from 911 call to EMS on scene were excluded from these analyses.
The odds ratios for each of the depth measures was estimated from a separate multivariable logistic regression model. The estimates and confidence intervals for the other covariates come from the model that includes depth as a linear variable.
DISCUSSION
Interpretation of Findings
We believe this is the first large clinical study to comprehensively evaluate the performance of EMS providers with regards to their performance of compression depth in OOHCA patients. We found that responders from 58 EMS agencies at seven major clinical sites were very often not within recommended range for compression depth guidelines. More than half of patients received less than the 2005 recommended chest compression depth of 38-51 mm and more than 90% received less than the 2010 recommended depth > 50 mm. We also found a significantly deleterious effect on compression depth when the mean compression rate was faster than recommended. We found an association between adequate compression depth and good outcomes but could not demonstrate that the 2010 recommendations are better than those from 2005. While we believe that compression depth is an important component of CPR and should be measured routinely during cardiac arrest resuscitation, we believe that the optimal depth is currently unknown.
Previous Studies
Current CPR guidelines for compression depth have been, for the most part, derived with relatively little robust human data to support them.3;12 Animal studies have suggested better outcomes with increased compression depth.20-22 Clinical studies of compression depth have been small with insufficient power to evaluate clinically important outcomes and have tended to focus on VF patients only.7;13-15 Wik described CPR performance measures in 176 patients in Europe and found that 33% of patients had compression depths less than the guidelines.7 Abella found compression depth to be too shallow in 37% of 67 in-hospital cardiac arrest cases but could not show an association between depth and outcome.13 Edelson and Babbs separately studied patients who received defibrillation and found an association between greater compression depth and shock success.14;23 Kramer-Johansen evaluated 284 patients and found better hospital admission rates with increased compression depth.15 The 2010 CPR guidelines have very significantly increased the recommended minimum compression depth from 38 mm to 50 mm, based on extrapolation from limited human data.12 Our results support compression depth > 38 mm but not necessarily depth > 50mm.
Limitations and Strengths
The study population represents a convenience sample of cases from sites where compression depth could be measured and where electronic recordings were available and during a period when the 2005 guideline standards were in use. Nevertheless, we could detect no selection bias in our cases. Our records could not capture CPR data prior to the placement of accelerometer pads, a time period likely to have been about 30 seconds. In addition, we did not collect data or adjust for body size, firmness of the surface under the patient, leaning, or duty cycle, possible confounders to the interpretation of compression depth data. We did, however, adjust for sex which may be considered a crude proxy for weight. A small proportion of cases had real-time CPR feedback that may have improved compression depth.24 Finally, we only evaluated CPR measurements in adults. The major strengths of the study include a relatively large sample of patients from seven geographically disparate locations in the U.S. and Canada and the use of devices from two different manufacturers.
We believe our survival rate of 4.9% is lower than in previous ROC Epistry studies because we excluded cases witnessed by EMS or that received bystander AED shocks. In addition, several sites with historically better survival rates were not included because of an inability to measure compression depth.
Some may be surprised that we did not find chest compression fraction to be positively associated with survival as was shown in another ROC Epistry study.11 Our study, however, differed by including all rhythms, by including cases from different sites, and by having a higher proportion (65%) of cases with moderate to high chest compression fraction (i.e. > 60%).
Clinical Implications
This study has a number of important implications for those performing CPR. Our data suggest that clinical outcomes are directly related to increased compression depth and EMS providers must strive to ensure that they provide adequate depth and perhaps as much depth as possible. This goal can be furthered by emphasis on proper depth during training, by use of real-time feedback during resuscitation, and post resuscitation review of quality assurance data. Interestingly, while our data support compression depth greater than 38 mm, it does not necessarily support the new 2010 guidelines that recommend > 50 mm of depth. We have also demonstrated that depth suffers when compression rate is too fast, another parameter that rescuers must be aware of. Of note, the 2010 guidelines also do not specify an upper limit for rate. The optimal combination of rate and depth is unknown but at this time, we believe that rescuers should be cautious not to exceed a compression rate of 120 in order to deliver sufficient compression depth. We expect the international guidelines will require further revisions as more data are acquired.
Research Implications
Even larger studies are required in order to evaluate the optimal compression depth for adults and to better understand the interplay with compression rate, ventilations, compression fraction, duty cycle, recoil, body size, and surface firmness. Such studies are particularly urgent in view of the new guidelines that recommend a substantial increase in recommended compression depth. In addition, more data for children are required in order to understand the best CPR process parameters to optimize survival.
Conclusions
This is the first clinical study to comprehensively evaluate the performance compression depth by EMS in a large sample of patients during OOHCA. We found suboptimal compression depth in half of patients by the existing 2005 guideline standards and almost all by the subsequent 2010 standards, as well as an inverse association between compression depth and rate. We found a strong association between survival outcomes and increased compression depth but no clear evidence to support or refute the 2010 recommendations of > 50 mm. While compression depth is an important component of CPR and should be measured routinely, the most effective depth is currently unknown.
Acknowledgements
We gratefully acknowledge the tremendous effort and contribution of thousands of EMS providers and first responders who made this logistically challenging trial possible.
Funding Acknowledgement
The ROC is supported by a series of cooperative agreements to 10 regional clinical centers and one Data Coordinating Center (5U01 HL077863, HL077881,HL077871 HL077872, HL077866, HL077908, HL077867, HL077885, HL077887, HL077873, HL077865) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Materiel Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada and the American Heart Association.
Footnotes
Disclosures
None
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ian G. Stiell, Department of Emergency Medicine and Ottawa Hospital Research Institute, University of Ottawa, Ottawa, ON, Canada
Siobhan P. Brown, Clinical Trials Centre, Department of Biostatistics, University of Washington, Seattle, WA, USA
James Christenson, Department of Emergency Medicine, University of British Columbia; BC Emergency and Health Services Commission; Vancouver, BC, Canada.
Sheldon Cheskes, Department of Family and Community Medicine, University of Toronto and Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada.
Graham Nichol, Clinical Trials Centre, Department of Biostatistics and Department of Medicine, University of Washington; University of Washington-Harborview Center for Prehospital Emergency Care, Seattle, WA, USA.
Judy Powell, Clinical Trials Centre, Department of Biostatistics, University of Washington, Seattle, WA, USA.
Blair Bigham, Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada.
Laurie J. Morrison, Department of Medicine, University of Toronto and Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON, Canada
Jonathan Larsen, Seattle Fire Department Medic One, Seattle, WA, USA.
Erik Hess, Department of Emergency Medicine, Division of Emergency Medicine Research, Mayo Clinic College of Medicine, Rochester, MN, USA.
Christian Vaillancourt, Department of Emergency Medicine and Ottawa Hospital Research Institute, University of Ottawa, Ottawa, ON, Canada.
Daniel P Davis, Department of Emergency Medicine, University of California, San Diego, CA, USA.
Clifton W. Callaway, Department of Emergency Medicine, University of Pittsburgh, Pittsburgh, PA, USA
REFERENCES
- (1).Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2).Cummins RO, Ornato JP, Thies WH, Pepe PE. Improving survival from sudden cardiac arrest: the “chain of survival” concept. Circulation. 1991;83:1832–1847. doi: 10.1161/01.cir.83.5.1832. [DOI] [PubMed] [Google Scholar]
- (3).2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- (4).Stiell IG, Wells GA, Field BJ, Spaite DW, Nesbitt L, De Maio VJ, et al. Advanced Cardiac Life Support in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2004;351:647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- (5).Rea TD, Cook AJ, Stiell IG, Powell J, Bigham B, Callaway CW, et al. Predicting survival after out-of-hospital cardiac arrest: role of the Utstein data elements. Ann Emerg Med. 2010;55(3):249–257. doi: 10.1016/j.annemergmed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- (6).Peberdy MA, Ornato JP. Post-resuscitation care: is it the missing link in the Chain of Survival? Resuscitation. 2005;64(2):135–137. doi: 10.1016/j.resuscitation.2004.09.015. [DOI] [PubMed] [Google Scholar]
- (7).Wik L, Kramer-Johansen J, Myklebust H, Sorebo H, Svensson L, Fellows B, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293(3):299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- (8).Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O’Hearn N, Wigder HN, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- (9).Kramer-Johansen J, Edelson DP, Losert H, Kohler K, Abella BS. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR) Resuscitation. 2007;74(3):406–417. doi: 10.1016/j.resuscitation.2007.01.024. [DOI] [PubMed] [Google Scholar]
- (10).Aase SO, Myklebust H. Compression depth estimation for CPR quality assessment using DSP on accelerometer signals. IEEE Trans Biomed Eng. 2002;49(3):263–268. doi: 10.1109/10.983461. [DOI] [PubMed] [Google Scholar]
- (11).Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, et al. Chest Compression Fraction Determines Survival in Patients With Out-of-Hospital Ventricular Fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Sayre MR, Koster RW, Botha M, Cave DM, Cudnik MT, Handley AJ, et al. Part 5: adult basic life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 Suppl 2):S298–S324. doi: 10.1161/CIRCULATIONAHA.110.970996. [DOI] [PubMed] [Google Scholar]
- (13).Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O’Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- (14).Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. 2006;71(2):137–145. doi: 10.1016/j.resuscitation.2006.04.008. [DOI] [PubMed] [Google Scholar]
- (15).Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sorebo H, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: A prospective interventional study. Resuscitation. 2006;71(3):283–292. doi: 10.1016/j.resuscitation.2006.05.011. [DOI] [PubMed] [Google Scholar]
- (16).Ornato JP, Peberdy MA. Measuring Progress in Resuscitation: It’s Time for a Better Tool. Circulation. 2006;114(25):2754–2756. doi: 10.1161/CIRCULATIONAHA.106.668095. [DOI] [PubMed] [Google Scholar]
- (17).Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry - Cardiac Arrest. Resuscitation. 2008;78:161–169. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Davis DP, Garberson LA, Andrusiek DL, Hostler D, Daya M, Pirrallo R, et al. A descriptive analysis of Emergency Medical Service Systems participating in the Resuscitation Outcomes Consortium (ROC) network. Prehosp Emerg Care. 2007;11(4):369–382. doi: 10.1080/10903120701537147. [DOI] [PubMed] [Google Scholar]
- (19).ZOLL Medical Corporation . E series operators guide. ZOLL Medical Corporation; Chelmsford, MA, USA: 2010. [Google Scholar]
- (20).Li Y, Ristagno G, Bisera J, Tang W, Deng Q, Weil MH. Electrocardiogram waveforms for monitoring effectiveness of chest compression during cardiopulmonary resuscitation. Crit Care Med. 2008;36(1):211–215. doi: 10.1097/01.CCM.0000295594.93345.A2. [DOI] [PubMed] [Google Scholar]
- (21).Ristagno G, Tang W, Chang YT, Jorgenson DB, Russell JK, Huang L, et al. The quality of chest compressions during cardiopulmonary resuscitation overrides importance of timing of defibrillation. Chest. 2007;132(1):70–75. doi: 10.1378/chest.06-3065. [DOI] [PubMed] [Google Scholar]
- (22).Wu JY, Li CS, Liu ZX, Wu CJ, Zhang GC. A comparison of 2 types of chest compressions in a porcine model of cardiac arrest. Am J Emerg Med. 2009;27(7):823–829. doi: 10.1016/j.ajem.2008.07.001. [DOI] [PubMed] [Google Scholar]
- (23).Babbs CF, Kemeny AE, Quan W, Freeman G. A new paradigm for human resuscitation research using intelligent devices. Resuscitation. 2008;77(3):306–315. doi: 10.1016/j.resuscitation.2007.12.018. [DOI] [PubMed] [Google Scholar]
- (24).Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]